Abstract
Objectives
A diagnosis of congenital heart disease (CHD) during fetal life or infancy can be devastating for parents, resulting in significant psychological stressors. The goals of this study were to (1) assess maternal resolution and adaptation to a new diagnosis of CHD, (2) explore how maternal resolution and adaptation relates to psychological well-being and (3) evaluate whether specific illness parameters impact resolution status.
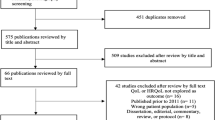
Methods
This cross-sectional study evaluated resolution to diagnosis in the first 6 months of life for mothers of children with CHD. Mothers completed a Reaction to Diagnosis Interview (RDI) and psychological surveys assessing stress, depression, and coping skills. The RDI invites parents to discuss the diagnosis, changes in their thoughts and feelings since the diagnosis, and reflections on why they think they have a child with a medical condition. A chart review of the child recording illness parameters was also performed.
Results
Thirty-six mothers participated in this study. Twelve of their children had a prenatal diagnosis of CHD (33.3%). Seventeen mothers (47.2%) were unresolved to the diagnosis of CHD in their child, regardless of the timing or severity of the diagnosis. Twenty-four participants (68.6%) had significant or highly significant life stress and 9 participants (25.7%) had clinical concerns or met criteria for Post-Traumatic Stress Disorder. Nineteen mothers (55.9%) were at risk for clinical depression. Mothers unresolved to the diagnosis had higher rates of post-traumatic stress than those resolved to the diagnosis (47.1% vs. 10.5%, p = 0.03). Mothers of infants with a prenatal diagnosis of CHD reported significantly lower rates of life stress despite higher severity of heart defects (p = 0.02).
Conclusions for Practice
Mothers of infants with CHD have similar proportions of resolution to diagnosis compared to mothers of children with other chronic diseases. They experience a high rate of symptoms of life stress, post-traumatic stress and clinical depression. Symptoms of post-traumatic stress are higher in mothers unresolved to the diagnosis. Identification of those at highest risk for poor adaptation to the diagnosis may allow for targeted psychological support services for those most vulnerable.
Significance Statement
A diagnosis of congenital heart disease can result in significant parental stress and negatively impact parental and child bonding. Our study demonstrates that parents of infants with cardiac disease experience high rates of life stress, post-traumatic stress and clinical depression. Mothers unresolved to the diagnosis have higher rates of post-traumatic stress. Those who received a prenatal diagnosis had lower life stress despite greater disease severity. Identification of mothers at highest risk for poor adaptation to the diagnosis may allow for targeted psychological support services for those most vulnerable.


Similar content being viewed by others
Data Availability
Deidentified participant data can be provided by request if in compliance with CT Children’s Institutional Review Board. The complete study protocol and analytical design is available upon request to the editors and reviewers for the purpose of assessing the manuscript.
References
Arafa, M. A., Zaher, S. R., El-Dowaty, A. A., & Moneeb, D. E. (2008). Quality of life among parents of children with heart disease. Health Quality of Life Outcomes. https://doi.org/10.1186/1477-7525-6-91
Brosig, C. L., Whitstone, B. N., Frommelt, M. A., Frisbee, S. J., & Leuthner, S. R. (2007). Psychological distress in parents of children with severe congenital heart disease: the impact of prenatal versus postnatal diagnosis. Journal of Perinatology, 27(11), 687–692. DOI:https://doi.org/10.1038/sj.jp.7211807.
Carver, C. S. (1997). You want to measure coping but your protocol’s too long: consider the brief COPE. International Journal of Behavioral Medicine, 4(1), 92–100. DOI: https://doi.org/10.1207/s15327558ijbm0401_6.
Chenni, N., Lacroze, V., Pouet, C., Fraisse, A., Kreitmann, B., et al. (2012). Fetal heart disease and interruption of pregnancy: Factors influencing the parental decision-making process. Prenatal Diagnosis, 32(2), 168–172. https://doi.org/10.1002/pd.2923
Christianson, S., & Marren, J. (2012). The impact of event scale – revised (IES-R). Medsurg Nursing: Official Journal of the Academy of Medical-Surgical Nurses, 21(5), 321–322.
Davis, C. C., Brown, R. T., Bakeman, R., & Campbell, R. (1998). Psychological adaptation and adjustment of mothers of children with congenital heart disease: stress, coping, and family functioning. Journal of Pediatric Psychology, 23(4), 219–228. DOI:https://doi.org/10.1093/jpepsy/23.4.219.
Derogatis, L. R., & Melisaratos, N. (1983). The brief Symptom Inventory: an introductory report. Psychological Medicine, 13(3), 595–605.
Hoehn, K. S., Wernovsky, G., Rychik, J., Zhi-yun, T., Donaghue, D., et al. (2004). Parental decision-making in congenital heart disease. Cardiology in the Young, 14(3), 309–314. DOI:https://doi.org/10.1017/S1047951104003099.
Holmes, T. (2021). “Life Stress Questionnaire.” Retrieved June 10 from https://corehealthmuskoka.com/wp-content/uploads/2017/04/10_Life-stress-questionnaire.pdf
Larsen, S. H., Pedersen, J., Jacobsen, J., Johnson, S. P., Hansen, O. K., et al. (2005). The RACHS-1 risk categories reflect mortality and length of stay in a danish population of children operated for congenital heart disease. European Journal of Cardiothoracic Surgery, 28(6), 877–881. DOI: https://doi.org/10.1016/j.ejcts.2005.09.008.
Lewinsohn, P. M., Seeley, J. R., Roberts, R. E., & Allen, N. B. (1997). Center for Epidemiological Studies-Depression Scale (CES-D) as a screening instrument for depression among community-residing older adults. Psychology and Aging, 12(2), 277–287. DOI: https://doi.org/10.1037//0882-7974.12.2.277.
Marvin, R. S., & Pianta, R. C. (1996). Mother’s reactions to their child’s diagnosis: relations with security of attachment. Journal of Clinical Child Psychology, 25, 436–445.
Milshtein, S., Yirmiya, N., Oppenheim, D., Koren-Karie, N., & Levi, S. (2010). Resolution of the diagnosis among parents of children with autism spectrum disorder: Associations with child and parent characteristics. Journal of Autism and Developmental Disorders, 40, 89–99. DOI: https://doi.org/10.1007/s10803-011-1315-9.
Pianta, R. C., & Marvin, R. S. (1993). Manual for classification of reaction to diagnosis interview (Unpublished manual) University of Virginia, USA.
Popp, J. M., Robinson, J. L., Britner, P. A., & Blank, T. O. (2014). Parent adaptation and family functioning in relation to narratives of children with chronic illness. Journal of Pediatric Nursing, 29(1), 58–64. DOI:https://doi.org/10.1016/j.pedn.2013.07.004.
Radloff, L. S. (1977). The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement, 1(3), 385–401.
Rychik, J., Donaghue, D. D., Levy, S., Fajardo, C., Combs, J., et al. (2013). Maternal psychological stress after prenatal diagnosis of congenital heart disease. Journal of Pediatrics, 162(2), 302–307. DOI:https://doi.org/10.1016/j.jpeds.2012.07.023.
Sheeran, T., Marvin, R. S., & Pianta, R. C. (1997). Mothers’ resolution of their childs diagnosis and self-reported measures of parenting stress, marital relations, and social support. Journal of Pediatric Psychology, 22(2), 197–212.
Sher-Censor, E., Ram-On, T., Rudstein-Sabbag, L., Watemberg, M., & Oppenheim, D. (2020). The reaction to diagnosis questionnaire: A preliminary validation of a new self-report measure to assess parents’ resolution of their child’s diagnosis. Attachment and Human Development, 22, 409–424. https://doi.org/10.1080/14616734.2019.1628081
Sher-Censor, K. E., Dolev, S., Said, M., Baransil, N., & Amara, K. (2017). Coherence of representations regarding the child, resolution of the child’s diagnosis and emotional availability: a study of arab-israeli mothers of children with ASD. Journal of Autism and Developmental Disorders, 17, 3130–3149. DOI: https://doi.org/10.1007/s10803-017-3228-8.
Williams, I. A., Shaw, R., Kleinman, C. S., Gersony, W. M., Prakash, A., et al. (2008). Parental understanding of neonatal congenital heart disease. Pediatric Cardiology, 29(6), 1059–1065. DOI:https://doi.org/10.1007/s00246-008-9254-8.
Yoo, Y. S., Popp, J., & Robinson, J. (2013). Maternal distress influences young children’s family representations through maternal view of child behavior and parent–child interactions. Child Psychiatry and Human Development, 45(1), 52–64. DOI:https://doi.org/10.1007/s10578-013-0377-7.
Funding
Research funded in part by the Connecticut Children’s Department of Research for study design, data collection, data analysis, and manuscript publication. B.D. [178,547 PRNT Reaction-Congenital Heart - https://www.connecticutchildrens.org/research ]
Author information
Authors and Affiliations
Contributions
BD, JP, and CO: contributed to study conception and design. Data collection and analysis were performed by JHL, AM, SG, and RR. The first draft of the manuscript was written by BD, JHL, and JP and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest to report regarding the present study.
Consent to Participate
This study protocol was reviewed and approved by both the Scientific Review Committee and Institutional Review Board at Connecticut Children’s (Study 14-056-CCMC, 45 CFR 46.110 (5) expedited review category). Ongoing monitoring and yearly renewal took place in compliance with the Connecticut Children’s Institutional Review Board. All participants provided informed consent to participate in the study in accordance with the protocol approved by the Connecticut Children’s Institutional Review Board.
Informed Consent
Informed consent form approved by the Connecticut Children’s Institutional Review Board and signed by all participants included the statement “At the conclusion of this study, the researchers may publish their findings. Information will be presented in summary format and you will not be identified in any publications or presentations.”
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Davey, B.T., Lee, J.H., Manchester, A. et al. Maternal Reaction and Psychological Coping After Diagnosis of Congenital Heart Disease. Matern Child Health J 27, 671–679 (2023). https://doi.org/10.1007/s10995-023-03599-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10995-023-03599-3