Abstract
Purpose
This review aimed to (1) evaluate the effectiveness of social media–based interventions for improving the quality of life, anxiety and depressive symptoms of patients with cancer at post-intervention and follow-up; (2) identify the essential features of social media–based interventions and (3) explore the covariates of the treatment effect.
Methods
All types of randomised controlled trials (RCTs) were included. Ten electronic databases, clinical trial registries and grey literature sources were searched from inception to 15 December 2021. Stata software was used to perform meta-analysis, subgroup analyses and meta-regression analyses. Individual quality assessment and certainty of evidence were assessed using Cochrane risk of bias tool version 1 and Grading of Recommendations Assessments, Development and Evaluation criteria, respectively.
Results
This review included 43 RCTs, which comprised 6239 patients with a total mean age of 49.71 years old from across 11 countries. Social media–based interventions significantly improved the quality of life (g = 0.25, 95% CI = 0.05–0.45) and anxiety symptoms (g = − 0.41, 95% CI = − 0.76–0.07) but not depressive symptoms. The essential features based on the subgroup analysis concluded that using a mobile device with a flexible frequency had a remarkably greater effect on the quality of life and anxiety symptoms than their counterparts. The meta-regression showed the covariate features, where having more social media features in interventions significantly improved the quality of life (β = 0.21, p = 0.01). The certainty of evidence was very low for all outcomes.
Conclusions
Participants who received social media–based interventions may experience an increase in quality of life and reduction in anxiety symptoms.
Implications for cancer survivors
Social media–based interventions may complement usual care in improving quality of life and anxiety symptoms.
Registration in PROSPERO
CRD42022297956.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cancer is one of the leading causes of disease burden globally. In 2020, 19.3 million new cases of cancer were recorded worldwide [1]. Patients with cancer face social isolation for several reasons. Firstly, the side effects of most cancer treatments, such as fatigue, weight gain, nausea, vomiting and pain, may cause changes in physical appearance and functional status [2,3,4]. These changes may produce constraints on physical interaction with others and lead to social isolation [5, 6]. Secondly, patients may experience stigmatisation due to discrimination from friends, family, and society, or self-blame [5, 7]. When faced with stigma, patients may isolate themselves from social circles. Social restrictions due to the coronavirus disease 2019 (COVID-19) pandemic have further limited patients’ social interactions, increasing the likelihood of mental health issues and lowering the quality of life [8,9,10]. Therefore, exploring how patients can interact using remote methods, such as social media, is needed.
Social media usage has soared with the advancement and increased usage of mobile devices and broadband networks. Today, more than half of the global population uses social media platforms [11]. Its extensive usage globally has made it a key tool for communication, information sharing and social support amidst isolation due to the COVID-19 pandemic [12, 13]. Social media are internet-based, mass or personal communication media that allow users to interact, synchronously or asynchronously [14]. Social media interventions may comprise various features, which are used to support communication and information exchange [15]. Features may include, identity representation, communication, peer grouping, data sharing, competition, activity data viewing and online social networking features [15]. The derived value from social media stems from the content generated by users from interactions.
The potential mechanisms of social media–based intervention on quality of life, anxiety symptoms and depressive symptoms using media system dependency [16] and social identity [17] theories are illustrated in Fig. 1. Socially isolated patients need social support, which can be provided through social media. In accordance with the media system dependency theory, patients will have increased dependency on social media when it is aligned with the needs of socially isolated patients [16, 18]. Increased dependency and the usage of social networking sites enhance patients’ exposure to information and other individuals online. Thus, patients are enabled to meet peers with similar attributes and form social categories and groups [19]. According to the theory of social identity, patients seek these social categories to help them make sense of changes in their self-context and social identity [17]. An optimally suitable group becomes psychologically salient to the individual’s social context and produces strong social and emotional ties [20, 21]. Constant interaction within the group produces in-group norms, which act as attitude and behavioural regulators [19]. This interaction gives patients stability and predictability, which can help reduce negative feeling during challenging times.
Social groups also provide social support in the form of social companionship, esteem, emotional, instrumental or informational support [22]. Traditional forms of support include family, friends and support groups organised by healthcare facilities. Social media has enhanced social networks with the formation of online support groups and communities. Online support groups can help overcome the logistical issues of face-to-face support groups and give patients more control over the choice of peers and groups that they engage with [23,24,25]. Through social media, online support groups provide good social support networks, which improves patients’ physical and emotional well-being and provides financial support and resources [26,27,28]. Overall dependency on social media for social support could potentially resolve ambiguities, change attitudes, relieve fear and anxiety, boost morale, reduce alienation and elicit positive health-related offline behaviour for patients [16, 29, 30]. Given that social media is a useful platform for socially isolated patients with cancer, it can improve quality of life, anxiety symptoms and depressive symptoms.
Patients with cancer suffer from poor quality of life, anxiety symptoms and depressive symptoms due to a myriad of reasons. Prolonged social isolation due to the COVID-19 pandemic has aggravated these issues. During the pandemic, the global prevalence of anxiety and depression amongst patients with cancer rose to 38% and 37%, respectively [31]. This increase is worrisome as anxiety and depressive symptoms, such as sleep disturbances, fatigue, nausea and appetite loss, impair daily functioning and worsen quality of life [32]. Poor quality of life affects patients’ stress responses, treatment-seeking behaviour and treatment compliance [33,34,35]. It impacts health outcomes and increases mortality risk [36]. Therefore, quality of life, anxiety symptoms and depressive symptoms are serious issues amongst patients with cancer and should be addressed as part of their care.
Several measurement tools have been developed to assess quality of life in patients with cancer, including European Organisation for Research and Treatment of Cancer Quality of Life Questionnaire [37], Functional Assessment of Cancer Therapy [38] and Paediatric Quality of Life Inventory [39]. State-Trait Anxiety Inventory [40], Beck Anxiety Inventory [41], Hospital Anxiety and Depression Scale-Anxiety [42], Beck Depression Inventory-II [43] and Centre for Epidemiologic Studies Depression Scale [44] are commonly used to measure anxiety and depressive symptoms.
A growing body of systematic reviews illustrate the usage of online interventions [45,46,47] and social media–based amongst patients with cancer [48,49,50]. Two scoping reviews on the usage of social media in adolescent and young adult oncology [51] and patients and caregivers [52] were conducted. However, these reviews have different study designs [48, 49] and interventions [47], used few databases [50], lack the inclusion of unpublished trials and grey literature [47, 49], had no information of the methodological quality of selected studies [49, 50] and only reported narrative synthesis [48, 50]. Previous reviews did not perform a meta-analysis, subgroup analysis or meta-regression analysis, and none of them evaluated the certainty of evidence.
The current review aimed to (1) evaluate the effectiveness of social media–based interventions for improving the quality of life, anxiety symptoms and depressive symptoms amongst patients with cancer at post-intervention and follow-up; (2) identify the essential features of social media–based interventions and (3) explore the covariates of the treatment effect. The findings from this review can help guide the design and implementation of future social media–based interventions for clinical practice and research.
Methods
This systematic review and meta-analysis adopted the Preferred Reporting Items for Systematic Reviews and Meta-Analyses 2020 statement (Table A1). This systematic review was prospectively registered (CRD42022297956) in the International Prospective Register of Systematic Reviews (PROSPERO) database.
Eligibility criteria
This review included RCTs that evaluated the effects of social media intervention on individuals diagnosed with cancer. Social media–based interventions are any form of online medium that allows participants to interact with one another. The media can be self-developed or commercial, such as Facebook, Instagram, TikTok and Twitter. Self-developed interventions have to contain one or a combination of the following features: identity representation, communication, peer grouping, data sharing, competition, activity data viewing or online social networking [15]. Comparators could be usual care, active comparator, placebo or waitlist control group. The outcomes include quality of life, anxiety symptoms and depressive symptoms at post-intervention and follow-up. Considering that quality of life, anxiety and depressive symptoms are widely reported in the extant literature, the current review is able to compare the effects of social media interventions on these outcomes meaningfully. Trials published in the English language were included. No limits on the publication year and publication status were imposed. The details of the eligibility criteria are listed in Table A2.
Search strategy
A scoping search was conducted in Cochrane Database of Systematic Reviews, PubMed Clinical Queries and PROSPERO databases for existing systematic reviews to prevent duplication. Search terms were developed in consultation with the university librarian. Then, an iterative process was used to test the sensitivity and selectivity of the search terms. The final search terms comprising index terms and keywords related to cancer and social media are included in Table A3. A three-step extensive search was conducted from inception till 15 December 2021. Firstly, a systematic search was conducted in 10 electronic databases: Cumulative Index to Nursing and Allied Health Literature, Cochrane Library, Excerpta Medica Database, Education Resources Information Centre, Institute of Electrical and Electronics Engineers, Institution of Engineering and Technology Xplore, ProQuest Dissertations and Theses Global, PsycINFO, PubMed, Scopus and Web of Science. Secondly, various clinical trial registries and grey literature sources were searched for unpublished trials and grey literature, respectively (Table A4). Lastly, the reference lists of the included studies and existing systematic reviews were handsearched.
Selection process
The retrieved articles were exported to EndNote 20 [53]. Articles were organised and duplicates removed using automated and manual functions. Two independent reviewers (DS and RT) screened the articles based on the eligibility criteria. Disagreements were resolved by the third reviewer (LY). The full texts of the included studies were subsequently downloaded. Cohen’s Kappa statistic was calculated to ensure inter-rater reliability, and 0.6 was deemed acceptable [54]. This calculation was done for trial selection, data extraction, risk of bias and certainty of evidence.
Data collection process
Data were extracted by two independent researchers (DS and RT) using an adapted version of the Cochrane data extraction form [55]. The form was piloted in six studies to ensure its clarity and comprehensibility. The items extracted included the trial characteristics and intervention description. The trial characteristics included author, year, country, design, mean age, sample size, intervention, control, attrition rate, intention-to-treat analysis, missing data management, publication of protocol, trial registration in various clinical registries and grant support. Intervention description, including the aim of intervention, regime of intervention, components of intervention, interactivity, communication style, device used, features included, presence of co-interventions, theoretical basis and outcome data, were extracted. Authors were contacted up to a maximum of three times for additional information.
Risk of bias
Risk of bias was assessed using the Cochrane Collaboration Risk of Bias Tool version 1 [56]. Risk of bias was assessed by two independent researchers (DS and RT) based on the following domains: random sequence generation, allocation sequence concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data and selective outcome reporting. Each domain is categorised as ‘low’, ‘high’ or ‘unclear’ risk [55]. Overall risk was rated using the lowest score of the six domains. Disagreements were resolved by a third reviewer (LY).
Data analysis
Stata version 17 [57] was used to perform the meta-analysis, subgroup analyses and meta-regression analyses. Meta-analysis was performed using inverse-variance method incorporated into random-effects model, which assumes that true intervention effects vary amongst studies [58]. This model measures between- and within-study variances [58]. Z statistics with p < 0.05 was used to assess the overall effect. Independent samples were used as the unit of analysis to reduce dependency issues [59]. For studies with multiple treatment groups (e.g. three arm) and compared with the same control group, the number of participants in the control group will be divided by two to ensure independence.
Effect size was measured using the magnitude of difference (e.g. mean and standard deviation) between intervention and comparator groups at the post intervention and follow-up. The effect size of continuous outcomes were expressed using Hedges’s g as it provides great precision for studies with small sample sizes [60]. Effect size was interpreted as small (0.2), medium (0.5), large (0.8) and very large (1.2) [61]. A 95% confidence interval (CI) was used to express the precision of the summary estimate and derive a p-value. Z statistic and p < 0.05 were used to determine the significance of the intervention effect [55]. Heterogeneity was measured using Cochran’s Q with p < 0.05 and I2. I2 values were interpreted as low (< 40%), moderate (40–60%), substantial (50–90%) and considerable (> 75%) [55]. A narrative analysis of the outcomes was conducted if meta-analysis was not possible.
Additional data analysis
Subgroup and meta-regression analyses were performed to address the reasons of heterogeneity. Subgroup analysis was conducted based on the components of the intervention and the characteristics of the studies to examine the essential features of the intervention and population that will most likely benefit from social media–based interventions. The predefined subgroups included country, comparator, frequency, presence of features and usage of mobile devices for the intervention. Chi-square value with p < 0.1 was calculated to determine the significance of subgroup differences, whereas I2 value was used to investigate heterogeneity [62]. Meta-regression with p < 0.05 was performed to investigate whether covariates (year of publication, sample size, attrition rate, mean age, duration of intervention and number of social media features) account for the treatment effect [63]. Regression coefficients (β) were the estimated increase or decrease in the effect size units of the covariates on particular outcomes. p < 0.05 was considered significant for random-effects meta-regression analyses [63].
Certainty of evidence
The overall quality of evidence and strength of recommendations were assessed by two independent reviewers (DS and RT) using the Grading of Recommendations Assessments, Development and Evaluation (GRADE) criteria [64]. Risk of bias, imprecision, inconsistency, indirectness and publication bias were rated as high, moderate, low or very low with justifications to support the judgements [64]. Publication bias was measured if 10 or more studies were used in the meta-analysis of each outcome [65]. Its presence was determined by funnel plot symmetry, where inverse standard error was plotted against standardised mean difference [66]. Egger’s regression test with p < 0.05 was used to evaluate the significance of asymmetry [67, 68].
Results
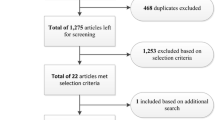
The initial search yielded a grand total of 13,821 records (Fig. 2). After the duplicates (n = 6,286) were removed, two reviewers (DS and RT) independently screened the title and abstract of 7535 articles. A total of 7424 records were excluded on based on the title (n = 7227) and abstract (n = 197). The full texts of 96 articles were assessed using the eligibility criteria, and 53 articles were excluded. The reasons for exclusion are detailed in Table A5. Only 43 articles were included from this search. In addition, 81 ongoing trials were retrieved from the trial registries, and the details are provided in Table A6. Cohen’s kappa was used to measure inter-rater agreement, which indicated strong agreement for study selection (k = 0.86) and data extraction (k = 0.83), as well as moderate agreement for risk of bias (k = 0.79) and certainty of evidence (k = 0.88) [54].
Characteristics of randomised controlled trials
The characteristics of the included RCTs are summarised in Table 1. Forty-three RCTs between 2001 [69] and 2021 [70] were included. The included studies across 11 countries had a total of 6239 patients with cancer with a grand mean age of 49.71 years old, ranging from 16.59 years old [71] to 67.20 years old [72]. Five studies are three-arm RCTs [73,74,75,76,77], one study is a four-arm RCT [78], and the rest (86.05%) are two-arm RCTs. The sample sizes ranged from 19 [79] to 794 [80]. There were different types of comparators used, usual, active or waitlist groups. The attrition rate of the trials was between 0 [81] and 42.2% [82].
Description of social media–based interventions
Table A7 shows the description of the interventions, such as essential component, medium, device, regime, goal setting, communication, interactivity, theoretical basis, reminder and follow-up assessment. The media used to deliver the interventions included websites (39.53%), social media (25.58%), mobile phone applications (20.93%) and other internet-based media (11.63%). Furthermore, most interventions were used on computers and/or mobile or smartphones. Fifteen interventions used unspecified devices with internet access. Intervention regime varied from flexible frequency (62.79%) to fixed frequency, such as weekly (27.91%), twice a week [83], at least thrice a week [72], every day [84] and twice a day [81]. Duration of interventions ranged from 3 h [85] to 24 months [82]. All study interventions contained two-way interactivity with asynchronous and/or synchronous communication. Nineteen studies had theoretical basis for their interventions. The social media features of the included interventions are summarised in Table A8 and Fig. A1. All of them comprised online social network, peer grouping and communication. More than half (53.49%) constitute data sharing, and few of them contain identity representation (39.53%) and activity data viewing (16.28%).
Risk of bias
The summary of the risk of bias assessment is shown in Fig. A2. More than half (52.71%) had low risks across six domains. All the studies used random sequence generation. However, allocation concealment was unclear in 26 studies, which were unable to overcome selection bias. The majority of the studies (81.40%) had high or unclear risk of performance bias. Detection bias was rated high in 34 studies. Most of the studies managed to overcome attrition bias (83.72%) and reporting bias (51.16%). The overall risk of bias was high for most (93.02%) of the studies.
Quality of life
Quality of life was evaluated in 30 RCTs. Seventeen studies were pooled for post-intervention meta-analysis as illustrated in Fig. 3. Statistically significant improvements in quality of life (Z = 2.48, p = 0.01) were observed after patients with cancer received social media–based interventions. At 3 months follow-up, meta-analysis also revealed statistically significant improvements in quality of life (Z = 2.07, p = 0.04). Considering the moderate to substantial heterogeneity (I2 = 58.28–79.36%), a series of subgroup and meta-regression analyses were conducted to examine the sources of heterogeneity.
Subgroup analyses for quality of life
A series of subgroup analyses of social media–based interventions on quality of life outcome was conducted to identify the sources for heterogeneity and essential features for social media interventions. Subgroups based on country, frequency, identity representation feature, device and comparator were conducted (Fig. A3). Significant subgroup differences were found amongst different countries (Q = 9.11, p < 0.01), types of device (Q = 6.61, p = 0.01) and comparator groups (Q = 8.20, p = 0.02). Studies conducted in Asia had a larger effect on quality of life (g = 0.70, 95% CI = 0.33–1.08) compared with studies in other regions (g = 0.07, 95% CI = − 0.10–0.23). With regard to devices, interventions delivered in mobile phones had a greater effect (g = 0.50, 95% CI = 0.23–0.78) than other types of devices (g = 0.05, 95% CI = − 0.16–0.26). The type of comparators also affected the quality of life scores with a larger effect size for usual care groups (g = 0.37, 95% CI = 0.11–0.62) than those with active comparators (g = 0.12, 95% CI = − 0.24–0.78) or waitlist control groups (g = − 0.07, 95% CI = − 0.24–0.09). On the basis of effect sizes, a larger effect was observed for trials that comprised an identity representation feature (g = 0.36, 95% CI = 0.02–0.69) than those without (g = 0.15, 95% CI = − 0.07–0.37). The subgroup analyses proposed that the essential features for future interventions include the use of mobile phones and compared with usual care control group.
Meta-regression analyses for quality of life
Univariate meta-regression analysis was conducted to examine the effect of the covariates on effect size (Table 2). The number of features (β = 0.21, p = 0.01) in a social media intervention significantly affected the effect size for quality of life outcome. The bubble plot is provided in Fig. A4. This result indicates that the presence of more social media features results in a better quality of life outcome. The remaining covariates, namely, year of publication (β < 0.001, p = 0.94), sample size (β < − 0.001, p = 0.87), attrition rate (β = − 1.21, p = 0.12), mean age (β < − 0.001, p = 0.95) and duration of intervention based on weeks (β < − 0.001, p = 0.95) did not have any effect on the quality of life outcome.
Anxiety symptoms
The effects of social media–based interventions on anxiety symptoms were investigated in 11 studies, amongst which 10 studies were pooled for post-intervention meta-analysis (Fig. 4). The random effects model revealed the statistically significant effects of social media–based interventions in improving anxiety symptom scores (Z = − 2.34, p = 0.02). However, no significant differences were found between the intervention and control groups (Z = 0.56, p = 0.58) in two trials at 1-month follow-up. A series of subgroup and meta-regression analyses were attempted because of the presence of moderate to substantial heterogeneity (I2 = 58.24–87.58%).
Subgroup analyses for anxiety symptoms
The findings of the subgroup analyses to identify the essential features are presented in Fig. A5. Significant subgroup differences in the frequency of intervention (Q = 7.23, p = 0.01) and the types of comparators (Q = 12.44, p < 0.01) were found. The social media–based interventions that adopted a flexible frequency had a greater effect (g = − 0.62, 95% CI = − 1.07–0.16) than those with a fixed schedule (g = 0.06, 95% CI = − 0.13–0.24). In addition, the trials that compared the intervention with usual care had a greater effect (g = − 0.76, 95% CI = − 1.23 to − 0.29) than those with an active control (g = 0.63, 95% CI = − 0.25–1.51) or waitlist control group (g = 0.06, 95% CI = − 0.13–0.24). Based on the effect sizes, countries conducted in Asia had a larger effect (g = − 0.84, 95% CI = − 1.58 to − 0.10) than non-Asian countries (g = − 0.17, 95% CI: − 0.53–0.19). Based on the subgroup analyses for anxiety symptoms, flexible schedule should be considered in future trials.
Meta-regression analysis for anxiety symptoms
Univariate meta-regression analysis was conducted to examine the effect of the covariates on effect size (Table 2). The covariates, namely, year of publication (β = − 0.04, p = 0.17), sample size (β < 0.001, p = 0.50), attrition rate (β = 0.87, p = 0.57), mean age (β < − 0.001, p = 0.92), duration of intervention based on weeks (β < 0.001, p = 0.90) and number of features (β = 0.40, p = 0.09), did not have any effect on anxiety symptoms. Considering that there are only 10 studies included into the meta-regression model, there could be insufficient statistical power to detect any significant differences.
Depressive symptoms
Seventeen RCTs evaluated the effects of social media–based interventions at post-intervention on depressive symptoms as shown in Fig. A6. The meta-analysis revealed no significant differences between the intervention and control groups in improving depressive symptom scores (Z = − 1.28, p = 0.20). Similarly, no significant differences were found at 6-month follow-up (Z = − 1.32, p = 0.19). Moderate to substantial heterogeneity were found (I2 = 58.28%–64.17%); hence, subgroup and meta-regression analyses were carried out to identify the sources of heterogeneity.
Subgroup analyses for depressive symptoms
The subgroup analysis for depressive symptoms is detailed in Fig. A7. Based on the effect sizes, the studies conducted in Asia had a larger effect (g = 0.33, 95% CI = − 0.85–0.19) compared with other regions (g = –0.04, 95% CI = − 0.18–0.10). In addition, a greater effect was found for interventions that did not comprise an identity representation feature (g = − 0.17, 95% CI = − 0.39–0.04) than those that did (g = 0.05, 95% CI = − 0.34–0.44). However, no subgroup differences were found. Hence, there were no significant recommendations for the features of social media interventions based on depressive symptoms.
Meta-regression analyses for depressive symptoms
The univariate meta-regression analysis (Table 2) concluded that the following covariates, the year of publication (β < 0.001, p = 0.78), sample size (β < 0.001, p = 0.76), attrition rate (β = − 0.09, p = 0.92), mean age (β = − 0.03, p = 0.24), duration of intervention based on weeks (β < − 0.001, p = 0.40) and number of features (β = 0.24, p = 0.09) did not have any effect on depressive symptoms.
Narrative analyses
Fourteen studies were excluded from the meta-analysis as they had insufficient information. Several emails were sent to request additional data from the authors of the trials, but they did not reply; therefore, narrative analyses were performed for these studies. The detail is presented in Table A9. Ten studies reported quality of life outcomes, but only one study found a remarkable improvement (p = 0.02) in quality of life at post intervention [74]. In comparison with the meta-analysis findings, nine RCTs found no remarkable differences between the intervention and control groups [69, 70, 72, 78, 79, 84, 86,87,88]. Out of the four studies that reported anxiety symptoms, one study found that social media–based interventions are substantially effective (p = 0.03), similar to the meta-analysis results of [73]. However, three studies found that such interventions have no considerable effect, contradicting the meta-analysis results [80, 89, 90]. Depressive symptoms were reported in five studies, where two studies found that the social media–based interventions have remarkable effects (p < 0.05) [73, 80]. In line with the findings of the meta-analysis, no substantial improvement in depressive symptoms was reported in the remaining studies [88,89,90].
Certainty of evidence
Forty-three studies were evaluated using the GRADE criteria for all outcomes. All domains had very serious concerns due to the high risk of bias, substantial heterogeneity, variations in population and intervention and small sample size with wide confidence interval. Overall, the level of certainty of evidence was downgraded to very low for all outcomes (Table A10). Publication bias was assessed for outcomes if more than 10 trials were included. No visible asymmetry was found in the funnel plots for quality of life, anxiety and depressive symptoms (Fig. A8). Egger’s regression tests also revealed no significant asymmetry for quality of life (p = 0.77), anxiety symptoms (p = 0.58) and depressive symptoms (p = 0.85).
Discussion
Summary of findings
This review aimed to analyse the effectiveness of social media–based interventions on quality of life, anxiety symptoms and depressive symptoms amongst patients with cancer. Forty-three RCTs with a total population of 6239 patients with a total mean age of 49.71 years old across 11 countries were included in this review. The meta-analyses demonstrated that social media–based interventions were significantly effective with a small effect size in improving quality of life (g = 0.25, 95% CI = 0.05–0.45) and anxiety symptoms (g = − 0.41, 95% CI = − 0.76–0.07). Subgroup analysis showed a greater effect on quality of life than their counterparts when the interventions used mobile devices in Asia compared with usual comparator. A greater effectiveness in improving anxiety symptoms was also found when the interventions used a flexible frequency compared with fixed frequency. The meta-regression results showed that using more social media features for the intervention (β = 0.21, p = 0.01) led to a better quality of life. The certainty of evidence for all outcomes was very low.
Enhancing short- and long-term quality of life
Consistent with a previous systematic review [45], social media–based interventions can remarkably improve short- and long-term quality of life. The incorporation of social media features, namely, peer grouping, group communication and online social network, in all studies enabled the formation of support networks (Fig. 1). Interaction with a community of individuals who are in similar situations gives patients validation to their feelings, opportunities to exchange information and experiences specific to each patients’ needs [15]. Companionship and support help decrease the loneliness of socially isolated patients [22]. Given that loneliness can significantly reduce patient’s quality of life [91], the findings from this review further highlight the importance of social media. In particular, elements of social media, such as peer support, could be considered in all forms of psychosocial oncology care plans. This phenomenon could be explained by media system dependency theory [16], where satisfying the needs of patients leads to the formation of dependency on social media for social support. This satisfaction elicits positive behaviour, attitude and emotions and thus improves patients’ quality of life [16, 18].
Reducing anxiety symptoms at post-intervention
Social media–based interventions also have a remarkable effect on anxiety symptom scores, which is in line with a previous systematic review [51]. Social media provides a platform for patients to discuss their feelings with peers who are more inclined to understand them. The listening ear provides emotional support to patients. Peers could also provide personalised encouragement and thus provide esteem support to each other [92]. As an individual’s experience of anxiety could be reactive to the situation or stimulus, the role of peer support could have a more immediate effect and therefore, reduce patient’s anxiety symptoms. Additionally, reading the advices and experiences of peers on the impact of cancer on their everyday lives and mental health could be more personal and less intimidating than information from healthcare professionals. Such informational support could relieve an anticipated worry of the future and help patients navigate through their day-to-day lives. The combination of emotional, esteem and informational support that social media provides can improve the overall social support of patients with cancer [22]. Good social support elicits positive social relationships, which acts as a buffer to the emotional impact of change and stressful events [22]. Therefore, based on the findings that the social support that social media provides can help relieve the anxiety symptoms of patients with cancer, future interventions should include chat room or discussion functions, to promote opportunities for interactions among its users.
Non-significant effect on depressive symptoms
Similar to a previous systematic review [45], the meta-analysis results showed that social media–based interventions have no remarkable effect on depressive symptoms. There are several potential reasons. First, living with cancer can lead to existential crisis among most individuals [93, 94]. Furthermore, cancer is a chronic and life-limiting disease; the experience of depressive symptoms is multifaceted and is prolonged throughout the cancer trajectory [95, 96]. Hence, there are expected difficulties in relieving depressive symptoms [93, 94]. Second, less than half of the included studies consist of psychotherapeutic elements in their intervention, leading to a reduced ability in relieving depressive symptoms. This suggests that future interventions could consider the inclusion of psychotherapeutic elements such as cognitive restructuring and behavioral modification techniques to complement the social media intervention.
Third, this result could be attributed to the lack of between-group significance amongst five studies [97,98,99,100,101]. Two studies [97, 102] also found no remarkable in changes in the baseline scores between the intervention and control groups. Additionally, two studies [83, 103] did not use a power analysis to report their findings. This factor may have led to the lack of statistical power to detect statistical differences between the two groups [104]. Finally, Duffecy et al. (2013) also found a ceiling effect, where participants who had higher depressive symptom scores at baseline demonstrated a greater decrease in scores compared with those with lower scores at baseline [83]. Therefore, the lack of statistical significance in results could have been due to the absence of participant screening.
Use of mobile devices with flexible frequency for social media–based intervention
Using social media on mobile devices increases the accessibility and convenience of social networks for social support [105]. The usage of social media exponentially increases with the high smartphone ownership and internet penetration rates [11]. In the same light, allowing patients the flexibility to access social media gives them the freedom to communicate and seek help from others at any time, especially when they are feeling lonely or worried [106]. This factor could potentially increase their usage of social media; thus, social media–based intervention that are delivered through mobile devices could have a larger effect on quality of life and anxiety symptoms.
More social media features of intervention
Meta-regression analysis showed that having more social media features in interventions improved quality of life scores. Patients have different needs and usage preferences. Some people may prefer sharing data within larger groups, whereas others may prefer to chat in smaller groups or one-to-one with peers [15]. Having a variety of features caters to different preferences and allows social media–based interventions to be more inclusive, which increases the usage of such interventions [107]. Therefore, more patients will benefit from these interventions and have a better quality of life.
Subgroup analysis also showed that interventions with identity representation features have a greater effect on quality of life. Identity representation features involve creating an avatar or the personalisation of online profiles that represents the individual in the community [15]. Being able to identify themselves as patients or survivors of cancer helps patients in accepting and coping with their diagnosis [108]. Furthermore, being able to view the profiles of others gives individuals the control to connect with more like-minded friends, join communities that are more representative of themselves or better able to suit their needs [109]. This factor enables them to form stronger associations and emotional connections within the community and thus have a better quality of life.
Asian countries
Our subgroup analyses showed greater effect sizes on quality of life, anxiety symptoms and depressive symptoms in Asian countries than non-Asian countries. Asian countries are believed to have a collective culture, whereas non-Asian countries lean towards individualistic culture. Cultural differences lead to variations in the usage and preferences of social media platforms [110, 111]. Collective culture leads individuals to prefer using social media to form and deepen relationships, thus providing social support and sharing data with others [112, 113]. On the flip side, individualistic cultures influence individuals to focus more on self-fulfillment and use social media to seek information and entertainment value [112, 113]. Therefore, Asians may tend to participate more actively and form strong bonds with peers in social media–based interventions. This could possibly be attributed to the greater effect of social media–based intervention on quality of life and anxiety symptoms in studies conducted in Asian countries compared with non-Asian countries as seen in the subgroup analysis.
Use of comparator
Subgroup analysis also showed that the usage of usual care comparator had a larger effect on quality of life and anxiety symptoms scores compared with wait-list or active comparators. Compared with usual care, having an intervention could result in greater between-group effects [114]. Furthermore, although the use of active comparator may be more ethical and helps to overcome performance bias, it could dilute the evidence of the effectiveness of the intervention [115]. Waitlist comparator could also perform as well as or even better than the intervention group and thus lead to the unremarkable between-group effects [116]. However, these findings need to be interpreted with caution due to the uneven number of studies in each comparator conditions. Further investigation is needed to ascertain how each condition (e.g. active, usual or waitlist comparators) could affect the effect size.
Implications for practice and policy
Patients diagnosed with cancer face social isolation at different periods of their treatment journey [6], potentially causing elevated psychological symptoms and lower quality of life. Amidst the isolation due to the social restrictions imposed during the COVID-19 pandemic, having a close group of virtual friends to journey alongside and share experiences can help avert feelings of loneliness [9, 10]. This review supports the implementation of social media–based interventions to improve quality of life and anxiety symptoms. Healthcare institutions can consider integrating such interventions into the care plan of patients with cancer in inpatient and outpatient settings. Based on the findings, mobile devices with flexible frequency and having more social media features are the components of social media–based interventions that showed greater improvement in quality of life and anxiety symptoms. Incorporating multiple features, such as blog posting, messaging and photo sharing features on smartphones, can provide diversified social support and drive positive attitude and behavioural change [51]. Therefore, these components can be considered when designing and implementing such interventions for clinical practice and research.
Strengths and limitations
To our knowledge, this systematic review is the first to evaluate the effectiveness of social media–based interventions on the quality of life and psychological outcomes of patients with cancer using meta-analytic methods. An extensive search strategy was used across a large number of databases to ensure a comprehensive search outcome. The risks of bias of the studies were assessed to appraise their quality. This review included a sizeable total number of RCTs across 11 countries. GRADE assessment was undertaken to provide holistic recommendations to other healthcare professionals and researchers. Using subgroup analysis and meta-regression analyses provided information on essential elements that could be used in the future development and research of social media–based interventions.
However, this review has several limitations. Firstly, all outcomes are subjective and were measured using self-reported surveys, which may have led to the social desirability bias of respondents and affected the reliability of the results [117]. Secondly, restricting the language of included studies to English may have limited the generalisation of findings. Thirdly, the population had a wide age group and varied in cancer type, stage and treatment. Furthermore, the design of interventions varied between studies. Substantial heterogeneity and high risk of bias were also found in the majority of the studies. Fourthly, the long-term effect of intervention is based on limited trials that restrict the generalisation of the findings. Next, this review largely focused on social media interventions, and it will be challenging to compare them with traditional psychosocial interventions that are not based on social media. In addition, due to the uneven number of studies in each type of comparators (Figures S3, S5, S7), it will be difficult to conclude which control or comparison conditions can be recommended. Nevertheless, it is recommended that future trials adopt a rigorous approach in the development of their interventions such as the medical research council framework for development of complex interventions [118]. This will ensure that the interventions are suitable to the context, easily implementable and effective for its target audience. Finally, the very low grade of evidence may also reduce the internal validity of the findings.
Conclusion
We conclude that social media–based interventions are effective for improving the quality of life and anxiety symptoms of patients with cancer. Social media–based interventions should contain a mixture of features and be delivered through mobile devices with a flexible frequency to maximise effects. Social media–based interventions enhance the interaction of patients to form social support groups and communities. The results need to be interpreted with caution because of the substantial heterogeneity, high overall risk of bias and low certainty of evidence. As such, future trials should use comprehensive research techniques to enhance the quality of trials. The use of masking, allocation concealment and protocols are recommended. Further investigations into the use of specific social media features for particular cancer types and stages are needed.
Directors for future research
The findings from this review provided some considerations for future research. Firstly, future trials should include elements of a well-designed RCT. This encompasses the use of allocation concealment methods, active control group, blinded researchers, intention-to-treat analysis, missing data management strategies, protocols or trial registries. Most importantly, trials need to be explicit when reporting methods to reduce risks of bias. Trials should also be conducted in accordance with recommendations from the consolidated standards of reporting trials statement [119]. Secondly, future trials can screen participants based on their quality of life, anxiety symptom score or depressive symptom score at baseline, allowing those with poorer outcomes to benefit from the intervention. This is due to the ceiling effect [83]. Thirdly, future trials can consider examining the effectiveness of individual social media feature for improving the quality of life and psychological outcomes of patients with a particular cancer type and stage from different cultures. Lastly, investigation into the inconsistency between meta-analysis and narrative analysis findings with a larger sample of studies can be considered in future research.
References
Sung H, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71(3):209–49.
Devlin EJ, Denson LA, Whitford HS. Cancer treatment side effects: a meta-analysis of the relationship between response expectancies and experience. J Pain Symptom Manag. 2017;54(2):245-258.e2.
Steentjes L, et al. Factors associated with current and severe physical side-effects after prostate cancer treatment: what men report. Eur J Cancer Care. 2018;27(1):e12589.
Binkley JM, et al. Patient perspectives on breast cancer treatment side effects and the prospective surveillance model for physical rehabilitation for women with breast cancer. Cancer. 2012;118(S8):2207–16.
Ettridge KA, et al. “Prostate cancer is far more hidden…”: perceptions of stigma, social isolation and help-seeking among men with prostate cancer. Eur J Cancer Care. 2018;27(2):e12790.
Adams RN, et al. Cancer-related loneliness mediates the relationships between social constraints and symptoms among cancer patients. J Behav Med. 2018;41(2):243–52.
Hamann HA, et al. Stigma among patients with lung cancer: a patient-reported measurement model. Psychooncology. 2014;23(1):81–92.
Frey MK, et al. Impact of the Coronavirus disease 2019 pandemic on the quality of life for women with ovarian cancer. Am J Obstet Gynecol. 2020;223(5):725.e1-9.
Hanghoj S, et al. Adolescents’ and young adults’ experiences of a prototype cancer smartphone app. Digital Health. 2021;7:14.
Grajek M, et al. Feelings related to the COVID-19 pandemic among patients treated in the oncology clinics (Poland). Front Psychol. 2021;12.
Poushter J, Bishop C, Chwe H. Social media use continues to rise in developing countries but plateaus across developed ones. Pew Research Center. 2018.
Chan AKM, et al. Social media for rapid knowledge dissemination: early experience from the COVID-19 pandemic. Anaesthesia. 2020;75(12):1579–82.
Saud M, Mashud MI, Ida R. Usage of social media during the pandemic: seeking support and awareness about COVID-19 through social media platforms. J Public Affairs. 2020;20(4):e2417.
Carr CT, Hayes RA. Social media: defining, developing, and divining. Atlantic J Commun. 2015;23(1):46–65.
Elaheebocus SMRA, et al. Peer-based social media features in behavior change interventions: systematic review. J Med Internet Res. 2018;20(2):e20.
Ball-Rokeach SJ, DeFleur ML. A dependency model of mass-media effects. Commun Res. 1976;3(1):3–21.
Tajfel H. Social identity and intergroup behaviour. Soc Sci Inf. 1974;13(2):65–93.
Morton TA, Duck JM. Communication and health beliefs: mass and interpersonal influences on perceptions of risk to self and others. Commun Res. 2001;28(5):602–26.
Hogg MA, Reid SA. Social identity, self-categorization, and the communication of group norms. Commun Theory. 2006;16(1):7–30.
Hogg MA, Abrams D, Brewer MB. Social identity: the role of self in group processes and intergroup relations. Group Process Intergroup Relat. 2017;20(5):570–81.
Cameron JE. A three-factor model of social identity. Self Identity. 2004;3(3):239–62.
Cohen S, Wills T. Stress, social support, and the buffering hypothesis. Psychol Bull. 1985;98(2):310–57.
Ussher JM, et al. A qualitative analysis of reasons for leaving, or not attending, a cancer support group. Soc Work Health Care. 2008;47(1):14–29.
Leykin Y, et al. Internet interventions for improving psychological well-being in psycho-oncology: Review and recommendations. Psychooncology. 2012;21(9):1016–25.
Joseph JJ, Florea D. Clinical topics in social media: the role of self-disclosing on social media for friendship and identity in specialized populations. In: Malinda D, editor. The Psychology and Dynamics Behind Social Media Interactions. Hershey, PA, USA: IGI Global; 2020. p. 28–56.
Kadambi S, et al. Social support for older adults with cancer: Young International Society of Geriatric Oncology review paper. J Geriatr Oncol. 2020;11(2):217–24.
Korotkin BD, et al. Social support in cancer: how do patients want us to help? J Psychosoc Oncol. 2019;37(6):699–712.
Uchino BN, et al. Psychological pathways linking social support to health outcomes: a visit with the “ghosts” of research past, present, and future. Soc Sci Med. 2012;74(7):949–57.
Lee CS. Exploring emotional expressions on YouTube through the lens of media system dependency theory. New Media Soc. 2012;14(3):457–75.
Kim Y-C, Jung J-Y. SNS dependency and interpersonal storytelling: an extension of media system dependency theory. New Media Soc. 2017;19(9):1458–75.
Ayubi E, Bashirian S, Khazaei S. Depression and anxiety among patients with cancer during COVID-19 pandemic: a systematic review and meta-analysis. J Gastrointest Cancer. 2021;52(2):499–507.
American Psychiatric Association, Diagnostic and statistical manual of mental disorders : DSM-5. 2013, American Psychiatric Association: Arlington, VA.
Nayak MG, et al. Symptom interference and relation between the domains of quality of life among cancer patients of tertiary care hospital. Indian J Palliat Care. 2019;25(4):575–9.
Elting LS, et al. Psychosocial and economic impact of cancer. Dent Clin North Am. 2008;52(1):231–52.
Wang YH, et al. Depression and anxiety in relation to cancer incidence and mortality: a systematic review and meta-analysis of cohort studies. Mol Psychiatry. 2020;25(7):1487–99.
Pinquart M, Duberstein PR. Depression and cancer mortality: a meta-analysis. Psychol Med. 2010;40(11):1797–810.
Aaronson NK, et al. The European Organization for Research and Treatment of Cancer QLQ-C30: a quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst. 1993;85(5):365–76.
Cella DF, et al. The Functional Assessment of Cancer Therapy (FACT) Scale: development and validation of the general measure. J Clin Oncol. 1993;11(3):570–9.
Varni JW, et al. The PedsQL™ in pediatric cancer. Cancer. 2002;94(7):2090–106.
Spielberger CD, Reheiser EC. Measuring anxiety, anger, depression, and curiosity as emotional states and personality traits with the STAI, STAXI and STPI. In: Hilsenroth MJ, Segal DL, editors. Comprehensive Handbook of Psychological Assessment, Volume 2: Personality Assessment. Hoboken, NJ, US: John Wiley & Sons Inc; 2004. p. 70–86.
Beck AT, et al. An inventory for measuring clinical anxiety: Psychometric properties. J Consult Clin Psychol. 1988;56(6):893–7.
Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67(6):361–70.
Beck A, Steer R, Brown G. Manual for the Beck depression inventory-II. 1996, The Psychological Corporation: San Antonio, TX.
Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1(3):385–401.
Lin H, et al. The effectiveness of online interventions for patients with gynecological cancer: An integrative review. Gynecol Oncol. 2020;158(1):143–52.
McAlpine H, et al. A systematic review of types and efficacy of online interventions for cancer patients. Patient Educ Couns. 2015;98(3):283–95.
Tariq A, et al. Assessment of the use of the Internet and social media among people with bladder cancer and their carers, and the quality of available patient-centric online resources: a systematic review. BJU Int. 2019;123(S5):10–8.
Han CJ, Lee YJ, Demiris G. Interventions using social media for cancer prevention and management: a systematic review. Cancer Nurs. 2018;41(6):e19–31.
Koskan A, et al. Use and taxonomy of social media in cancer-related research: a systematic review. Am J Public Health. 2014;104(7):e20–37.
Pellino G, et al. Social media and colorectal cancer: a systematic review of available resources. PLoS One. 2017;12(8):e0183031.
De Clercq E, et al. Moving beyond the friend-foe myth: a scoping review of the use of social media in adolescent and young adult oncology. J Adolesc Young Adult Oncol. 2020;9(5):561–71.
Hamm MP, et al. Social media use among patients and caregivers: a scoping review. BMJ Open. 2013;3:e002819.
The EndNote Team, EndNote. 2013, Clarivate: Philadelphia, PA.
McHugh ML. Interrater reliability: the kappa statistic. Biochemia Medicia. 2012;22(3):276–82.
Higgins JPT, et al. Cochrane handbook for systematic reviews of interventions. 2019, John Wiley & Sons: Chichester (UK).
Higgins JPT, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928.
Stata, A., Stata base reference manual release 14. 2015.
Borenstein M, et al. A basic introduction to fixed-effect and random-effects models for meta-analysis. Res Synth Methods. 2010;1(2):97–111.
Cooper H, Hedges LV, Valentine JC. The handbook of research synthesis and meta-analysis. 2019: Russell Sage Foundation.
Rosenthal R, Cooper H, Hedges L. Parametric measures of effect size. Handb Res Synth. 1994;621(2):231–44.
Hedges LV, Olkin I. Statistical methods for meta-analysis. 2014: Academic press.
Richardson M, Garner P, Donegan S. Interpretation of subgroup analyses in systematic reviews: a tutorial. Clin Epidemiol Global Health. 2019;7(2):192–8.
Morton SC, et al. Meta-regression approaches: what, why, when, and how? 2004, Agency for Healthcare Research and Quality (US), Rockville (MD).
Guyatt G, et al. GRADE guidelines: 1. Introduction—GRADE evidence profiles and summary of findings tables. J Clin Epidemiol. 2011;64(4):383–94.
Sterne JAC, Gavaghan D, Egger M. Publication and related bias in meta-analysis: power of statistical tests and prevalence in the literature. J Clin Epidemiol. 2000;53(11):1119–29.
Torgerson CJ. Publication bias: the Achilles’ heel of systematic reviews? Br J Educ Stud. 2006;54(1):89–102.
Egger M, et al. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–34.
Purssell E, McCrae N. How to perform a systematic literature review: a guide for healthcare researchers, practitioners and students. 1 ed. 2020: Springer International Publishing.
Gustafson DH, et al. Effect of computer support on younger women with breast cancer. J Gen Intern Med. 2001;16(7):435–45.
Chow EJ, et al. Feasibility of a behavioral intervention using mobile health applications to reduce cardiovascular risk factors in cancer survivors: a pilot randomized controlled trial. J Cancer Surviv. 2021;15(4):554–63.
Mendoza JA, et al. A Fitbit and Facebook mHealth intervention for promoting physical activity among adolescent and young adult childhood cancer survivors: a pilot study. Pediatr Blood Cancer. 2017;64(12).
Osei DK, et al. Effects of an online support group for prostate cancer survivors: a randomized trial. Urol Nurs. 2013;33(3):123–33.
Børøsund E, et al. Comparing effects in regular practice of e-communication and Web-based self-management support among breast cancer patients: preliminary results from a randomized controlled trial. J Med Internet Res. 2014;16(12):e295.
Gustafson DH, et al. Internet-based interactive support for cancer patients: are integrated systems better? J Commun. 2008;58(2):238–57.
Syrjala KL, et al. An online randomized controlled trial, with or without problem-solving treatment, for long-term cancer survivors after hematopoietic cell transplantation. J Cancer Surviv. 2018;12(4):560–70.
Omidi Z, et al. Effect of lymphedema self-management group-based education compared with social network-based education on quality of life and fear of cancer recurrence in women with breast cancer: a randomized controlled clinical trial. Qual Life Res. 2020;29(7):1789–800.
Li L, et al. Effect of two interventions on sleep quality for adolescent and young adult cancer survivors: a pilot randomized controlled trial. Cancer Nurs. 2022;45(2):E560–72.
Baker TB, et al. Optimizing eHealth breast cancer interventions: which types of eHealth services are effective? Transl Behav Med. 2011;1(1):134–45.
Mackowski N. Fit survivor: a multicomponent health intervention for adolescent and young adult childhood cancer survivors. 2018, Rutgers The State University of New Jersey, School of Graduate Studies: New Brunswick, New Jersey. p. 92.
Høybye M, et al. Effect of Internet peer-support groups on psychosocial adjustment to cancer: a randomised study. Br J Cancer. 2010;102:1348–54.
Yan FX, et al. Effects of extended care based on the WeChat platform on self-efficacy and quality of life of postoperative breast cancer patients. Indian J Pharm Sci. 2021;83(1):23–30.
Hauffman A, et al. Cocreated internet-based stepped care for individuals with cancer and concurrent symptoms of anxiety and depression: results from the U-CARE AdultCan randomized controlled trial. Psychooncology. 2020;29(12):2012–8.
Duffecy J, et al. Project onward: an innovative e-health intervention for cancer survivors. Psychooncology. 2013;22(4):947–51.
Dong X, et al. The effects of the combined exercise intervention based on internet and social media software (CEIBISMS) on quality of life, muscle strength and cardiorespiratory capacity in Chinese postoperative breast cancer patients: a randomized controlled trial. Health Qual Life Outcomes. 2019;17(1):109.
Stanton AL, et al. Project connect online: randomized trial of an internet-based program to chronicle the cancer experience and facilitate communication. J Clin Oncol. 2013;31(27):3411–7.
Devine KA, et al. Feasibility of FitSurvivor: a technology-enhanced group-based fitness intervention for adolescent and young adult survivors of childhood cancer. Pediatr Blood Cancer. 2020;67(9):e28530.
Farnham S, et al. Hutchworld: clinical study of computer-mediated social support for cancer patients and their caregivers. Conf Human Factors Comput Syst - Proc. 2002;1(1):375–82.
Ruland CM, et al. Effects of an internet support system to assist cancer patients in reducing symptom distress: a randomized controlled trial. Cancer Nurs. 2013;36(1):6–17.
Classen CC, et al. Psychosexual distress in women with gynecologic cancer: a feasibility study of an online support group. Psychooncology. 2013;22(4):930–5.
Wise M, et al. Suffering in advanced cancer: a randomized control trial of a narrative intervention. J Palliat Med. 2018;21(2):200–7.
Hyland KA, et al. Loneliness as a mediator of the relationship of social cognitive variables with depressive symptoms and quality of life in lung cancer patients beginning treatment. Psychooncology. 2019;28(6):1234–42.
Lazard AJ, et al. Using social media for peer-to-peer cancer support: interviews with young adults with cancer. JMIR Cancer. 2021;7(3):e28234.
Khoshnood Z, et al. Getting out or remaining in the cage of inauthentic self: the meaning of existential challenges in patients’ with cancer. Indian J Palliat Care. 2018;24(2):131.
Odh I, Löfving M, Klaeson K. Existential challenges in young people living with a cancer diagnosis. Eur J Oncol Nurs. 2016;24:54–60.
Ang WHD, et al. Path analysis of survivorship care needs, symptom experience, and quality of life among multiethnic cancer survivors. Support Care Cancer. 2021;29(3):1433–41.
Sullivan DR, et al. Longitudinal changes in depression symptoms and survival among patients with lung cancer: a national cohort assessment. J Clin Oncol. 2016;34(33):3984.
Kim HJ, et al. A mobile game for patients with breast cancer for chemotherapy self-management and quality-of-life improvement: randomized controlled trial. J Med Internet Res. 2018;20(10):e273.
Owen JE, et al. Randomized trial of a social networking intervention for cancer-related distress. Ann Behav Med. 2017;51(5):661–72.
Klemm P. Effects of online support group format (moderated vs peer-led) on depressive symptoms and extent of participation in women with breast cancer. CIN: Comput Inform Nurs. 2012;30(1):9–18.
Zhu J, et al. Mobile breast cancer e-support program for Chinese women with breast cancer undergoing chemotherapy (part 2): multicenter randomized controlled trial. JMIR Mhealth Uhealth. 2018;6(4):e104.
Changrani J, et al. Online cancer support groups: experiences with underserved immigrant Latinas. Prim Psychiatry. 2008;15(10):55–62.
Pope Z, et al. Effectiveness of combined smartwatch and social media intervention on breast cancer survivor health outcomes: a 10-week pilot randomized trial. J Clin Med. 2018;7(6):140.
Wright H, et al. A digital self-management program (help to overcome problems effectively) for people living with cancer: feasibility randomized controlled trial. J Med Internet Res. 2021;23(11):e28322.
Forbes LS. A note on statistical power. Auk. 1990;107(2):438–9.
Richards R, et al. Use of mobile devices to help cancer patients meet their information needs in non-inpatient settings: systematic review. JMIR Mhealth Uhealth. 2018;6(12):e10026.
Baker B, Yang I. Social media as social support in pregnancy and the postpartum. Sex Reprod Healthc. 2018;17:31–4.
Moran G, Muzellec L, Johnson D. Message content features and social media engagement: evidence from the media industry. J Product Brand Manag. 2020;29(5):533–45.
Park CL, Zlateva I, Blank TO. Self-identity after cancer: “survivor”, “victim”, “patient”, and “person with cancer.” J Gen Intern Med. 2009;24(Suppl 2):S430–5.
Wheeler SC, Bechler CJ. Objects and self-identity. Curr Opin Psychol. 2021;39:6–11.
Jackson LA, Wang J-L. Cultural differences in social networking site use: a comparative study of China and the United States. Comput Hum Behav. 2013;29(3):910–21.
Kowal M, et al. Reasons for Facebook usage: Data From 46 countries. Front Psychol. 2020;11.
Ji YG, et al. The influence of cultural differences on the use of social network services and the formation of social capital. Int J Human-Comput Interact. 2010;26(11/12):1100–21.
Kim Y, Sohn D, Choi SM. Cultural difference in motivations for using social network sites: a comparative study of American and Korean college students. Comput Hum Behav. 2011;27(1):365–72.
Mohr DC, et al. The selection and design of control conditions for randomized controlled trials of psychological interventions. Psychother Psychosom. 2009;78(5):275–84.
Temple R, Ellenberg SS. Placebo-controlled trials and active-control trials in the evaluation of new treatments. Part 1: Ethical and scientific issues. Ann Intern Med. 2000;133(6):455–63.
Cunningham JA, Kypri K, McCambridge J. Exploratory randomized controlled trial evaluating the impact of a waiting list control design. BMC Med Res Methodol. 2013;13(1):150.
Latkin CA, et al. The relationship between social desirability bias and self-reports of health, substance use, and social network factors among urban substance users in Baltimore. Maryland Addict Behav. 2017;73:133–6.
Skivington K, et al. A new framework for developing and evaluating complex interventions: update of Medical Research Council guidance. Bmj. 2021;374.
Schulz KF, Altman DG, Moher D. CONSORT 2010 Statement: updated guidelines for reporting parallel group randomised trials. BMC Med. 2010;8:18.
Acknowledgements
We would like to thank authors for sending further information on their studies for the purpose of our systematic review
Author information
Authors and Affiliations
Contributions
Li En Dana Siew: conceptualization, investigation, data curation, formal analysis, writing—original draft. Neil Russell Teo: data curation, writing—original draft. Wei How Darryl Ang: formal analysis, software, writing—original draft, writing—review and editing. Ying Lau: conceptualization, methodology, software, formal analysis, writing—original draft, writing—review and editing, supervision, project administration.
Corresponding author
Ethics declarations
Ethical approval
Not required.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Siew, L.E.D., Teo, N.R., Ang, W.H.D. et al. Social media–based interventions for patients with cancer: a meta-analysis and meta-regression of randomised controlled trials. J Cancer Surviv 17, 1606–1627 (2023). https://doi.org/10.1007/s11764-022-01244-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11764-022-01244-6