Abstract
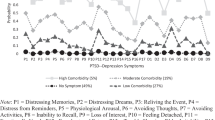
Although there are an increasing number of studies that have explored the mental health consequences of COVID-19 focusing on revealing risk factors, the longitudinal research examining the potential mechanism of the co-occurrence of posttraumatic stress symptoms (PTSS) and depression symptoms among adolescents were scarce. The present study identified the important comorbidity symptoms and explored longitudinal relationship of PTSS and depression symptoms from the network perspective. A two-wave investigation (4 months interval; T1 and T2) was conducted with a sample of 1225 Chinese adolescents. Cross-sectional network and cross-lagged panel network (CLPN) analyses were adopted. Results showed that comorbidity symptoms consisted of both overlapping and non-overlapping symptoms, including “Future foreshortening” at T1 and T2 from PTSS, and “Hard to get started” at T1 and “Not sleep well” at T2 from depression symptoms. Strong longitudinal pathways appeared from all PTSS to depression symptoms, among which the pathway from “Difficulty concentrating” to “Hard to get started” was the strongest. These findings suggest that the possible comorbidity between PTSS and depression symptoms is caused by their independent and related structures, and their longitudinal association. Clinical intervention for these symptoms may alleviate adolescents’ psychological problems in the aftermath of traumatic events.




Similar content being viewed by others
Data Availability
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
References
Afzali MH, Sunderland M, Teesson M, Carragher N, Mills K, Slade T (2017) A network approach to the comorbidity between posttraumatic stress disorder and major depressive disorder: the role of overlapping symptoms. J Affect Disord 208:490–496. https://doi.org/10.1016/j.jad.2016.10.037
Alamolhoda SH, Zare E, HakimZadeh A, Zalpour A, Vakili F, Chermahini RM, Ebadifard R, Masoumi M, Khaleghi N, Nasiri M (2023) Adolescent mental health during covid-19 pandemics: a systematic review. Int J Adolesc Med Health 35(1):41–60. https://doi.org/10.1515/ijamh-2022-0058
American Psychiatric Association (2013) Diagnostic and statistical manual of mental disorders, 5th edn. American Psychiatric Association, Washington, DC
An Y, Shi J, Chuan-Peng H, Wu X (2021) The symptom structure of posttraumatic stress disorder and co-morbid depression among college students with childhood abuse experience: a network analysis. J Affect Disord 293:466–475. https://doi.org/10.1016/j.jad.2021.06.065
An Y, Huang J, Chen Y, Deng Z (2019) Longitudinal cross-lagged relationships between posttraumatic stress disorder and depression in adolescents following the Yancheng tornado in China. Psychol Trauma Theory Res Pract Policy 11(7):760–766. https://doi.org/10.1037/tra0000455
Armour C, Greene T, Contractor AA, Weiss N, Dixon-Gordon K, Ross J (2020) Posttraumatic stress disorder symptoms and reckless behaviors: a network analysis approach. J Trauma Stress 33(1):29–40. https://doi.org/10.1002/jts.22487
Babson KA, Feldner MT (2010) Temporal relations between sleep problems and both traumatic event exposure and PTSD: a critical review of the empirical literature. J Anxiety Disord 24(1):1–15. https://doi.org/10.1016/j.janxdis.2009.08.002
Bates LC, Zieff G, Stanford K, Moore JB, Kerr ZY, Hanson ED, Barone Gibbs B, Kline CE, Stoner L (2020) COVID-19 impact on behaviors across the 24-hour day in children and adolescents: physical activity, sedentary behavior, and sleep. Children 7(9):9. https://doi.org/10.3390/children7090138
Blanken TF, Deserno MK, Dalege J, Borsboom D, Blanken P, Kerkhof GA, Cramer AOJ (2018) The role of stabilizing and communicating symptoms given overlapping communities in psychopathology networks. Sci Rep 8(1):5854. https://doi.org/10.1038/s41598-018-24224-2
Borsboom D, Cramer AOJ (2013) Network analysis: an integrative approach to the structure of psychopathology. Annu Rev Clin Psychol 9(1):91–121. https://doi.org/10.1146/annurev-clinpsy-050212-185608
Carey RL, Bailey MJ, Polanco CI (2023) How the COVID-19 pandemic shaped adolescents’ future orientations: insights from a global scoping review. Curr Opin Psychol 53:101655. https://doi.org/10.1016/j.copsyc.2023.101655
Chavez-Baldini U, Verweij K, De Beurs D, Bockting C, Lok A, Sutterland AL, Van Rooijen G, Van Wingen G, Denys D, Vulink N, Nieman D (2022) The interplay between psychopathological symptoms: Transdiagnostic cross-lagged panel network model. BJPsych Open 8(4):e116. https://doi.org/10.1192/bjo.2022.516
Chen J, Yang K, Cao Y, Du Y, Wang N, Qu M (2022) Depressive symptoms among children and adolescents in china during the coronavirus disease-19 epidemic: a systematic review and meta-analysis. Front Psych 13:870346. https://doi.org/10.3389/fpsyt.2022.870346
Chen S, Bi K, Lyu S, Sun P, Bonanno GA (2022) Depression and PTSD in the aftermath of strict COVID-19 lockdowns: a cross-sectional and longitudinal network analysis. Eur J Psychotraumatol 13(2):2115635. https://doi.org/10.1080/20008066.2022.2115635
Choi KW, Batchelder AW, Ehlinger PP, Safren SA, O’Cleirigh C (2017) Applying network analysis to psychological comorbidity and health behavior: depression, PTSD, and sexual risk in sexual minority men with trauma histories. J Consult Clin Psychol 85(12):1158–1170. https://doi.org/10.1037/ccp0000241
Conlin WE, Hoffman M, Steinley D, Sher KJ (2022) Cross-sectional and longitudinal AUD symptom networks: they tell different stories. Addict Behav 131:107333. https://doi.org/10.1016/j.addbeh.2022.107333
Cox RC, Tuck BM, Olatunji BO (2017) Sleep disturbance in posttraumatic stress disorder: epiphenomenon or causal factor? Curr Psychiatry Rep 19(4):22. https://doi.org/10.1007/s11920-017-0773-y
Cramer AOJ, Waldorp LJ, Van Der Maas HLJ, Borsboom D (2010) Comorbidity: a network perspective. Behav Brain Sci 33(2–3):137–150. https://doi.org/10.1017/S0140525X09991567
Deng J, Zhou F, Hou W, Heybati K, Lohit S, Abbas U, Silver Z, Wong CY, Chang O, Huang E, Zuo QK, Moskalyk M, Ramaraju HB, Heybati S (2023) Prevalence of mental health symptoms in children and adolescents during the COVID-19 pandemic: a meta-analysis. Ann N Y Acad Sci 1520(1):53–73. https://doi.org/10.1111/nyas.14947
Ehlers A, Hackmann A, Steil R, Clohessy S, Wenninger K, Winter H (2002) The nature of intrusive memories after trauma: the warning signal hypothesis. Behav Res Ther 40(9):995–1002. https://doi.org/10.1016/S0005-7967(01)00077-8
Epskamp S (2020) Psychometric network models from time-series and panel data. Psychometrika 85(1):206–231. https://doi.org/10.1007/s11336-020-09697-3
Epskamp S, Borsboom D, Fried EI (2018) Estimating psychological networks and their accuracy: a tutorial paper. Behav Res Methods 50(1):195–212. https://doi.org/10.3758/s13428-017-0862-1
Epskamp S, Cramer AOJ, Waldorp LJ, Schmittmann VD, Borsboom D (2012) qgraph: network visualizations of relationships in psychometric data. J Stat Softw 48:1–18. https://doi.org/10.18637/jss.v048.i04
Fan F, Zhou Y, Liu X (2017) Sleep disturbance predicts posttraumatic stress disorder and depressive symptoms: a cohort study of Chinese adolescents. J Clin Psychiatry 78(7):882–888. https://doi.org/10.4088/JCP.15m10206
Fendrich M, Weissman MM, Warner V (1990) Screening for depressive disorder in children and adolescents: validating the center for epidemiologic studees depression scale for children. Am J Epidemiol 131(3):538–551. https://doi.org/10.1093/oxfordjournals.aje.a115529
Flory JD, Yehuda R (2015) Comorbidity between post-traumatic stress disorder and major depressive disorder: alternative explanations and treatment considerations. Dialog Clin Neurosci 17(2):141–150. https://doi.org/10.31887/DCNS.2015.17.2/jflory
Fried EI, Nesse RM (2015) Depression sum-scores don’t add up: Why analyzing specific depression symptoms is essential. BMC Med 13(1):72. https://doi.org/10.1186/s12916-015-0325-4
Fruchterman TMJ, Reingold EM (1991) Graph drawing by force-directed placement. Software 21(11):1129–1164. https://doi.org/10.1002/spe.4380211102
Funkhouser CJ, Chacko AA, Correa KA, Kaiser AJE, Shankman SA (2021) Unique longitudinal relationships between symptoms of psychopathology in youth: a cross-lagged panel network analysis in the ABCD study. J Child Psychol Psychiatry 62(2):184–194. https://doi.org/10.1111/jcpp.13256
Geng F, Zhou Y, Liang Y, Zheng X, Li Y, Chen X, Fan F (2019) Posttraumatic stress disorder and psychiatric comorbidity among adolescent earthquake survivors: a longitudinal cohort study. J Abnorm Child Psychol 47(4):671–681. https://doi.org/10.1007/s10802-018-0462-2
Hageman J (2020) Children’s and families’ behavioral and mental health during COVID-19. Pediatr Ann 49(10):e405–e406. https://doi.org/10.3928/19382359-20200922-05
Hallion LS, Steinman SA, Kusmierski SN (2018) Difficulty concentrating in generalized anxiety disorder: an evaluation of incremental utility and relationship to worry. J Anxiety Disord 53:39–45. https://doi.org/10.1016/j.janxdis.2017.10.007
Haws JK, Laifer LM, Acosta LM, Ralston AL, Ruggiero KJ, Davidson TM, Andrews AR (2023) A distinction without a difference? A Multi-method approach to understanding PTSD and depression symptom overlap among disaster-exposed adolescents. Res Child Adolesc Psychopathol 51(7):1021–1035. https://doi.org/10.1007/s10802-023-01042-3
Helmsdal G, Hanusson KD, Kristiansen MF, Foldbo BM, Danielsen ME, Steig BÁ, Gaini S, Strøm M, Weihe P, Petersen MS (2022) Long COVID in the long run-23-month follow-up study of persistent symptoms. Open Forum Infect Dis 9(7):270. https://doi.org/10.1093/ofid/ofac270
Horesh D, Brown AD (2020) Traumatic stress in the age of COVID-19: a call to close critical gaps and adapt to new realities. Psychol Trauma Theory Res Pract Policy 12(4):331–335. https://doi.org/10.1037/tra0000592
Isvoranu A-M, Epskamp S, Waldorp LJ, Borsboom D (2022) Network psychometrics with R. Routledge. https://doi.org/10.4324/9781003111238
Jahangiri K, Yousefi K, Mozafari A, Sahebi A (2020) The prevalence of suicidal ideation after the earthquake: a systematic review and meta-analysis. Iran J Public Health 49(12):2330–2338. https://doi.org/10.18502/ijph.v49i12.4815
Janoff-Bulman R, Frieze IH (1983) A theoretical perspective for understanding reactions to victimization. J Soc Issues 39(2):1–17. https://doi.org/10.1111/j.1540-4560.1983.tb00138.x
Jones PJ (2023) networktools: Tools for Identifying Important Nodes in Networks. R package version 1.5.1. https://CRAN.R-project.org/package=networktools
Jones PJ, Ma R, McNally RJ (2021) Bridge centrality: a network approach to understanding comorbidity. Multivar Behav Res 56(2):353–367. https://doi.org/10.1080/00273171.2019.1614898
Karatzias T, Shevlin M, Murphy J, McBride O, Ben-Ezra M, Bentall RP, Vallières F, Hyland P (2020) Posttraumatic stress symptoms and associated comorbidity during the COVID-19 pandemic in Ireland: a population-based study. J Trauma Stress 33(4):365–370. https://doi.org/10.1002/jts.22565
Kola L, Kohrt BA, Hanlon C et al (2021) COVID-19 mental health impact and responses in low-income and middle-income countries: Reimagining global mental health. Lancet Psychiatry 8(6):535–550. https://doi.org/10.1016/S2215-0366(21)00025-0
Lange J (2021) CliquePercolation: an R Package for conducting and visualizing results of the clique percolation network community detection algorithm. J Open Source Softw 6(62):3210. https://doi.org/10.21105/joss.03210
Lazarov A, Suarez-Jimenez B, Levi O, Coppersmith DDL, Lubin G, Pine DS, Bar-Haim Y, Abend R, Neria Y (2020) Symptom structure of PTSD and co-morbid depressive symptoms: a network analysis of combat veteran patients. Psychol Med 50(13):2154–2170. https://doi.org/10.1017/S0033291719002034
Liang Y, Yang L, Xi J, Liu Z (2022) The unique role of sleep problems among symptoms of posttraumatic stress disorder: a cross-lagged panel network analysis. Acta Psychol Sin 54(10):1206–1217
Li J, Wang X, Cui Y (2014) Uncovering the overlapping community structure of complex networks by maximal cliques. Physica A 415:398–406. https://doi.org/10.1016/j.physa.2014.08.025
Li Q, Luo R, Zhang X, Meng G, Dai B, Liu X (2021) Intolerance of COVID-19-related uncertainty and negative emotions among Chinese adolescents: a moderated mediation model of risk perception, social exclusion and perceived efficacy. Int J Environ Res Public Health 18(6):6. https://doi.org/10.3390/ijerph18062864
Ma L, Mazidi M, Li K, Li Y, Chen S, Kirwan R, Zhou H, Yan N, Rahman A, Wang W, Wang Y (2021) Prevalence of mental health problems among children and adolescents during the COVID-19 pandemic: a systematic review and meta-analysis. J Affect Disord 293:78–89. https://doi.org/10.1016/j.jad.2021.06.021
Mahmud MdS, Talukder MU, Rahman SKM (2021) Does ‘Fear of COVID-19’ trigger future career anxiety? An empirical investigation considering depression from COVID-19 as a mediator. Int J Soc Psychiatry 67(1):35–45. https://doi.org/10.1177/0020764020935488
Mercader Rubio I, Sánchez-López P, Ángel NG, Ruiz NFO (2022) Psychological consequences of fear of COVID-19: symptom analysis of triggered anxiety and depression disorders in adolescents and young adults. Int J Environ Res Public Health 19(21):21. https://doi.org/10.3390/ijerph192114171
Mullarkey MC, Stein AT, Pearson R, Beevers CG (2020) Network analyses reveal which symptoms improve (or not) following an Internet intervention (Deprexis) for depression. Depress Anxiety 37(2):115–124. https://doi.org/10.1002/da.22972
Niu X, Snyder HR (2023) The role of maladaptive emotion regulation in the bidirectional relation between sleep and depression in college students during the COVID-19 pandemic. Anxiety Stress Coping 36(1):83–96. https://doi.org/10.1080/10615806.2022.2073441
Octavius GS, Silviani FR, Lesmandjaja A, Juliansen A (2020) Impact of COVID-19 on adolescents’ mental health: a asystematic review. Middle East Curr Psychiatry 27(1):72. https://doi.org/10.1186/s43045-020-00075-4
Phalet K, Andriessen I, Lens W (2004) How future goals enhance motivation and learning in multicultural classrooms. Educ Psychol Rev 16(1):59–89. https://doi.org/10.1023/B:EDPR.0000012345.71645.d4
Qi J, Ye Y, Sun R, Zhen R, Zhou X (2023) Comorbidity of posttraumatic stress disorder and depression among adolescents following an earthquake: a longitudinal study based on network analysis. J Affect Disord 324:354–363. https://doi.org/10.1016/j.jad.2022.12.119
Radloff LS (1977) The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Meas 1(3):385–401. https://doi.org/10.1177/014662167700100306
Robinaugh DJ, Millner AJ, McNally RJ (2016) Identifying highly influential nodes in the complicated grief network. J Abnorm Psychol 125(6):747–757. https://doi.org/10.1037/abn0000181
Rodríguez-Cano R, Cortés-García L, Ulset VS, Von Soest T (2022) Worries about COVID-19 and adolescents’ mental health and life satisfaction: the role of sociodemographics and social support. Front Pediatr 10:847434. https://doi.org/10.3389/fped.2022.847434
Sanchez-Gomez M, Giorgi G, Finstad GL, Urbini F, Foti G, Mucci N, Zaffina S, León-Perez JM (2021) COVID-19 pandemic as a traumatic event and its associations with fear and mental health: a cognitive-activation approach. Int J Environ Res Public Health 18(14):14. https://doi.org/10.3390/ijerph18147422
Schindel-Allon I, Aderka IM, Shahar G, Stein M, Gilboa-Schechtman E (2010) Longitudinal associations between post-traumatic distress and depressive symptoms following a traumatic event: a test of three models. Psychol Med 40(10):1669–1678. https://doi.org/10.1017/S0033291709992248
Schmittmann VD, Cramer AOJ, Waldorp LJ, Epskamp S, Kievit RA, Borsboom D (2013) Deconstructing the construct: a network perspective on psychological phenomena. New Ideas Psychol 31(1):43–53. https://doi.org/10.1016/j.newideapsych.2011.02.007
Shi W, Yuan GF, Hall BJ, Liu X, Su Y, Zhao L, Jia P (2021) Mental disorders and emotional competence among Chinese adolescents before and during COVID-19 pandemic: a longitudinal mediation model. Front Public Health 9:767004. https://doi.org/10.3389/fpubh.2021.767004
Shi W, Yuan GF, Hall BJ, Zhao L, Jia P (2023) Chinese adolescents’ depression, anxiety, and family mutuality before and after COVID-19 lockdowns: longitudinal cross-lagged relations. Fam Relat 72(1):77–91. https://doi.org/10.1111/fare.12761
Shoshani A, Kor A (2022) The mental health effects of the COVID-19 pandemic on children and adolescents: risk and protective factors. Psychol Trauma Theory Res Pract Policy 14(8):1365–1373. https://doi.org/10.1037/tra0001188
Smith K, Haliwa I, Chappell A, Wilson JM, Strough J (2023) Psychological health benefits of focusing on the ‘here and now’ versus a limited future during the COVID-19 pandemic. J Am Coll Health. https://doi.org/10.1080/07448481.2022.2155059
Stander VA, Thomsen CJ, Highfill-McRoy RM (2014) Etiology of depression comorbidity in combat-related PTSD: a review of the literature. Clin Psychol Rev 34(2):87–98. https://doi.org/10.1016/j.cpr.2013.12.002
Terluin B, De Boer MR, De Vet HCW (2016) Differences in connection strength between mental symptoms might be explained by differences in variance: reanalysis of network data did not confirm staging. PLoS ONE 11(11):e0155205. https://doi.org/10.1371/journal.pone.0155205
Wang X, (1993) Rating Scales for Mental Health (Chinese Journal of Mental Health Supplement). Chinese Association of Mental Health, Beijing
World Health Organization (2019) Adolescent Health. Retrieved from: https://www.who.int/southeastasia/health-topics/adolescent-health
World Health Organization (2020) Statement on the second meeting of the international health regulations (2005) emergency committee regarding the outbreak of novel coronavirus (2019). Retrieved from: https://www.who.int/zh/news/item/30-01-2020-statement-on-the-second-meeting-of-the-international-health-regulations-(2005)-emergency-committee-regarding-the-outbreak-of-novel-coronavirus-(2019-ncov)
Wysocki A, Rhemtulla M, van Bork R, Cramer AOJ (2022) Cross-lagged network models. Doi:https://doi.org/10.31234/osf.io/vjr8z
Xu W, Yuan G, Liu Z, Zhou Y, An Y (2018) Prevalence and predictors of PTSD and depression among adolescent victims of the Summer 2016 tornado in Yancheng City. Arch Psychiatr Nurs 32(5):777–781. https://doi.org/10.1016/j.apnu.2018.04.010
Yang F, Lodder P, Fu M, Guo J (2022) Six-year changes of posttraumatic stress symptoms and depressive symptoms among Chinese earthquake survivors: a network analysis. J Affect Disord 310:32–42. https://doi.org/10.1016/j.jad.2022.05.002
Ying L-H, Wu X-C, Lin C-D (2012) Longitudinal linkages between depressive and posttraumatic stress symptoms in adolescent survivors following the Wenchuan earthquake in China: A three-wave, cross-lagged study. Sch Psychol Int 33(4):416–432. https://doi.org/10.1177/0143034311421271
Yue J, Zang X, Le Y, An Y (2022) Anxiety, depression and PTSD among children and their parent during 2019 novel coronavirus disease (COVID-19) outbreak in China. Curr Psychol 41(8):5723–5730. https://doi.org/10.1007/s12144-020-01191-4
Zhang L, Yao B, Zhang X, Xu H (2020) Effects of irritability of the youth on subjective well-being: mediating effect of coping styles. Iran J Public Health. https://doi.org/10.18502/ijph.v49i10.4685
Zhao Y, An Y, Tan X, Li X (2020) Mental health and its influencing factors among self-isolating ordinary citizens during the beginning epidemic of COVID-19. J Loss Trauma 25(6–7):580–593. https://doi.org/10.1080/15325024.2020.1761592
Zhao Y-J, Jin Y, Rao W-W, Li W, Zhao N, Cheung T, Ng CH, Wang Y-Y, Zhang Q-E, Xiang Y-T (2021) The prevalence of psychiatric comorbidities during the SARS and COVID-19 epidemics: a systematic review and meta-analysis of observational studies. J Affect Disord 287:145–157. https://doi.org/10.1016/j.jad.2021.03.016
Zhen R, Zhou X (2022) Latent patterns of posttraumatic stress symptoms, depression, and posttraumatic growth among adolescents during the COVID-19 pandemic. J Trauma Stress 35(1):197–209. https://doi.org/10.1002/jts.22720
Zhou X, Wu X, Zhen R (2018) Self-esteem and hope mediate the relations between social support and post-traumatic stress disorder and growth in adolescents following the Ya’an earthquake. Anxiety Stress Coping 31(1):32–45. https://doi.org/10.1080/10615806.2017.1374376
Acknowledgements
The authors would like to thank all the subjects who participated in this study. The authors thank all the researchers and scientific advisors for their contribution to the design of this study.
Funding
This work was supported by the National Social Science Fund of China (Grant Number 20CSH068).
Author information
Authors and Affiliations
Contributions
JJ assisted in the data curation, investigation and wrote the original draft; GFY assisted in review, editing and the data curation; YA contributed to review and in charge of project administration; XL assisted in review and editing.
Corresponding author
Ethics declarations
Competing interest
The authors declare no competing interests.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the School of Psychology, Nanjing Normal University and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The IRB number is 202007013.
Informed Consent
Informed consent was obtained from all enrolled participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Jin, J., Yuan, G.F., An, Y. et al. Longitudinal Association Between Posttraumatic Stress Symptoms and Depression Symptoms Among Chinese Adolescents During COVID-19: Evidence from Network Perspective. Child Psychiatry Hum Dev (2024). https://doi.org/10.1007/s10578-023-01650-6
Accepted:
Published:
DOI: https://doi.org/10.1007/s10578-023-01650-6