Abstract
Purpose
Dementia caregiving presents a challenge in life transition wherein the adult child is caring for his or her parents. The study examined the effects of a telephone-administered perspective-taking intervention for adult child caregivers of persons with Alzheimer’s Disease and Dementia to reduce levels of depressive symptoms as well as presence and reaction to behavioral problems and also to enhance social support. The mediation effect of perspective-taking on depressive symptoms was also examined.
Method
A two-arm cluster randomized controlled trial was conducted for 176 participants with 24 clusters for the 12-week Connecting Through Caregiving (CTC) intervention and Basic Skill Training (BSB). The CTC intervention integrated perspective taking with basic skill training. The primary outcome was depressive symptoms. The first secondary outcome was the presence and reaction to behavioral problems in the care-recipients. The second secondary outcome was social support. The trial also examined whether intervention effects were mediated by perspective-taking. Measures were obtained at baseline Week 1 (pre-intervention), Week 12 (post-intervention) and Week 24 (three-month follow up).
Results
Data was collected from 2018 to 2021. Ninety-one participants completed the intervention for CTC and eighty-five completed BSB. In terms of the primary outcome, as compared to the BSB group, the CTC group reported significantly greater reductions in depressive symptoms. For the secondary outcomes, the CTC group also reported reduced perceived presence and reaction to behavioral and memory problems of the care recipient as well as increased social support. Perspective-taking was found to mediate between intervention and reduction of depressive symptoms of the caregiver. No moderation effect on the intervention was found for the presence of COVID-19.
Conclusion
The results provided support for the efficacy of the CTC telephone intervention. Findings have implications for enhancing sustainable care for non-digitalized older adults in the wider society.
Trial Registration
ClinicalTrial.gov NCT03030027
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Challenges and Opportunities of Dementia Caregiving
It has been estimated that the number of people with dementia would increase from 57·4 million cases globally in 2019 to 152·8 million cases in 2050, rising particularly in low-income and middle-income countries. Projected increases in cases could be attributed to population growth contributing most to the increases in sub-Saharan Africa and also population ageing contributing most to the increases in east Asia (GDB Forecasting Group, 2020). Western Pacific Region has the highest number of people with dementia (WHO, 2021; Jia et al., 2020). Improvements in life expectancy have changed the structure of multigenerational families and have resulted in extended periods of social and emotional support exchanges including caregiving over the life span.
Developmental transitions into the adult child caregiver role can present both challenges to intergeneration relationships in caregiving. At the same time, dementia can lead to exclusion disadvantage for the care-recipient. Thus, a balance is needed to meet the emotional demands as well as to maintain a distance for problem-solving, taking into various perspectives of all parties involved (Haapala et al., 2019; Biggs et al., 2019; Silverstein et al., 2012; Biggs & Lowenstein, 2011). Various specific challenges over the sustained supply of intergenerational support were identified over the deteriorating course of Alzheimer’s Disease and Dementia. These include the financial and emotional support as well as sustainable filial piety (Yang et al., 2023). Furthermore, intergeneration independence can be intensified due to urbanization and migration in which adult children are more likely to live separately and independently (Janus & Koslowski, 2020).)
Interventions for Dementia Caregivers
Dementia caregivers often experience disruption of self-care and social engagement (Miron et al., 2019; Tsapanou et al., 2021). On the other hand, positive aspects of dementia caregiving can also lead to personal growth and empathy (Tulloch et al., 2022). Specific interventions for family caregivers can ameliorate depression symptoms and increase quality of life (Livingston et al., 2020). Psychosocial interventions to support AD caregivers include psycho-education, individual/ family counselling, multicomponent programs and those involving the use of new technology (e.g., internet or smartphones) to administer (Cheng et al., 2020). Examples of the mechanisms of change include cognitive restructuring (Gallagher-Thompson et al., 2010, 2020), behavioral activation procedures (Au et al., 2019b), acceptance and commitment interventions (Losada et al., 2015) as well as gain-focused appraisal (Cheng et al., 2022).
Moreover, in terms of the caregivers’ perception, caregivers with a “we-perspective” or relationship-centred approach were found to cope better with the burden of caregiving (Stedje et al., 2023; Dewitte et al., 2021; Au et al., 2019a). Thus, it is important to help caregivers to develop reflective capacity to distance themselves from, but not suppressing negative feelings (Gallagher-Thompson et al., 2020; Au et al., 2019a; Biggs & Lowenstein, 2011). At the same time, social support plays an important role in the care eco-system (Merrilees et al., 2020; Friedman & Kennedy 2021; Rote et al., 2021; Au et al., 2009). Apart from reducing distress, social support can also facilitate caregivers to develop reflective capacity to distance themselves from negative reactions to disruptive behavioral problems (Xu et al., 2021; Giebel et al., 2021; Gaugler et al., 2016). At the same time, social support for the caregivers is important. While emotional support involves the sense of being cared for and instrumental support involves getting help and advice when needed (Rote et al. 2021, Gallagher-Thompson et al., 2020, Au et al., 2009).
Adopting a Perspective-taking Approach
Caregiving is a dyadic process. The responses of both the caregiver and the care recipient can impact on the well-being of one another (Miller et al., 2019; Lyons et al., 2002). There is also a need for adult child caregiver to understand that the disruptive behaviors exhibited by the parents were not due to personal animosity (Gaugler et al., 2016). Thus, sustainable caregiving requires empathetic understanding to both the care-recipients.
Perspective-taking reappraisal has been reported to be one of the most effective emotional regulation strategies (Rippon et al., 2020; Matthews et al., 2021). Intergeneration ambivalence, characterized by conflicing emotions, can be intensified with increasing parental dependence on adult children (Chan et al., 2021). Perspective-taking involves asking the participant to actively take a more objective or different stance to re-evaluate the emotional trigger. While distraction may offer some relief from a distressing situation, it does not permit deeper processing which would require reappraisal, continued monitoring and active engagement with emotional events. With caregiving, reappraisals will need to take into account not only the self but also the care recipient. Caregivers who attained an understanding that they themselves in future would also be a recipient of care would expereince less buden (Bei et al., 2023). Thus, a “we-perspective” is an important element in dementia caregiving (Ebert et al., 2020; Ferraris et al., 2022; Silverstein et al., 2012). Finally, a recent trend is the effective use of technological aids (e.g., the telephone or internet) to deliver psychosocial support, reaching more caregivers in order to minimize disruption to the caregiver’s routine and to overcome access issues in some communities (Au et al., 2019b; Cheng et al., 2019). The present study attempted to address some major gaps on dementia caregiving areas: 1) specific interventions for intergenerational caregiving, 2) perspective-taking mechanisms contributing to better mental health in caregiving and 3) the use of low-cost technology to enhance accessibility and sustainability of care.
In particular, the intervention targeted at balancing self-care and caring for others by developing perspective-taking reappraisals involving self-awareness and empathy for others. The study used prospective design to test the intervention effects Connecting Through Caregiving (CTC) intervention involving 1) appreciating relational insights; 2) enhancing self-awareness; 3) empathetic understanding of care-recipient; 4) integrating self-care and caring for others and 5) negotiation. Telephone sessions were to maximize accessibility and sustainability of interventions. The CTC program was evaluated against a Basic Skill Building (BSB) as active control in a two-arm randomized controlled trial. Both intervention and control had 12 weeks of telephone intervention and a three-month follow-up. Measures were obtained at baseline Week 1 (T0: pre-intervention), Week 12 (T1: post-intervention) with a follow-up (T2) at Week 24. The primary outcome was the reduction of depressive symptoms. For the secondary outcomes, we tested whether, as compared to those in BSB, CTC participants would perceive a greater social support from family and friends as well as a decrease in caregivers’ perceived intensity of behavioral problems and related distress caused by behavioral problems. We also examined the possible mediation effects of perspective taking strategies on intervention with regard to the primary outcome (i.e. depressive symptoms of the caregivers. Finally, as part of the study was conducted during Coronavirus disease (COVID-19), we tested for moderation effect of COVID-19 on intervention effects.
Methods
Procedures and Participants
The caregivers were recruited from social services centers in urban areas in Hong Kong. The selection criteria were as follows. First, the study participants involved primary adult child caregivers aged 20 or above, who had been caring for persons (aged 60 or above) with a medical diagnosis of Alzheimer’s disease in the mild to moderate range as determined by the Clinical Dementia Rating Scale. They could be daughter/son or daughter-/son-in-law of the care recipient. Second, these caregivers were known to these agencies as their care recipients were attending one to two weekly sessions in the community centers. Third, these caregivers had been providing unpaid care for a minimum of 12 hours a week for at least the past three months. This criterion was based on the minimum hours of care stated to qualify as dementia caregiver based on previous large-scale studies (Alzheimer’s Disease International, 2018; Bremer et al., 2015). Fourth, the care should involve day-to-day decision-making as well as activities of daily living. As for the care-recipients, they had on average about one weekly session in the community centers. With COVID, the session was implemented online. Exclusion criteria for the caregivers were as follows: signs of severe intellectual deficits, reported suicidal ideation, exhibited evidence of psychotic disorders, hearing/ visual impairment or inability to read or speak Chinese/Cantonese fluently.
A cluster randomized controlled trial was conducted with twelve clusters for each arm (CTC versus BSB) with eight caregivers for each cluster. The rationale was to minimize the risk of the control group participants inadvertently being exposed to the intervention which they were not supposed to be involved in information. For the sample size confirmation for implementing our plans of a cluster randomized trial, the following provides the rationale of estimation. The rationale for the sample size calculation was as follows. A variety of effect sizes have been detected in the outcome variables for recent caregiving studies (Walter and Pinquart, 2020; Cheng et al., 2020). For the present study to detect a medium effect size, the sample size for an individual-level randomized controlled trial would be 64 per group with power at 0.8 and alpha at 0.05 (Cohen, 1992). For cluster randomized controlled trial, we used the adjustment formula of 1+ (n-1) ρ (Campbell, 2000) with the following specifications: intra-class correlation (ρ) of 0.05 estimated (Cheng et al., 2016) and a cluster sample (n) = 7. Twelve clusters per arm (CTC versus BSB) with 7 caregivers for each cluster would be sufficient to detect a difference of medium size effect.
For the procedure, an invitation was sent out by the participating social service centers via text messages and email. There were altogether twelve rounds of subject recruitment. The staff in the respective agency would collect the information from the interested caregiver to do the screening according to the criteria stated above. All interventions were carried by phone throughout the study. Data was collected from 2018 to 2021. During the period of data collection, The Hong Kong Government has declared the Coronavirus Disease 2019 (COVID-19) viral outbreak as an "emergency" with highest warning tier on 25 January 2020. During COVID-19, we continued recruitment and interventions by phone and text messages. A total of eight therapists were trained to conduct the interventions with 4 for each condition. All therapists have an undergraduate qualification in either social work or counseling. Each therapist was involved in eight-hour training and discussion of the protocol followed by bi-weekly discussion of the cases. Data was collected from 2018 to 2021.
Interventions
The study used prospective design to test the intervention effects Connecting Through Caregiving (CTC) intervention constituting the following components 1) relational insights; 2) self-awareness; 3) empathetic understanding of care-recipient; 4) integrating self-care and caring for others and 5) negotiation. Telephone sessions were used to maximize accessibility and sustainability of interventions. The CTC program was evaluated against a Basic Skill Building (BSB) as active control in a two-arm randomized controlled trial. Both groups had 12 weeks of telephone intervention and a three-month follow-up. Measures were obtained at baseline Weeks 1 (pre-intervention), Week 12 (post-intervention) with a follow-up at Week 24. Recruitment, random assignment and blinding procedures were carried out according to the guidelines specified in the CONSORT statement. The primary outcome was the reduction of depressive symptoms. The four secondary outcomes relating to behavioral problems of the care recipient and social support received by the caregiver were as follows. First, we tested whether, as compared to those in BSB, CTC participants would perceive a decrease in behavioral problems of the care recipients. Second, CTC participants would report a decreased caregiver's distress caused by behavioral problems. The third and fourth outcomes were enhanced emotional and instrumental support perceived by the CTC participants. We examined the possible mediation effects of perspective taking strategies on intervention with regard to the primary outcome (i.e. depressive symptoms of the caregivers. Finally, as part of the study was conducted during COVID-19, we tested for moderation effect of COVID-19 on intervention effects.
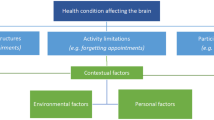
The 12 sessions of the CTC program can be divided into three four-week components. These components included the following: awareness of self, understanding others and integrating positive and negative aspects of caregiving to form implementation plans (Fig. 1). Both CTC and BSB shared similar structures. However, while BSB spent more time on basic skills, CTC spent more time on perspective- taking. Interventions were delivered by phone by trained social workers or counsellors. All phone sessions took about 45 minutes. While BSB would concentrate sole on building skill, CTC participants would spend less time on skills and use 50 % of the session time to participate with intergeneration perspective-taking reappraisal exercises. For both groups, there were basically three blocks subdividing the twelve sessions: 1) self-orientated; 2) others-orientated and 3) integration and implementation. Both groups involved skills building and worksheets adapted from Gallagher-Thompson et al. (2010). For the first block, skills included monitoring mood and activities, relaxation techniques and scheduling pleasant events. For the second block, skill building includes basic communication with the care recipient (simplifying and distraction), and effective/ assertive communication skills to communicate the caregivers’ own needs with other family member or related persons including helpers and professional staff. The third component involved integration, designing implementation plans and subsequent review of plans Au et al. (2019b).
Intervention Components and Session Plan. (CG: caregiver; CR: care recipient) The CTC aims to develop self-awareness and empathetic understanding followed by subsequent integration of different perspectives. While BSB will concentrate sole on building skill, CTC participants will spend 50% of time on skills and use 50 % of the session time to participate with intergeneration perspective-taking reappraisal exercises
Unique components of the CTC were based the theoretical model of perspective taking in Biggs et al. formulation and were initially tested in our pilot study (Au et al., 2019a, b). The CTC aimed to provide a structure for reappraisal of intergeneration relationships by develop self-awareness and empathetic understanding followed by subsequent integration of different perspectives. To facilitate self-understanding in the first block, participants was asked to reflect on 1) their occupation/ life events prior to caregiving; 2) process leading to their adoption of the caregiving role and 3) major adjustments to their lives after being a caregiver. To facilitate empathetic understanding of the care recipient in the second block, participants reflected on the following: 1) the life history of the person they were caring for; 2) immediate events prior to onset of dementia and 3) major changes in the care recipients not only at the functional level but also to possible unfulfilled goals. To understand more about other family members who could offer potential/ actualized help, the participant would think about 1) process leading to their assistance in caregiving role and 2) how this role affects them. Participants were encouraged to develop some understanding of their own experience and also be able to perceive the priorities and difficulties of the care-recipient and other helpers which might or might not overlap with their own. The third block focused on integrating perspectives from different people and possibly, associated affection and conflicts. Positive, negative and/or ambivalent caregiving experiences were reviewed. Finally, the caregiver was encouraged to negotiate with other family members strategies which would help to protect the well-being of the caregivers and sustain the caregiving relationship. In sum, the intervention adopted the multiple perspectives and re-appraisals to an emotionally-laden event (i.e. dementia caregiving) to modulate the emotional response and subsequent behaviors.
Measures
Measures taken included the following. First, demographic and related information including age, sex (male/female), education, socio-economic information and number of hours spent in caregiving per week and nature of tasks involved, presence of and help from domestic helper, attendance in day centers and services received from community centers (all recorded at Week 1 only). All primary and secondary outcomes were taken at Week 1 (T0 : pre-intervention), Week 12 (T1 : post-intervention) and Week 24 (T2 : three-month follow-up). The primary outcome was depressive symptoms as measured by CES-D (Radloff, 1977). There were two secondary outcomes. The first secondary outcome was gauged by the Revised Memory and Behavior Checklist (Rice et al. 2022, Teri et al., 1992). Scores were computed for the presence or absence (BP) of each of the 24 listed problem first, and then for caregiver reactions (BR) as gauged by the extent to which caregivers were “bothered” or “distressed” by each behavior. Frequency of behaviors are assessed based on a Likert-scale of 0 ( never occurs) to 4 (occurs daily or more often). Reactions are assessed by asking how upsetting the behavior was on a Likert scale of 0 (not at all) to 4 (extremely). Social Support (SS) was measured by two items tapping on the frequency of receipt of emotional and instrumental support (Au et al., 2009): “How often does/do your [spouse and children/relatives/friends] make you feel cared for and listened to?” and “How often does your [spouse and children/relatives/friends] help with daily tasks and give you advice when needed?” Participants rated each item on a 5-point scale that ranged from 0=none, 1= rarely, 2=sometimes, 3=most of the time, 4=all the time. Finally, the mediation effect of perspective-taking (PT) was tested. Based on Au et al., 2019a), the frequency of using perspective taking was gauged by a 7-item scale (rating from 0 to10) validated to measure intergeneration perspective taking, Items include the 1) caregiver’s self-understanding of own situation, needs and feelings; 2) understanding the care-recipient’s situation, needs and feelings, 3) caregiver’s self-understanding that his/her life experience can influence his thoughts and feelings, 4) understanding that the care-recipients life experience can influence his or her thoughts and feelings 5) understanding that there can be different perspectives 6) taking into account different perspectives in communication and 7) paying attention to these different perspectives.
Data Analysis
SPSS Linear Mixed Model procedures (Shek & Ma, 2011) was used to evaluate the effect of intervention on the outcomes, with Time 0 (Baseline), Time 1 (Week12) and Time 2 (Week 12) as the within-subject variable. An unstructured covariance pattern was modelled. Both main effects of the intervention and Time, and the interaction between Intervention and Time will be tested at 95% confidence level. The Kolmogorov-Smirmov test results suggested that the variables were not normally distributed. Hence, the Mann-Whitney U test was used to compare all the variables between the CTC and BSB across three time points. The Process Model was used to test the mediation effect of perspective-taking between intervention and CES-D (Hayes, 2022). Finally, moderation analysis was also carried to test whether the presence of COVID-19 had any effect on the intervention results (Table 1).
A two-arm cluster randomized controlled trial was conducted for 176 participants with 24 clusters. A total of 176 adult caregiver participants were recruited. Ninety-one caregivers completed CTC and eighty-five completed BSB (Fig. 2). The demographics of the caregiver and care recipients can be found in Table 1. There were no significant differences between the 2 groups in terms of demographics, relationship with care-recipients (mostly daughters), education (both secondary and tertiary), occupation (mostly full-time), hours of caregiving and caregiving tasks as well as the age, gender and stage of dementia of the care-recipients.
The reliabilities (Cronbach alpha) of the scales used ranged between 0.78 to 0.82. Significant results were obtained for the primary variable: Centre for Epidemiological Studies-Depresion-20 [F=21.79, p<.001].] The secondary variables are also all significant: 1) Revised Memory and Behavioral Problems Checklist (RMBP) Symptoms [F=7.20, p=.003] and Reaction (RMPR) [F=17.95, p<.001]) as well as Social Support [F= 24.99, p<.001]. The mediating variable Perspective Taking was significant [F=18.39, p<.001]. The comparison of the two groups was carried out by using the Mann-Whitney test. The reliabilities (Cronbach alpha) of the scales used ranged between 0.78 to 0.82. The effect size Cohen r was calculated by dividing Z by the square root of the number of participants. Apart from the presence of behavioral problems, the Cohen r of all other variables ranged from 0.31 to 0.37, suggesting an overall medium effect size for the CTC intervention (Brydges, 2019; Carriedo et al., 2020; Fritz et al., 2012). The results of these variables with effect sizes across three time-points can be found in Table 2.
Perspective taking (PT) was found to have a partial mediation effect between Intervention and CES-D. The direct path between Group and CES-D was significant [B = -2.77, SE = 0.51, t=-5.41, p < 0.001, 95% CI = -3.77, -1.76]. The path from Group to Perspective-taking was significant [B = 5.74, SE = 1.32, t = 4.33, p<0.001, 95% CI = 3.13, 8.56]. The path from PT to CESD was also significant [B = -0.12, SE = 0.03, t = -4.42, CI = -0.18, -0.07, p <0.001]. The direct path between Intervention and CESD was as follows: [B = -2.77, SE = 0.51, t = -5.41, p < 0.01, 95% CI = -3.77, -1.76]. The indirect path effect was 0.70 [SE = 0.28, CI= -1.33, -0.25]. In addition, the possible moderation effect of COVID-19 on intervention effect was also tested. Prior to COVID-19, 38 caregivers completed CTC and 34 completed BSB. During COVID-19, 53 caregivers completed CTC and 51 caregivers completed BSB. The results obtained were as follows. No significant moderation effect was found for COVID-19 (CES-D: F=0.66, p=0.42; PT: F=1.17, p=0.28; RMBP: F= 0.27, p= 0.61; RMBR: F=2.5, p=0.11; SS: F=2.33, p=0.13).
Conclusion & Discussion
The present findings provided empirical support that perspective-taking interventions could reduce depressive symptoms and enhance perspective-taking. The mediation effect of perspective-taking on change in depressive symptoms was also supported. At the same time, there was significant improvement in both emotional and instrumental social support. In addition, while the changes in perceived presence of symptoms in the care-recipients had a relatively small effect size, the negative reactions to these symptoms were reduced with medium effect sizes. No moderation of COVID-19 was found on the intervention effects. Results of the present study provided support for an intervention model incorporating the facilitation of self-awareness and empathetic insight. Western Pacific Region has the highest number of people with dementia (WHO, 2021; Jia et al., 2020). Improvements in life expectancy have changed the structure of multigenerational families and have resulted in extended periods of social and emotional support exchanges including caregiving over the life span. The study is relevant to this cultural context of dementia care.
The study has made three major advancements. First, a more comprehensive perspective-taking protocol and more detailed assessments were developed to promote and gauge relational insights. Second, the findings provided support for the intervention could be effectively delivered using of non-digitalized and low-cost technology. Finally, the present findings would support that the CTC intervention was effective for both pre-pandemic and pandemic situations. These advancements will be discussed with more details in the following.
First, we have used a more comprehensive perspective-taking intervention protocol and assessment framework. In the pilot study (Au et al., 2019a), we have simply asked the caregiver about changing the way you think by adopting different perspectives about the caregiving role and the care-recipient. In the present study, we have used a more detailed perspective scale to capture more dimensions of perspective-taking developed in a more detailed protocol. These included more detailed facilitation of a more individualized caregiver’s and the care-recipient’s life experience and how these experiences could influence thoughts and feelings. In terms of outcomes, the present study also suggested that CTC contributed to the caregiver’s reduced reactions to behavioural symptoms and enhanced social support. For gauging the outcomes of the present study, we have also included social support as well as presence and reactions to behavioral problems.
Second, telephone-administered interventions allowed more opportunities for addressing the individualized concerns of each caregiver. As the sessions were carried out at times convenient to the caregivers, they offered the increased capacity to support the caregiver without the added burden of traveling outside the home. While interventions by virtual reality have been found to be effective for dementia caregivers (Jütten et al., 2018), the phone intervention of the present study could help non-digitalized caregivers. The present study also provides evidence that perspective-taking reappraisal exercises can also be implemented via low-cost technology (i.e. telephone) which enhance the availability of interventions even during COVID-19.
Finally, the intervention was found to be effective for both pre-pandemic and pandemic situations. COVID-19 had resulted in sudden reduction in the availability of social support services. These sudden changes could add on to the distress for both the unpaid caregiver and the care-recipient (Moon et al., 2022; Giebel et al., 2021). Risks for COVID-19 may be heightened for family members who work outside the home and provide care, or for those family members who care for multiple generations (Stokes and Patterson, 2020). However, closer relationships with the care-recipient during the COVID-19 pandemic was also observed (Tulloch et al., 2022). Results of the present study would suggest that the present intervention was effective during the pandemic. The present study also provided support that perspective-taking reappraisal exercises can also be implemented via low-cost technology (i.e. telephone) which enhance the availability of interventions during pandemic conditions. Results suggest that the present telephone administered intervention can offer a safe and cost-effective means to overcome some barriers of caregiving during COVID-19 and pandemic situations.
However, there are some aspects of the study that require improvement. With reference to the likelihood of changing demands of caregiving over time, more attention should be given to understanding how to deal with complex and conflicting emotions in some cases. Second, perceived family and social support is significantly associated with well-being of dementia caregivers (Rote et al. 2021; Au et al., 2009). Filial piety has also been found to be a protective function to reduce the negative effects of stressors and to enhance the positive effect of appraisal factors on caregiving burden (Lai, 2010). However, these caregivers often have very little support and small network sizes (Cheng et al., 2013). More effort should be directed to understanding ways of empowering family members who are potentially able to assist the primary caregiver (Kunik et al., 2020; Wang et al., 2019). Third, more attention should be paid to how one member of the dyad can affect the well-being of the other in terms of both mental and physical health. Future studies should also consider enhancing more mutual support among the caregivers and also access to community resources. Finally, more longitudinal research is needed for both caregivers and care-recipients with a framework that emphasizes the the intersectionality of sociocultural factors, health care systems’ factors, and dementia care needs as they evolve across time (Gallagher-Thompson et al., 2020).
References
Alzheimer’s Disease International. (2018), Global Estimates of informal care. https://doi.org/10.1016/j.jalz.2016.07.150.
Au, A., Lai, M. K., Lau, K. M., Pan, P. C., Lam, L., Thompson, L., & Gallagher-Thompson, D. (2009). Social support and well-being in dementia family caregivers: the mediating role of self-efficacy. Aging and Mental Health, 13(5), 761–768. https://doi.org/10.1080/13607860902918223
Au, A., Lai, D. W. L., Biggs, S., Cheng, S. T., Biggs, I. H., Chow, A., & Gallagher-Thompson, D. (2019a). Perspective-taking Interventions for Intergenerational Caregivers of Alzheimer’s Diseases: A Randomized Controlled Trial. Research on Social Work Practice, 30(3), 309–316. https://doi.org/10.1177/1049731519864165
Au, A., Yip, H.-M., Lai, S., Ngai, S., Cheng, S. T., Losada, A., Thompson, L., & Gallagher-Thompson, D. (2019b). Telephone-based behavioral activation intervention for dementia family caregivers: Outcomes and mediation effect of a randomized controlled trial. Patient Education and Counseling, 102(11), 2049–2059. https://doi.org/10.1016/j.pec.2019.06.009
Bei, E., Morrison, V., Zarzycki, M., & Vilchinsky, N. (2023). Barriers, facilitators, and motives to provide distance care, and the consequences for distance caregivers: A mixed-methods systematic review. Social Science & Medicine, 115782. https://doi.org/10.1016/j.socscimed.2023.115782
Biggs, S., & Lowenstein, A. (2011). A Critical Approach to Age Relationships. Routledge. https://doi.org/10.4324/9780203827918
Biggs, S., Carr, A., & Haapala, I. (2019). Dementia as a source of social disadvantage and exclusion. Australasian Journal on Ageing, 38, 26–33. https://doi.org/10.1111/ajag.12654
Bremer, P., Cabrera, E., Leino-Kilpi, H., Lethin, C., Saks, K., Sutcliffe, C., Soto, M., Zwakhalen, S. M., Wübker, A., & RightTimePlaceCare Consortium. (2015). Informal dementia care: Consequences for caregivers' health and health care use in 8 European countries. Health Policy., 119(11), 1459–1471. https://doi.org/10.1016/j.healthpol.2015.09.014
Brydges, C. R. (2019). Effect Size Guidelines, Sample Size Calculations, and Statistical Power in Gerontology. Innovations in Aging. https://doi.org/10.1093/geroni/igz036
Campbell, M. J. (2000). Cluster randomized trials in general family practice research. Statistical Methods in Medical Research, 9(2), 81–94. https://doi.org/10.1177/096228020000900202
Carriedo, A., Cecchini, J. A., Fernandez-Rio, J., & Méndez-Giménez, A. (2020). Psychological Well-being and Physical Activity Levels in Older Adults During the Nationwide Lockdown in Spain. American Journal of Geriatric Psychiatry, 28(11), 1146–1155. https://doi.org/10.1016/j.jagp.2020.08.007
Chan C.Y., Cheung G., Martinez-Ruiz A., Chau P.Y.K, Wang K., Yeoh E.K, Wong E.L.Y. (2021). Caregiving burnout of community-dwelling people with dementia in Hong Kong and New Zealand: a cross-sectional study. BMC Geriatrics, 21(1):261. https://doi.org/10.1186/s12877-021-02153-6.
Cheng, S. T., Lam, L. C., Kwok, T., Ng, N. S., & Fung, A. W. (2013). The social networks of Hong Kong Chinese family caregivers of Alzheimer's disease: correlates with positive gains and burden. Gerontologist, 53(6), 998–1008. https://doi.org/10.1093/geront/gns195
Cheng, S. T., Fung, H. H., Chan, W. C., & Lam, L. C. (2016). Short-Term Effects of a Gain-Focused Reappraisal Intervention for Dementia Caregivers: A Double-Blind Cluster-Randomized Controlled Trial. Am J Geriatr Psychiatry., 24(9), 740–750. https://doi.org/10.1016/j.jagp.2016.04.012
Cheng, S. T., Au, A., Losada, A., Thompson, L. W., & Gallagher-Thompson, D. (2019). Psychological Interventions for Dementia Caregivers: What We Have Achieved, What We Have Learned. Current Psychiatry Report, 21(7), 59. https://doi.org/10.1007/s11920-019-1045-9
Cheng, S. T., Li, K. K., Losada, A., Zhang, F., Au, A., Thompson, L. W., & Gallagher-Thompson, D. (2020). The effectiveness of nonpharmacological interventions for informal dementia caregivers: An updated systematic review and meta-analysis. Psychology of Aging, 35(1), 55–77. https://doi.org/10.1037/pag0000401
Cheng, S.-T., Chan, W. C., & Lam, L. C. W. (2022). Are care-recipient outcomes attributable to improved caregiver well-being? A cluster-randomized controlled trial of benefit-finding intervention. The American Journal of Geriatric Psychiatry, 30(8), 903–913. https://doi.org/10.1016/j.jagp.2021.08.009
Cohen, J. (1992). Statistical power analysis. Current directions in psychological science, 1(3), 98–101.
Dewitte, L., van Wijngaarden, E., Schellekens, T., Vandenbulcke, M., & Dezutter, J. (2021). Continuing to participate in the dance of life as oneself: The lived experience of meaning in life for older adults with Alzheimer’s disease. The Gerontologist, 61(7), 1019–1029. https://doi.org/10.1093/geront/gnaa206
Ebert, A. R., Miron, A. M., Hodel, A. E., Rowley, S. K., Davis, R., & Melotik, E. (2020). Perspective taking and empathic emotions in letters written by grandchildren to their grandparent with dementia versus grandparent without dementia. Journal of Family Issues, 41(1), 62–84. https://doi.org/10.1177/0192513X19868830
Ferraris, G., Dang, S., Woodford, J., & Hagedoorn, M. (2022). Dyadic Interdependence in Non-spousal Caregiving Dyads' Wellbeing: A Systematic Review. Frontiers Psychology, 13, 882389. https://doi.org/10.3389/fpsyg.2022.882389
Friedman, E. M., & Kennedy, D. P. (2021). Typologies of dementia caregiver support networks: A pilot study. The Gerontologist, 61(8), 1221–1230. https://doi.org/10.1093/geront/gnab013
Fritz, C. O., Morris, P. E., & Richler, J. J. (2012). Effect size estimates: current use, calculations, and interpretation. Journal of Experimental Psychology Genernal, 141(1), 2–18. https://doi.org/10.1037/a0024338 Erratum in: J Exp Psychol Gen. 2012 Feb;141(1):30.
Gallagher-Thompson, D., Wang, P. C., Liu, W., Cheung, V., Peng, R., China, D., & Thompson, L. W. (2010). Effectiveness of a psychoeducational skill training DVD program to reduce stress in Chinese American dementia caregivers: results of a preliminary study. Aging and Mental Health, 14(3), 263–273. https://doi.org/10.1080/13607860903420989
Gallagher-Thompson, D., Choryan Bilbrey, A., Apesoa-Varano, E. C., Ghatak, R., Kim, K. K., & Cothran, F. (2020). Conceptual Framework to Guide Intervention Research Across the Trajectory of Dementia Caregiving. The Gerontologist, 60(Suppl 1), S29–S40. https://doi.org/10.1093/geront/gnz157
Gaugler, J. E., Reese, M., & Mittelman, M. S. (2016). Effects of the Minnesota Adaptation of the NYU Caregiver Intervention on Primary Subjective Stress of Adult Child Caregivers of Persons With Dementia. Gerontologist., 56(3), 461–474. https://doi.org/10.1093/geront/gnu125
GBD 2019 Dementia Forecasting Collaborators. (2020). Estimation of the global prevalence of dementia in 2019 and forecasted prevalence in 2050: an analysis for the Global Burden of Disease Study 2019. Lancet, 2020(396), 413–446. https://doi.org/10.1016/S2468-2667(21)00249-8
Giebel, C., Cannon, J., Hanna, K., Butchard, S., Eley, R., Gaughan, A., et al. (2021). Impact of COVID-19 related social support service closures on people with dementia and unpaid carers: a qualitative study. Aging & mental health, 25(7), 1281–1288. https://doi.org/10.1080/13607863.2020.1822292
Haapala, I., Carr, A., & Biggs, S. (2019). What you say and what I want: Priorities for public health campaigning and initiatives in relation to dementia. Australasian Journal on Ageing, 38. Suppl, 2, 59–67. https://doi.org/10.1111/ajag.12647
Hayes, A. F. (2022). Introduction to mediation, moderation, and conditional process analysis: A regression-based approach (3rd ed.). The Guilford Press.
Janus, A. L., & Koslowski, A. (2020). Whose responsibility? Elder support norms regarding the provision and financing of assistance with daily activities across economically developed countries. European Journal of Ageing, 17(1), 95–108. https://doi.org/10.1007/s10433-019-00515-z
Jia, L., Quan, M., Fu, Y., Zhao, T., Li, Y., Wei, C., Tang, Y., Qin, Q., Wang, F., Qiao, Y., Shi, S., Wang, Y. J., Du, Y., Zhang, J., Zhang, J., Luo, B., Qu, Q., Zhou, C., Gauthier, S., & Jia, J. (2020). Group for the Project of Dementia Situation in China. Dementia in China: epidemiology, clinical management, and research advances. Lancet Neurology, 1, 81–92. https://doi.org/10.1016/S1474-4422(19)30290-X
Jütten, L. H., Mark, R. E., & Sitskoorn, M. M. (2018). Can the Mixed Virtual Reality Simulator Enhance Empathy and Understanding and Decrease Burden in Informal Dementia Caregivers? Dementia and Geriatric Cognitive Disorder Extra, 8(3), 453–466. https://doi.org/10.1159/000494660
Kunik, M. E., Stanley, M. A., Shrestha, S., Ramsey, D., Richey, S., Snow, L., Freshour, J., Evans, T., Newmark, M., Williams, S., Wilson, N., & Amspoker, A. B. (2020). Aggression Prevention Training for Individuals With Dementia and Their Caregivers: A Randomized Controlled Trial. Am J Geriatr Psychiatry., 28(6), 662–672. https://doi.org/10.1016/j.jagp.2020.01.190
Lai, D. W. L. (2010). Filial piety, caregiving appraisal, and caregiving burden. Research on Aging, 32(2), 200–223. https://doi.org/10.1177/0164027509351475
Livingston, G., Huntley, J., Sommerlad, A., Ames, D., Ballard, C., Banerjee, S., Brayne, C., Burns, A., Cohen-Mansfield, J., Cooper, C., Costafreda, S. G., Dias, A., Fox, N., Gitlin, L. N., Howard, R., Kales, H. C., Kivimäki, M., Larson, E. B., Ogunniyi, A., et al. (2020). 2020 report of the Lancet Commission. Lancet, 8(396), 413–446. https://doi.org/10.1016/S0140-6736(20)30367-6
Losada, A., Márquez-González, M., Romero-Moreno, R., Mausbach, B. T., López, J., Fernández-Fernández, V., & Nogales-González, C. (2015). Cognitive-behavioral therapy (CBT) versus acceptance and commitment therapy (ACT) for dementia family caregivers with significant depressive symptoms: Results of a randomized clinical trial. Journal of Consulting Clinical Psychology, 83(4), 760–772. https://doi.org/10.1037/ccp0000028
Lyons, K. S., Zarit, S. H., Sayer, A. G., & Whitlatch, C. J. (2002). Caregiving as a dyadic process: Perspectives from caregiver and receiver. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 57(3), 195–204. https://doi.org/10.1093/geronb/57.3
Matthews, M., Webb, T. L., Shafir, R., Snow, M., & Sheppes, G. (2021). Identifying the determinants of emotion regulation choice: a systematic review with meta-analysis. Cognition and Emotion, 35(6), 1056–1084. https://doi.org/10.1080/02699931.2021.1945538
Merrilees, J. J., Bernstein, A., Dulaney, S., Heunis, J., Walker, R., Rah, E., et al. (2020). The Care Ecosystem: promoting self-efficacy among dementia family caregivers. Dementia, 19(6), 1955–1973. https://doi.org/10.1177/1471301218814121
Miller, L. M., Kaye, J. A., Lyons, K. S., Lee, C. S., Whitlatch, C. J., & Caserta, M. S. (2019). Well-being in dementia: a cross-sectional dyadic study of the impact of multiple dimensions of strain on persons living with dementia and their family care partners. International Psychogeriatrics, 31(5), 617–626. https://doi.org/10.1017/S104161021800203X
Miron, A. M., Thompson, A. E., McFadden, S. H., & Ebert, A. R. (2019). Young Adults' Concerns and Coping Strategies Related to their Interactions with their Grandparents and Great-Grandparents with Dementia. Dementia (London), 18(3), 1025–1041. https://doi.org/10.1177/1471301217700965
Moon, H. E., Rote, S. M., Sears, J., & Schepens Niemiec, S. L. (2022). Racial differences in the dementia caregiving experience during the COVID-19-19 pandemic: Findings from the National Health and Aging Trends Study (NHATS). The Journals of Gerontology: Series B, 77(12), e203–e215. https://doi.org/10.1093/geronb/gbac098
Radloff, L. S. (1977). The CES-D Scale: A self-report depression scale for research in the general population. Applied Psychological Measurement, 1(3), 385–401. https://doi.org/10.1177/014662167700100306
Rice, J. D., Sperling, S. A., Brown, D. S., Mittleman, M. S., & Manning, C. A. (2022). Evaluating the efficacy of TeleFAMILIES: a telehealth intervention for caregivers of community-dwelling people with dementia. Aging & Mental Health, 26(8), 1613–1619. https://doi.org/10.1080/13607863.2021.1935462
Rippon, I., Quinn, C., Martyr, A., Morris, R., Nelis, S. M., Jones, I. R., et al. (2020). The impact of relationship quality on life satisfaction and well-being in dementia caregiving dyads: Findings from the IDEAL study. Aging & mental health, 24(9), 1411–1420. https://doi.org/10.1080/13607863.2019.1617238
Rote, S. M., Angel, J. L., Kim, J., & Markides, K. S. (2021). Dual Trajectories of Dementia and Social Support in the Mexican-Origin Population. Gerontologist, 61(3), 374–382. https://doi.org/10.1093/geront/gnaa100
Shek, D. R., & Ma, C. M. (2011). Longitudinal data analyses using linear mixed models in SPSS: concepts, procedures and illustrations. ScientificWorld Journal, 11, 42–76. https://doi.org/10.1100/tsw2011.2
Silverstein, M., Conroy, S. J., & Gans, D. (2012). Beyond solidarity, reciprocity and altruism: moral capital as a unifying concept in intergenerational support for older people. Ageing and Society, 32(7), 1246–1262. https://doi.org/10.1017/S0144686X1200058X
Stedje, K., Kvamme, T. S., Johansson, K., Sousa, T. V., Odell-Miller, H., Stensæth, K. A., Bukowska, A. A., Tamplin, J., Wosch, T., & Baker, F. A. (2023). The Influence of Home-Based Music Therapy Interventions on Relationship Quality in Couples Living with Dementia-An Adapted Convergent Mixed Methods Study. International Journal of Environmental Research and Public Health, 20(4), 2863. https://doi.org/10.3390/ijerph20042863
Stokes, J. E., & Patterson, S. E. (2020). Intergenerational relationships, family caregiving policy, and COVID-19-19 in the United States. Journal of Aging & Social Policy, 32(4-5), 416–424. https://doi.org/10.1080/08959420.2020.1770031
Teri, L., Truax, P., Logsdon, R., Uomoto, J., Zarit, S., & Vitaliano, P. P. (1992). Assessment of behavioral problems in dementia: the revised memory and behavior problems checklist. Psychology and Aging, 7(4), 622–631. https://doi.org/10.1037/0882-7974.7.4.622
Tsapanou, A., Papatriantafyllou, J. D., Yiannopoulou, K., Sali, D., Kalligerou, F., Ntanasi, E., Zoi, P., Margioti, E., Kamtsadeli, V., Hatzopoulou, M., Koustimpi, M., Zagka, A., Papageorgiou, S. G., & Sakka, P. (2021). The impact of COVID-19 pandemic on people with mild cognitive impairment/dementia and on their caregivers. International Journal of Geriatric Psychiatry., 36(4), 583–587. https://doi.org/10.1002/gps.5457
Tulloch, K., McCaul, T., & Scott, T. L. (2022). Positive aspects of dementia caregiving during the COVID-19-19 pandemic. Clinical Gerontologist, 45(1), 86–96. https://doi.org/10.1080/07317115.2021.1929630
Walter, E., & Pinquart, M. (2020). How Effective Are Dementia Caregiver Interventions? An Updated Comprehensive Meta-Analysis. Gerontologist, 60(8), 609–619. https://doi.org/10.1093/geront/gnz118
Wang, Q., Sheng, Y., Wu, F., Zhang, Y., & Xu, X. (2019). Effect of different sources support on adaptation in families of patient with moderate-to-severe dementia in China. American Journal of Alzheimer's Disease & Other Dementias®, 34(6), 361–375. https://doi.org/10.1177/1533317519855154
World Health Organization. (2021). Global Status Report on the Public Health Response to Dementia. ISBN: 978-92-4-003324-5
Xu, L., Liu, Y., He, H., Fields, N. L., Ivey, D. L., & Kan, C. (2021). Caregiving intensity and caregiver burden among caregivers of people with dementia: The moderating roles of social support. Archives of Gerontology and Geriatrics, 94, 104334. https://doi.org/10.1016/j.archger.2020.104334
Yang, B., Feldman, M. W., & Li, S. (2023). Care-receivers’ expected intergenerational support in aging rural China: A perspective of sustainable livelihoods and the sandwich effect. The Social Science Journal, 1-21. https://doi.org/10.1080/03623319.2022.2156441
Acknowledgements
The study was funded by the General Research Fund of the Research Grant Council in Hong Kong (15606317). For the recruitment of participants, we thank the District and Neighbourhood Elderly Community Centres in Kowloon East, Kowloon Central and Hong Kong West. In particular, we wish to thank the Christian Family Service, Hong Kong Family Society, Yan Oi Tong and Tung Wah Group of Hospitals Community Services. We are also grateful for the support of the Integrative Community Health Centre and Institute of Active Ageing at Hong Kong Polytechnic University.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics Approval
Ethics Approval has been obtained from the Hong Kong Polytechnic University with the following reference number: HSEARS20161020001. The Authors declare that there is no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Au, A., Lai, D.W.L., Chow, A.Y.M. et al. Connecting Through Caregiving: Reappraising Intergeneration Relationship in Dementia Caregiving. Applied Research Quality Life 18, 2441–2457 (2023). https://doi.org/10.1007/s11482-023-10193-w
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11482-023-10193-w