Background
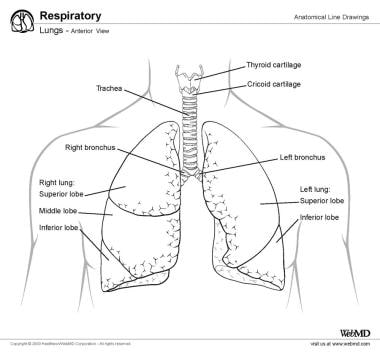
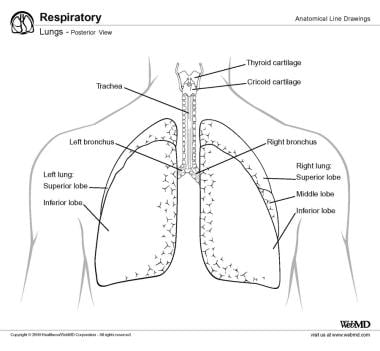
Although many newer imaging techniques for the evaluation of lung pathology have been developed (eg, ultrasonography of the lung [1] ), auscultation of the chest remains an invaluable clinical tool and is still probably the most common method of evaluating the lung. Evaluation of lung sounds is a routine part of a clinical examination. Relevant lung anatomy is depicted in the images below.
Breath sounds can be classified into the following two broad categories [2, 3] :
-
Normal breath sounds
-
Adventitious (or abnormal) sounds - These include wheezes, coarse crackles, fine crackles, and rhonchi
Technique
A significant amount of information about the upper and lower airways and lung parenchyma can be obtained by listening to the chest. If possible, auscultation of the chest should be done with the patient in the seated position. The diaphragm of the stethoscope should be used. The examiner should warm the stethoscope between his or her palms before placing it on the patient's chest. The stethoscope should be placed against the patient’s bare skin; the examiner should not try to listen through the patient's clothes. (See the video below.)
The examination should include listening to the anterior chest, the midaxillary region, and the posterior chest. The posterior chest should be examined from the apex to the base of the chest. The breath sounds should be assessed during both quiet and deep breathing. A full breath should be auscultated in each location. The examiner should listen for the pitch, intensity, duration, and distribution of breath sounds, as well as note any abnormal or adventitious sounds. [4, 5]
Computer-assisted methods of lung sound analysis may augment the accuracy of lung auscultation. [6, 7] Such methods may be particularly promising for diagnosing and monitoring infectious diseases such as COVID-19. [8]
Normal vs Abnormal (Adventitious) Breath Sounds
Breath sounds can be divided into two categories: normal and abnormal (adventitious). [9]
Normal breath sounds
Normal breath sounds can be further divided into two subcategories: vesicular and tracheal. Vesicular breath sounds are the sounds heard during auscultation of the chest of a healthy person (listen to the audio recording below). The inspiratory component predominates and is generated by turbulent airflow within the lobar and segmental bronchi, whereas the expiratory component is due to flow within the larger airways.
Vesicular breath sounds (MP3) Audio courtesy of MEDiscuss.
Tracheal sounds are the sounds heard over the sternum. They are louder and higher-pitched than vesicular sounds are. With tracheal sounds, the expiratory phase is as long as or longer than the inspiratory phase. [4, 5, 10]
Abnormal (adventitious) breath sounds
Wheeze
A wheeze is defined as a continuous musical sound lasting longer than 250 ms (listen to the audio recording below). It is thought to be due to oscillation of opposing airway walls that are narrowed almost to the point of contact. A wheeze may be either expiratory or inspiratory and may contain either a single note or multiple notes. Wheezing is common, estimated to occur in 25% of the population at some point. It is frequently more audible at the trachea than in the chest. [11]
Wheeze (MP3) Audio courtesy of MEDiscuss.
Clinically, wheezing indicates airflow obstruction, though its absence does not exclude obstruction. [12] Such obstruction may occur at any point along the airway. Conditions associated with wheezing include the following:
-
Infection ( croup, whooping cough, bronchiolitis)
-
Laryngeal or tracheal tumors
-
Other causes of large airway compression or stenosis
A wheeze may be detected during forced expiration in normal subjects. Although wheezing is associated with airflow obstruction, the degree of obstruction cannot be reliably predicted by the presence or absence of wheezing. Generally, a polyphonic wheeze (ie, a wheeze with multiple notes) is characteristic of large airway obstruction, whereas a monophonic wheeze is more typical of small airway obstruction. [10, 11]
A study by Kevat et al found that the use of digital stethoscopes was superior to standard auscultation for detecting wheeze in children. [15] Digital stethoscopes have also been used to assess breath sounds at birth. [16]
Squawk
A squawk is defined as a very short wheeze. It is thought to occur when a closed airway suddenly opens during inspiration and the airway walls briefly remain in light contact. Squawks are most common in fibrotic disorders, particularly hypersensitivity pneumonitis. [11]
Crackles
Crackles are defined as a short, explosive, nonmusical sound (listen to the audio recording below). They can be divided into two types: fine and coarse. Compared with coarse crackles, fine crackles have a higher frequency and a shorter duration. Fine crackles are caused by the sudden opening of a closed airway; coarse crackles are thought to be related to secretions.
Crackles (MP3) Audio courtesy of MEDiscuss.
Crackles may occur on either inspiration or expiration but are more common during inspiration. Inspiratory crackles may be classified as early inspiratory, midinspiratory, or late inspiratory. Crackles are more frequently heard in the basilar regions of the lungs because the distribution of airway closure is gravity-dependent.
The number of crackles has been shown to correlate with disease severity. Crackles may be heard in cardiac disease, fibrotic lung disease, obstructive lung disease, and pulmonary infections. They may also be heard in healthy older individuals. [10, 17]
General characteristics of these crackles have been described for many different disorders (though there may be variations among individual patients). In idiopathic pulmonary fibrosis, crackles have been described as fine, short in duration, higher-pitched, and occurring in late inspiration. A basilar predominance exists in early disease.
Asbestosis is associated with fine crackles. The presence of crackles has been shown to be associated with honeycombing on imaging and with the duration of dust exposure. In bronchiectasis, crackles have been described as high-frequency and coarse. They occur in early inspiration or midinspiration and are thought to be secondary to bronchial wall collapse during expiration and sudden opening in inspiration.
In COPD, crackles are most commonly due to airway secretions and typically disappear after coughing; they may also be due to the opening and closing of narrowed bronchi with weakened airway walls. Crackles in COPD are characterized as coarse, early, and low-pitched and tend to be infrequent.
The crackles associated with pulmonary edema are attributed to the opening of airways narrowed by peribronchial edema. They are described as coarse, late-occurring, and high-pitched. They may be inspiratory or expiratory.
In pneumonia, two types of crackles have been described. Early pneumonia is associated with coarse, midinspiratory crackles; crackles during the recovery phase are described as shorter and occurring at the end of expiration.
Crackles are relatively rare with sarcoidosis (because of the upper-lobe predominance of the disease); when they do occur, they are described as fine and either late inspiratory or midinspiratory. [17]
Rhonchi
Rhonchi are defined as low-pitched continuous sounds that have a tonal, sonorous quality. They are caused by the rupture of fluid films and airway wall vibrations and are associated with disorders that cause increased airway secretion or reduced clearance of secretions. Rhonchi tend to clear with coughing. [4, 10]
Stridor
Stridor is defined as a high-pitched continuous sound heard over the trachea. It is due to turbulent flow generated in the upper airway during extrathoracic airway obstruction, and it tends to occur when the upper airway is narrowed to 5 mm or less. Stridor is louder than wheezing, and it is longer in inspiration than in expiration. It may be caused by any condition that leads to narrowing of the extrathoracic airway. [10]
Other abnormal sounds
Pulmonary parenchymal consolidation may cause several changes in the quality of breath sounds. Bronchial breath sounds are breath sounds that are overly well transmitted to the chest wall as a consequence of increased sound transmission through the consolidated lung parenchyma (listen to the audio recordings below). These sounds are described as similar to tracheal sounds and are loud, high-pitched, tubular, and whistling. Expiration is as loud as, or louder than, inspiration.
Bronchial breath sounds (MP3) Audio courtesy of MEDiscuss.
Bronchovesicular breath sounds (MP3) Audio courtesy of MEDiscuss.
Consolidation also leads to changes in voice-generated sounds. Normally, the spoken voice has a muffled, indistinct quality when heard during auscultation of the chest. With a consolidated lung, the voice may take on a high-pitched, bleating quality (egophony) or may exhibit increased pitch or transmission of words (bronchophony or pectoriloquy). The so-called E-to-A sign has also been described, in which a spoken “E” sounds like “A” on auscultation of the abnormal area. [10]
Several conditions are associated with a decrease in or absence of normal breath sounds. Diffusely decreased breath sounds may be noted in conditions that alter the transmission of sound through the chest wall (eg, obesity), as well as in obstructive lung disease. A focal decrease or absence in breath sounds may be due to pleural effusion, pneumothorax, or atelectasis. [10]
-
Anterior view of lungs and trachea.
-
Posterior view of lungs and trachea.
-
Breath sound assessment. Courtesy of Therese Canares, MD, and Jonathan Valente, MD, Rhode Island Hospital, The Warren Alpert Medical School of Brown University.