Abstract
Depression is common during pregnancy and is associated with reduced adherence to HIV-related care, though little is known about perinatal trajectories of depression and viral suppression among women living with HIV (WLHV) in sub-Saharan Africa. We sought to assess any association between perinatal depressive symptoms and viral non-suppression among WLWH. Depressive symptomatology and viral load data were collected every 6 months from WLWH enrolled in the African Cohort Study (AFRICOS; January 2013–February 2020). Generalized estimating equations modeled associations between depressive symptoms [Center for Epidemiological Studies Depression (CES-D) ≥ 16] and viral non-suppression. Of 1722 WLWH, 248 (14.4%) had at least one pregnancy (291 total) and for 61 pregnancies (21.0%), women reported depressive symptoms (13.4% pre-conception, 7.6% pregnancy, 5.5% one-year postpartum). Depressive symptomatology was associated with increased odds of viral non-suppression (aOR 2.2; 95% CI 1.2–4.0, p = 0.011). Identification and treatment of depression among women with HIV may improve HIV outcomes for mothers.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Girls and women of childbearing age account for 59% of new HIV infections in sub-Saharan Africa (SSA) [1], and many women living with HIV (WLWH) intend to have children [2]. Fortunately, over the last two decades, the number of children born with HIV due to vertical transmission has decreased dramatically with public health measures such as increased uptake of safe and effective antiretroviral therapy (ART) for pregnant women [3,4,5,6]. Though effective HIV prevention and treatment interventions exist and are available in SSA [7, 8], dramatic gaps in uptake are reported, including loss to follow up (as high as 88% in some contexts) and poor adherence to ART [9], particularly among young women of reproductive age in SSA [10, 11]. HIV incidence among pregnant women at antenatal clinics ranges from 1.5% (South Africa) [12] to 3.3% (Western Kenya) [13]. The rate of vertical HIV transmission with no intervention (defined as the rate of children born with HIV that was acquired from their mother during pregnancy, childbirth, or breastfeeding) ranges between 13 and 48% [14, 15].
Depression is a common mental disorder that affects many WLWH and is associated with both ART adherence and pregnancy outcomes [14, 16,17,18,19]. WLWH have a significantly higher odds of depressive symptoms during the antenatal (odds ratio [OR] 1.42; 95% confidence interval [CI] 1.12–1.80) and postnatal (OR 1.58; 95% CI 1.08–2.32) periods (together termed the “perinatal period”), compared to pregnant women living without HIV [20]. Globally, studies estimate that between 25 to 50% of pregnant WLWH have antenatal depressive symptoms at time points in every trimester of pregnancy [15, 16, 20,21,22,23]. Depression and low social support can reduce ART adherence for pregnant WLWH [24], which can lead to viral non-suppression and increased risk of vertical transmission of HIV [25,26,27]. In addition to the behavioral link between depressive symptoms and viral load, depression has also been shown to be directly associated with viral load, even in cases of high adherence to ART, through an altered immune response [28,29,30]. Evidence suggests that treatment with antidepressant medication may reduce susceptibility to cellular infection [30, 31]. Additionally, pregnant WLWH facing mental health difficulties experience risk of medical sequelae for their newborns such as preterm birth, stillbirths, and babies born with low birthweight [32]. ART usage has shown mixed results in alleviating this risk [3, 32].
Studies of HIV and mental health among pregnant WLWH have largely focused on ART use and adherence as proxies for viral non-suppression [33,34,35]. While associations between self-report adherence to ART and viral load are generally strong among pregnant women, pharmacologic tests of viral non-suppression are more robust and allow for a more accurate assessment of risk for vertical transmission than adherence metrics alone [36, 37]. Viral load is an important clinical indicator of HIV care and the final target of the UNAIDS 90–90–90 [38]. Understanding whether depression directly affects viral non-suppression for pregnant WLWH would enable providers to target HIV and maternal health services to address depressive symptoms, reduce vertical HIV transmission, and improve child survival. In addition, gaps remain in understanding the impact of depression on viral load throughout the perinatal period, from pre-conception, through pregnancy, and postpartum. The primary objective of this analysis is to understand the association between depressive symptoms and viral non-suppression among pregnant WLWH in Nigeria, Kenya, Uganda, and Tanzania during their perinatal period. The secondary objective is to explore associations between depressive symptoms and viral non-suppression on birth outcomes, including preterm birth and pregnancy loss.
Methods
Study Design and Participants
The African Cohort Study (AFRICOS) is an ongoing prospective longitudinal cohort study enrolling people living with HIV (PLWH) at 12 HIV care clinical sites in Kenya, Tanzania, Uganda and Nigeria [34, 39,40,41]. These sites are maintained by five President's Emergency Plan for AIDS Relief (PEPFAR) programs. The primary objective of AFRICOS is to assess the impact of clinical practices, biological and socio-behavioral factors on HIV infection and disease progression in an African context. AFRICOS began enrollment in January 2013. The primary objective of the parent study, AFRICOS, is descriptive, and the hypotheses tested will be exploratory. Therefore, the enrollment targets for AFRICOS were determined by the relative size of each PEPFAR Program, research capacity at each site, and available resources.
Since 2013, AFRICOS has enrolled individuals aged 18 years or older with and without HIV, in an approximate 5:1 ratio. Participants living with HIV were invited from clinical site patient lists to participate in the study by random selection stratified by gender and ART status. PLWH were selected from current HIV clinic client lists, with the number of participants reflective of the proportion of PLWH observed in the clinic population. A small proportion (less than 9%) [42] were recruited from other HIV studies conducted locally. PLWH were eligible for AFRICOS if they were at least 18 years old, consented to data and specimen collection, and had ongoing receipt of HIV care at the enrolling clinical site. Notably, AFRICOS began to enroll 15- to 17-year-old participants in January 2020, but since this analysis only includes data up to February 2020, these participants are not included in this analysis. PLWH are selected to proportionally reflect the ratio of females to males and the ratio of participants on ART to those not on ART (current ART status at screening/enrollment) at each of the PEPFAR sites. This is accomplished through the use of clinic registries, and randomization is conducted in SAS (SAS Institute, Cary, North Carolina). Minimum viral load results at enrollment/baseline were not considered for randomization Participants are seen once every six months during their participation. Individuals who were pregnant at enrollment were excluded from AFRICOS but women who became pregnant during participation continued enrollment and were included in the cohort. Participants in previous PEPFAR vaccine, therapeutic and cohort studies at locations where AFRICOS enrollment occurs were eligible for enrollment into AFRICOS. Furthermore, enrollment in AFRICOS does not preclude enrollment into future vaccine, therapeutic or cohort studies. For this analysis, we examined the prospective relationship between pregnancy, depressive symptoms, HIV viral non-suppression, and child outcomes among WLWH. Participants were eligible for the present analysis if they were enrolled between January 2013 and February 2020 and reported a birth during the study period.
Data Collection
Participants completed a medical history and physical examination, demographic and behavior questionnaire, and underwent phlebotomy at every visit. Enrolled participants were seen at study clinical sites once every six months. They were offered ART and prenatal care per each country’s national guidelines. Data are captured on paper case report forms and then entered and verified in the ClinPlus platform (Anju Software, Tempe, AZ). Data are stored on a secure server located at the U.S. Military HIV Research Program headquarters.
Demographics
Participant age, gender, and obstetric history were determined through chart review. Participant household income (i.e., “What is your household’s total income per week?”) and food insecurity (i.e., “Have you had enough food to eat over the past 12 months?”) were determined through subject questionnaires.
Household Income
Household income was reported at baseline via self-report. We converted the household incomes into Purchasing Power Parity (PPP) values for comparability. First, we converted local currency into USD for the year that the income was reported [43]. Then we multiplied by the price level ratio of PPP conversion factor (GDP) to market exchange rate for each country as reported by the World Bank for the respective year reported [44].
Perinatal Period
For our analysis we defined three phases: (1) pre-conception (52 weeks prior to estimated date of conception), (2) pregnancy (length of pregnancy in weeks), and (3) postpartum (52 weeks following birth). We selected these periods based on recognition that perinatal mood disorders are now defined as occurring in pregnancy and the 12 months postpartum [45,46,47]. Pregnancy was defined as the duration of gestational age of the baby in weeks. If gestational age was missing it was estimated to be 40 weeks since most births occur between 38 and 42 weeks [48]. Timepoints outlining these three time periods were calculated using the date of birth (DOB) of the baby and gestational age. DOB was recorded by chart review. If DOB was missing but age of child was reported at a subsequent visit, we backdated the age of the child from the visit date to estimate DOB. If no subsequent visit or DOB was recorded, the DOB was estimated to be the visit date that the mother first reported the birth outcome.
Depressive Symptoms
Depressive symptoms were evaluated using the Center for Epidemiologic Studies Depression (CES-D) scale [49], which was translated into Luganda, Luo, Pidgin English, and Kiswahili and performed as part of an interviewer-administered questionnaire. This scale has been previously validated among pregnant WLWH and HIV-uninfected pregnant women in Uganda [50]. The scale has also been validated among other populations in Uganda [51], Kenya [52], and Tanzania [52]. For this analysis, elevated depressive symptoms were defined as a CES-D score ≥ 16 and were our primary exposure. We also considered highly elevated depressive symptoms (CES-D ≥ 20) in secondary analyses. A cut-off score of 20 has been suggested as an optimal threshold for detection of major depression, minor depression, and dysthymia [53]. In our analysis, elevated or highly elevated depressive symptoms during a phase of the perinatal period were defined as at least one CES-D score above 16 or 20, respectively, during that phase. For example, if a participant had a score of 17 (elevated depressive symptoms) at one visit during the pre-conception phase, and a score of 8 (not elevated depressive symptoms) at the next visit during the same phase, the participant would be counted as having elevated depressive symptoms during the pre-conception phase. We also conducted secondary analyses where we defined elevated depressive symptoms as CES-D ≥ 10 [54].
Viral Load
Viral loads (plasma HIV RVA levels) were measured using the on-site, Roche COBAS® Taqman® HIV-1 or Abbott RealTime HIV-1 Viral Load assays. AFRICOS sites running viral load tests were all enrolled in external quality assessment (EQA); the EQA providers vary by site, typically with 2 to 3 testing cycles per year. All panel members are run and analyzed in the same manner as patient samples. Results are submitted to the EQA Provider and graded by the provider inclusive of peer review, and final report returned to site. The site reviews the final report for acceptability, monitors, tracks, and in cases of unacceptable results, completes an investigation along with corrective and preventative actions as needed. For the primary analysis, viral non-suppression was defined as a viral load of ≥ 200 copies per milliliter of blood. Viral non-suppression for a phase of the perinatal period was defined as at least one viral non-suppression result during that phase. We used 200 copies/ml as our cutoff to be in alignment with the Center for Disease Control and Prevention (CDC) definition of viral non-suppression [55] and to remain consistent with literature on conservative estimates of viral non-suppression among pregnant women [56, 57].
Birth Outcome and Gestational Age
Birth outcome data was collected through medical record chart review at each clinical site. Since data was recorded every 6 months, the same birth outcome could be reported at consecutive visits. In cases where the same birth was reported at multiple visits, data was merged to capture as many variables about a single birth as possible.
Gestational age data was collected via chart review and reported in units of days, weeks, or months. For analysis, all gestational ages were converted to gestational weeks. Where gestational age was not reported or missing, gestational weeks was assumed to be full term (40 weeks) for live births and still births and 20 weeks for spontaneous abortions or miscarriages.
Preterm birth is defined by WHO as babies born alive before 37 weeks of pregnancy are completed (through 37 weeks 6 days) [58]. For this analysis, “full-term” was defined as live births with a gestational age of greater than 37 completed weeks. “Moderate-to-late preterm” is defined as born between 32 and 36 completed weeks of pregnancy. “Very preterm” is defined as born at less than 32 weeks of pregnancy [58]. Other birth outcomes reported were stillbirths or spontaneous abortions and are referred to as pregnancy loss in this analysis. Birth outcomes were categorized as binary variables of (a) alive and full term or (b) pre-term or pregnancy loss.
Statistical Analysis
We used descriptive statistics (frequencies, medians) to summarize demographic information among participants and the frequency of elevated depressive symptoms, viral non-suppression, and birth outcomes during the study period. Our baseline descriptive statistics used the total number of participants as the denominator. Other descriptive statistics use the total number of pregnancies as the denominator.
For our primary analysis, we were interested in exploring the effect of depressive symptoms (CES-D ≥ 16) on viral non-suppression (viral load ≥ 200 copies/ml) in WLWH who ever had a pregnancy during participation in AFRICOS. To answer this question, we constructed a visit-level dataset where each visit during a women’s perinatal period represented a unique record. We used generalized estimating equations (GEE) to model the association between depressive symptoms and viral non-suppression during the perinatal period. We fit the model using a logistic link, binomial distribution, and robust standard errors to estimate odds ratios while accounting for repeated measures over time and correlated demographic and behavioral data among a subset of mothers who were included more than once because they reported multiple births in the cohort. We included pregnancy phase (preconception, pregnancy, or postpartum), study site, and gravida a priori in our regression models. We also explored confounding by several additional covariates hypothesized to have a relationship with depressive symptoms and viral non-suppression, including literacy, food insecurity, PPP, highest education level, ARV medication type (EFV and/or NVP), and country. EFV and NVP medication types have been associated with depressive symptoms and suicidal ideation in previous studies [59, 60]. Our multivariable model included those covariates that we identified to be statistically significantly associated with viral non-suppression (any baseline factors associated with viral non-suppression with p-value < 0.10 were included in the multivariable models). Retrospective power calculations estimated the power based on the sample size, 0.05 Type I error rate, and odds ratios of viral non-suppression by depressive symptom status [61].
In addition to this primary analysis, we conducted several sensitivity analyses by altering our exposure and outcome definitions and sample selection criteria for our GEE models. Specifically, these sensitivity analyses included: (1) using self-reported ART adherence as our outcome variable in place of viral non-suppression, with any self-reported missed doses in the past one month categorized as non-adherence; (2) using a CES-D score of ≥ 10 as our exposure variable to capture a more sensitive depressive symptom measurement; (3) using a CES-D score of ≥ 20 as our exposure variable to capture a more specific depressive symptom measurement; and (4) restricting the analysis to mothers who had live births. In the second and third sensitivity analyses, we included a lower and higher threshold for elevated depressive symptoms to evaluate a dose–response relationship between our primary predictor (depressive symptoms) and outcome (viral non-suppression). We expected to see a smaller and higher magnitude of associations for the lower and higher thresholds, respectively.
We were also interested in exploring the associations between depressive symptoms, viral non-suppression, and birth outcomes. For this analysis, a birth-level dataset was used to run logistic regressions for depressive symptoms, viral non-suppression, and birth outcome. Analyses were conducted using SPSS (IBM Corp. Released 2020. IBM SPSS Statistics for Windows, Version 27.0. Armonk, NY: IBM Corp).
Ethical Consideration
All participants provided written informed consent. The institutional review boards of the Walter Reed Army Institute of Research, Makerere University School of Public Health, Kenya Medical Research Institute, Tanzania National Institute of Medical Research, and Nigerian Ministry of Defense approved the study. This analysis was conducted using an anonymized dataset.
Results
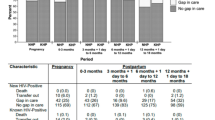
From January 2013 to February 2020, 1722 WLWH were enrolled in the AFRICOS study. Of WLWH, 248 (14.4%) had at least one pregnancy after enrollment; these 248 women reported 291 total pregnancies. One woman (0.4%) recorded four pregnancies, four women (1.6%) recorded three pregnancies, 32 women (12.9%) recorded two pregnancies, and 211 women (85.1%) recorded one pregnancy. The majority of women lived in Kenya (44.8%), followed by Uganda (25.4%), Nigeria (17.3%), and Tanzania (12.5%). Most women were married or living with their partner (61.7%) and the median number of previous pregnancies was 4. About 50% of the women had completed primary school and just over one third had completed secondary school (34.3%). There were 50 pregnancy losses comprising 42 spontaneous abortions and 8 stillbirths. One child (0.3%) was confirmed to have acquired HIV through vertical transmission, 68 children (23.4%) were confirmed HIV-uninfected, and 222 children (76.3%) had an unknown or not reported HIV status at the time of chart review. Approximately 21.0% of women had depressive symptoms at their enrollment visit (Table 1).
A total of 106 women (36.4% of all 291 pregnancies) completed all study visits during their perinatal period (5 or 6 visits depending on pregnancy duration and visit timing), 108 women (37.1%) missed 1 study visit, 58 women (19.9%) missed 2 study visits, 17 women (5.8%) missed 3 study visits, and 2 women (0.7%) missed 4 study visits. Among women who did not miss their visit, only one did not have a CESD reported at their visit (postpartum) and 19 were missing a viral load result at their visit (4 in pre-conception, 1 in pregnancy, and 14 in postpartum). Due to missed visits and incomplete data at study visits, a total of 81.1% of women had a CES-D score and 79.4% of women had a viral load value for all perinatal periods. DOB was missing for 127 children (43.6%) and of these children, 63 (49.6%) had a reported age at the study visit which allowed us to estimate their DOB. Sixty-four children (22.0%) were missing both DOB and estimated age. Only 17 children (5.8%) were missing their gestational age at birth. Gestational age was missing for two live births, four still births, and 11 spontaneous abortions or miscarriages.
Associations Between Depressive Symptoms and Viral Non-suppression
A total of 1263 participant visits were included in the analysis of associations between depressive symptoms and viral non-suppression during the perinatal period. Elevated depressive symptoms (CES-D ≥ 16) were reported at least once among 61 (21.0%) of the 291 pregnancies. Of those who reported depressive symptoms, 45 (74%) had elevated symptoms at one visit, 12 (20%) had elevated symptoms at two visits, 3 (5%) had elevated symptoms at three visits, and 1 (2%) had elevated symptoms at four visits during the period.
Throughout the 1-year pre-conception phase, 39 women (13.4%) had elevated, and 25 women (8.6%) had highly elevated depressive symptoms. During pregnancy, 22 women (7.6%) had elevated, and 9 women (3.1%) had highly elevated depressive symptoms. For 1 year postpartum, 16 women (5.5%) had elevated, and 13 women (4.5%) had highly elevated depressive symptoms (Fig. 1). A total of 93 women (32.0%) were virally non-suppressed at least once during one-year pre-conception, 57 women (19.6%) during pregnancy, and 26 women (8.9%) during one-year postpartum.
In our primary, visit-level, multivariable analysis, elevated depressive symptoms (CES-D ≥ 16) were associated with an increased odds of viral non-suppression compared to participants with lower symptom scores, after adjusting for perinatal period (aOR 2.2; 95% confidence interval [CI] 1.2–4.0, p = 0.011) (Table 2). The pre-conception and pregnancy phases of the perinatal period were also associated with an increased odds of viral non-suppression when compared to the post-partum phase (aOR 4.7 and 2.7, respectively; 95% CI 3.1–7.3 and 1.8–4.3, p ≤ 0.001 and < 0.001, respectively). In our sensitivity analysis, the association between elevated depressive symptoms and non-adherence was of a similar magnitude and direction, although we were only able to assess unadjusted associations in this analysis due to small numbers of poor adherence and elevated depressive symptoms (OR 2.0; 95% CI 1.0–3.9, p = 0.06). Additional sensitivity analyses with cutoffs of CES-D ≥ 10 and CES-D ≥ 20 also resulted a statistically significant association between depressive symptoms and viral non-suppression (CES-D ≥ 10 aOR 2.1; 95% CI 1.3–3.3, p < 0.01; CES-D ≥ 20 aOR 2.4; 95% CI 1.2–4.5, p = 0.01). Among only those mothers who had a live birth, depressive symptoms were associated with greater odds of viral non-suppression, although this association was not statistically significant (aOR 1.7; 95% CI 1.0–3.1, p = 0.07). Based on this sample size, we had 89% power to detect an OR of 2.1 in our unadjusted GEE analysis.
Associations Between Depressive Symptoms, Viral Non-suppression and Birth Outcomes
Our second objective was to explore the relationships between depressive symptoms, viral non-suppression, and birth outcomes throughout the perinatal period in a series of unadjusted, participant-level, exploratory analyses (Fig. 2). Among women who had a live birth, viral non-suppression during pregnancy may be associated with greater odds of pre-term birth (OR 2.6; 95% CI 1.0–6.7; p = 0.05), although this association was not statistically significant at α = 0.05 (Table 3). Among all women who were pregnant, viral non-suppression during pregnancy was significantly associated with depression during the postpartum phase (OR 3.2; 95% CI 1.1–9.7, p = 0.04).
Discussion
Among WLWH who became pregnant during their participation in the AFRICOS cohort, approximately one fifth had elevated depressive symptoms (CES-D ≥ 16) at any point during their perinatal period, though few women, overall, had depressive symptoms at consecutive visits during their perinatal period. We found that, in the perinatal period, elevated depressive symptom levels were associated with doub1le the odds of viral non-suppression. This finding was robust to a number of sensitivity analyses including varying exposure definitions of depressive symptom severity, using non-adherence rather than viral non-suppression, and restricting to women who had a live birth. When we looked at timing of viral non-suppression and depression through the perinatal periods, we found that viral non-suppression in pregnancy was significantly associated with depressive symptoms postpartum. These findings have important implications for improving HIV and mental health care of women and timing of interventions.
The prevalence of depressive symptoms in this sample is lower than that reported in other studies of perinatal depression among HIV-positive women [20,21,22,23]. Studies using similar measures for depression among perinatal WLWH have found prevalence between 25% [62] and 50% [63, 64]. Meta-analyses of depression among perinatal WLWH found an average depression prevalence of 44% [21] and 36% [20]. Few WLWH in our sample had depressive symptoms throughout the perinatal period and, consistent with other studies, depressive symptoms were most prevalent during pre-conception and decreased by the postpartum period [20, 21]. There are several potential reasons for the lower prevalence of depressive symptoms observed in our study. First, the time since HIV diagnosis was longer among WLWH in this study—nearly 4 years—than among cohorts reported in the literature. This could have contributed to better HIV symptom control due to length of time since first ART prescription [65, 66] and lower risk of mental distress associated with recent diagnosis [67,68,69]. While some studies found higher rates of positive depression screening scores for women diagnosed with HIV during pregnancy [70]; the women included in the current study were engaged in HIV care prior to becoming pregnant. Second, the population in this analysis reported low rates of risk factors associated with perinatal depression—interpersonal violence (12%), poor literacy (12%) and never being married (20%)—which could have contributed to the low prevalence of depression [71]. Finally, pregnancy and children can be a motivator for treating depression [72], and adherence to ART improves among mothers who know their status before becoming pregnant [73]. The support structure of dedicated clinical HIV care could have positively influenced the participants’ risk of depression and detectable viral load. However, despite existing clinical support through participation in AFRICOS, depressive symptoms were associated with viral non-suppression.
Previous studies have found similar associations of depressive symptoms increasing risk for ART non-adherence or viral non-suppression, [28, 74, 75] but to our knowledge none has looked at this association across the perinatal period. For example, a previous analysis of the AFRICOS cohort showed that depressive symptoms reduced odds of ART adherence in adults (OR 0.59, p = 0.01) [40]. Another study of WLWH in Tanzania found that women with depression had 1.94 times the risk of viral non-suppression after 6 months of treatment, compared to women who had no depression [75]. We expected that our sensitivity analyses using a higher cut-off would result in a stronger magnitude of association between depressive symptoms and viral non-suppression [76]. Consistent with these hypotheses, we found twice the odds of viral non-suppression among mothers with the higher score indicating highly elevated depressive symptoms, strengthening our confidence in the association between depressive symptoms and viral non-suppression in this population. We also found that restricting the cohort to only mothers who had a live birth resulted in a weaker association (aOR 1.7; 95% CI 1.0–3.1, p = 0.07) between depressive symptoms and viral non-suppression, suggesting that poor outcomes of higher viral load, depression, and pregnancy loss may cluster together.
There are several biological and behavioral mechanisms that could explain our findings. Biologically, depression can alter the function of the body’s immune response and lead to an increase in viral load [28, 29]. Additionally, depression can increase risk of viral non-suppression through behavior changes that reduce ART adherence [26, 77,78,79], co-occurring alcohol use, and through poor social support [26, 79]. The emotional and behavioral effects of depression, including feelings of hopelessness, limited social interactions, and lack of motivation, can reduce adherence to ART [77, 79]. Our sensitivity analysis found increased, although not significant, odds of non-adherence among perinatal women with depressive symptoms (OR 2.0, p = 0.06). A previous study of pregnant women in PMTCT care in South Africa found that elevated depressive symptoms were directly associated with significantly lower adherence to ART [26]. Additional research is needed to assess the relative contribution of these mechanisms to the outcomes we observe.
We found that women who were virally non-suppressed had more than twice the odds of a pre-term birth in exploratory unadjusted analyses. Previous studies have found that pregnant women experiencing depression are up to 40% more likely to have a preterm birth, a relationship that is stronger in low- and middle-income countries [80,81,82]. Another study in Kenya found that risk of preterm birth was 3.6 times higher among pregnant women with depressive symptoms [83]. Moreover, WLWH are known to be more likely to have a preterm birth or baby with low birthweight than HIV-negative women [84,85,86]. One study in Botswana showed that pregnant women continuing highly active ART from before pregnancy had higher odds (aOR 1.4) of preterm delivery, compared to women who started ART in pregnancy after adjusting for maternal hypertension and anemia [87]. We also found significantly higher odds of elevated depressive symptoms postpartum among women who had viral non-suppression in their pregnancy. Previous studies have found that viral suppression is associated with a reduced odds of depression symptom severity among pregnant and postpartum women (aOR 0.45) [88]. One meta-analysis showed significantly increased odds of postpartum depressive symptoms among WLWH compared to women without HIV (OR 1.58) [20]. Biologically, indoleamine 2,3-dioxygenase-1 (IDO) is an enzyme that is induced both in HIV infection and post-partum depression and stimulates tryptophan catabolism, contributing to decreased T-cell proliferation and depletion of serotonin–factors that can lead to viral non-suppression and depressive symptoms [89]. Further research is needed to understand this relationship in more detail, including analyses with large sample sizes which would allow for mediation analyses using marginal structural models.
The 2018 Lancet Commission on strengthening the global HIV response highlighted the need to integrate HIV and other health care delivery [6]. The integration of mental health and HIV care is critical to ensure the wellbeing of WLWH and the health of children born to them. This study has several implications for policy and clinical intervention. Our robust findings of twice the odds of viral non-suppression among women with depressive symptoms during the perinatal period supports the inclusion of screening and care for mental disorders for pregnant women, women planning to become pregnant, and women of reproductive potential in general. Timing of screening and intervention is also an important consideration, as we found significant relationships between viral non-suppression and depressive symptoms from pregnancy through postpartum. Low adherence to ART and high viral load among pregnant WLHV who have depressive symptoms can increase risk of vertical transmission for pregnant mothers [77, 90]. The findings of this analysis support a growing body of research that advocates for the integration of mental health and HIV care programs to support WLWH of childbearing age. [91]. Several integrated mental health and adherence interventions (i.e. Life Steps) [92] have shown improvements in both depressive symptoms and adherence, but few have been implemented among pregnant populations [93]. The perinatal period, with multiple antenatal and child care visits, presents a unique opportunity to screen for and treat mental health conditions [94]. Integration of screening and care for mental health conditions can strengthen HIV prevention and care outcomes [1] in addition to perinatal mental health disorder treatments and ultimately support improved maternal and child outcomes [91].
A number of limitations of this analysis should be considered. First, pregnancy-related variables were all collected through chart review abstraction, and we were limited by the availability and quality of data. Data on antidepressant medication is likely incomplete and therefore could not be included as a covariate in our models. Antidepressant use, if data were available, would be a confounding factor in examining the association of prenatal depression with pregnancy outcome such as preterm birth. Accurate adjustment for this factor may decrease the strength of our association. In our analysis, there may be unmeasured confounders of the relationship between depression and viral non-suppression. Both depression and viral load are influenced by gender-based violence, empowerment, stigma, and other factors that were not measured in AFRICOS [95,96,97,98]. Additionally, pregnancy intention data was not recorded in this cohort study and unintended pregnancy is associated with transient elevated depression symptomatology [99]. We were unable to adjust for non-nucleoside reverse transcriptase inhibitors (NNRTIs) for HIV treatment (efavirenz, nevirapine) that have been associated with depressive symptoms and suicidal ideation [59], since most women (86%) were on an EFV/NVP regimen. Additionally, women in this study had clinic visits once every six months and were asked about their depressive symptoms for the previous two weeks. Therefore, we may not capture women who only experienced immediate postpartum depressive symptoms. However, there is growing evidence that perinatal depression is present throughout pregnancy and the year postpartum, beyond the first 6 weeks [45,46,47]. Finally, we are unable to draw conclusions about the causal relationship between depression and viral load from this analysis since we cannot rule out the potential bidirectional relationship, and we have identified several unmeasured and time-varying confounding factors. Additionally, in our secondary analysis we had few outcomes of elevated depressive symptoms and viral non-suppression at most time points, limiting our ability to explore causal pathways. Future work is needed to explore the temporality of these associations. Despite these limitations, our findings on the association between depressive symptoms and viral non-suppression were consistent across multiple sensitivity analyses modifying the analysis exposure, outcome, and population definitions. There are also several strengths to this analysis. We found high statistical power to detect the effect in our primary analysis. We included WLWH from a variety of countries and sites within countries, increasing potential generalizability of findings. The study followed women throughout each stage of the perinatal period with regular depression measurements and validated depression scales for HIV-positive pregnant women. High retention in the cohort through the perinatal stages reduced the risk of bias. Also, while most previous studies have looked at the association between depressive symptoms and HIV treatment outcomes using ART adherence measures as an outcome [78], our analysis utilized regularly collected viral load data as a clinical outcome. Finally, we also included a clear definition of the perinatal period and included the preconception period, which is rarely included in studies of the perinatal period.
Conclusion
Our analysis showed an increased odds of viral non-suppression associated with depressive symptoms among perinatal women living with HIV. Future research is needed to further explore this relationship with a larger sample size and including a wider array of maternal and child clinical outcomes. These findings accentuate the need for screening and treatment of pregnant women with depressive symptoms in HIV care settings which has the potential to improve HIV, perinatal mental health, as well as birth outcomes.
Data Availability (Data Transparency)
The Henry M. Jackson Foundation for the Advancement of Military Medicine (HJF) and the Water Reed Army Institute of Research (WRAIR) are committed to safeguarding the privacy of research participants. Distribution of data will require compliance with all applicable regulatory and ethical processes, including establishment and approval of an appropriate data-sharing agreement. To request a minimal data set, please contact the data coordinating and analysis center (DCAC) at PubRequest@hivresearch.org and indicate the RV329 study along with the name of the manuscript.
Code Availability (Software Application or Custom Code)
Data analysis code can be made available upon request.
References
UNAIDS. 2020 Global AIDS Update—Seizing the moment Tackling entrenched inequalities to end epidemics. Geneva, Switzerland: Joint United Nations Programme on HIV/AIDS; 2020. https://www.unaids.org/sites/default/files/media_asset/2020_global-aids-report_en.pdf
Kaida A, Laher F, Strathdee SA, Janssen PA, Money D, Hogg RS, et al. Childbearing intentions of HIV-positive women of reproductive age in Soweto, South Africa: the influence of expanding access to HAART in an HIV hyperendemic setting. Am J Public Health. 2011;101:350–8.
Li H, Liu J, Tan D, Huang G, Zheng J, Xiao J, et al. Maternal HIV infection and risk of adverse pregnancy outcomes in Hunan province, China: a prospective cohort study. Medicine. 2020;99: e19213.
Malaba TR, Phillips T, Le Roux S, Brittain K, Zerbe A, Petro G, et al. Antiretroviral therapy use during pregnancy and adverse birth outcomes in South African women. Int J Epidemiol. 2017;46:1678–89.
Chetty T, Thorne C, Coutsoudis A. Preterm delivery and small-for-gestation outcomes in HIV-infected pregnant women on antiretroviral therapy in rural South Africa: results from a cohort study, 2010–2015. PLoS ONE. 2018;13: e0192805.
Bekker L-G, Alleyne G, Baral S, Cepeda J, Daskalakis D, Dowdy D, et al. Advancing global health and strengthening the HIV response in the era of the Sustainable Development Goals: the International AIDS Society-Lancet Commission. Lancet. 2018;392:312–58.
Tanser F, Bärnighausen T, Grapsa E, Zaidi J, Newell M-L. High coverage of ART associated with decline in risk of HIV acquisition in rural KwaZulu-Natal, South Africa. Science. 2013;339:966–71.
Reynolds SJ, Makumbi F, Nakigozi G, Kagaayi J, Gray RH, Wawer M, et al. HIV-1 transmission among HIV-1 discordant couples before and after the introduction of antiretroviral therapy. AIDS. 2011;25:473–7.
Ferguson L, Grant AD, Watson-Jones D, Kahawita T, Ongech JO, Ross DA. Linking women who test HIV-positive in pregnancy-related services to long-term HIV care and treatment services: a systematic review. Trop Med Int Health. 2012;17:564–80.
Ramjee G, Daniels B. Women and HIV in sub-Saharan Africa. AIDS Res Therapy. 2013;10:1–9.
Karim SSA, Baxter C. HIV incidence rates in adolescent girls and young women in sub-Saharan Africa. Lancet Global Health. 2019;7:e1470–1.
Woldesenbet S, Kufa-Chakezha T, Lombard C, Manda S, Cheyip M, Ayalew K, et al. Recent HIV infection among pregnant women in the 2017 antenatal sentinel cross-sectional survey, South Africa: assay-based incidence measurement. PLoS ONE. 2021;16:e0249953.
Ndege S, Washington S, Kaaria A, Prudhomme-O’Meara W, Were E, Nyambura M, et al. HIV prevalence and antenatal care attendance among pregnant women in a large home-based HIV counseling and testing program in Western Kenya. PLoS ONE. 2016;11:e0144618.
UNAIDS. UNAIDS Report on the Global HIV/AIDS Epidemic 2008. Geneva, Switzerland: Joint United Nations Programme on HIV/AIDS (UNAIDS); 2008.
Rubio EV, Gahona RG. Vertical Transmission of HIV—Medical Diagnosis, Therapeutic Options and Prevention Strategy. In: Okechukwu IB, editor. Trends in Basic and Therapeutic Options in HIV Infection. Rijeka: Intech; 2015. p. 51.
Ngocho JS, Watt MH, Minja L, Knettel BA, Mmbaga BT, Williams PP, et al. Depression and anxiety among pregnant women living with HIV in Kilimanjaro region, Tanzania. PLoS ONE. 2019;14: e0224515.
Nyamukoho E, Mangezi W, Marimbe B, Verhey R, Chibanda D. Depression among HIV positive pregnant women in Zimbabwe: a primary health care based cross-sectional study. BMC Pregnancy Childbirth. 2019;19:1–7.
Wingood GM, Reddy P, Peterson SH, DiClemente RJ, Nogoduka C, Braxton N, et al. HIV stigma and mental health status among women living with HIV in the Western Cape, South Africa. S Afr J Sci. 2008;104:237–40.
Wingood GM, DiClemente RJ, Mikhail I, McCree DH, Davies SL, Hardin JW, et al. HIV discrimination and the health of women living with HIV. Women Health. 2007;46:99–112.
Zhu Q-Y, Huang D-S, Lv J-D, Guan P, Bai X-H. Prevalence of perinatal depression among HIV-positive women: a systematic review and meta-analysis. BMC Psychiatry. 2019;19:330.
Sowa NA, Cholera R, Pence BW, Gaynes BN. Perinatal depression in HIV-infected African women: a systematic review. J Clin Psychiatry. 2015;76:1385–96.
Rochat TJ, Tomlinson M, Newell M-L, Stein A. Detection of antenatal depression in rural HIV-affected populations with short and ultrashort versions of the Edinburgh Postnatal Depression Scale (EPDS). Arch Womens Ment Health. 2013;16:401–10.
Levine AB, Aaron EZ, Criniti SM. Screening for depression in pregnant women with HIV infection. J Reprod Med. 2008;53:352–6.
Onono M, Odwar T, Abuogi L, Owuor K, Helova A, Bukusi E, et al. Effects of depression, stigma and intimate partner violence on postpartum women’s adherence and engagement in HIV care in Kenya. AIDS Behav. 2019;24:1807–15.
de Lemos LMD, Lippi J, Rutherford GW, Duarte GS, Martins NGR, Santos VS, et al. Maternal risk factors for HIV infection in infants in northeastern Brazil. Int J Infect Dis. 2013;17:e913–8.
Psaros C, Smit JA, Mosery N, Bennett K, Coleman JN, Bangsberg DR, et al. PMTCT adherence in pregnant South African Women: the role of depression, social support, stigma, and structural barriers to care. Ann Behav Med. 2020. https://doi.org/10.1093/abm/kaaa005/5775771.
Sturt AS, Dokubo EK, Sint TT. Antiretroviral therapy (ART) for treating HIV infection in ART-eligible pregnant women. Cochrane Database Syst Rev. 2010. https://doi.org/10.1002/14651858.CD008440.
Evans DL, Ten Have TR, Douglas SD, Gettes DR, Morrison M, Chiappini MS, et al. Association of depression with viral load, CD8 T lymphocytes, and natural killer cells in women with HIV infection. Am J Psychiatry. 2002;159:1752–9.
Cruess DG, Douglas SD, Petitto JM, Have TT, Gettes D, Dubé B, et al. Association of resolution of major depression with increased natural killer cell activity among HIV-seropositive women. Am J Psychiatry. 2005;162:2125–30.
Passchier RV, Abas MA, Ebuenyi ID, Pariante CM. Effectiveness of depression interventions for people living with HIV in Sub-Saharan Africa: a systematic review & meta-analysis of psychological & immunological outcomes. Brain Behav Immun. 2018;73:261–73.
Greeson JM, Gettes DR, Spitsin S, Dubé B, Benton TD, Lynch KG, et al. The selective serotonin reuptake inhibitor citalopram decreases human immunodeficiency virus receptor and coreceptor expression in immune cells. Biol Psychiatry. 2016;80:33–9.
Xiao P-L, Zhou Y-B, Chen Y, Yang M-X, Song X-X, Shi Y, et al. Association between maternal HIV infection and low birth weight and prematurity: a meta-analysis of cohort studies. BMC Pregnancy Childbirth. 2015. https://doi.org/10.1186/s12884-015-0684-z.
Momplaisir F, Hussein M, Kacanek D, Brady K, Agwu A, Scott G, et al. Perinatal depressive symptoms, human immunodeficiency virus (HIV) suppression, and the underlying role of antiretroviral therapy adherence: a longitudinal mediation analysis in the IMPAACT P1025 cohort. Clin Infect Dis. 2021;73:1379–87.
Jones DL, Rodriguez VJ, Soni Parrish M, Kyoung Lee T, Weiss SM, Ramlagan S, et al. Maternal and infant antiretroviral therapy adherence among women living with HIV in rural South Africa: a cluster randomised trial of the role of male partner participation on adherence and PMTCT uptake. SAHARA J. 2021;18:17–25.
Lin D, Zhang C, Shi H. Adverse impact of intimate partner violence against HIV-positive women during pregnancy and post-partum: results from a meta-analysis of observational studies. Trauma Violence Abuse. 2022. https://doi.org/10.1177/15248380211073845.
Phillips T, Brittain K, Mellins CA, Zerbe A, Remien RH, Abrams EJ, et al. A self-reported adherence measure to screen for elevated HIV viral load in pregnant and postpartum women on antiretroviral therapy. AIDS Behav. 2017;21:450–61.
Phillips TK, Wilson IB, Brittain K, Zerbe A, Mellins CA, Remien RH, et al. Decreases in self-reported ART adherence predict HIV viremia among pregnant and postpartum South African women. J Acquir Immune Defic Syndr. 2019;80:247–54.
Sidibé M, Loures L, Samb B. The UNAIDS 90–90–90 target: a clear choice for ending AIDS and for sustainable health and development. J Int AIDS Soc. 2016;19:1.
Esber A, Polyak C, Kiweewa F, Maswai J, Owuoth J, Maganga L, et al. Persistent low-level viremia predicts subsequent virologic failure: is it time to change the third 90? Clin Infect Dis. 2019;69:805–12.
Meffert SM, Neylan TC, McCulloch CE, Maganga L, Adamu Y, Kiweewa F, et al. East African HIV care: depression and HIV outcomes. Global Mental Health. 2019. https://doi.org/10.1017/gmh.2019.6.
African Cohort Study (AFRICOS). MHRP. https://www.hivresearch.org/pepfar/african-cohort-study-africos accessed 28 Apr 28 2022.
Ake JA, Polyak CS, Crowell TA, Kiweewa F, Semwogerere M, Maganga L, et al. Noninfectious comorbidity in the African cohort study. Clin Infect Dis. 2019;69:639–47.
Official exchange rate (LCU per US$, period average) - Nigeria, Kenya, Uganda, Tanzania | Data. https://data.worldbank.org/indicator/PA.NUS.FCRF?end=2019&locations=NG-KE-UG-TZ&start=2013 accessed 7 Dec 2020.
Price level ratio of PPP conversion factor (GDP) to market exchange rate - Nigeria, Kenya, Uganda, Tanzania | Data. https://data.worldbank.org/indicator/PA.NUS.PPPC.RF?locations=NG-KE-UG-TZ accessed 7 Dec 2020.
Woody CA, Ferrari AJ, Siskind DJ, Whiteford HA, Harris MG. A systematic review and meta-regression of the prevalence and incidence of perinatal depression. J Affect Disorders. 2017;219:86–92.
Mangla K, Hoffman MC, Trumpff C, O’Grady S, Monk C. Maternal self-harm deaths: an unrecognized and preventable outcome. Am J Obst Gynecol. 2019;221:295–303.
Goodman JH. Postpartum depression beyond the early postpartum period. J Obstet Gynecol Neonatal Nurs. 2004;33:410–20.
Chawanpaiboon S, Vogel JP, Moller A-B, Lumbiganon P, Petzold M, Hogan D, et al. Global, regional, and national estimates of levels of preterm birth in 2014: a systematic review and modelling analysis. Lancet Global Health. 2019;7:e37-46.
Radloff LS. The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1:385–401.
Natamba BK, Achan J, Arbach A, Oyok TO, Ghosh S, Mehta S, et al. Reliability and validity of the center for epidemiologic studies-depression scale in screening for depression among HIV-infected and -uninfected pregnant women attending antenatal services in northern Uganda: a cross-sectional study. BMC Psychiatry. 2014;14:303.
Akena D, Joska J, Obuku EA, Stein DJ. Sensitivity and specificity of clinician administered screening instruments in detecting depression among HIV-positive individuals in Uganda. AIDS Care. 2013;25:1245–52.
Kilburn K, Prencipe L, Hjelm L, Peterman A, Handa S, Palermo T. Examination of performance of the Center for Epidemiologic Studies Depression Scale Short Form 10 among African youth in poor, rural households. BMC Psychiatry. 2018;18:201.
Julian LJ, Gregorich SE, Tonner C, Yazdany J, Trupin L, Criswell LA, et al. Using the Center for Epidemiologic Studies Depression Scale to screen for depression in systemic lupus erythematosus. Arthritis Care Res (Hoboken). 2011;63:884–90.
Tomita A, Labys CA, Burns JK. Depressive symptoms prior to pregnancy and infant low birth weight in South Africa. Matern Child Health J. 2015;19:2179–86.
HIV Treatment as Prevention | HIV Risk and Prevention | HIV/AIDS | CDC. https://www.cdc.gov/hiv/risk/art/index.html. 2022. Accessed 28 Apr 2022.
Lesko CR, Chander G, Moore RD, Lau B. Variation in estimated viral suppression associated with the definition of viral suppression used. AIDS. 2020;34:1519–26.
McMahon JH, Elliott JH, Bertagnolio S, Kubiak R, Jordan MR. Viral suppression after 12 months of antiretroviral therapy in low- and middle-income countries: a systematic review. Bull World Health Organ. 2013;91:377-385E.
Preterm birth [Internet]. 2018 [cited 2020 Dec 7]. https://www.who.int/news-room/fact-sheets/detail/preterm-birth. 2018. Accessed 7 Dec 2022.
Chang JL, Tsai AC, Musinguzi N, Haberer JE, Boum Y, Muzoora C, et al. Depression and suicidal ideation among HIV-infected adults receiving efavirenz versus nevirapine in Uganda. Ann Intern Med. 2018;169:146–55.
Kenedi CA, Goforth HW. A systematic review of the psychiatric side-effects of efavirenz. AIDS Behav. 2011;15:1803–18.
Test Odds Ratio Equality | Power and Sample Size Calculators | HyLown. http://powerandsamplesize.com/Calculators/Test-Odds-Ratio/Equality. Accessed 1 May 2022.
Futterman D, Shea J, Besser M, Stafford S, Desmond K, Comulada WS, et al. Mamekhaya: a pilot study combining a cognitive-behavioral intervention and mentor mothers with PMTCT services in South Africa. AIDS Care. 2010;22:1093–100.
Nöthling J, Martin CL, Laughton B, Cotton MF, Seedat S. Maternal post-traumatic stress disorder, depression and alcohol dependence and child behaviour outcomes in mother–child dyads infected with HIV: a longitudinal study. BMJ Open. 2013;3: e003638.
Mundell JP, Visser MJ, Makin JD, Kershaw TS, Forsyth BWC, Jeffery B, et al. The impact of structured support groups for pregnant south african women recently diagnosed HIV positive. Women Health. 2011;51:546–65.
Pimentel GS, Ceccato MGB, Costa JO, Mendes JC, Bonolo PF, Silveira MR. Quality of life in individuals initiating antiretroviral therapy: a cohort study. Rev Saude Publica. 2020;54:146.
Yigit I, Bayramoglu Y, Weiser SD, Johnson MO, Mugavero MJ, Turan JM, et al. Changes in internalized stigma and HIV health outcomes in individuals new to HIV care: the mediating roles of depression and treatment self-efficacy. AIDS Patient Care STDS. 2020;34:491–7.
LeMasters K, Dussault J, Barrington C, Bengtson A, Gaynes B, Go V, et al. “Pain in my heart”: understanding perinatal depression among women living with HIV in Malawi. PLoS ONE. 2020;15: e0227935.
Valente SM. Depression and HIV disease. J Assoc Nurses AIDS Care. 2003;14:41–51.
Cholera R, Pence BW, Gaynes BN, Bassett J, Qangule N, Pettifor A, et al. Depression and engagement in care among newly diagnosed HIV-infected adults in Johannesburg, South Africa. AIDS Behav. 2017;21:1632–40.
Kwalombota M. The effect of pregnancy in HIV-infected women. AIDS Care. 2002;14:431–3.
Fisher J, Cabraldeello M, Patel V, Rahman A, Tran T, Holton S, et al. Prevalence and determinants of common perinatal mental disorders in women in low- and lower-middle-income countries: a systematic review. Bull World Health Organ. 2012;90:139–49.
Rao D, Horton R, Raguram R. Gender inequality and structural violence among depressed women in South India. Soc Psychiatry Psychiatr Epidemiol. 2012;47:1967–75.
Omonaiye O, Kusljic S, Nicholson P, Manias E. Medication adherence in pregnant women with human immunodeficiency virus receiving antiretroviral therapy in sub-Saharan Africa: a systematic review. BMC Public Health. 2018;18:805.
Gokhale RH, Weiser J, Sullivan PS, Luo Q, Shu F, Bradley H. Depression prevalence, antidepressant treatment status, and association with sustained HIV viral suppression among adults living with HIV in care in the United States, 2009–2014. AIDS Behav. 2019;23:3452–9.
Regan M, Muhihi A, Nagu T, Aboud S, Ulenga N, Kaaya S, et al. Depression and viral suppression among adults living with HIV in Tanzania. AIDS Behav. 2021;25:1–9.
Lyon DE, Munro C. Disease severity and symptoms of depression in Black Americans infected with HIV. Appl Nurs Res. 2001;14:3–10.
Starace F, Ammassari A, Trotta MP, Murri R, De Longis P, Izzo C, et al. Depression is a risk factor for suboptimal adherence to highly active antiretroviral therapy. J Acquir Immune Defic Syndr. 2002;31(Suppl 3):S136-139.
Camargo CC, Cavassan NRV, Tasca KI, Meneguin S, Miot HA, Souza LR. Depression and coping are associated with failure of adherence to antiretroviral therapy among people living with HIV/AIDS. AIDS Res Hum Retroviruses. 2019;35:1181–8.
Nakimuli-Mpungu E, Bass JK, Alexandre P, Mills EJ, Musisi S, Ram M, et al. Depression, alcohol use and adherence to antiretroviral therapy in sub-Saharan Africa: a systematic review. AIDS Behav. 2012;16:2101–18.
Grote NK, Bridge JA, Gavin AR, Melville JL, Iyengar S, Katon WJ. A meta-analysis of depression during pregnancy and the risk of preterm birth, low birth weight, and intrauterine growth restriction. Arch Gen Psychiatry. 2010;67:1012–24.
Liu C, Cnattingius S, Bergström M, Östberg V, Hjern A. Prenatal parental depression and preterm birth: a national cohort study. BJOG. 2016;123:1973–82.
Premji SS, Yim IS, Dosani Mawji A, Kanji Z, Sulaiman S, Musana JW, et al. Psychobiobehavioral model for preterm birth in pregnant women in low- and middle-income countries. Biomed Res Int. 2015;2015: 450309.
Mochache K, Mathai M, Gachuno O, Vander Stoep A, Kumar M. Depression during pregnancy and preterm delivery: a prospective cohort study among women attending antenatal clinic at Pumwani Maternity Hospital. Ann Gen Psychiatry. 2018. https://doi.org/10.1186/s12991-018-0202-6.
Sukwa TY, Bakketeig L, Kanyama I, Samdal HH. Maternal human immunodeficiency virus infection and pregnancy outcome. Cent Afr J Med. 1996;42:233–5.
Leroy V, Ladner J, Nyiraziraje M, De Clercq A, Bazubagira A, Van de Perre P, et al. Effect of HIV-1 infection on pregnancy outcome in women in Kigali, Rwanda, 1992–1994. Pregnancy and HIV study group. AIDS. 1998;12:643–50.
Brocklehurst P, French R. The association between maternal HIV infection and perinatal outcome: a systematic review of the literature and meta-analysis. Br J Obstet Gynaecol. 1998;105:836–48.
Chen JY, Ribaudo HJ, Souda S, Parekh N, Ogwu A, Lockman S, et al. Highly active antiretroviral therapy and adverse birth outcomes among HIV-infected women in Botswana. J Infect Dis. 2012;206:1695–705.
Kaida A, Matthews LT, Ashaba S, Tsai AC, Kanters S, Robak M, et al. Depression during pregnancy and the postpartum among HIV-infected women on antiretroviral therapy in Uganda. J Acquir Immune Defic Syndr. 2014;67:S179–87.
Martinez P, Tsai AC, Muzoora C, Kembabazi A, Weiser SD, Huang Y, et al. Reversal of the Kynurenine pathway of tryptophan catabolism may improve depression in ART-treated HIV-infected Ugandans. J Acquir Immune Defic Syndr. 2014;65:456–62.
Mayston R, Kinyanda E, Chishinga N, Prince M, Patel V. Mental disorder and the outcome of HIV/AIDS in low-income and middle-income countries: a systematic review. AIDS. 2012;26(Suppl 2):S117-135.
Rahman A, Surkan PJ, Cayetano CE, Rwagatare P, Dickson KE. Grand challenges: integrating maternal mental health into maternal and child health programmes. PLoS Med. 2013;10:e1001442.
Safren SA, Bedoya CA, O’Cleirigh C, Biello KB, Pinkston MM, Stein MD, et al. Cognitive behavioural therapy for adherence and depression in patients with HIV: a three-arm randomised controlled trial. Lancet HIV. 2016;3:e529–38.
Pellowski JA, Price DM, Harrison AD, Tuthill EL, Myer L, Operario D, et al. A systematic review and meta-analysis of antiretroviral therapy (ART) adherence interventions for women living with HIV. AIDS Behav. 2019;23:1998–2013.
Kaaya SF, Blander J, Antelman G, Cyprian F, Emmons KM, Matsumoto K, et al. Randomized controlled trial evaluating the effect of an interactive group counseling intervention for HIV-positive women on prenatal depression and disclosure of HIV status. AIDS Care. 2013;25:854–62.
Dadi AF, Akalu TY, Baraki AG, Wolde HF. Epidemiology of postnatal depression and its associated factors in Africa: a systematic review and meta-analysis. PLoS ONE. 2020;15: e0231940.
Dadi AF, Wolde HF, Baraki AG, Akalu TY. Epidemiology of antenatal depression in Africa: a systematic review and meta-analysis. BMC Pregnancy Childbirth. 2020;20:251.
Hatcher AM, Smout EM, Turan JM, Christofides N, Stöckl H. Intimate partner violence and engagement in HIV care and treatment among women: a systematic review and meta-analysis. AIDS. 2015;29:2183–94.
Belayneh Z, Mekuriaw B, Mehare T, Shumye S, Tsehay M. Magnitude and predictors of common mental disorder among people with HIV/AIDS in Ethiopia: a systematic review and meta-analysis. BMC Public Health. 2020;20:689.
Lancaster CA, Gold KJ, Flynn HA, Yoo H, Marcus SM, Davis MM. Risk factors for depressive symptoms during pregnancy: a systematic review. Am J Obstet Gynecol. 2010;202:5–14.
Acknowledgements
The views expressed are those of the authors and should not be construed to represent the positions of the US Army, Department of Defense, or HJF. The investigators have adhered to the policies for protection of human subjects as prescribed in AR 70–25.
Funding
This research was supported by the President's Emergency Plan For AIDS Relief (PEPFAR) collaboration, funded via a cooperative agreement (Grant No. W81XWH-11-2-0174) between the Henry M. Jackson Foundation for the Advancement of Military Medicine, Inc., and the U.S. Department of Defense (DOD). This work was also supported by the University of Washington Behavioral Research Center for HIV (BIRCH), funded by the U.S. National Institute of Mental Health (NIMH) (Grant No. P30 MH123248). JV was supported by a career development award from NIMH (Grant No. K99 MH123369).
Author information
Authors and Affiliations
Contributions
TC, PYC, CGK, IMB, AB, and DR contributed to study conception and design. TC drafted the manuscript. JV provided substantial input for the analyses. Material preparation, data collection, and analysis were performed by AE, ND, CSP, JAA, JM, JO, VS, EB, MI and HK. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest.
Ethical Approval (Include Appropriate Approvals or Waivers)
The study protocol was approved by institutional review boards at the Walter Reed Army Institute of Research, Makerere University School of Public Health, Kenya Medical Research Institute, Tanzania National Institute of Medical Research, and the Nigerian Ministry of Defense.
Consent to Participate (Include Appropriate Consent Statements)
Written, voluntary, informed consent was provided by all study participants prior to enrollment.
Consent for Publication
Consent statement regarding publishing an individual’s data or image.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Concepcion, T., Velloza, J., Kemp, C.G. et al. Perinatal Depressive Symptoms and Viral Non-suppression Among a Prospective Cohort of Pregnant Women Living with HIV in Nigeria, Kenya, Uganda, and Tanzania. AIDS Behav 27, 783–795 (2023). https://doi.org/10.1007/s10461-022-03810-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-022-03810-6