Abstract
Insecure attachment is regarded as a risk factor for depressive symptoms. However, insecure attachment can be divided into attachment avoidance and anxiety, so a better understanding of the relationship between attachment avoidance, attachment anxiety, and depressive symptoms is needed. The current study applied a structural equation model to verify our hypothesis that different facets of affective empathy mediate the relationship between attachment avoidance, attachment anxiety, and depressive symptoms. The participants of this study included four hundred and sixty-four undergraduate students who completed the Experiences in Close Relationships-Relationship Structures Questionnaire, Interpersonal Reactivity Index, and Center for Epidemiologic Studies Depression Scale. The results indicated that the correlation between attachment avoidance and depressive symptoms was mediated by empathic concern, while the correlation between attachment anxiety and depressive symptoms was mediated by personal distress. These results implied that attachment avoidance and attachment anxiety work on depressive symptoms through different pathways.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Attachment and depressive symptoms
Depression has increasingly become a significant public health problem worldwide. Although depression in youth (Thapar et al., 2012) and older adults (Fiske et al., 2009) has received much attention, depression in emerging adults has not. Their mental health deserves more attention (Ferro et al., 2015). Aged between 18 and 25 years and being in a transitional period of life (Arnett, 2000), emerging adults face substantial interpersonal pressure and chronic interpersonal stress, which are two unique predictors of risks for depressive symptoms (Vrshek-Schallhorn et al., 2015). Even if they are not diagnosed with depression, they might also be disturbed by depressive symptoms. According to ecological systems theory (Bronfenbrenner & Morris, 2006), the family, as an essential microenvironment system, plays a role in individual growth. Family also provides room for the formation of attachment during the early interactions between children and parents, which may be an essential factor explaining the subsequent formation and development of depressive symptoms.
A growing stream of research suggests a close correlation between insecure attachment and depressive symptoms. Attachment is a unique emotional connection between an individual and an important person, and it also represents an individual's natural tendency to seek closeness and emotional connection with a vital individual (Bowlby, 1977a). In accordance with attachment theory, people develop internal working models of attachment figures by interacting with others, which influences the cognitive and affective process of how we handle social information and shape mental representations of social relationships (Bowlby, 1982). Individuals with insecure attachment were more likely to have a higher risk of suffering from depressive symptoms than those with secure attachment (Galynker et al., 2012). A recent meta-analysis showed that insecure attachment was positively related to depressive symptoms, whether measured by questionnaire or using representational methods (Madigan et al., 2016).
Attachment, Empathy, and Depressive Symptoms
Insecure attachment can be divided into attachment avoidance and attachment anxiety. Attachment avoidance refers to the degree to which an individual does not trust others and keeps a distance from others, while attachment anxiety addresses the degree of an individual's fear of being rejected or abandoned by others (Brennan et al., 1998; Fraley et al., 2011). Although attachment avoidance and attachment anxiety are positively related to depressive symptoms, they might function differently. Attachment avoidance may deactivate the attachment behavior system. Suslow et al. (2010) found that attachment avoidance correlated negatively with the automatic emotional response to sad faces, and the correlation remained the same when the attachment type was changed to attachment anxiety. An identical result was also found in Huang et al. (2019), and they found that attachment avoidance was negatively correlated with fearful prosodic emotion recognition. This might explain why depressive symptoms persisted in individuals with attachment avoidance.
In contrast, attachment anxiety may hyperactivate the attachment behavior system. Collins (1996) found that although both participants with attachment anxiety and those with attachment avoidance might explain events in negative ways, the former is prone to report more emotional distress. These results implied that attachment avoidance might weaken emotional responses. In contrast, attachment anxiety might strengthen the emotional response. Additionally, previous studies found a positive association between anxious attachment and depressive symptoms and no significant relationship between avoidant attachment and depressive symptoms (Bishop, Norona, Roberson, Welsh, & Mccurry, 2019). Therefore, the relationship between attachment and depressive symptoms is not simply direct, but different attachment dimensions contribute to depressive symptoms through different mediating variables.
One potential mechanism of particular interest in understanding the links between attachment and depressive symptoms is affective empathy. Affective empathy is the capacity to match with or feel others’ emotions (de Waal, 2017). According to the theoretical and empirical literature, attachment formation, especially with one’s mother, is based on early parent–child interactions (Noriuchi et al., 2008). We develop our empathy during early parent–child interactions (Decety & Svetlova, 2012; Pérez-Manrique & Gomila, 2018). Stern and Cassidy (2017) even suggested that attachment might be the root of empathy, meaning that attachment influences an individual's social functioning through empathy, especially affective empathy. Affective empathy is measured mainly by the subscales of the Interpersonal Reactivity Index (IRI, Davis, 1983), such as empathic concern and personal distress. Secure attachment means that an individual's emotional needs have been met and that one has received empathic caregiving. Furthermore, individuals with secure attachment can develop this ability to respond empathically to others (Kestenbaum et al., 1989). However, empathy is also a risky strength that might lead to depressive symptoms (Tone & Tully, 2014). Some research evidence has shown that affective empathy is significantly and positively related to depressive symptoms (Calandri et al., 2019; Gambin & Sharp, 2018). Affective empathy might bring emotional contagion and emotional understanding of others' distress, inducing personal distress and increasing the risk of depressive symptoms (Russell & Brickell, 2015). It is worth noting that affective empathy can be divided into empathic concern and personal distress, and the two have different functions: according to the empathy-altruism hypothesis, the former leads to approach behavior, while the latter gives rise to avoidance behavior (Batson et al., 2015). Above all, the relationship between insecure attachment and depressive symptoms might be mediated by different facets of affective empathy.
Different facets of affective empathy play different roles. First, the correlation between insecure attachment and affective empathy is distinct. Attachment avoidance might relate to empathic concern, and attachment anxiety might relate to empathic concern and personal distress (Britton & Fuendeling, 2005; Laible et al., 2004). Second, differences exist in the relationship between affective empathy and depressive symptoms. Although both personal distress and empathic concern are regarded as emotional components, they are considered to have opposite functions, with personal distress-making individuals focus on themselves and empathic concern enabling individuals to attend to others (Davis, 1983). Previous research found that empathic concern was negatively related to depressive symptoms, while personal distress was linked with the negative emotionality aspects of empathy (O'Connor et al., 2002), which were positively related to depressive symptoms (Burnette et al., 2009; Neumann et al., 2016). According to classic theoretical models (Decety & Lamm, 2006; Preston & de Waal, 2002), individuals with deep empathic concern are more likely to take others’ perspectives into account, are less likely to be overwhelmed by others’ distress, and consequently, are more resistant to mental health problems (Huang et al., 2020; Thirioux et al., 2016). Conversely, individuals with high personal distress are more likely to look at things from their own perspectives, resulting in stronger feelings of personal distress when observing others in pain (Decety & Lamm, 2006). Thus, a multipath model was considered to investigate the relationship between maternal attachment and depressive symptoms and the mediating effect of different facets of affective empathy.
The Current Study
In summary, the current study applied a structural equation model to test the links between attachment and depressive symptoms and the mediating role of affective empathy. First, we propose two hypotheses.
H1: Both attachment avoidance and attachment anxiety are significantly positively related to depressive symptoms.
H2: Affective empathy mediates the relationship between attachment and depressive symptoms.
Method
Participants
Five hundred and six Chinese undergraduate students from the local university were recruited to participate in this study. All subjects participated by choice and were paid at the end of the study. They were told that the questionnaire would be used to measure their mental health. Due to COVID-19, data were collected on the internet, and no data were lost. These questionnaires were measured in sequence. The answers of forty-two people were excluded because they failed to pass the online attention check or the two comprehension checks, and 464 final samples (286 women) remained. The participants ranged in age from 17 to 22 years old (M = 19.71 years, SD = 1.32). The response rate was 91.70%. All participants were provided with informed consent, which met the ethical standards outlined by the Declaration of Helsinki.
Measurement
Attachment
The Experiences in Close Relationships-Relationship Structures Questionnaire (ECR-RS, Fraley, et al., 2011) was employed to measure attachment avoidance and attachment anxiety. The ECR-RS consists of 9 items for four types of intimate relationships, six items for attachment avoidance (e.g., “I easily rely on my mother”), and three items for attachment anxiety (e.g., “I am afraid my mother will abandon me”). The cultural equivalence of ECR-RS has been demonstrated (Hao et al., 2019). In this study, participants were asked to rate statements regarding their relationships with their mothers on a 7-point scale, from 1 (strongly disagree) to 7 (strongly agree). In this study, the Cronbach's alphas of attachment avoidance and attachment anxiety were 0.81 and 0.86, respectively. The confirmatory factor analysis model-fitting index was also good (x2(26) = 79.79, p < 0.001, CFI = 0.95; TLI = 0.91; RMSEA = 0.08; SRMR = 0.07).
Affective Empathy
Affective empathy was measured by the subscale of the Interpersonal Reactivity Index (IRI, Davis, 1983), the most popular tool in this field (Yan et al., 2020). According to a previous study, empathic concern and personal distress were measure the affective empathy of the participants, of which options ranged from 1 (does not describe me well) to 5 (describes me very well). The cultural equivalence of IRI has been demonstrated (Siu & Shek, 2005). Ranging from 0.62 to 0.71 in previous research (Davis, 1983), the Cronbach's alphas of empathic concern and personal distress in this study were 0.62 and 0.67, respectively. The confirmatory factor analysis model-fitting index was also good (x2(76) = 48.40, p < 0.001, CFI = 0.90; TLI = 0.90; RMSEA = 0.08; SRMR = 0.05).
Depressive Symptoms
The Center for Epidemiologic Studies Depression Scale (CES-D, Radloff, 1977), which consists of 20 items rated on a scale from 0 (rarely and less than 1 day) to 3 (often and more than 5–7 days), was suitable to measure the depressive symptoms (e.g., I felt depressed) of individuals. The cultural equivalence of CES-D has been demonstrated (Jiang et al., 2019). Cronbach's alpha was 0.90 in this study. The confirmatory factor analysis model-fitting index was also good (x2(170) = 524.14, p < 0.001, CFI = 0.90; TLI = 0.90; RMSEA = 0.07; SRMR = 0.05).
Statistical Analysis
A structural equation model (SEM) with maximum likelihood estimation and the bootstrap method with 5000 iterations was adopted to confirm our hypotheses. JASP (version 0.16.1, Wagenmakers et al., 2018) was used to test the proposed mediation model.
In this study, insecure attachment and depressive symptoms were selected as the independent and dependent variables, respectively, and affective empathy was chosen as a mediator. All variables were constructed as latent variables to decrease biased estimation, and the item-parceling method was used to increase the reliability of the indicators and the power of the tests of model fit (Matsunaga, 2008). More specifically, we used the item-to-construct balance strategy to parcel items, and each indicator was estimated by three parcels in SEM (Kline, 2011).
The following indices were used to evaluate the data-model fit, as Hu and Bentler (1999) suggested: the chi-square statistics (χ2), comparative fit index (CFI), Tucker–Lewis index (TLI), root-mean-square error of approximation (RMSEA), and standardized root-mean-square residual (SRMR). This model was accepted if CFI and TLI > 0.90 and SRMR and RMSEA < 0.08 were both achieved. Meanwhile, if there were multiple suitable models, we chose the most concise one.
Results
Common Method Biases Analysis
Consistent with previous studies, this study used Harman's single-factor test to address the issue of common method variance (Podsakoff et al., 2003), with attachment, affective empathy, and depressive symptoms combined for exploratory factor analysis. The results showed that eight factors were extracted, and the first factor could explain 11.07% of the overall variance, showing that common method biases were not apparent in the current study.
Descriptive Statistics and Correlation Analysis
Descriptive statistics are provided in Table 1. First, we checked the normality of the data following previous research guidelines (skewness < 2; kurtosis < 7, West et al., 1995), which was suitable for further analysis. Second, we performed correlation analysis and found that attachment avoidance and attachment anxiety were significantly positively related to depressive symptoms. Attachment avoidance was significantly negatively related to empathic concern. Attachment anxiety was significantly negatively related to empathic concern and positively related to personal distress. Empathic concern was significantly negatively related to depressive symptoms, and personal distress was significantly positively associated with depressive symptoms.
Measurement Model
The confirmatory factor analysis results showed that the measurement model (Model 1) was well fitted for the current data, x2(80) = 278.93, p < 0.001; CFI = 0.936; TLI = 0.916; RMSEA = 0.073; SRMR = 0.063. The factor loadings of the indicators ranged from.45 to.97, and all indicators were significantly related to the latent variables, suggesting that the indicators adequately represented the latent constructs.
Mediation Model
Subsequently, we tested structural models with the mediating effect of affective empathy on the relationships among attachment anxiety, attachment avoidance, and depression. According to our hypotheses and correlation results, we built a model in which empathic concern and personal distress were set as mediators of the relationship between attachment and depressive symptoms. SEM was used to examine the hypothesized model, which included all direct and indirect pathways to depressive symptoms from each type of insecure attachment.
The hypothesized model (Model 1) was found to be an acceptable fit for the data, x2(80) = 278.93, p < 0.001; CFI = 0.936; TLI = 0.916; RMSEA = 0.073; SRMR = 0.063. However, several of the parameter estimates were not significant. Specifically, the standardized coefficients were not significant for the predictive links between attachment avoidance and personal distress (β = − 0.05, 95% CI − 0.187, 0.078, Z = − 0.81, p = 0.42), between attachment anxiety and empathic concern (β = − 0.11, 95% CI − 0.163, 0.013, Z = − 1.66, p = 0.10), and between attachment avoidance and depressive symptoms (β = − 0.01, 95% CI − 0.197, 0.173, Z = − 0.13, p = 0.90). Attachment could explain 41.90% of the variance in depressive symptoms, 11.5% of the variance in empathic concern and 7.0% of the variance in personal distress.
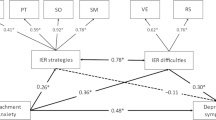
Then, we built a partial mediation model and tested Model 2. Model 2 fits well, with x2 (82) = 283.03, p < 0.001; CFI = 0.935; TLI = 0.917; RMSEA = 0.073; SRMR = 0.066 (see Fig. 1). In the partial mediation model, nonsignificant indirect paths were eliminated to generate a more parsimonious model. Thus, Model 2 should be retained. Model 2 revealed different patterns of predictive relationships for each of the two insecure attachments. We found that the indirect effect of empathic concern on the relationship between attachment avoidance and depressive symptoms was significant (β = 0.18, 95% CI 0.096, 0.394, Z = 3.22, p < 0.01), while the direct effect of attachment avoidance on depressive symptoms was not significant (β = − 0.03, 95% CI − 0.230, 0.146, Z = − 0.44, p = 0.66). Empathic concern fully mediated the relationship between attachment avoidance and depressive symptoms. The indirect effect of personal distress on the relationship between attachment anxiety and depressive symptoms was also significant (β = 0.17, 95% CI = 0.093, 0.302, Z = 3.70, p < 0.001), and the direct effect of attachment anxiety on depressive symptoms was significant (β = 0.18, 95% CI 0.071, 0.361, Z = 2.91, p < 0.01). Personal distress partially mediated the relationship between attachment anxiety and depressive symptoms. The total effect of attachment on depressive symptoms was significant (β = 0.50, 95% CI 0.444, 0.788, Z = 7.02, p < 0.001). Attachment could explain 41.60% of the variance in depressive symptoms, 9.5% of the variance in empathic concern, and 8.6% of the variance in personal distress.
Furthermore, we also tested a full mediation model (Model 3) in which the direct paths from attachment to depressive symptoms were deleted to provide additional evidence for full mediation. The results of this full mediation model showed that Model 3 (x2(84) = 290.75, p < 0.001; CFI = 0.933; TLI = 0.917; RMSEA = 0.073; SRMR = 0.070) was still a good approximation of fit, but the index reported was worse than that of Model 2. At the same time, direct paths from attachment to depressive symptoms do exist, so Model 3 is also less applicable than Model 2. The chi-square difference test showed that Model 2 was better than Model 3 (△x2 = 7.72, df = 2, p < 0.05), and Model 1 was better than Model 3 (△x2 = 11.82, df = 4, p < 0.05); there was no significant difference between Model 1 and Model 2 (△x2 = 4.10, df = 2, p = 0.13). Therefore, Model 2 was the most suitable model in our current study.
Discussion
Following the hypotheses of this study, we investigate not only the relationships between attachment avoidance, attachment anxiety, and depressive symptoms but also the mediating effect of affective empathy. The correlation analysis results indicated that attachment avoidance and attachment anxiety were positively related to depressive symptoms (Hypothesis 1). Nevertheless, the correlations between attachment avoidance and attachment anxiety and affective empathy were slightly different. Empathic concern fully mediates the correlation between attachment avoidance and depressive symptoms, and personal distress partially mediated the correlation between attachment anxiety and depressive symptoms (Hypothesis 2).
The Mediating Effect of Empathy
The findings suggest that affective empathy plays different roles in the relationship between insecure attachment and depressive symptoms. According to Stern and Cassidy (2017), empathy is the product of attachment development. Therefore, insecure attachment might increase the risk of depressive symptoms by impeding the growth of empathy. Due to the difference between attachment avoidance and attachment anxiety, empathy works differently.
First, empathic concern fully mediates the correlation between attachment avoidance and depressive symptoms. Attachment could influence an individual’s representation of self and others. Secure attachment develops a valuable, lovable, and worthy self, while insecure attachment does not (Morley & Moran, 2011). The latter point is supported by the fact that the negative correlation between attachment avoidance and empathic concern emerged in the early stage of development (Ştefan & Avram, 2019). Attachment avoidance refers to the degree to which an individual does not trust others and keeps a distance from others, which leads to avoidance behavior rather than empathic concern. For example, attachment avoidance is negatively correlated with individual emotion recognition, especially fearful prosodic emotion recognition (Huang et al., 2019), which means that individuals are self-oriented and do not feel sympathy and concern for others' misfortunes. However, empathic concern is essential to social interactions (Davis, 1983). Higher empathic concern always brings greater friendship quality to individuals (Bianchi et al., 2020), while lower empathic concern does the opposite. In other words, individuals with lower empathic concern are more prone to depressive symptoms due to decreased interpersonal relationship quality and low interpersonal communication efficiency. Hence, attachment avoidance may increase the risk of depressive symptoms by reducing empathic concern.
Second, personal distress partially mediated the correlation between attachment anxiety and depressive symptoms. Attachment theory reveals that secure attachment constructed in the early stage of life will enable individuals to form positive cognitions and emotions about themselves (Bowlby, 1977a, 1977b). In contrast, insecure attachment may develop negative cognitions, feelings, and interpersonal expectations about the self, eventually leading to depressive symptoms. Significantly and positively related to depression (Tone & Tully, 2014), personal distress reflects the participant’s feelings of personal unease and discomfort regarding others’ emotions (Davis, 1983). Individuals with high attachment anxiety always have emotional problems, and they are prone to report more emotional distress when they confront negative events (Collins, 1996). The root of the problem may be their excessive acceptance of others' emotional information, especially negative emotions, resulting in personal distress; these individuals are unable to extricate themselves from negative emotions, which ultimately lead to depressive symptoms. Furthermore, as a negative emotion, anxiety occupies many psychological resources, leaving no room for individuals to take into account the feelings of others and making them unable to accept and adopt others' views. Anxiety will also affect their interpersonal communication and be a chief factor affecting depressive symptoms. Applying skin conductance responses to investigate the relationship between attachment and empathy, Henschel et al., (2020a, 2020b) found that individuals with attachment anxiety displayed higher skin conductance responses than those with secure attachment when viewing distressing pictures. Henschel et al. (2020a) also found that anxious individuals reported higher personal distress than secure and avoidant individuals. Undoubtedly, higher personal distress induces depressive symptoms. Thus, attachment anxiety may increase the risk of depressive symptoms by increasing personal distress.
Limitations and Future Directions
The current study still has some limitations and further research is needed. First, it is difficult to make a causal inference from self-reports. Our results only support the proposed models because the data are cross sectional. However, we do not rule out alternative models (Cole & Maxwell, 2003). In addition, some other experimental methods could also help further this research. For example, the influence of attachment might be examined by using an affective priming procedure (Mikulincer et al., 2001). Empathy could also be manipulated by perspective instruction (Batson et al., 1997). Second, maternal attachment undoubtedly plays an essential role in our development, but the influence of attachment to fathers on individual development may differ from that to mothers and has unique effects (Papini et al., 1991). Therefore, further research could investigate whether this model is suitable for examining the attachment to fathers. Third, further research should consider the role of affective empathy in social relationships and relationship quality, as well as generalized anxiety and communication skills. It seems that these factors can also act as mediators of the relationship between affective empathy and depression, suggesting an even more complex model is needed. Therefore, a mechanism by which affective empathy affects depression levels should also be considered in the future. Fourth, the measurement of empathy is still facing considerable debate. As Chrysikou and Thompson (2015) suggested, IRI is unsuitable for a two-factor structure. Thus, the current study investigates how empathy concern and personal distress influence the relationship between insecure attachment and depressive symptoms instead of affective empathy. Whether the mediating effect will vary with different empathy measurements is still unclear and deserves further verification. Finally, recent investigations suggest that the CES-D might not be a single-factor scale (Carleton et al., 2013). Although the reliability of indicators and the power of the tests of model fit could be increased with the item-parceling method, we might miss the results of different dimensions.
Conclusion
The current study found that affective empathy might explain the relationship between attachment and depressive symptoms. Moreover, empathic concern fully mediates the correlation between attachment avoidance and depressive symptoms; personal distress partially mediates the correlation between attachment anxiety and depressive symptoms.
References
Arnett, J. J. (2000). Emerging adulthood. A theory of development from the late teens through the twenties. American Psychologist, 55(5), 469–480. https://doi.org/10.1037/0003-066X.55.5.469
Batson, C. D., Lishner, D., & Stocks, E. (2015). The Empathy–Altruism Hypothesis. In The Oxford Handbook of Prosocial Behavior. In A. S. David & G. G. William (Eds.), Oxford University Press.
Batson, C. D., Sager, K., Garst, E., Kang, M., Rubchinsky, K., & Dawson, K. (1997). Is empathy-induced helping due to self–other merging? Journal of Personality and Social Psychology, 73(3), 495–509. https://doi.org/10.1037/0022-3514.73.3.495
Bianchi, D., Lonigro, A., Baiocco, R., Baumgartner, E., & Laghi, F. (2020). Social anxiety and peer communication quality during adolescence: The interaction of social avoidance, empathic concern and perspective taking. Child & Youth Care Forum, 49, 853–876. https://doi.org/10.1007/s10566-020-09562-5
Bowlby, J. (1982). Attachment and loss: Vol. 1. Attachment (2nd ed.). New York, NY: Basic Books.
Bowlby, J. (1977a). The making and breaking of affectional bonds. I: Aetiology and psychopathology in the light of attachment theory. British Journal of Psychiatry, 130, 201–210. https://doi.org/10.1192/bjp.130.3.201
Bowlby, J. (1977b). The making and breaking of affectional bonds: II. Some principles of psychotherapy: The fiftieth maudsley lecture (expanded version). British Journal of Psychiatry, 130, 421–431. https://doi.org/10.1192/bjp.130.5.421
Brennan, K. A., Clark, C. L., & Shaver, P. R. (1998). Self-report measurement of adult attachment: An integrative overview. In J. A. Simpson & W. S. Rholes (Eds.), Attachment Theory and Close Relationships (pp. 46–76). Guilford Press.
Britton, P. C., & Fuendeling, J. M. (2005). The relations among varieties of adult attachment and the components of empathy. The Journal of Social Psychology, 145(5), 519–530. https://doi.org/10.3200/socp.145.5.519-530
Bronfenbrenner, U., & Morris, P. A. (2006). The bioecological model of human development. In D. Damon & R. M. Lerner (Eds.), Handbook of child psychology: Theoretical models of human development, Volume 1, 6th ed. (pp. 793–828). Hoboken, NJ, US: John Wiley & Sons Inc.
Burnette, J. L., Davis, D. E., Green, J. D., Worthington, E. L., & Bradfield, E. (2009). Insecure attachment and depressive symptoms: The mediating role of rumination, empathy, and forgiveness. Personality and Individual Differences, 46(3), 276–280. https://doi.org/10.1016/j.paid.2008.10.016
Calandri, E., Graziano, F., Testa, S., Cattelino, E., & Begotti, T. (2019). Empathy and depression among early adolescents: The moderating role of parental support. Frontiers in Psychology, 10, 1447. https://doi.org/10.3389/fpsyg.2019.01447
Carleton, R. N., Thibodeau, M. A., Teale, M. J., Welch, P. G., Abrams, M. P., Robinson, T., & Asmundson, G. J. (2013). The center for epidemiologic studies depression scale: A review with a theoretical and empirical examination of item content and factor structure. PLoS ONE. https://doi.org/10.1371/journal.pone.0058067
Chrysikou, E. G., & Thompson, W. J. (2015). Assessing cognitive and affective empathy through the interpersonal reactivity index: An argument against a two-factor model. Assessment, 23(6), 769–777. https://doi.org/10.1177/1073191115599055
Cole, D. A., & Maxwell, S. E. (2003). Testing mediational models with longitudinal data: Questions and tips in the use of structural equation modeling. Journal of Abnormal Psychology, 112(4), 558–577. https://doi.org/10.1037/0021-843X.112.4.558
Collins, N. L. (1996). Working models of attachment: Implications for explanation, emotion, and behavior. Journal of Personality and Social Psychology, 71(4), 810–832. https://doi.org/10.1037/0022-3514.71.4.810
Davis, M. H. (1983). Measuring individual differences in empathy: Evidence for a multidimensional approach. Journal of Personality and Social Psychology, 44(1), 113–126. https://doi.org/10.1037/0022-3514.44.1.113
de Waal, F. B. M., & Preston, S. D. (2017). Mammalian empathy: Behavioural manifestations and neural basis. Nature Reviews Neuroscience, 18(8), 498–509. https://doi.org/10.1038/nrn.2017.72
Decety, J., & Lamm, C. (2006). Human empathy through the lens of social neuroscience. The Scientific World Journal, 6, 1146–1163. https://doi.org/10.1100/tsw.2006.221
Decety, J., & Svetlova, M. (2012). Putting together phylogenetic and ontogenetic perspectives on empathy. Developmental Cognitive Neuroscience, 2(1), 1–24. https://doi.org/10.1016/j.dcn.2011.05.003
Ferro, M. A., Gorter, J. W., & Boyle, M. H. (2015). Trajectories of depressive symptoms in Canadian emerging adults. American Journal of Public Health, 105, 2322–2327. https://doi.org/10.2105/AJPH.2015.302817
Fiske, A., Wetherell, J. L., & Gatz, M. (2009). Depression in older adults. Annual Review of Clinical Psychology, 5(1), 363–389. https://doi.org/10.1146/annurev.clinpsy.032408.153621
Fraley, R. C., Heffernan, M. E., Vicary, A. M., & Brumbaugh, C. C. (2011). The experiences in close relationships relationship structures questionnaire a method for assessing attachment orientations across relationships. Psychological Assessment, 23(3), 615–625. https://doi.org/10.1037/a0022898
Galynker, I. I., Yaseen, Z. S., Katz, C., Zhang, X., Jennings-Donovan, G., Dashnaw, S., Hirsch, J., Mayberg, H., Cohen, L. J., & Winston, A. (2012). Distinct but overlapping neural networks subserve depression and insecure attachment. Social Cognitive and Affective Neuroscience, 7(8), 896–908. https://doi.org/10.1093/scan/nsr074
Gambin, M., & Sharp, C. (2018). The relations between empathy, guilt, shame and depression in inpatient adolescents. Journal of Affective Disorders, 241, 381–387. https://doi.org/10.1016/j.jad.2018.08.068
Hao, J., Chan, R. C. K., & Wilkinson, R. B. (2019). A cross-cultural examination of the experiences in Close Relationships — Revised — General Short Form (ECR-R-GSF) in an Australian and a Chinese sample. Journal of Relationships Research. https://doi.org/10.1017/jrr.2019.8
Henschel, S., Nandrino, J.-L., & Doba, K. (2020b). Emotion regulation and empathic abilities in young adults: The role of attachment styles. Personality and Individual Differences. https://doi.org/10.1016/j.paid.2019.109763
Henschel, S., Nandrino, J.-L., Pezard, L., Ott, L., Vulliez-Coady, L., & Doba, K. (2020a). The influence of attachment styles on autonomic correlates of perspective-taking. Biological Psychology, 154, 107908. https://doi.org/10.1016/j.biopsycho.2020.107908
Hu, L. T., & Bentler, P. M. (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling, 6(1), 1–55. https://doi.org/10.1080/10705519909540118
Huang, H., Liu, Y., & Su, Y. (2020). What Is the relationship between empathy and mental health in preschool teachers: The role of teaching experience. Frontiers in Psychology. https://doi.org/10.3389/fpsyg.2020.01366
Huang, Y. L., Chen, S. H., & Tseng, H. H. (2019). Attachment avoidance and fearful prosodic emotion recognition predict depression maintenance. Psychiatry Research, 272, 649–654. https://doi.org/10.1016/j.psychres.2018.12.119
Jiang, L., Wang, Y., Zhang, Y., Li, R., Wu, H., Li, C., & Tao, Q. (2019). The reliability and validity of the center for epidemiologic studies depression scale (CES-D) for Chinese university students. Frontiers in Psychiatry. https://doi.org/10.3389/fpsyt.2019.00315
Kestenbaum, R., Farber, E. A., & Sroufe, L. A. (1989). Individual differences in empathy among preschoolers: Relation to attachment history. New Directions for Child and Adolescent Development, 44, 51–64. https://doi.org/10.1002/cd.23219894405
Kline, R. B. (2011). Principles and practice of structural equation modeling (3rd ed.). Guilford Press.
Laible, D. J., Carlo, G., & Roesch, S. C. (2004). Pathways to self-esteem in late adolescence: The role of parent and peer attachment, empathy, and social behaviours. Journal of Adolescence, 27(6), 703–716. https://doi.org/10.1016/j.adolescence.2004.05.005
Madigan, S., Brumariu, L. E., Villani, V., Atkinson, L., & Lyons-Ruth, K. (2016). Representational and questionnaire measures of attachment: A meta-analysis of relations to child internalizing and externalizing problems. Psychological Bulletin, 142(4), 367–399. https://doi.org/10.1037/bul0000029
Matsunaga, M. (2008). Item parceling in structural equation modeling: A primer. Communication Methods and Measures, 2(4), 260–293. https://doi.org/10.1080/19312450802458935
Mikulincer, M., Hirschberger, G., Nachmias, O., & Gillath, O. (2001). The affective component of the secure base schema: Affective priming with representations of attachment security. Journal of Personality and Social Psychology, 81(2), 305–321. https://doi.org/10.1037/0022-3514.81.2.305
Morley, T. E., & Moran, G. (2011). The origins of cognitive vulnerability in early childhood: Mechanisms linking early attachment to later depression. Clinical Psychology Review, 31(7), 1071–1082. https://doi.org/10.1016/j.cpr.2011.06.006
Neumann, D. L., Chan, R. C. K., Wang, Y., & Boyle, G. J. (2016). Cognitive and affective components of empathy and their relationship with personality dimensions in a Chinese sample. Asian Journal of Social Psychology, 19(3), 244–253. https://doi.org/10.1111/ajsp.12138
Noriuchi, M., Kikuchi, Y., & Senoo, A. (2008). The functional neuroanatomy of maternal love: Mother’s response to infant’s attachment behaviors. Biological Psychiatry, 63(4), 415–423. https://doi.org/10.1016/j.biopsych.2007.05.018
O’Connor, L. E., Berry, J. W., Weiss, J., & Gilbert, P. (2002). Guilt, fear, submission, and empathy in depression. Journal of Affective Disorders, 71, 19–27. https://doi.org/10.1016/S0165-0327(01)00408-6
Papini, D. R., Roggman, L. A., & Anderson, J. (1991). Early-adolescent perceptions of attachment to mother and father: A test of the emotional-distancing and buffering hypotheses. The Journal of Early Adolescence, 11(2), 258–275. https://doi.org/10.1177/0272431691112006
Pérez-Manrique, A., & Gomila, A. (2018). The comparative study of empathy: Sympathetic concern and empathic perspective-taking in non-human animals. Biological Reviews, 93(1), 248–269. https://doi.org/10.1111/brv.12342
Podsakoff, P. M., MacKenzie, S. B., Lee, J. Y., & Podsakoff, N. P. (2003). Common method biases in behavioral research: A critical review of the literature and recommended remedies. Journal of Applied Psychology, 88(5), 879–903. https://doi.org/10.1037/0021-9010.88.5.879
Preston, S. D., & de Waal, F. B. M. (2002). Empathy: its ultimate and proximate bases. Behavioral and Brain Sciences, 25, 1–71. https://doi.org/10.1017/S0140525X02000018
Radloff, L. S. (1977). The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement, 1(3), 385–401. https://doi.org/10.1177/014662167700100306
Russell, M., & Brickell, M. (2015). The “double-edge sword” of human empathy: A unifying neurobehavioral theory of compassion stress injury. Social Sciences, 4(4), 1087–1117. https://doi.org/10.3390/socsci4041087
Siu, A. M. H., & Shek, D. T. L. (2005). Validation of the Interpersonal reactivity index in a Chinese context. Research on Social Work Practice, 15(2), 118–126. https://doi.org/10.1177/1049731504270384
Ştefan, C. A., & Avram, J. (2019). Investigating attachment status effects on preschoolers’ empathic perspective-taking. Child & Youth Care Forum, 48(5), 663–675. https://doi.org/10.1007/s10566-019-09498-5
Stern, J. A., & Cassidy, J. (2017). Empathy from infancy to adolescence: An attachment perspective on the development of individual differences. Developmental Review, 47, 1–22. https://doi.org/10.1016/j.dr.2017.09.002
Suslow, T., Dannlowski, U., Arolt, V., & Ohrmann, P. (2010). Adult attachment avoidance and automatic affective response to sad facial expressions. Australian Journal of Psychology, 62(4), 181–187. https://doi.org/10.1080/00049530903567203
Thapar, A., Collishaw, S., Pine, D. S., & Thapar, A. K. (2012). Depression in adolescence. The Lancet, 379(9820), 1056–1067. https://doi.org/10.1016/s0140-6736(11)60871-4
Thirioux, B., Birault, F., & Jaafari, N. (2016). Empathy is a protective factor of burnout in physicians: New neuro-phenomenological hypotheses regarding empathy and sympathy in care relationship. Frontiers in Psychology. https://doi.org/10.3389/fpsyg.2016.00763
Tone, E. B., & Tully, E. C. (2014). Empathy as a “risky strength”: A multilevel examination of empathy and risk for internalizing disorders. Development and Psychopathology, 26(4 Pt 2), 1547–1565. https://doi.org/10.1017/S0954579414001199
Vrshek-Schallhorn, S., Stroud, C. B., Mineka, S., Hammen, C., Zinbarg, R. E., Wolitzky-Taylor, K., & Craske, M. G. (2015). Chronic and episodic interpersonal stress as statistically unique predictors of depression in two samples of emerging adults. Journal of Abnormal Psychology, 124(4), 918–932. https://doi.org/10.1037/abn0000088
Wagenmakers, E. J., Love, J., Marsman, M., Jamil, T., Ly, A., Verhagen, J., & Morey, R. D. (2018). Bayesian inference for psychology. Part II: Example applications with JASP. Psychonomic Bulletin & Review, 25(1), 58–76. https://doi.org/10.3758/s13423-017-1323-7
West, S. G., Finch, J. F., & Curran, P. J. (1995). Structural equation models with nonnormal variables: Problems and remedies. In R. H. Hoyle (Ed.), Structural equation modeling: Concepts, issues and applications (pp. 56–75). Sage.
Yan, Z., Hong, S., Liu, F., & Su, Y. (2020). A meta-analysis of the relationship between empathy and executive function. Psych Journal, 9(1), 34–43. https://doi.org/10.1002/pchj.311
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The author declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Yan, Z., Zhu, X., Zhou, K. et al. The Mediating Role of Affective Empathy in the Relationship Between Insecure Attachment and Depressive Symptoms Among Emerging Adult. J Adult Dev 29, 279–286 (2022). https://doi.org/10.1007/s10804-022-09402-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10804-022-09402-x