Abstract
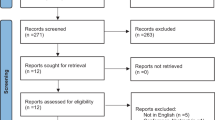
Wearable sensory-feedback technology has been shown to improve walking in individuals with neurological conditions. This study examined the feasibility and acceptability of procedures to use this technology with older adults who have fear of falling. Recruitment, retention, measurement, and intervention procedures were assessed in a single-center, pre-post, within-subject design study. Older adults with fear of falling were recruited to use wearable sensory feedback technology during a single session conducted in a laboratory setting under the supervision of a physical therapist. Objective measures consisted of gait and posture measures that were made at three time-points during the study session: “baseline,” “during” (after training, while wearing the device), and “post” (after the second assessment following removal of the device). Participants ended the session by reporting on their perceptions of the technology. Twenty-four participants were enrolled over a period of 12 months. All enrolled participants were able to complete the study protocol without adverse or unexpected events. Participants provided favorable feedback indicating that it was easy to find a natural rhythm for walking while using the technology. Small to moderate effect sizes were obtained regarding pre-post increases in cadence and double support time and decreases in single limb stance time. Overall, intervention procedures were found to be feasible and acceptable but preliminary data did not point to improvements in gait or balance, i.e., the direction of the effects suggested of pre-post worsening of gait. Areas for improvement were identified that may inform the design and execution of future studies with this patient population.

Similar content being viewed by others
References
Paraskevoudi N, Balci F, Vatakis A. “Walking” through the sensory, cognitive, and temporal degradations of healthy aging. Ann N Y Acad Sci. 2018;1426:72–92.
Herssens N, Verbecque E, Hallemans A, Vereeck L, Rompaey VV, Saeys W. Do spatiotemporal parameters and gait variability differ across the lifespan of healthy adults? A systematic review. Gait Posture. 2018;64:181–90.
Osoba M, Rao A, Agrawal S, Lalwani A. Balance and gait in the elderly: A contemporary review. Laryngoscope Investigative Otolaryngology. 2019;4:143–53.
Kujala UM, Hautasaari P, Vähä-Ypyä H, Waller K, Lindgren N, Iso-Markku P, Heikkilä K, Rinne J, Kaprio J, Sievänen H. Chronic diseases and objectively monitored physical activity profile among aged individuals – a cross-sectional twin cohort study. Ann Med. 2019;51(1):78. https://doi.org/10.1080/07853890.2019.1566765.
George C, Verghese J. Polypharmacy and Gait Performance in Community-dwelling Older Adults. J Am Geriatr Soc. 2017;65:2082–7.
Rantakokko M, Wilkie R. Environmental Factors and Onset of Restricted Mobility Outdoors in Older Adults with Osteoarthritis. Innov Aging. 2017;1:453–453.
Satariano WA, Guralnik JM, Jackson RJ, Marottoli RA, Phelan EA, Prohaska TR. Mobility and aging: new directions for public health action. Am J Public Health. 2012;102:1508–15.
Katzmarzyk PT. Physical activity, sedentary behavior, and health: paradigm paralysis or paradigm shift? Diabetes. 2010;59:2717–25.
Haddad YK, Bergen G, Florence CS. Estimating the Economic Burden Related to Older Adult Falls by State. J Public Health Manag Pract. 2018. https://doi.org/10.1097/PHH.0000000000000816.
Lach HW. Incidence and Risk Factors for Developing Fear of Falling in Older Adults. Public Health Nurs. 2005;22:45–52.
Patel K, Phelan E, Leveille S, Wallace R, Missikpode C, Lamb S, Guralnik J, Turk D. High prevalence of falls, fear of falls, and impaired balance among older adults with pain in the United States: findings from the 2011 National Health and Aging Trends Study. J Am Geriatr Soc. 2014;62:1844–52.
Boyd R, Stevens JA. Falls and fear of falling: burden, beliefs and behaviours. Age Ageing. 2009;38:423–8.
Arfken CL, Lach HW, Birge SJ, Miller JP. The prevalence and correlates of fear of falling in elderly persons living in the community. Am J Public Health. 1994;84:565–70.
Kressig RW, Wolf SL, Sattin RW, Ogrady M, Greenspan A, Curns A, Kutner M. Associations of Demographic, Functional, and Behavioral Characteristics with Activity-Related Fear of Falling Among Older Adults Transitioning to Frailty. J Am Geriatr Soc. 2001;49:1456–62.
Chamberlin ME, Fulwider BD, Sanders SL, Medeiros JM. Does Fear of Falling Influence Spatial and Temporal Gait Parameters in Elderly Persons Beyond Changes Associated With Normal Aging? J Gerontol A Biol Sci Med Sci. 2005;60:1163–7.
Tiedemann A, Sherrington C, Lord SR. Physiological and Psychological Predictors of Walking Speed in Older Community-Dwelling People. Gerontology. 2005;51:390–5.
Delbaere K, Sturnieks DL, Crombez G, Lord SR. Concern about falls elicits changes in gait parameters in conditions of postural threat in older people. Journal of Gerontology: Medical Sciences. 2009;64A:237–42.
Reelick MF, Iersel MBV, Kessels RPC, Rikkert MGMO. The influence of fear of falling on gait and balance in older people. Age Ageing. 2009;38:435–40.
Rochat S, Büla CJ, Martin E, Seematter-Bagnoud L, Karmaniola A, Aminian K, Piot-Ziegler C, Santos-Eggimann B. What is the Relationship Between Fear of Falling and Gait in Well-Functioning Older Persons Aged 65 to 70 Years? Arch Phys Med Rehabil. 2010;91:879–84.
Kirkwood RN, Moreira BDS, Vallone ML, Mingoti SA, Dias RC, Sampaio RF. Step length appears to be a strong discriminant gait parameter for elderly females highly concerned about falls: a cross-sectional observational study. Physiotherapy. 2011;97:126–31.
Donoghue OA, Cronin H, Savva GM, O’Regan C, Kenny RA. Effects of fear of falling and activity restriction on normal and dual task walking in community dwelling older adults. Gait Posture. 2013;38:120–4.
Bueno G, Gervásio F, Ribeiro D, Martins A, Lemos T, de Menezes R. Fear of Falling Contributing to Cautious Gait Pattern in Women Exposed to a Fictional Disturbing Factor: A Non-randomized Clinical Trial. Front Neurol. 2019;10:283.
Binda SM, Culham EG, Brouwer B. Balance, Muscle Strength, and Fear of Falling in Older Adults. Exp Aging Res. 2003;29:205–19.
Hadjistavropoulos T, Carleton RN, Delbaere K, Barden J, Zwakhalen S, Fitzgerald B, Ghandehari OO, Hadjistavropoulos H. The relationship of fear of falling and balance confidence with balance and dual tasking performance. Psychol Aging. 2012;27:1–13.
Uemura K, Yamada M, Nagai K, Tanaka B, Mori S, Ichihashi N. Fear of falling is associated with prolonged anticipatory postural adjustment during gait initiation under dual-task conditions in older adults. Gait Posture. 2012;35:282–6.
Ayoubi F, Launay C, Annweiler C, Fantino B, Kabeshova A, Beauchet O. Fear of Falling, Falls, and Gait Variability in Older Community-Dwelling Individuals: Is There an Association? J Am Geriatr Soc. 2013;61:1236–8.
Stevens JA, Phelan EA. Development of STEADI. Health Promot Pract. 2012;14:706–14.
Province MA. The effects of exercise on falls in elderly patients. A preplanned meta-analysis of the FICSIT Trials. Frailty and Injuries: Cooperative Studies of Intervention Techniques. JAMA: J Am Med Assoc. 1995;273:1341–1347.
Zijlstra GAR, Haastregt JCMV, Ambergen T, Rossum EV, Eijk JTMV, Tennstedt SL, Kempen GIJM. Effects of a Multicomponent Cognitive Behavioral Group Intervention on Fear of Falling and Activity Avoidance in Community-Dwelling Older Adults: Results of a Randomized Controlled Trial. J Am Geriatr Soc. 2009;57:2020–8.
Yang W-C, Wang H-K, Wu R-M, Lo C-S, Lin K-H. Home-based virtual reality balance training and conventional balance training in Parkinson’s disease: A randomized controlled trial. J Formos Med Assoc. 2016;115:734–43.
Corbetta D, Imeri F, Gatti R. Rehabilitation that incorporates virtual reality is more effective than standard rehabilitation for improving walking speed, balance and mobility after stroke: a systematic review. J Physiother. 2015;61:117–24.
Mirelman A, Maidan I, Herman T, Deutsch JE, Giladi N, Hausdorff JM. Virtual Reality for Gait Training: Can It Induce Motor Learning to Enhance Complex Walking and Reduce Fall Risk in Patients With Parkinson’s Disease? J Gerontol A Biol Sci Med Sci. 2011;66A:234–40.
Baram Y, Aharon-Peretz J, Simionovici Y, Ron L. Walking on virtual tiles. Neural Process Lett. 2002;16:227–33.
Chong R, Lee K-H, Morgan J, Mehta S. Closed-Loop VR-Based Interaction to Improve Walking in Parkinson’s Disease. Journal of Novel Physiotherapies. 2011. https://doi.org/10.4172/2165-7025.1000101.
Espay AJ, Baram Y, Dwivedi AK, Shukla R, Gartner M, Gaines L, Duker AP, Revilla FJ. At-home training with closed-loop augmented-reality cueing device for improving gait in patients with Parkinson disease. The Journal of Rehabilitation Research and Development. 2010;47:573.
Badarny S, Aharon-Peretz J, Susel Z, Habib G, Baram Y. Virtual reality feedback cues for improvement of gait in patients with Parkinson’s disease. Tremor and Other Hyperkinetic Movements. 2014;4:225.
Baram Y, Miller A. Virtual reality cues for improvement of gait in patients with multiple sclerosis. Neurology. 2006;66:178–81.
Baram Y, Miller A. Glide-symmetric locomotion reinforcement in patients with multiple sclerosis by visual feedback. Disabil Rehabil Assist Technol. 2010;5:323–6.
Baram Y, Lenger R. Gait Improvement in Patients with Cerebral Palsy by Visual and Auditory Feedback. Neuromodulation: Technol Neural Interf. 2012;15:48–52.
Baram Y, Aharon-Peretz J, Lenger R. Virtual Reality Feedback for Gait Improvement in Patients with Idiopathic Senile Gait Disorders and Patients with History of Stroke. J Am Geriatr Soc. 2010;58:191–2.
Young WR, Williams AM. How fear of falling can increase fall-risk in older adults: Applying psychological theory to practical observations. Gait Posture. 2015;41:7–12.
Jefferis BJ, Iliffe S, Kendrick D, et al. How are falls and fear of falling associated with objectively measured physical activity in a cohort of community-dwelling older men? BMC Geriatr. 2014. https://doi.org/10.1186/1471-2318-14-114.
Balaban C, Furman J, Staab J. Threat Assessment and Locomotion: Clinical Applications of an Integrated Model of Anxiety and Postural Control. Semin Neurol. 2013;33:297–306.
Hadjistavropoulos T, Delbaere K, Fitzgerald TD. Reconceptualizing the Role of Fear of Falling and Balance Confidence in Fall Risk. J Aging Health. 2010;23:3–23.
Martens KAE, Ellard CG, Almeida QJ. Does Anxiety Cause Freezing of Gait in Parkinson’s Disease? PLoS ONE. 2014. https://doi.org/10.1371/journal.pone.0106561.
Martens KAE, Ellard CG, Almeida QJ. Anxiety-provoked gait changes are selectively dopa-responsive in Parkinson’s disease. Eur J Neurosci. 2015;42:2028–35.
Martens KAE, Ellard CG, Almeida QJ. Virtually-induced threat in Parkinson’s: Dopaminergic interactions between anxiety and sensory–perceptual processing while walking. Neuropsychologia. 2015;79:322–31.
Velu PD, Mullen T, Noh E, Valdivia MC, Poizner H, Baram Y, Sa VRD. Effect of Visual Feedback on the Occipital-Parietal-Motor Network in Parkinson’s Disease with Freezing of Gait. Front Neurol. 2014. https://doi.org/10.3389/fneur.2013.00209.
Yardley L, Beyer N, Hauer K, Kempen G, Piot-Ziegler C, Todd C. Development and initial validation of the Falls Efficacy Scale-International (FES-I). Age Ageing. 2005;34:614–9.
Folstein MF, Folstein SE, White T, Messer MA. Mini-mental state examination user's manual. Psychologic Assess Resour. 2010.
Brodie MA, Dean RT, Beijer TR, Canning CG, Smith ST, Menant JC, Lord SR. Symmetry matched auditory cues improve gait steadiness in most people with Parkinson’s disease but not in healthy older people. J Parkinson’s Dis. 2015;5:105–16.
Delbaere K, Close JCT, Mikolaizak AS, Sachdev PS, Brodaty H, Lord SR. The Falls Efficacy Scale International (FES-I). A comprehensive longitudinal validation study. Age Ageing. 2010;39:210–6.
Spielberger CD, Sydeman SJ. State-Trait Anger Expression Inventory. ME Maruish (Ed), The use of psychological testing for treatment planning and outcome assessment. 2010;292–321.
Radloff LS. The CES-D Scale. Appl Psychol Meas. 1977;1:385–401.
World Health Organization. World Health Organization Disability Assessment Schedule (WHODAS) 2.0. Geneva: World Health Organization. 2012.
Duque G, Boersma, Loza-Diaz, Hassan, Suarez H, Geisinger, Suriyaarachchi, Sharma, Demontiero. Effects of balance training using a virtual-reality system in older fallers. Clinic Intervent Aging. 2013;257–263.
Levy F, Rautureau G, Komano O, Millet B, Jouvent R, Leboucher P. Fear of falling: efficacy of virtual reality associated with serious games in elderly people. Neuropsych Dis Treat. 2016;877–881.
Hollman JH, Mcdade EM, Petersen RC. Normative spatiotemporal gait parameters in older adults. Gait Posture. 2011;34:111–8.
Chen Y, Gao Q, He C, Bian R. Effect of Virtual Reality on Balance in Individuals With Parkinson Disease: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Phys Ther. 2020;100:933–45.
Tuerk C, Zhang H, Sachdev P, Lord SR, Brodaty H, Wen W, Delbaere K. Regional Gray Matter Volumes Are Related to Concern About Falling in Older People: A Voxel-Based Morphometric Study. J Gerontol A Biol Sci Med Sci. 2015;71:138–44.
Acknowledgements
Preliminary findings from this study were presented as a scientific poster at the Annual Meeting of the Gerontological Society of America in New Orleans on November 20, 2013. The authors thank Dr. Yoram Baram for providing the sensory feedback device used in this study and for his input on its use in the study.
Funding
This study was funded by internal grant awards by Cornell-Technion Institute and Weill Cornell Medical College to Dr. Jayasinghe and Dr. Yoram Baram. The funder had no involvement in the study design, analysis and interpretation of data, writing of this report, or decision to publish.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None of the investigators have conflicts of interest to report.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Jayasinghe, N., Backus, S., Gibbons, M. et al. Brief training of gait and posture using a wearable sensory feedback device with older adults who have fears of falling: A feasibility study. Health Technol. 12, 433–442 (2022). https://doi.org/10.1007/s12553-021-00623-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12553-021-00623-w