- 1Department of Pharmacology and Toxicology, Faculty of Pharmacy, University of Uyo, Uyo, Nigeria
- 2Department of Anatomy, Faculty of Basic Medical Sciences, College of Health Sciences, University of Port Harcourt, Port Harcourt, Nigeria
- 3Department of Cardiovascular and Endocrine-Metabolic Diseases, and Aging, Istituto Superiore di Sanità, Rome, Italy
- 4Department of Experimental Pharmacology & Toxicology, Faculty of Pharmacy, University of Port Harcourt, Port Harcourt, Nigeria
- 5African Centre of Excellence for Public Health and Toxicological Research (ACE-PUTOR), University of Port Harcourt, Port Harcourt, Nigeria
There is a strong relationship between a healthy diet and mental well-being. Several foods and food compounds are known to modulate biomarkers and molecular mechanisms involved in the aetiogenesis of several mental disorders, and this can be useful in containing the disease progression, including its prophylaxis. This is an updated systematic review of the literature to justify the inclusion and recognition of nutrition in the management of psychiatric illnesses. Such foods and their compounds include dietary flavanols from fruits and vegetables, notable antioxidant and anti-inflammatory agents, probiotics (fermented foods) known to protect good gut bacteria, foods rich in polyunsaturated fatty acids (e.g., Omega-3), and avoiding diets high in saturated fats and refined sugars among others. While the exact mechanism(s) of mitigation of many nutritional interventions are yet to be fully understood, the evidence-based approach warrants the inclusion and co-recognition of nutrition in the management of psychiatric illnesses. For the greater public health benefit, there is a need for policy advocacy aimed at bridging the knowledge gap and encouraging the integration of nutritional intervention with contemporary therapies in clinical settings, as deficiencies of certain nutrients make therapy difficult even with appropriate medication.
Introduction
Mental disorders are widespread and impact significantly on health (1). In 2016, mental and addictive disorders affected more than 1 billion people globally and contributed 7% of the global burden of diseases (2). However, mental disorders manifest differently; according to WHO, they are generally characterized by a combination of abnormal thoughts, perceptions, emotions, behavior, and relationships with others (1). Current treatment involves the use of drugs such as antidepressants, antipsychotics, sedative-hypnotics, anxiolytics, stimulants, and mood stabilizers, along with psychotherapy (talk therapy). Electroconvulsive therapy (ECT) involving the application of electrical currents to the brain is used in some disorders that are unresponsive to other treatments.
“Nutritional psychiatry” pivots on the impact of nutrition (food) on the state of mind and mood. This presents an opportunity to augment clinical interventions as well as to mitigate the adverse effects of medications used in the treatment of psychiatric disorders (3, 4). Accumulating literature suggests a significant relationship between poor diet and the exacerbation of mood disorders, such as anxiety, depression, and other neuropsychiatric conditions (5). The likelihood of a healthy diet to produce beneficial effects on mental health among clinical and non-clinical subjects deserves more attention (6), and dietary interventions need to be refined and scaled up for maximum benefit in the management of mental disorders (7–9).
This review aims at updating the concept of “Nutritional Psychiatry” by (i) highlighting the various biomarkers and molecular mechanisms that form the hallmark of various mental disorders; (ii) examining foods and food compounds that can ameliorate the mechanistic derangement as evidence for the possibility of incorporating dietary interventions in the clinical management of psychiatric disorders.
Methodology
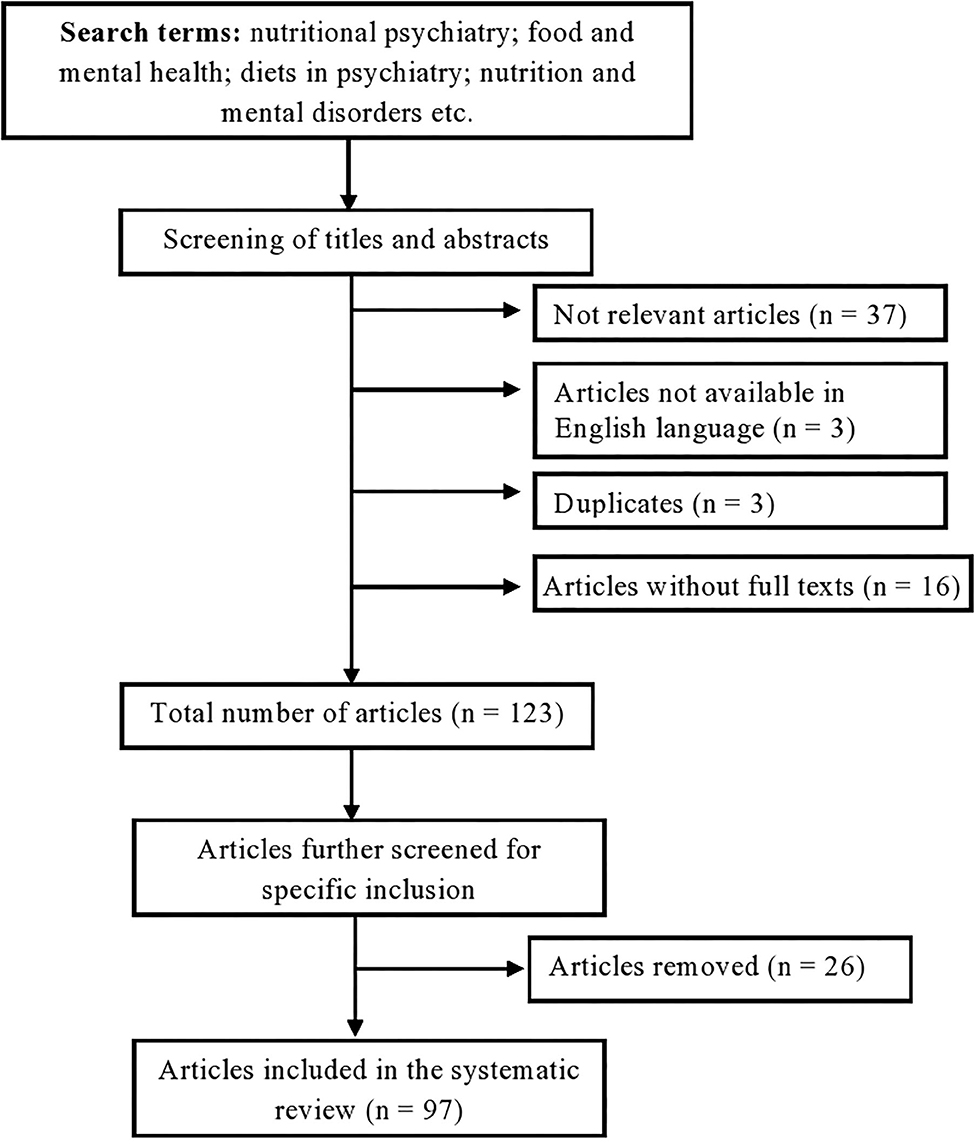
Multiple online searches were carried out in the databases of Medline, Pubmed, Scopus and Google Scholar in May 2020 using terms like “Nutritional psychiatry,” “food and mental health,” “diets in psychiatry,” “nutrition and mental disorders,” “food and food compounds and mental health,” “biomarkers of psychiatric disorders,” and “mechanisms of mental disorders.” Sourced works of literature were screened, and full texts were obtained. Inclusion and exclusion criteria determined the suitability of the literature used in this review. In particular, studies were included if focusing on a whole food, supplements, or compounds (isolated from food) targeting psychiatric disorders. Articles were excluded when (a) not relevant, i.e., the nutritional source was meant to mitigate illnesses different from mental disorders, (b) unavailable in English, and (c) unavailable in full-text.
Results and Discussion
Search Results
One hundred and eighty-two (182) studies were found in the initial search. After a screening of both titles and abstracts, 59 articles were excluded; in particular, 37 articles were not relevant, 16 full texts were unavailable, 3 were unavailable in English, 3 were duplicates. Further review of the full texts of the remaining 123 articles with strict application of the inclusion and exclusion criteria resulted in the exclusion of 26 articles, thus leaving 97 studies that were included in this review (Figure 1).
There are several types of diagnosable mental disorders that are known to cause significant alterations in behavioral, thoughts, emotional and functional disabilities. They include but are not limited to the following: depression (1), bipolar disorder (10), schizophrenia (11), dementia, autism spectrum disorder, generalized anxiety disorder (12, 13), attention-deficit/hyperactivity disorder (14), obsessive-compulsive disorder (15, 16), post-traumatic stress disorder (17) and eating disorders such as anorexia nervosa and bulimia nervosa (18).
Molecular Mechanisms and Biomarkers of Psychiatric Disorders
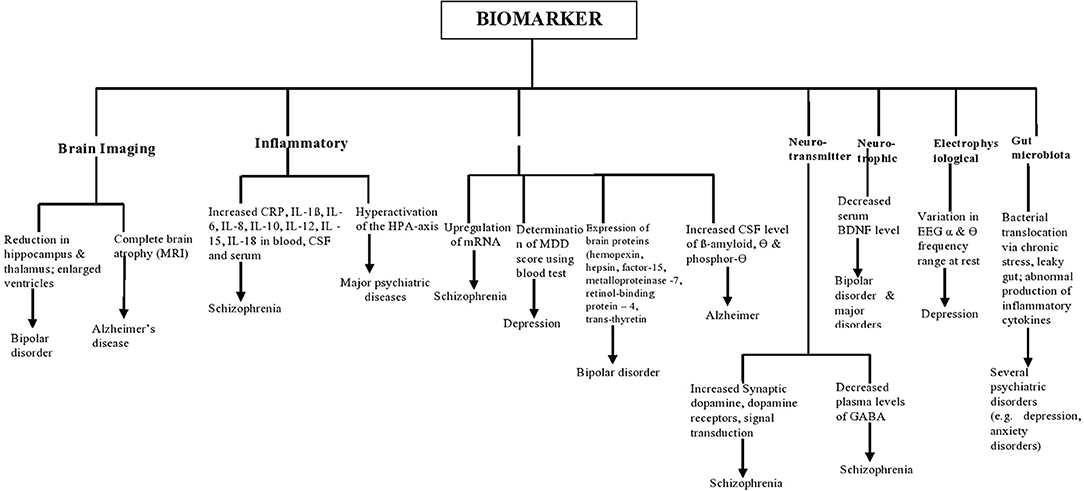
The term biomarker can be referred to as a characteristic that is objectively measured and evaluated as an indicator of normal biologic processes, pathologic processes, or biological responses to a therapeutic intervention (19). It can be a gene, a group of genes, proteins, or other biomolecules (20). Due to the complexity of psychiatric disorders, biomarkers cannot be limited to molecular biology in psychiatry. Advances in neuroimaging methods have modernized the understanding of the bio-clinical substrata of many psychiatric disorders (21, 22). Clinical uses of biomarkers in psychiatry involve measuring them before the intervention and with the goal of predicting drug response, diagnosis, therapeutic failure, prognosis, pharmacotoxicity, and classification within diagnostic categories (23–26). They include inflammatory biomarkers such as high levels of cytokines and C-reactive protein (CRP), changes in serum molecules involved in pro-inflammatory and oxidative stress response, including hyperactivation of the hypothalamic-pituitary-adrenal (HPA) axis (27). Elevated levels of pro-inflammatory cytokines have been observed in patients with depression (28–31), schizophrenia (32, 33), and eating disorders (34).
Protein biomarkers involve the expression of proteins in the brains such as growth differentiation factor-15, hemopexin, hepsin, matrix metalloproteinase-7, retinol-binding protein-4, and trans-thyretin, which have been reported as biomarkers to distinguish patients with bipolar disorder from those without the disorder (35); up-regulation of microRNA utilized as a biomarker for diagnosis of patients with schizophrenia (36); increased cerebrospinal fluid levels of β-amyloid, tau, and phosphor-tau for Alzheimer's disease (37).
Disturbances in central and peripheral Neurotransmitters biomarkers are also indicators of mental disorders such as major depressive disorders. These neurotransmitters include dopamine, glutamate, γ-aminobutyric acid (GABA), and serotonin (38). Neurotrophic biomarkers such as expression of the brain-derived neurotrophic factor, BDNF in cognitive impairments in individuals with mental disorders is of utmost research interest (39). Electrophysiological biomarkers used in psychiatry include imbalances in resting heart rate (RHR), heart rate variability (HRV), respiration rate (RR), skin temperature (ST), skin conductance (SC) (40, 41), event-related potentials (ERP) and visual evoked potentials (42). ERP measures the electrical activity of the cerebral surface that represents a distinct phase of cortical processing. It is made up of two components, namely P300 positivity and N200 negativity (43). It has been reported that P300 activity may serve as a useful biomarker of attention and as a screen for combination-drug therapy in investigations of anti-Alzheimer drugs (44). In addition, several neuroimaging techniques like Magnetic Resonance Imaging (MRI), Positron Emission Tomography scan (PET scan), Single Positron Emission Tomography scan (SPECT scan), Magnetic [Resonance Spectroscopy (MRS), Functional Magnetic Resonance Imaging (fMRI), and Diffuse Tensor Imaging (DTI) are currently employed to find biomarkers for mental illness (45) and to clearly elucidate the neural basis of the psychiatric disorder (40)]. The gut microbiota could control functional pathways in the brain and, therefore, useful as both biomarkers and potential drug targets in mental disorders (46). The gut microbiome has been demonstrated to play an essential role in the development and function of the hypothalamic-pituitary-adrenal (HPA) axis, which mediates the stress response and is involved in a range of psychiatric disorders, especially depression and anxiety disorders (47, 48). The use of antibiotics, Western diets, and excessive-stress lifestyles culminate in gut bacterial imbalances, known as dysbiosis, in addition to low diversity. Bacteria have the ability to produce GABA, tryptophan, 5-HT, and several neurotransmitters and monoamines MOA. Pathophysiology of mental disorders has also been linked to bacterial translocation via increased gut permeability (49). Anxiety, stress, and depression can increase gut barrier permeability, resulting in a ‘leaky gut,’ which allows bacteria to seep into circulation, leading to the inflammatory response (50–52).
A schematic illustration of some biomarkers in psychiatric disorders is shown in Figure 2.
Foods and Food Compounds that Affect Psychiatric Biomarkers
A strong relationship between a healthy diet and mental well-being is often reported by people. Elation, mental health, and well-being have reportedly been increased by the increase in the consumption of fresh fruits and vegetables (53–56). Dietary flavanols, namely kaempferol, isorhamnetin, and myricetin (i.e., components of many fruits, vegetables, and tea), have been linked to a significantly lower risk of development of Alzheimer's disease (57). Many flavonoid classes, including flavonols, are anti-inflammatory and antioxidants.
Some common fruits like citrus (e.g., lime, lemon, orange, tangerine, grape), guava, cashew, mango, pawpaw, pineapple, avocado, banana, African star apple, sweetsop/ sugar apple, breadfruit, soursop, African bush mango, passion fruit, apple, dates (58) and vegetables (e.g., tomatoes, okra, eggplant, cucumber, beets, garlic, onion, and ginger) found in sub-Saharan Africa may be of nutritional psychiatry relevance (58). These fruits and vegetables have high levels of micronutrients such as zinc, magnesium, selenium, iron, and vitamins (59, 60). These micronutrients may modulate the risk of mental disorder, such as depression, via effects on the production and activity of monoamine neurotransmitters like serotonin, alterations to the HPA system, glutamatergic signaling, or inflammatory and oxidative stress (61, 62). These plant-based foods contain antioxidant phytochemicals, such as polyphenols, vitamin C, and flavonoids, i.e., substances whose antidepressant-like or anxiolytic effects have been reported (63, 64).
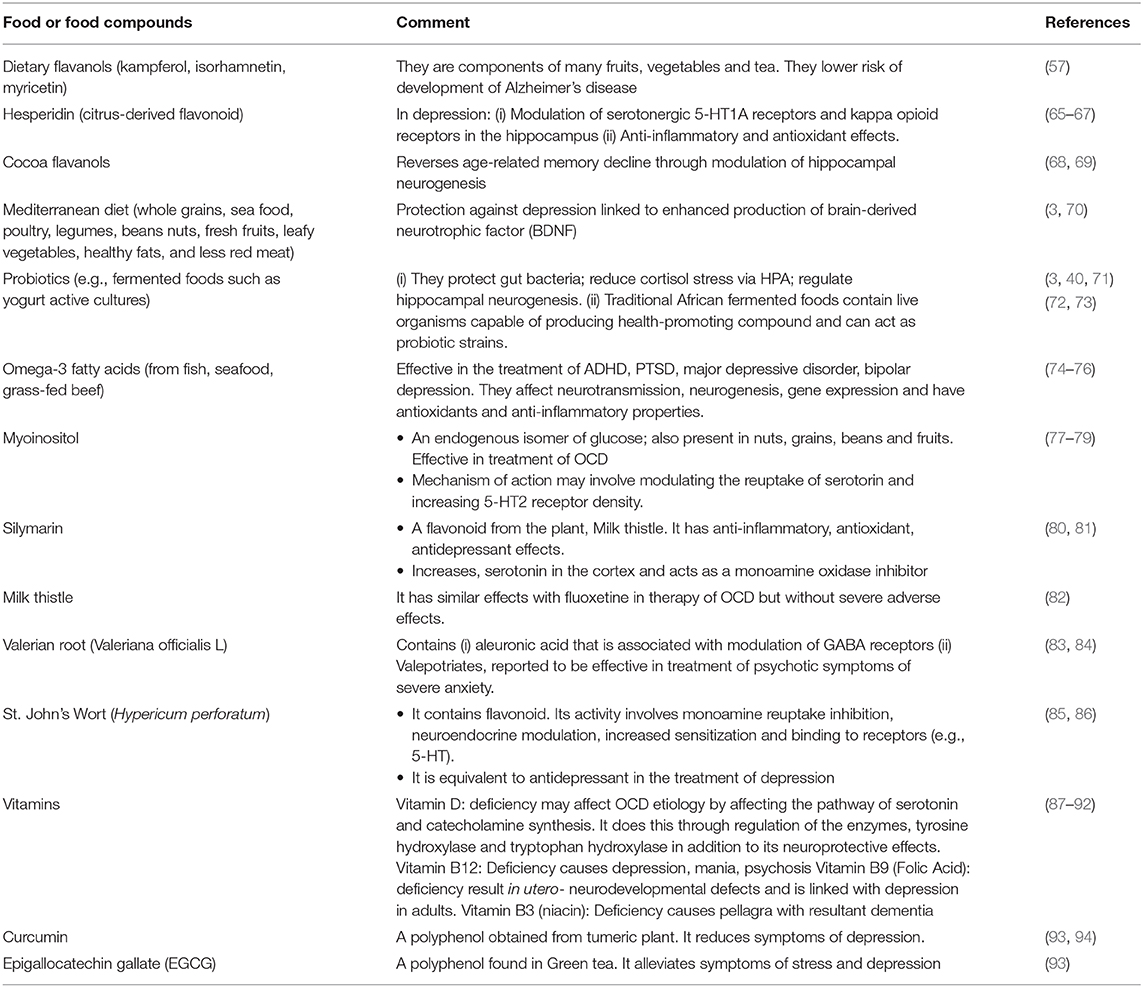
Several foods/food compounds are known to affect some psychiatric disorders in different ways. They include several phytochemicals like flavonoids, probiotics, omega-3 fatty acids, vitamins, myoinositol, Curcumin, plant parts like valerian root, milk thistle, and green tea (Table 1). These nutrients may affect mental disorders via several mechanisms such as the production and activity of monoamine neurotransmitters, neurotransmission, modulation of hippocampal neurogenesis, hypothalamic-pituitary-adrenal (HPA) system, anti-inflammatory and antioxidant effects, augmenting the production of brain-derived neurotrophic factor, BDNF or the protection of gut bacteria, among others. These bio-molecular mechanisms of dietary interventions in some mental disorders are summarized in Figure 3.
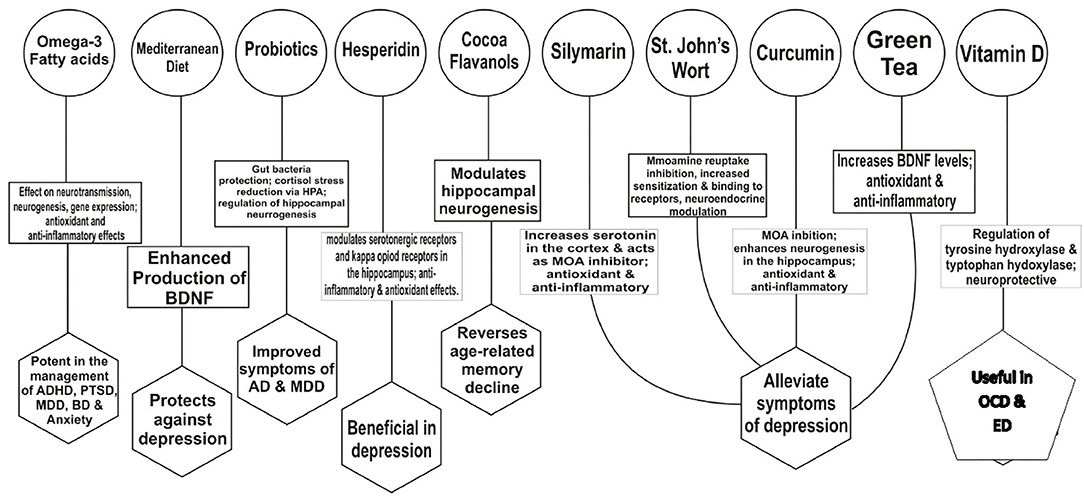
Figure 3. Bio-molecular mechanisms of dietary interventions in some mental disorders. HPA, hypothalamic-pituitary-adrenal axis; OCD, Obsessive-Compulsive Disorder; MOA, Monoamine oxidase; BD, Bipolar disorder; BDNF, brain-derived neurotrophic factor; MDD, Major Depressive Disorder; ADHD, Attention deficit hyperactivity disorder; PTSD, Post traumatic stress disorder; AD, Alzheimer dementia; ED, Eating disorders.
High doses of naturally occurring cocoa flavanols have been reported to reverse memory decline associated with age (68). Flavanols seem to selectively improve the function of the dentate gyrus, i.e., a region within the hippocampus that is associated with aging and age-related memory decline (68). The hippocampus is a region of the brain associated with memory, learning, and mood. The extent of neurogenesis in the hippocampus is directly related to cognition and mood. Modulation of hippocampal neurogenesis by diet is a possible mechanism by which nutrition affects brain function, plasticity, and mental health (69).
Hesperidin, i.e., a citrus-derived flavonoid, has been reported to have neuroprotective effects, particularly against depression, learning, and memory deficits (95–97). Possible mechanisms of its antidepressant-like effects are regulation of serotonergic 5-HT1A receptors (65) and kappa opioid receptors in the hippocampus (66). Hesperidin has both anti-inflammatory and antioxidant effects (67). In a model of aluminum chloride-induced neuroinflammation in the hippocampus, the anti-inflammatory properties of hesperidin involve a reduction in the levels of pro-inflammatory mediators like tumor necrosis factor α (TNF-α) (98). Hesperidin has also been shown to protect the hippocampus by reducing levels of nitrate/nitrite while increasing levels of BDNF in the mouse (99). Its free radical scavenging and antioxidant abilities tend to ameliorate the shortfalls in the activity of glutathione peroxidase, glutathione reductase, catalase, and superoxide dismutase. In experimental models of stroke, irradiation, and LPS-induced endotoxicity, these antioxidant enzymes are down-regulated in the brain (100–102). The Mediterranean diet involves eating whole grains, seafood, and poultry (at least twice a week) and consuming legumes, beans, fresh fruit, leafy green vegetables, nuts (almonds, walnuts), cruciferous vegetables (cauliflower, broccoli), healthy fats (olive and canola oil), and a limited amount of red meat (3). According to a recent study, a Mediterranean diet and avoiding inflammation-producing foods may protect against depression (103). The mechanisms involved may be linked to enhanced production of BDNF, and therefore important functions such as neuroplasticity, neuronal survival, as well as growth and differentiation of new neurons and synapses (70). Low serum BDNF levels have been found in a number of psychiatric disorders like schizophrenia, major depressive disorder, PTSD, and Alzheimer's dementia (104). Diet can regulate or dysregulate the gut microbiome. Healthy gut microbiota is central in the regulation of serotonin metabolism because at least 90% of serotonin receptors are located in the gut (105). Alteration in the balance between “good” and “bad” bacteria may result in several diseases, including mood and cognitive disorders. Probiotic-rich foods (e.g., fermented foods such as yogurt with active cultures) are known to protect good gut bacteria (3). Fermented foods contain strains of Lactobacillus as well as yeasts and are vital because they contain both probiotic microbiota and microbial metabolites (59). Prebiotics, in their turns, include non-digestible fiber, which stimulates the growth of probiotics (70). Many prebiotics and probiotics reduce cortisol stress in healthy subjects (71, 106, 107). Several studies suggest that both individuals with clinically diagnosed cases and healthy individuals experiencing some anxiety and mood disorders benefit from the consumption of probiotics (108, 109). Several fermented foods are traditionally used in different parts of Africa' (110). These include fermented non-alcoholic cereals (mainly from sorghum, millet, and maize), starchy root crops (mainly from cassava), animal proteins (mainly dairy products), vegetable proteins (from legumes and oilseeds), and alcoholic beverages (e.g., from cereals, sap, honey, fruits) (111). These traditional African probiotics contain live microorganisms capable of producing health-promoting compounds like antimicrobials and essential nutrients or molecules with antioxidant activity (72, 73). The western diet, known for its content of ultra-processed foods, has been reported to change microbiome (gut environment), leading to reduced Lactobacilli (112), gut inflammation, and possibly contribute to disorders (113). Mediterranean diet reduces the numbers of inflammatory/pathogenic bacteria like Escherichia coli and increases important commensal bacteria such as Bifidobacteria (114), Clostridium cluster XVIa, and Faecalibacterium prausnitzii (115). Vegetarian diets have been reported to alter the microbial composition and reduce inflammation of the gut (116, 117). Pathogenesis of psychosis has been linked to anomalies in glucose tolerance, insulin resistance, mitochondrial dysfunction, and energy metabolism disturbances. These could be potential mechanisms for the effect of a ketogenic diet. This diet, high in fat, and low in carbohydrate, utilize ketone bodies as the fuel source for the brain, instead of glucose (118, 119). A report from investigators with the Nutrition Network of the European College of Neuropsychopharmacology (ECNP) postulates that a ketogenic diet may decrease seizures in children with epilepsy (5, 120).
Some diets have potentially harmful effects on the brain. A diet high in saturated fats and refined sugars has a powerful negative impact on brain proteins (neutrophins). Neutrophins are very important in depression: they protect the brain against oxidative stress and promote the growth of new brain cells (121). Del-Ponte and co-workers reported recently that food high in refined sugar and saturated fat might cause an increased risk for hyperactivity (ADHD) compared to fruits and vegetables (122). Eliminating the underlying suspected trigger foods may work as secondary prevention of food-induced ADHD: the “few-foods approach” is a diagnostic protocol allowing to determine whether or not individually composed few food diets (one food per week is added to the diet) are a trigger of ADHD. If the behavioral problems do not recur, the food can be included in the diet without restriction (123, 124).
Foods that contain aspartame, a food additive, are forbidden for people with phenylketonuria (a birth defect that causes the amino acid phenylalanine to build up in the body) as this can result in brain damage, intellectual disabilities, behavioral symptoms, or seizures (125).
Several studies have corroborated the fact that deficiency of some vitamins and other essential nutrients lead to cognitive impairments (126, 127). Vitamin D plays an important role in immunity modulation, inflammatory response, and antioxidant processes, as well as in normal brain development and functioning, neurotransmission, neuroprotection, proliferation, and differentiation (80, 128, 129). Vitamin D deficiency can be associated with numerous neuropsychiatric diseases, including autism, major depressive disorder, schizophrenia, and Obsessive-Compulsive Disorder (OCD) (130, 131). Vitamin D deficiency may contribute to OCD etiology by (i) affecting the pathway of serotonin and catecholamines synthesis, (ii) regulation of the levels of the enzymes tyrosine hydroxylase and tryptophan hydroxylase, (iii) deprived neuroprotective effect (87, 88). In adults aged 65 years and above, higher vitamin D serum levels were associated with better attention and working memory performance (132). Vitamin D has also been reported to support the nervous system and brain functions such as impulsive behaviors, known to be of importance in the prognosis and treatment of patients with Eating Disorders (133). Vitamin B12 deficiency causes depression, lethargy, poor memory, fatigue, mania, and psychosis (89), while vitamin B3 (niacin) deficiency causes pellagra with resultant dementia (90). Deficiency of vitamin B1 (thiamine) causes beriberi and numbness as CNS symptoms, while vitamin B9 (folic acid) deficiency results in in utero neurodevelopmental defects and is linked with depression in adults (91, 92).
Foods rich in polyunsaturated fatty acids, PUFAs (e.g., Omega-3s), and polyphenols have also been reported to have beneficial effects in neuroinflammation, cognitive performance, mood, and stress reactivity (134–137). Omega-3 fatty acids are effective in the treatment of attention-deficit/ADHD, major depressive disorder, bipolar depression, and post-traumatic stress disorder, or PTSD (74, 75). Omega-3 fatty acids are found in fish, seafood, and grass-fed beef (70). Omega-3 fatty acids are an integral part of neuronal cell membranes and affect several physiological mechanisms in the central nervous system. They affect neurotransmission, gene expression, neurogenesis, neuronal survival and also have antioxidants and anti-inflammatory properties (76). A balance between omega-6 and omega-3 fatty acids seems to be relevant in some mental disorders, as high omega-6 to an omega-3 fatty acid ratio in the blood has been associated with major depressive disorder and ADHD (56, 70).
Myoinositol (MI), an endogenous isomer of glucose also present in nuts, grains, beans, and fruits, is used in the treatment of mental disorders. It is essential for the synthesis of membrane phospholipids and for the intracellular secondary messenger cycle (77). Although some studies found no evidence for the efficacy of myoinositol in OCD treatment, others have reported the effectiveness of myoinositol supplementation in the treatment of OCD (78, 138). Available clinical evidence suggests that MI may potentially be effective as monotherapy in OCD (80). The suggested mechanisms of action involve modulation of the reuptake of serotonin and an increase in 5-HT2 receptor density (79). Silymarin, a flavonoid derived from the plant Milk thistle (Silybummarianum), has been reported to have anti-inflammatory, antioxidant, immune modulator, sedative, and antidepressant effects (80). It increases serotonin in the cortex and acts as a monoamine oxidase inhibitor (81). The effect of milk thistle and fluoxetine are alike in the treatment of OCD, and their positive effect starts in the 5th week without severe adverse effects (82). Valerian root (obtained from the plant Valeriana officinalis L contains aleuronic acid associated with the modulation of GABA receptors) (83) and valepotriates (effective in the treatment of the psychotic symptoms of severe anxiety) (84). St John's Wort (Hypericum perforatum), which is of plant origin, has been reported to be equivalent to an antidepressant in the treatment of depression (85, 86). It contains flavonoids, and its neurobiological activity involves monoamine reuptake inhibition, neuroendocrine modulation, increased sensitization, and binding to receptors (e.g., 5-HT) (85). Although some herbal medicines may provide a synergistic effect with conventional drugs, there should be some precautions in the use of some herbal supplements and some pharmaceuticals, for example, St John's Wort with SSRIs due to potential adverse serotonin syndrome (80). Polyphenols are natural compounds present in plant-based foods. They have unique properties and are capable of combatting oxidative stress as well as stimulate the activation of molecules that aid in synaptic plasticity, thereby enhancing cognitive function (93). Notable examples of polyphenols include Epigallocatechin gallate (EGCG) from green tea and Curcumin from turmeric. Apart from their antioxidant and anti-inflammatory properties, their mechanisms of action involve increased expression of BDNF, which enhances the reversal of neuronal atrophy and behavioral deficits (139). Curcumin has been reported to mitigate symptoms of depression by enhancing neurogenesis in the hippocampus and frontal cortex (94). It also inhibits the action of monoamine oxidase enzymes, thus preventing the breakdown of monoaminergic neurotransmitters, thereby increasing serotonin and dopamine levels (140). Epigallocatechin gallate from green tea has been reported to alleviate symptoms of stress and depression (93).
Conclusion
The field of nutritional psychiatry though still new, is currently undergoing intensive research, resulting in several positive research findings. As with many other diseases, several foods and food compounds are known to modulate biomarkers and molecular mechanisms involved in the aetiogenesis of several mental disorders, and this can be useful in containing the disease progression, including its prophylaxis. While the exact mechanism(s) of mitigation of many nutritional interventions are yet to be fully understood, the evidence-based approach warrants the inclusion and co-recognition of nutrition in the management of psychiatric illnesses. For the greater public health benefit, there is a need to advocate for policies aimed at bridging the knowledge gap and encourage the utilization and integration of nutrition in addition to contemporary therapies in clinical settings, as deficiencies of certain nutrients make therapy difficult even with the right medication. This is especially advantageous in developing, resource-challenged nations laden with inadequate healthcare funding for mental disorders, despite the condition being rife in the region and given the fact that these food substances are affordable and readily available in these nations.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
Author Contributions
SO conducted the search, data extraction, and drafting of manuscript. CO and OO conceptualization, reviewed the draft manuscript, and certified final manuscript. CF reviewed the draft manuscript. All authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. WHO, World health Organization. Mental Disorders. (2019). Available online at: https://www.who.int/news-room/fact-sheets/detail/mental-disorders (accessed April 3, 2020).
2. Rehm J, Shield KD. Global burden of disease and the impact of mental and addictive disorders. Curr Psychiatry Rep. (2019) 21:10. doi: 10.1007/s11920-019-0997-0
4. Sarris J, Logan AC, Akbaraly TN, Amminger GP, Balanzá-Martínez V, Freeman MP, et al. Nutritional medicine as mainstream in psychiatry. Lancet Psychiatry. (2015) 2:271–4. doi: 10.1016/S2215-0366(14)00051-0
5. Adan RAH, van der Beek EM, Buitelaar JK, Cryan JF, Hebebrand J, Higgs S, et al. Nutritional psychiatry: Towards improving mental health by what you eat. Eur Neuropsychopharmacol. (2019) 29:1321–32. doi: 10.1016/j.euroneuro.2019.10.011
6. Wu K, Gao X, Shi B, Chen S, Zhou X, Li Z, et al. Enriched endogenous n-3 polyunsaturated fatty acids alleviate cognitive and behavioral deficits in a mice model of Alzheimer's disease. Neuroscience. (2016) 333:345–55. doi: 10.1016/j.neuroscience.2016.07.038
7. Jacka FN. Nutritional psychiatry: where to next? EBioMedicine. (2017) 17:24–9. doi: 10.1016/j.ebiom.2017.02.020
8. Sanchez-Villegas A, Martinez-Gonzalez MA, Estruch R, Salas-Salvado J, Corella D, Covas MI, et al. Mediterranean dietarypattern and depression: the PREDIMED randomized trial. BMC Med. (2013) 11:208. doi: 10.1186/1741-7015-11-208
9. O'Neil A, Berk M, Itsiopoulos C, Castle D, Opie R, Pizzinga JA. Randomised, controlled trial of a dietary intervention for adults with major depression (the “SMILES” trial): study protocol. BMC Psychiatry. (2013) 13:114. doi: 10.1186/1471-244X-13-114
10. APA, American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th edn. Washington DC (2013).
11. Frankenburg FR. Schizophrenia. Medscape. (2020). Available online at: https://emedicine.medscape.com/article/288259-overview#a2 (accessed May 6, 2020).
12. NIMH, National Institute of Mental Health. Anxiety Disorders. (2018). Available online at: http://www.nimh.nih.gov/health/topics/eating-disorders/index.shtml (accessed May 9, 2020).
13. Brown TA, O'Leary TA, Barlow DH. Generalized anxiety disorder. In: Barlow DH, editor. Clinical Handbook of Psychological Disorders: A Step-by-Step Treatment Manual. 3rd edn. New York, NY: Guilford Press (2001). p. 154–208.
14. NIMH, National Institute of Mental Health. Attention-Deficit/Hyperactivity Disorder. (2019). Available online at: https://www.nimh.nih.gov/health/topics/attention-deficit-hyperactivity-disorder-adhd/index.shtml (accessed May 9, 2020).
15. NIMH, National Institute of Mental Health. Obsessive-Compulsive Disorder. (2019). Available online at: https://www.nimh.nih.gov/health/topics/obsessive-compulsive-disorder-ocd/index.shtml (accessed May 9, 2020).
16. Lochner C, Stein DJ. Heterogeneity of obsessive-compulsive disorder: a literature review. Harv Rev Psychiatry. (2003) 11:113–32. doi: 10.1080/10673220303949
17. Foa EB, Keane TM, Friedman MJ. Effective Treatments for PTSD: Practice Guidelines From the International Society for Traumatic Stress Studies. New York, NY: The Guilford Press (2008).
18. Díaz-Marsá M, Alberdi-Páramo I, Niell-Galmés L. Nutritional supplements in eating disorders. Actas Esp Psiquiatr. (2017) 45(Suppl. 1):26–36.
19. Downing G. Biomarkers definitions working group. biomarkers and surrogate endpoints. Clin Pharmacol Ther. (2001) 69:89–95. doi: 10.1067/mcp.2001.113989
20. Venkatasubramanian G, Keshavan MS. Biomarkers in psychiatry-a critique. Ann Neurol. (2016) 23:3–5. doi: 10.1159/000443549
21. Ahmed S, Memon RI, Venigalla H, Mekala HM, Ramadan O. Biomarkers in psychiatric disorders – a perspective. Ann Clin Case Rep. (2017) 2:1289.
22. Phillips ML, Vieta E. Identifying functional neuroimaging biomarkers of bipolar disorder: toward DSM-V. Schizophr Bull. (2007) 33:893–904. doi: 10.1093/schbul/sbm060
23. Venigalla H, Mekala HM, Hassan M, Ahmed R, Zain H, Dar S, et al. An update on biomarkers in psychiatric disorders- are we aware, do we use in our clinical practice? Ment Health Fam Med. (2017) 13:471–9.
24. Scarr E, Millan MJ, Bahn S, Bertolino A, Turck CW, Kapur S, et al. Biomarkers for psychiatry: the journey from fantasy to fact, a report of the 2013 CINP think tank. Int J Neuropsychopharmacol. (2015) 18:42. doi: 10.1093/ijnp/pyv042
25. Dean B. Dissecting the syndrome of schizophrenia: progress toward clinically useful biomarkers. Schizophr Res Treat. (2011) 2011:614730. doi: 10.1155/2011/614730
27. Bauer IE, Pascoe MC, Wollenhaupt-Aguiar B, Kapczinski F, Soares JC. Inflammatory mediators of cognitive impairment in bipolar disorder. J Psychiatr Res. (2014) 56:18–27. doi: 10.1016/j.jpsychires.2014.04.017
28. Yuan N, Chen Y, Xia Y, Dai J, Liu C. Inflammation-related biomarkers in major psychiatric disorders: a cross-disorder assessment of reproducibility and specificity in 43 meta-analyses. Transl Psychiatry. (2019) 9:233. doi: 10.1038/s41398-019-0570-y
29. Howren MB, Lamkin DM, Suls J. Associations of depression with C-reactive protein, IL-1, and IL-6: a meta-analysis. Psychosom Med. (2009) 71:171–86. doi: 10.1097/PSY.0b013e3181907c1b
30. Haapakoski R, Mathieu J, Ebmeier KP, Alenius H, Kivimäki M. Cumulative meta-analysis of interleukins 6 and 1β, tumour necrosis factorα and C-reactive protein in patients with major depressive disorder. Brain Behav Immun. (2015) 49:206–15. doi: 10.1016/j.bbi.2015.06.001
31. Ripke S, Neale BM, Corvin A, Walters JTR, Farh KH, Holmans PA, et al. Biological insights from 108 schizophrenia-associated genetic loci. Nature. (2014) 511:421–7. doi: 10.1038/nature13595
32. De Witte L, Tomasik J, Schwarz E, Guest PC, Rahmoune H, Kahn RS, et al. Cytokine alterations in first episode schizophrenia patients before and after antipsychotic treatment. Schizophr Res. (2014) 154:23–9. doi: 10.1016/j.schres.2014.02.005
33. Wan C, La Y, Zhu H, Yang Y, Jiang L, Chen Y, et al. Abnormal changes of plasma acute phase proteins in schizophrenia and the relation between schizophrenia and haptoglobin (Hp) gene. Amino Acids. (2007) 32:101–8. doi: 10.1007/s00726-005-0292-8
34. Dalton B, Bartholdy S, Robinson L, Solmi M, Ibrahim MAA, Breen G, et al. A meta-analysis of cytokine concentrations in eating disorders. J Psychiatr Res. (2018) 103:252–64. doi: 10.1016/j.jpsychires.2018.06.002
35. Frye MA, Nassan M, Jenkins G, Kung S, Veldic M, Palmer BA, et al. Feasibility of investigating differential proteomic expression in depression: implications for biomarker development in mood disorders. Transl Psychiatry. (2015) 5:689. doi: 10.1038/tp.2015.185
36. Sun XY, Lu J, Zhang L, Song HT, Zhao L, Fan H, et al. Aberrant microRNA expression in peripheral plasma and mononuclear cells as specific blood-based biomarkers in schizophrenia patients. J Clin Neurosci. (2015) 22:570–4. doi: 10.1016/j.jocn.2014.08.018
37. Ahmed R, Paterson R, Warren J, Zetterberg H, O'Brien J, Fox NC, et al. Biomarkers in dementia: clinical utility and new directions. J Neurol Neurosurg Psychiatry. (2014) 85:1426–34. doi: 10.1136/jnnp-2014-307662
38. Pan JX, Xia JJ, Deng FL, Liang WW, Wu J, Yin BM, et al. Diagnosis of major depressive disorder based on changes in multiple plasma neurotransmitters: a targeted metabolomics study. Transl Psychiatry. (2018) 8:130. doi: 10.1038/s41398-018-0183-x
39. Kuipers SD, Bramham CR. Brain-derived neurotrophic factor mechanisms and function in adult synaptic plasticity: new insights and implications for therapy. Curr Opin Drug Discov Devel. (2006) 9:580–6.
40. Lozupone M, La Montagna M, D'Urso F, Daniele A, Greco A, DavideSeripa D, et al. The role of biomarkers in psychiatry. In: Guest PC, editor Advances in Experimental Medicine and Biology. Switzerland: Springer Nature (2019).
41. Alonso JF, Romero S, Ballester MR, Antonijoan RM, Mañanas MA. Stress assessment based on EEG univariate features and functional connectivity measures. Physiol Meas. (2015) 36:1351–65. doi: 10.1088/0967-3334/36/7/1351
42. Yamasaki T, Tobimatsu S. Electrophysiological biomarkers for improved etiological diagnosis of cognitive impairment. Curr Biomarker Findings. (2014) 4:69–79. doi: 10.2147/CBF.S46067
43. Patel SH, Azzam PN. Characterization of N200 and P300: selected studies of the event-related potential. Int J Med Sci. (2005) 2:147–54. doi: 10.7150/ijms.2.147
44. Olichney JM, Hillert DG. Clinical applications of cognitive event-related potentials in Alzheimer's disease. Phys Med Rehabil Clin N Am. (2004) 15:205–33. doi: 10.1016/S1047-9651(03)00103-7
45. Venigalla H, Mekala HM, Hassan M, Ahmed R, Zain H, Dar SS, et al. An update on biomarkers in psychiatric disorders- are we aware, do we use in our clinical practice? Mental Health Fam Med. (2017) 13:471–9.
46. Cenit MC, Sanz Y, Codoñer-Franch P. Influence of gut microbiota on neuropsychiatric disorders. World J Gastroenterol. (2017) 23:5486–98. doi: 10.3748/wjg.v23.i30.5486
47. Butler MI, Mörkl S, Sandhu KV, Cryan JF, Dinan TG. The gut microbiome and mental health: what should we tell our patients?: Le microbiote Intestinal et la Santé Mentale: que Devrions-Nous dire à nos Patients? Can J Psychiatry. (2019) 64:747–60. doi: 10.1177/0706743719874168
48. Rea K, Dinan TG, Cryan JF. The microbiome: A key regulator of stress and neuroinflammation. Neurobiol Stress. (2016) 4:23–33. doi: 10.1016/j.ynstr.2016.03.001
49. Kelly JR, Borre Y, O'Brien C, Patterson E, El Aidy S, Deane J, et al. Transferring the blues: depression-associated gut microbiota induces neuro behavioural changes in the rat. J Psychiatr Res. (2016) 82:109–18. doi: 10.1016/j.jpsychires.2016.07.019
50. Kiecolt-Glaser JK, Derry HM, Fagundes CP. Inflammation: depression fans the flames and feasts on the heat. Am J Psychiatry. (2015) 172:1075–91. doi: 10.1176/appi.ajp.2015.15020152
51. Madison A, Kiecolt-Glaser JK. Stress, depression, diet, and the gut microbiota: human–bacteria interactions at the core of psychoneuroimmunology and nutrition. Curr Opin Behav Sci. (2019) 28:105–10. doi: 10.1016/j.cobeha.2019.01.011
52. Maes M, Kubera M, Leunis J-C, Berk M. Increased IgA and IgM responses against gut commensals in chronic depression: further evidence for increased bacterial translocation or leaky gut. J Affect Disord. (2012) 141:55–62. doi: 10.1016/j.jad.2012.02.023
53. Dinan TG, Stanton C, Long-Smith C, Kennedy P, Cryan JF, Cowan CSM, et al. Feeding melancholic microbes: my new gut recommendations on diet and mood. Clin Nutr. (2019) 38:1995–2001. doi: 10.1016/j.clnu.2018.11.010
54. Fresan U, Bes-Rastrollo M, Segovia-Siapco G, Sanchez-Villegas A, Lahortiga F, de la Rosa PA, et al. Does the mind diet decrease depression risk? A comparison with Mediterranean diet in the SUN cohort. Eur J Nutr. (2019) 58:1271–82. doi: 10.1007/s00394-018-1653-x
55. Emerson SD, Carbert NS. An apple a day: protective associations between nutrition and the mental health of immigrants in Canada. Soc Psychiatry Psychiatr Epidemiol. (2019) 54:567–78. doi: 10.1007/s00127-018-1616-9
56. Mujcic R, Oswald J. Evolution of well-being and happiness after increases in consumption of fruit and vegetables. Am J Publ Health. (2016) 106:1504–10. doi: 10.2105/AJPH.2016.303260
57. McNanara D. First Evidence Dietary Flavonols Linked to Lower Alzheimer Risk. Medscape. (2020). Available online at: https://www.medscape.com/viewarticle/924543 (accessed May 6, 2020).
58. Amao I. Health Benefits of Fruits and Vegetables: Review From Sub-Saharan Africa, Vegetables - Importance of Quality Vegetables to Human Health, Md. London: IntechOpen (2018). doi: 10.5772/intechopen.74472
59. Bear TLK, Dalziel JE, Coad J, Roy NC, Butts CA, Gopal PK. The Role of the gut microbiota in dietary interventions for depression and anxiety. Adv Nutr. (2020) 11:890–907. doi: 10.1093/advances/nmaa016
60. Jacka FN, Maes M, Pasco JA, Williams LJ, Berk M. Nutrient intakes and the common mental disorders in women. J Affect Disord. (2012) 141:79–85. doi: 10.1016/j.jad.2012.02.018
61. Wang J, Um P, Dickerman BA, Liu J. Zinc, magnesium, selenium and depression: a review of the evidence, potential mechanisms and implications. Nutrients. (2018) 10:584. doi: 10.3390/nu10050584
62. Rybka J, Kedziora-Kornatowska K, Banas-Lezanska P, Majsterek I, Carvalho LA, Cattaneo A, et al. Interplay between the pro-oxidant and antioxidant systems and proinflammatory cytokine levels, in relation to iron metabolism and the erythron in depression. Free Radic Biol Med. (2013) 63:187–94. doi: 10.1016/j.freeradbiomed.2013.05.019
63. Zhang M, Robitaille L, Eintracht S, Hoffer LJ. Vitamin C provision improves mood in acutely hospitalized patients. Nutrition. (2011) 27:530–3. doi: 10.1016/j.nut.2010.05.016
64. Bouayed J. Polyphenols: a potential new strategy for the prevention and treatment of anxiety and depression. Curr Nutr Food Sci. (2010) 6:13–8. doi: 10.2174/157340110790909608
65. Souza LC, de Gomes MG, Goes AT, Del Fabbro L, Filho CB, Boeira SP, et al. Evidence for the involvement of the serotonergic 5-HT(1A) receptors in the antidepressant-like effect caused by hesperidin in mice. Prog Neuropsychopharmacol Biol Psychiatry. (2013) 40:103–9. doi: 10.1016/j.pnpbp.2012.09.003
66. Filho CB, Del Fabbro L, de Gomes MG, Goes AT, Souza LC, Boeira SP, et al. Kappa-opioid receptors mediate the antidepressant- like activity of hesperidin in the mouse forced swimming test. Eur J Pharmacol. (2013) 698:286–91. doi: 10.1016/j.ejphar.2012.11.003
67. Parhiz H, Roohbakhsh A, Soltani F, Rezaee R, Iranshahi M. Antioxidant and anti-inflammatory properties of the citrus flavonoids hesperidin and hesperetin: an updated review of their molecular mechanisms and experimental models. Phytother Res. (2015) 29:323–31. doi: 10.1002/ptr.5256
68. Davenport L. Cocoa Flavanols may Reverse Age-Related Memory Decline. Medscape. (2014). Available online at: https://www.medscape.com/viewarticle/833972 (accessed May 6, 2020).
69. Owen L, Corfe BM. The role of diet and nutrition on mental health and wellbeing. P Nutr Soc. (2017) 76:425–6. doi: 10.1017/S0029665117001057
70. Lachance L, Ramsey D. Food, mood, and brain health: implications for the modern clinician. Mo Med. (2015) 112:111–5.
71. Schmidt K, Cowen PJ, Harmer CJ, Tzortzis G, Errington S, Burnet PW. Prebiotic intake reduces the waking cortisol response and alters emotional bias in healthy volunteers. Psychopharmacology. (2015) 232:1793–801. doi: 10.1007/s00213-014-3810-0
72. Tamang JP, Shin DH, Jung SJ, Chae SW. Functional properties of microorganisms in fermented foods. Front Microbiol. (2016) 7:578. doi: 10.3389/fmicb.2016.00578
73. Franz CM, Huch M, Mathara JM, Abriouel H, Benomar N, Reid G, et al. African fermented foods and probiotics. Int J Food Microbiol. (2014) 190:84–96. doi: 10.1016/j.ijfoodmicro.2014.08.033
74. Mischoulon D, Freeman MP. Omega-3 fatty acids in psychiatry. Psychiatr Clin North Am. (2013) 36:15–23. doi: 10.1016/j.psc.2012.12.002
75. Bloch MH, Qawasmi A. Omega-3 fatty acid supplementation for the treatment of children with attention-deficit/hyperactivity disorder symptomatology: systematic review and meta-analysis. J Am Acad Child Adolesc. (2011) 50:991–1000. doi: 10.1016/j.jaac.2011.06.008
76. Simopoulos A. Evolutionary aspects of diet: the Omega-6/Omega-3 ratio and the brain. Mol Neurobiol. (2011) 44:203–15. doi: 10.1007/s12035-010-8162-0
77. Kim H, McGrath BM, Silverstone PH. A review of the possible relevance of inositol and the phosphatidylinositol second messenger system (PI-cycle) to psychiatric disorders—focus on magnetic resonance spectroscopy (MRS) studies. Hum Psychopharmacol. (2005) 20:309–26. doi: 10.1002/hup.693
78. Carey PD, Warwick J, Harvey BH, Stein DJ, Seedat S. Single photon emission computed tomography (SPECT) in obsessive–compulsive disorder before and after treatment with inositol. Metab Brain Dis. (2004) 19:125–34. doi: 10.1023/B:MEBR.0000027423.34733.12
79. Harvey BH, Brink CB, Seedat S, Stein DJ. Defining the neuromolecular action of myo-inositol: application to obsessive-compulsive disorder. Prog NeuroPsychopharmacol Biol Psychiatry. (2002) 26:21–32. doi: 10.1016/S0278-5846(01)00244-5
80. Karci CK, Celik GG. Nutritional and herbal supplements in the treatment of obsessive compulsive disorder. Gene Psychiatry. (2020) 33:e100159. doi: 10.1136/gpsych-2019-100159
81. Mazzio E, Harris N, Soliman K. Food constituents attenuate monoamine oxidase activity and peroxide levels in C6 astrocyte cells. Planta Med. (1998) 64:603–6. doi: 10.1055/s-2006-957530
82. Sayyah M, Boostani H, Pakseresht S, Malayeri A. Comparison of Silybum marianum (L.) Gaertn. with fluoxetine in the treatment of obsessive-compulsive disorder. Prog Neuropsychopharmacol Biol Psychiatry. (2010) 34:362–5. doi: 10.1016/j.pnpbp.2009.12.016
83. Khom S, Baburin I, Timin E, Hohaus A, Trauner G, Kopp B, et al. Valerenic acid potentiates and inhibits GABAA receptors: molecular mechanism and subunit specificity. Neuropharmacology. (2007) 53:178–87. doi: 10.1016/j.neuropharm.2007.04.018
84. Andreatini R, Sartori VA, Seabra MLV, Leite JR. Effect of valepotriates (valerian extract) in generalized anxiety disorder: a randomized placebo-controlled pilot study. Phytother Res. (2002) 16:650–4. doi: 10.1002/ptr.1027
85. Sarris J, Kavanagh DJ, Kava KDJ. Kava and St. John's wort: current evidence for use in mood and anxiety disorders. J Altern Complement Med. (2009) 15:827–36. doi: 10.1089/acm.2009.0066
86. Rahimi R, Nikfar S, Abdollahi M. Efficacy and tolerability of Hypericum perforatum in major depressive disorder in comparison with selective serotonin reuptake inhibitors: a meta-analysis. Prog Neuropsychopharmacol Biol Psychiatry. (2009) 33:118–27. doi: 10.1016/j.pnpbp.2008.10.018
87. Cui X, Pertile R, Liu P, Eyles DW. Vitamin D regulates tyrosine hydroxylase expression: N-cadherin a possible mediator. Neuroscience. (2015) 304:90–100. doi: 10.1016/j.neuroscience.2015.07.048
88. Kaneko I, Sabir MS, Dussik CM, Whitfield GK, Karrys A, Hsieh J, et al. 1,25-Dihydroxyvitamin D regulates expression of the tryptophan hydroxylase 2 and leptin genes: implication for behavioral influences of vitamin D. Faseb J. (2015) 29:4023–35. doi: 10.1096/fj.14-269811
89. Tangney CC, Aggarwal NT, Li H, Wilson RS, Decarli C, Evans DA, et al. Vitamin B12, cognition, and brain MRI measures: a cross-sectional examination. Neurology. (2011) 77:1276–82. doi: 10.1212/WNL.0b013e3182315a33
90. Hegyi J, Schwartz RA, Hegyi V. Pellagra: dermatitis, dementia, and diarrhea. Int J Dermatol. (2004) 43:1–5. doi: 10.1111/j.1365-4632.2004.01959.x
91. Enderami A, Zarghami M, Darvishi-Khezri H. The effects and potential mechanisms of folic acid on cognitive function: a comprehensive review. Neurol Sci. (2018) 39:1667–75. doi: 10.1007/s10072-018-3473-4
92. Black MM. Effects of vitamin B12 and folate deficiency on brain development in children. Food Nutr Bull. (2008) 29:S126–31. doi: 10.1177/15648265080292S117
93. Gomez-Pinilla F, Nguyen TTJ. Natural mood foods: The actions of polyphenols against psychiatric and cognitive disorders. Nutr Neurosci. (2012) 15:127–33. doi: 10.1179/1476830511Y.0000000035
94. Kulkarni S, Dhir A, Akula KK. Potentials of curcumin as an antidepressant. Sci World J. (2009) 9:1233–41. doi: 10.1100/tsw.2009.137
95. Kim J, Wie M, MeejungAhn M, Akane TA, Hiroshi MH, Taekyun ST. Benefits of hesperidin in central nervous system disorders: a review. Anat Cell Biol. (2019) 52:369–77. doi: 10.5115/acb.19.119
96. Cirmi S, Ferlazzo N, Lombardo GE, Ventura-Spagnolo E, Gangemi S, Calapai G, et al. Neurodegenerative diseases: might citrus flavonoids play a protective role? Molecules. (2016) 21:E1312. doi: 10.3390/molecules21101312
97. Hwang SL, Shih PH, Yen GC. Neuroprotective effects of citrus flavonoids. J Agric Food Chem. (2012) 60:877–85. doi: 10.1021/jf204452y
98. Justin-Thenmozhi A, DhivyaBharathi M, Kiruthika R, Manivasagam T, Borah A, Essa MM. Attenuation of aluminum chloride-induced neuroinflammation and caspase activation through the AKT/GSK-3β pathway by hesperidin in Wistar rats. Neurotox Res. (2018) 34:463–76. doi: 10.1007/s12640-018-9904-4
99. Donato F, de Gomes MG, Goes AT, Filho CB, Del Fabbro L, Antunes MS, et al. Hesperidin exerts antidepressant-like effects in acute and chronic treatments in mice: possible role of l-arginine-NO-cGMP pathway and BDNF levels. Brain Res Bull. (2014) 104:19–26. doi: 10.1016/j.brainresbull.2014.03.004
100. Raza SS, Khan MM, Ahmad A, Ashafaq M, Khuwaja G, Tabassum R, et al. Hesperidin ameliorates functional and histological outcome and reduces neuroinflammation in experimental stroke. Brain Res. (2011) 1420:93–105. doi: 10.1016/j.brainres.2011.08.047
101. Said UZ, Saada HN, Abd-Alla MS, Elsayed ME, Amin AM. Hesperidin attenuates brain biochemical changes of irradiated rats. Int J Radiat Biol. (2012) 88:613–8. doi: 10.3109/09553002.2012.694008
102. Rotimi SO, Bankole GE, Adelani IB, Rotimi OA. Hesperidin prevents lipopolysaccharide-induced endotoxicity in rats. Immunopharmacol Immunotoxicol. (2016) 38:364–71. doi: 10.1080/08923973.2016.1214142
103. Lassale C, Batty GD, Baghdadli A, Jacka F, Sánchez-Villegas A, Kivimäki M, et al. Healthy dietary indices and risk of depression outcomes; a systematic review and meta-analysis of observational studies. Mol Psychiatry. (2018) 24:965–86. doi: 10.1038/s41380-018-0299-7
104. Bocchio-Chiavetto L, Bagnardi V, Zanardini R, Molteni R, Nielsen MG, Placentino A, et al. Serum and plasma BDNF levels in major depression: a replication study and meta-analyses. World J Biol Psychiatry. (2010) 11:763–73. doi: 10.3109/15622971003611319
105. O'Mahony SM, Clarke G, Borre YE, Dinan TG, Cryan JF. Serotonin, tryptophan metabolism and the brain-gut-microbiome axis. Behav Brain Res. (2015) 277:32–48. doi: 10.1016/j.bbr.2014.07.027
106. Allen AP, Hutch W, Borre YE, Kennedy PJ, Temko A, Boylan G, et al. Bifidobacterium longum 1714 as a translational psychobiotic: modulation of stress, electrophysiology and neurocognition in healthy volunteers. Transl Psychiatry. (2016) 6:e939. doi: 10.1038/tp.2016.191
107. Takada M, Nishida K, Kataoka-Kato A, Gondo Y, Ishikawa H, Suda K, et al. Probiotic Lactobacillus casei strain shirota relieves stress-associated symptoms by modulating the gut-brain interaction in human and animal models. Neurogastroenterol Motil. (2016) 28:1027–36. doi: 10.1111/nmo.12804
108. Ng QX, Peters C, Ho CYX, Lim DY, Yeo WS. A meta-analysis of the use of probiotics to alleviate depressive symptoms. J Affect Disor. (2018) 228:13–9. doi: 10.1016/j.jad.2017.11.063
109. McKean J, Naug H, Nikbakht E, Amiet B, Colson N. Probiotics and subclinical psychological symptoms in healthy participants: a systematic review and meta-analysis. J Altern Complement Med. (2017) 23:249–58. doi: 10.1089/acm.2016.0023
110. Diaz M, Kellingray L, Akinyemi N, Adefiranye OO, Olaonipekun AB, Bayili GR, et al. Comparison of the microbial composition of African fermented foods using amplicon sequencing. Sci Rep. (2019) 9:13863. doi: 10.1038/s41598-019-50190-4
111. Olasupo N, Odunfa S, Obayori O. Ethnic African Fermented Foods in: Fermented Foods and Beverages of the World. Boca Raton, FL: CRC press (2010). doi: 10.1201/EBK1420094954-c12
112. Mitsou EK, Kakali A, Antonopoulou S, Mountzouris KC, Yannakoulia M, Panagiotakos DB, et al. Adherence to the mediterranean diet is associated with the gut microbiota pattern and gastrointestinal characteristics in an adult population. Br J Nutr. (2017) 117:1645–55. doi: 10.1017/S0007114517001593
113. Zinöcker MK, Lindseth IA. The Western diet-microbiome-host interaction and its role in metabolic disease. Nutrients. (2018) 10:E365. doi: 10.3390/nu10030365
114. Gow NAR, Yadav B. Microbe profile: Candida albicans: a shape changing, opportunistic pathogenic fungus of humans. Microbiology. (2017) 163:1145–7. doi: 10.1099/mic.0.000499
115. Gutierrez-Diaz I, Fernandez-Navarro T, Salazar N, Bartolome B, Moreno-Arribas MV, de Andres-Galiana EJ, et al. Adherence to a mediterranean diet influences the fecal metabolic profile of microbial derived phenolics in a Spanish cohort of middle-age and older people. J Agric Food Chem. (2017) 65:586–95. doi: 10.1021/acs.jafc.6b04408
116. David LA, Maurice CF, Carmody RN, Gootenberg DB, Button JE, Wolfe BE, et al. Diet rapidly and reproducibly alters the human gut microbiome. Nature. (2013) 505:559–63. doi: 10.1038/nature12820
117. Kim M-S, Hwang S-S, Park E-J, Bae J-W. Strict vegetarian diet improves the risk factors associated with metabolic diseases by modulating gut microbiota and reducing intestinal inflammation. Environ Microbiol Rep. (2013) 5:765–75. doi: 10.1111/1758-2229.12079
118. Aucoin M, LaChance L, Cooley K, Kidd S. Diet and psychosis: a scoping review. Neuropsychobiology. (2020) 79:20–42. doi: 10.1159/000493399
119. Palmer CM. Ketogenic diet in the treatment of schizoaffective disorder: two case studies. Schizophr Res. (2017) 189:208–9. doi: 10.1016/j.schres.2017.01.053
120. Brauser D. Diet and Mental Health: The Evidence to Date. Medscape. (2020). Available online at: https://www.medscape.com/viewarticle/923817 (accessed May 6, 2020).
121. Melville NA. Culinary Culprits: Foods that May Harm the Brain. Medscape. (2014). Available online at: https://www.medscape.com/viewarticle/819974#vp_1 (accessed May 6, 2020).
122. Del-Ponte B, Quinte GC, Cruz S, Grellert M, Santos IS. Dietary patterns and attention deficit/hyperactivity disorder (ADHD): a systematic review and meta-analysis. J Affect Disord. (2019) 252:160–73. doi: 10.1016/j.jad.2019.04.061
123. Hill P, Taylor E. An auditable protocol for treating attention deficit/ hyperactivity disorder. Arch Dis Childhood. (2001) 84:404–9. doi: 10.1136/adc.84.5.404
124. Pelsser L, Frankena K, Toorman J, Rodrigues PR. Retrospective outcome monitoring of ADHD and nutrition (ROMAN): the effectiveness of the few-foods diet in general practice. Front Psychiatry. (2020) 11:96. doi: 10.3389/fpsyt.2020.00096
125. Borghi L, Salvatici E, Riva E, Giovannini M, Vegni EA. Psychological and psychosocial implications for parenting a child with phenylketonuria: a systematic review. Minerva Pediatr. (2019) 71:181–95. doi: 10.23736/S0026-4946.17.04950-7
126. Giannunzio V, Degortes D, Tenconi E, Collantoni E, Solmi M, Santonastaso P, et al. Decision-making impairment in anorexia nervosa: new insights into the role of age and decision-making style. Eur Eat Disord Rev. (2018) 26:302–14. doi: 10.1002/erv.2595
127. Gaudio S, Wiemerslage L, Brooks SJ, Schioth HB. A systematic review of resting-state functional-MRI studies in anorexia nervosa: evidence for functional connectivity impairment in cognitive control and visuospatial and body-signal integration. Neurosci Biobehav Rev. (2016) 71:578–89. doi: 10.1016/j.neubiorev.2016.09.032
128. Cannell JJ, Grant WB. What is the role of vitamin D in autism? Dermatoendocrinol. (2013) 5:199–204. doi: 10.4161/derm.24356
129. Eyles DW, Burne THJ, McGrath JJ. Vitamin D Effects on brain development, adult brain function and the links between low levels of vitamin D and neuropsychiatric disease. Front Neuroendocrinol. (2013) 34:47–64. doi: 10.1016/j.yfrne.2012.07.001
130. Chiang M, Natarajan R, Fan X. Vitamin D in schizophrenia: a clinical review. Evid Based Ment Health. (2016) 19:6–9. doi: 10.1136/eb-2015-102117
131. Wang T, Shan L, Du L, Feng J, Xu Z, Staal WG, et al. Serum concentration of 25-hydroxyvitamin D in autism spectrum disorder: a systematic review and meta-analysis. Eur Child Adolesc Psychiatry. (2016) 25:341–50. doi: 10.1007/s00787-015-0786-1
132. Brouwer-Brolsma EM, Dhonukshe-Rutten RA, van Wijngaarden NL, van de Zwaluw JP, Wins S, Swart KMA, et al. Cognitive performance: a cross-sectional study on serum vitamin D and its interplay with glucose homeostasis in Dutch older adults. J Am Med Dir Assoc. (2015) 16:621–7. doi: 10.1016/j.jamda.2015.02.013
133. Todisco P, Meneguzzo P, Vogazianos P, Garolla A, Antoniades A, Tozzi F. Relation between vitamin D and impulse behaviours in patients with eating disorder: a pilot observational study. Eur Eat Disord Rev. (2020) 28:587–93. doi: 10.1002/erv.2740
134. McGrattan AM, McGuinness B, McKinley MC, Kee F, Passmore P, Woodside JV, et al. Diet and inflammation in cognitive ageing and Alzheimer's disease. Curr Nutr Rep. (2019) 8:53–65. doi: 10.1007/s13668-019-0271-4
135. Firth J, Stubbs B, Teasdale SB, Ward PB, Veronese N, Shivappa N, et al. Diet as a hot topic in psychiatry: a population-scale study of nutritional intake and inflammatory potential in severe mental illness. World Psychiatry. (2018) 17:365–7. doi: 10.1002/wps.20571
136. Rapaport MH, Nierenberg AA, Schettler PJ, Kinkead B, Cardoos A, Walker R, et al. Inflammation as a predictive biomarker for response to omega-3 fatty acids in major depressive disorder: a proof-of-concept study. Mol Psychiatry. (2016) 21:71–9. doi: 10.1038/mp.2015.22
137. Pusceddu MM, Kelly P, Ariffin N, Cryan JF, Clarke G, Dinann TG. n-3 PUFAs have beneficial effects on anxiety and cognition in female rats: effects of early life stress. Psychoneuroendocrinology. (2015) 58:79–90. doi: 10.1016/j.psyneuen.2015.04.015
138. Fux M, Levine J, Aviv A, Belmaker RH. Inositol treatment of obsessive-compulsive disorder. Am J Psychiatry. (1996) 153:1219–21. doi: 10.1176/ajp.153.9.1219
139. Wollen KA. Alzheimer's disease: the pros and cons of pharmaceutical, nutritional, botanical, stimulatory therapies, with a discussion of treatment strategies from the perspective of patients and practitioners. Altern Med Rev. (2010) 15:223–44.
Keywords: psychiatry, mental disorder, microbiome, biomarker, probiotics, nutrition, food
Citation: Offor SJ, Orish CN, Frazzoli C and Orisakwe OE (2021) Augmenting Clinical Interventions in Psychiatric Disorders: Systematic Review and Update on Nutrition. Front. Psychiatry 12:565583. doi: 10.3389/fpsyt.2021.565583
Received: 07 July 2020; Accepted: 07 April 2021;
Published: 05 May 2021.
Edited by:
Shaohua Hu, Zhejiang University, ChinaCopyright © 2021 Offor, Orish, Frazzoli and Orisakwe. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Orish E. Orisakwe, orishebere@gmail.com
 Samuel J. Offor
Samuel J. Offor Chinna N. Orish2
Chinna N. Orish2 Chiara Frazzoli
Chiara Frazzoli Orish E. Orisakwe
Orish E. Orisakwe