Medical Care
When hiatal hernias are symptomatic, acid reflux usually produces the symptoms. If the hernia itself is causing chest discomfort or other symptoms, surgery may be necessary.
When symptoms are due to GERD, the goals of treatment include prevention of reflux of gastric contents, improved esophageal clearance, and reduction in acid production. This is achieved in the majority of patients by a combination of the following:
-
Modifying lifestyle factors
-
Neutralizing acid or inhibiting acid production
-
Enhancing esophageal and gastric motility
The treatment of GERD is beyond the scope of this article and is discussed in Gastroesophageal Reflux Disease.
Large hiatal hernias may cause iron deficiency anemia regardless of whether Cameron ulcers are present. This anemia responds well to PPI therapy with surgery offering no clear advantage over medical therapy.
Surgical Care
The goal of surgery is to remove the hernia sac and close the abnormally wide esophageal hiatus.
Surgery is necessary only in the minority of patients with complications of GERD despite aggressive treatment with proton pump inhibitors (PPIs). Because only a minority of patients with hiatal hernia have any problems, this represents a very small proportion of patients with sliding hiatal hernia; most patients with problems are managed medically.
By far, the majority of patients who would have undergone surgery in the past are managed successfully today with PPIs. However, young patients with severe or recurrent complications of GERD, such as strictures, ulcers, and bleeding, who cannot afford lifelong PPI treatment or would prefer to avoid taking medications long term, may be surgical candidates. Another group of patients who are surgical candidates are those with pulmonary complications, in particular, asthma, recurrent aspiration pneumonia, chronic cough, or hoarseness linked to reflux disease.
Most patients with a paraesophageal hernia remain asymptomatic. In this type of hernia, symptoms from acid reflux usually do not occur. Instead, the most common symptom is epigastric or substernal pain. Some patients complain of substernal fullness, nausea, and dysphagia. A significant proportion of patients with this type of hernia develop incarceration of the hernia and possible gastric volvulus, which can lead to perforation. If perforation occurs, the mortality rate is high. Because of this, many surgeons advise elective repair when the diagnosis is made.
A patient with a large hiatal hernia may experience vague intermittent chest discomfort or pain. The paraesophageal hernia may strangulate and frequently is operated on prophylactically to prevent this complication. Paraesophageal hernias may present in infants or adults as a potentially life-threatening complication of strangulation, and prompt surgical repair is key. When found in asymptomatic individuals, laparoscopic repair is often undertaken, with large defects in the diaphragm being closed with mesh. [9, 10, 11, 12]
Three major types of surgical procedures correct gastroesophageal reflux and repair the hernia in the process. They can be performed by open laparotomy or with laparoscopic approaches, which currently are being employed more frequently. These procedures offer relief of symptoms in 80-90% of patients.
In most cases, the procedure of choice is the one with which the surgeon is most familiar. These procedures carry low mortality and morbidity rates, lower than 15-20%.
A systematic review and meta-analysis of 4 trials comprising 406 patients found comparable results and outcomes between suture cruroplasty and prosthetic hiatal herniorrhaphy for large hiatal hernia closure. [13] In another study consisting of data from 65 patients over nearly two decades, left thoracoscopic Collis gastroplasty-laparoscopic Nissen (Collis-Nissen) procedure and conventional laparoscopic Nissen fundoplication yielded similarly satisfactory results in uncomplicated patients with true short esophagus in the setting of gastroesophageal reflux disease and type III-IV hiatal hernia. [14]
In another systematic study and meta-analysis of mesh (n=673) versus suture (n=521) cruroplasty during laparoscopic large hiatal hernia repair, data from 13 studies consisting of 1194 patients showed symptomatic improvement in most studies, with fewer odds of recurrence but not need for reoperation with mesh cruroplasty. [15] However, the quality of the evidence for supporting routine use of mesh cruroplasty was low.
DeMeester et al found the Nissen procedure superior to the Belsey and Hill repairs with regard to symptom relief and prevention of reflux postoperatively (as judged by pH monitoring). Good long-term results have been reported for antireflux surgery, with adequate control of reflux in the range of 80% at 10 years.
See the video below for a discussion of surgical options for paraesophageal hernia repair.
Recurrent paraesophageal hernia (PEH) repair is performed for symptomatic recurrent hiatal hernia and/or reflux and appears to have similar outcomes to those of initial PEH, although increased operative time, blood loss, persistent symptoms, and need for Collis gastroplasty occurred more often in those who underwent revisional repair. [16]
Nissen fundoplication
The Nissen fundoplication performed laparoscopically has gained popularity because of its lower morbidity and shorter hospital stay compared to the open procedure performed previously. Although a relatively high incidence of postoperative complications, such as dysphagia and gas bloating, are reported, DeMeester and Peters [17] have shown that placing a larger bougie in the esophagus during this procedure, along with a shorter wrap and more complete mobilization of the stomach, have markedly reduced postoperative complications. [18, 19]
This procedure involves a 360° fundic wrap around the gastroesophageal junction. The diaphragmatic hiatus also is repaired.
A transthoracic approach may be used in patients who have had a previous Nissen wrap or those who have an irreducible hernia.
In a study involving 26 patients who underwent Nissen fundoplication, the use of permanent mesh following fundoplication resulted in symptom improvement in 23 patients (88.5%), with hernia recurrence reported by the remaining three patients (11.5%). No mesh erosions occurred during the mean 65-month follow-up period. [20]
The Toupet procedure is a variant of the Nissen wrap and involves a 180° wrap in an attempt to lessen the likelihood of postoperative dysphagia.
Belsey fundoplication
This operation involves a 270° wrap in an attempt to reduce the incidence of gas bloating and postoperative dysphagia. It also is preferred when minimal esophageal dysmotility is suspected. To complete this operation, the left and right crura of the diaphragm are approximated.
Hill repair
In this procedure, the cardia of the stomach is anchored to the posterior abdominal areas, such as the medial arcuate ligament. This also has the effect of augmenting the angle of His and thus strengthening the antireflux mechanism.
Some surgeons then tack the stomach down in the abdomen to prevent it from migrating upwards again, or, they perform a temporary gastrostomy to help decompress the stomach and anchor it in place in the abdominal cavity.
Magnetic Sphincter Augmentation
Magnetic sphincter augmentation (MSA) is an innovative surgical procedure in which a small, flexible band of magnetic titanium beads is implanted around the esophagus laparoscopically (see the images below). The band augments a weak lower esophageal sphincter (LES). The magnetic attraction between the beads prevents reflux of gastric contents but is weak enough to allow for swallowing, belching or vomiting. MSA has been shown to be effective to control GERD symptoms and to reduce esophageal acid exposure. In a systemic review and meta-analysis involving 1211 patients, both anti-reflux procedures are safe and effective up to 1-year follow-up. PPI suspension rate, dysphagia requiring endoscopic dilatation, and disease-related quality of life are similar in the two patient groups. MSA is associated with less gas/bloat symptoms and increased ability to vomit and belch. [21]
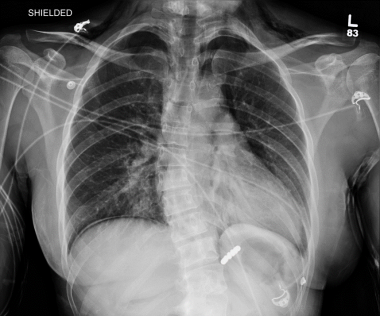 Hiatal Hernia. This image demonstrates a Linx device in place on x-ray. Courtesy of Shawn S Groth, MD, MS, FACS.
Hiatal Hernia. This image demonstrates a Linx device in place on x-ray. Courtesy of Shawn S Groth, MD, MS, FACS.
Diet
An appropriate diet maintains an ideal body mass index. Obesity predisposes to reflux disease.
Burkitt et al suggest that the Western, fiber-depleted diet leads to a state of chronic constipation and straining during bowel movement, which would explain the higher incidence of this condition in Western countries. [3]
-
Hiatal Hernia. Figure 1 shows the normal relationship of the gastroesophageal (GE) junction, stomach, esophagus, and diaphragm. Figure 2 shows a sliding hiatal hernia, in which the stomach immediately below the GE junction is seen to prolapse through the diaphragmatic hiatus into the chest. Figure 3 shows a paraesophageal hernia in which the cardia or fundus of the stomach prolapses through the diaphragmatic hiatus, leaving the GE junction within the esophageal cavity.
-
Hiatal Hernia. These anteroposterior (left) and lateral views (right) on a chest radiograph showing a large hiatal hernia. Courtesy of David Y Graham, MD.
-
Hiatal Hernia. This barium study shows a sliding hiatal hernia: The gastric folds can be seen extending above the diaphragm. GE = gastroesophageal. Courtesy of David Y Graham, MD.
-
Hiatal Hernia. A paraesophageal hernia is seen on an upper gastrointestinal radiograph series. Note that the gastroesophageal (GE) junction remains below the diaphragm. Courtesy of David Y Graham, MD.
-
Hiatal Hernia. A paraesophageal hernia is seen on a barium upper gastrointestinal radiograph series. The mucosal folds are seen going up into the chest, next to the esophagus. GE = gastroesophageal. Courtesy of David Y Graham, MD.
-
Hiatal Hernia. This image is a barium radiograph view of a large paraesophageal hernia. GE = gastroesophageal. Courtesy of David Y Graham, MD.
-
Hiatal Hernia. This barium radiograph shows a large paraesophageal hernia in which the entire stomach is seen in the chest cavity. Courtesy of David Y Graham, MD.
-
Hiatal Hernia. These barium studies show gastric volvulus as the herniated stomach undergoes rotation. This situation requires surgical intervention. Courtesy of David Y Graham, MD.
-
Hiatal Hernia. A retrograde view of a hiatal hernia seen at endoscopy shows the gastric folds to the left of the scope shaft extending up into the hernia. Courtesy of David Y Graham, MD.
-
Hiatal Hernia. Inderpal S Sarkaria, MD, discusses the options for paraesophageal hernia repair. Courtesy of Memorial Sloan-Kettering Cancer Center.
-
Hiatal Hernia. This image shows a Linx device in place during laparoscopic surgery. Courtesy of Shawn S Groth, MD, MS, FACS.
-
Hiatal Hernia. This image demonstrates a Linx device in place on x-ray. Courtesy of Shawn S Groth, MD, MS, FACS.









