Effects of high-intensity and moderate-intensity exercise training on cardiopulmonary function in patients with coronary artery disease: A meta-analysis
- 1National Clinical Research Center for Chinese Medicine Cardiology, Xiyuan Hospital, China Academy of Chinese Medical Sciences, Beijing, China
- 2Graduate School of Beijing University of Traditional Chinese Medicine, Beijing, China
Purpose: The study aims to evaluate the effects of high-intensity and moderate-intensity exercise training on cardiopulmonary function and exercise endurance in patients with coronary artery diseases (CAD).
Methods: We performed a systematic search of the English and Chinese databases from their inception to March 2022. Randomized controlled trials (RCTs) were included to compare high-intensity and moderate-intensity exercise training on cardiopulmonary function in patients with CAD. The primary outcomes included peak oxygen uptake (peak VO2) and anaerobic threshold (AT). The secondary outcomes included left ventricular ejection fraction (LVEF), exercises duration (ED), respiratory exchange ratio (RER), resting heart rate (RHR), peak heart rate (PHR) and oxygen pulse (O2 pulse). The continuous variables were expressed as mean differences (MD) along with their corresponding standard deviations (SD), and the I2 test was applied in the assessment of heterogeneity.
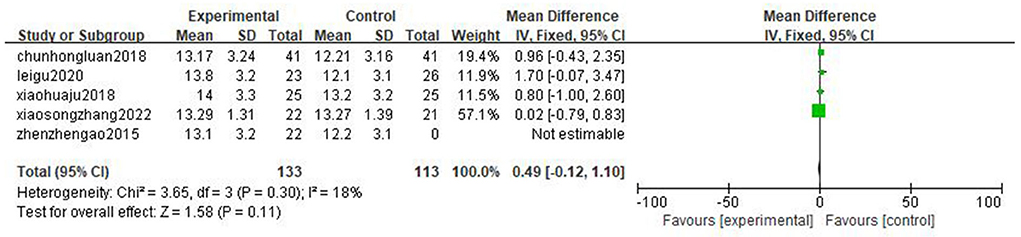
Results: After systematically literature search, 19 studies were finally selected for our meta-analysis (n = 1,036), with 511 patients in the experimental group (high-intensity exercise) and 525 patients in the control group (moderate-intensity exercise). The results showed that high-intensity exercise significantly increased patients' Peak VO2 [MD = 2.67, 95% CI (2.24, 3.09), P < 0.00001], LVEF [MD = 3.60, 95% CI (2.17, 5.03), P < 0.00001], ED [MD = 37.51, 95% CI (34.02, 41.00), P < 0.00001], PHR [MD = 6.86, 95% CI (4.49, 9.24), P < 0.00001], and O2 pulse [MD = 0.97, 95% CI (0.34, 1.60), P = 0.003] compared with moderate-intensity exercise. However, there were no significant differences in AT [MD = 0.49, 95% CI (−0.12, 1.10), P = 0.11], RER [MD = 0.00, 95% CI (−0.01, 0.02), P = 0.56], and RHR [MD = 1.10, 95% CI (−0.43, 2.63), P = 0.16].
Conclusion: Our results show that high-intensity exercise training has more significant positive effects compared with moderate-intensity exercise training in improving peak VO2, LVEF, ED, PHR and O2 pulse in patients with CAD, while no significant differences were observed in AT, RER and RHR. To sum up, high-intensity exercise training is better than moderate-intensity exercise training in improving cardiopulmonary function and exercise endurance in patients with CAD.
Systematic review registration: PROSPERO (CRD42022328475), https://www.crd.york.ac.uk/PROSPERO/.
Introduction
Cardiovascular diseases are the leading cause of death among non-communicable diseases worldwide (1), in which CAD is known having the highest occurrence (2). Thus, CAD has been recognized as a major public health issue worldwide, causing a heavy economic burden to the society (3). Cardiac rehabilitation is internationally recognized as a Class 1A recommendation to improve the prognosis and quality of life in patients with cardiovascular diseases, including patients who have undergone percutaneous coronary implantation (PCI) and coronary artery bypass grafting (CABG). Exercise training is the principal component of cardiac rehabilitation (4). Studies have shown that regular exercise can effectively control the risk factors associated with cardiovascular diseases, such as lowering blood pressure (5), controlling blood glucose (6), controlling body fat, and weight loss (7). Furthermore, it can also improve cardiopulmonary function in patients with CAD (8), improve vascular endothelial function (9), improve ventricular filling, and reverse ventricular remodeling (10). Thereby, it can reduce the incidence of cardiovascular diseases, improve the quality of life of patients, and reduce all-cause mortality (11). Exercise training mainly includes endurance exercise, resistance exercise and aerobic exercise (12). Aerobic exercise training is further classified into three types of exercise intensities: low, medium and high. Until now, there is no international consensus on the choice of exercise intensity. The United States and Canada prefer medium or high-intensity sports training, while Australia and Japan support low or moderate-intensity exercise training (13). The 2016 European Guidelines for the Prevention of Cardiovascular Disease recommended moderate-intensity continuous aerobic training with high safety as an exercise method for patients with cardiovascular diseases (14). Recently, an increasing number of studies have shown that high-intensity aerobic training has the advantages of short training time and high efficiency compared with long and boring moderate-intensity aerobic training (15). However, high-intensity exercise may trigger cardiac arrest in individuals with cardiovascular disease, especially in sedentary patients or those who have advanced cardiovascular diseases (16, 17). Therefore, it is pertinent and urgent to systematically evaluate the effects of the duration and intensity of exercise training and evaluate its effects on patients, and thus establish an optimal exercise training intensity prescription that optimizes the synergy between the rewards and safety (18).
The cardiopulmonary function is a powerful indicator of body's ability to exercise, diagnose diseases and efficiently evaluate prognosis. It can reflect the ability of the circulatory, respiratory and muscular systems to supply oxygen during continuous physical activity (19). Research evidence suggests that improvements in cardiorespiratory fitness are strongly associated with a reduction in all-cause mortality and cardiovascular mortality. And this is why the American Heart Association (AHA) has identified cardiorespiratory fitness as an important landmark indicator in the assessment and intervention of cardiovascular risks and cardiovascular mortality (20). Randomized controlled trials and meta-analyses have demonstrated that both high and moderate exercise intensity can improve cardiopulmonary function in patients with cardiovascular diseases, enhance exercise tolerance, and improve their quality of life compared with drug therapy alone. However, there are numerous controversies regarding the efficacy and safety of different exercise intensities. Therefore, this study is aimed toward the evaluation of the effects of different exercise intensities (moderate and high) on cardiopulmonary function in patients with CAD, to optimize the exercise mode, and provide actionable recommendations for the improvement of cardiopulmonary function and prognosis.
Methods
Registration
The protocol was registered on the International Prospective Register of Systematic Reviews (PROSPERO registration number: CRD42022328475). And our Meta-analysis was performed based on the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.
Search strategy
The following electronic databases were searched systematically: PubMed, EMBASE, the Cochrane Library, China National Knowledge Infrastructure (CNKI), Sino-Med, Chongqing VIP, and the Wanfang database, from their inception to March 2022. Taking PubMed as an example, the search strategy was (((((coronary heart disease) OR (coronary artery bypass grafting)) OR (PCI)) OR (ischemic heart disease)) OR (coronary artery stenosis)) AND (exercise intensity) AND (randomized controlled trial). All retrieved articles are imported into EndNote (English publication) and NoteExpress (Chinese publication).
Inclusion criteria
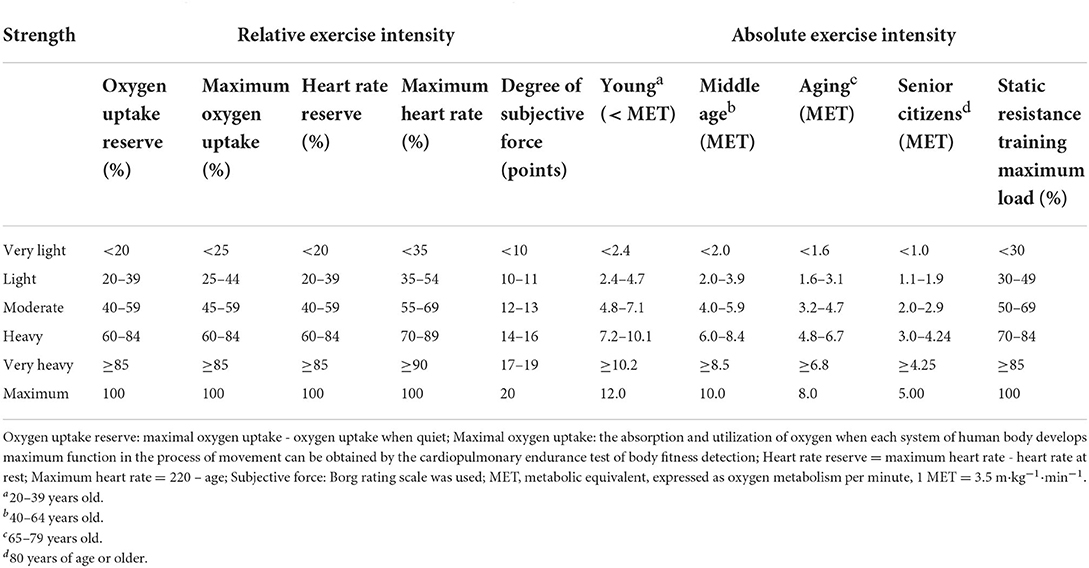
Clinical trials that satisfy the following criteria were included in our study: (1) Population: the target population was patients with CAD (including patients who have undergone PCI and CABG), consistent with 2014 ACC/AHA/AATS/PCNA/SCAI/STS the diagnostic criteria for patients with stable ischemic heart disease (21), and there are no restrictions on gender, age or duration of disease; (2) Intervention and comparisons: studies that compared exercise training at high (intervention measures) and moderate (control measures) intensities (the classification of exercise intensity was based on the American College of Sports Medicine Exercise Intensity Classification for Healthy Adults, as shown in Table 1), the intervention time for each exercise intervention time is more than 30 mins (22), and the intervention period is more than 4 weeks (23); (3) Outcomes: Outcome indicators must include at least one of peak oxygen uptake and anaerobic threshold; (4) Study Design: Randomized controlled trials (RCTs).
Exclusion criteria
(1) Studies involving patients with other serious comorbidities; (2) Repeated studies (when there is an overlapping of patient populations overlapped in multiple studies, only the studies with the largest sample sizes were included).
Data extraction
The literature screening and data extraction were independently performed by two investigators (Zheng LY and Gu YM) independently. The basic information extracted includes: (1) first author, publication time and country; (2) study characteristics: including the patients' ages, sample size, type of exercise, exercise duration and frequency; (3) intervention and control measures; (4) outcome indicators; (5) the Jadad scale quality scoring.
If there are any discrepancies, a third author is consulted to resolve these differences.
Risk of bias assessment
The quality of the included studies was independently assessed by two researchers independently and scored using the Jadad scale for quality assessment of randomized controlled trials. The total score on the Jadad scale is 5. And a score of 1–2 indicates low literature quality, while a score of 3–5 indicates high literature quality. The risk of bias for each study was assessed using the risk of bias assessment tool recommended in the Cochrane Systematic Evaluator's Manual 5.3. The evaluation indexes include seven aspects such as: the randomization method, assignment hiding, subject blindness, outcome evaluation blindness, data integrity, selective reporting and other bias. Each item was deemed to either be low risk, unknown risk and/or high risk.
Data synthesis
Data were synthesized using Review Manager Software (Version 5.3; Nordic Cochrane Center, Cochrane Collaboration). Due to the continuous nature of the extracted data, the analysis comprises mean difference (MD) and standard deviation (SD). X2 test and I2 statistical test were used to analyze heterogeneity. The value for high heterogeneity was set as I2 > 50% and P < 0.10, and a random effects model was used to evaluate the combined effect size of included data (24); however, if I2 < 50% and P > 0.10, heterogeneity was considered small and the fixed effects model was used. In case of large heterogeneity, the sources of heterogeneity were examined through sensitivity and subgroup analyses. Publication bias was assessed using funnel plots.
Results
Study selection
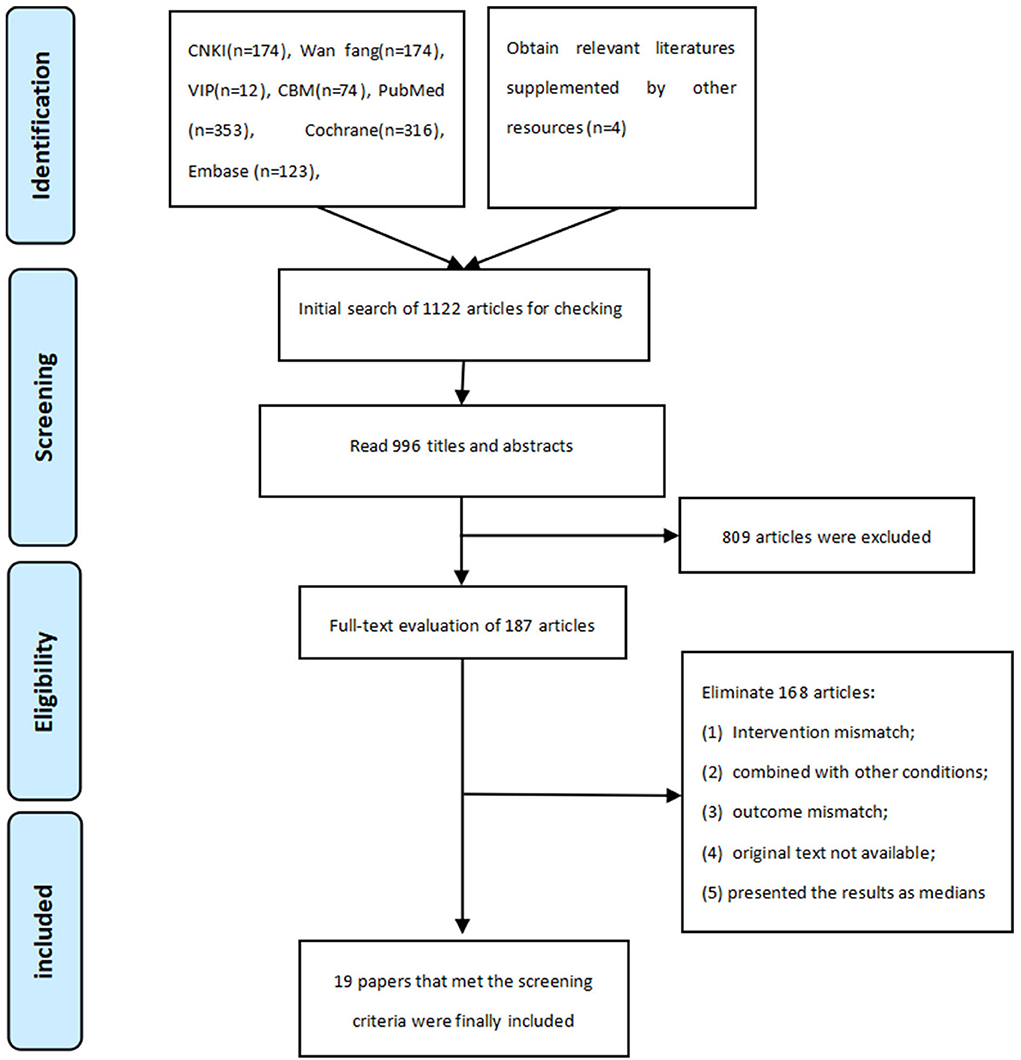
Our literature search is started from the inception of the aforementioned databases to March 2022. The literature screening flow chart of literature screening is shown in Figure 1. A total of 1,225 literatures were retrieved, which comprises 434 Chinese literature and 791 English literature, and four literatures was supplemented by manual retrieval from other sources. We imported the literature into EndNote X9 and NoteExpress (both are literature management software) and eliminated 233 duplicate literature. Furthermore, 809 articles were excluded by reading the titles and abstracts, subsequently, we perused through the remaining 187 articles, and finally selected 19 articles that met the inclusion criteria (25–43).
Study characteristics
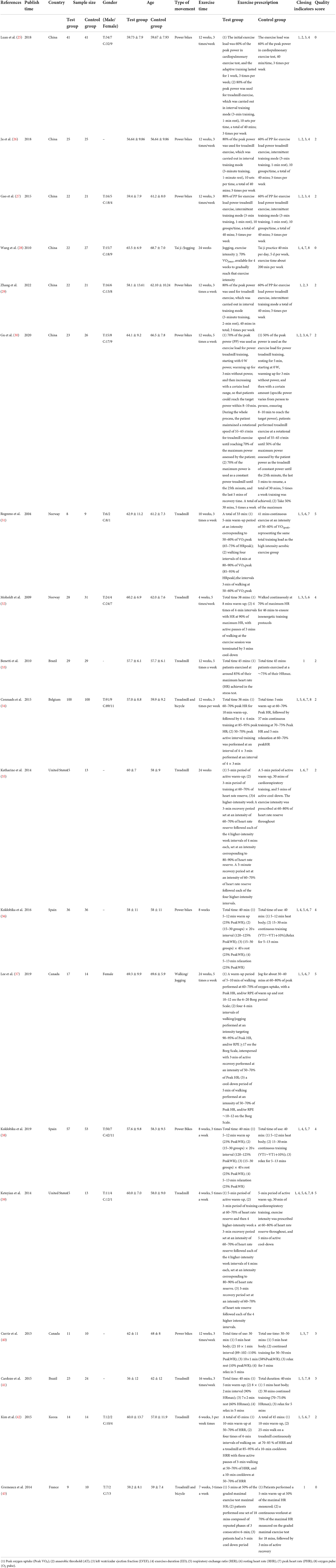
Nineteen trials were included (Table 2) involving a total of 1,036 patients which include 511 in the high-intensity exercise training group and 525 in the moderate-intensity exercise training group. 7 literatures (31, 32, 36, 38, 39, 42, 43) had an intervention period of <12 weeks, and 12 literatures (25–30, 33–35, 37, 40, 41) had an intervention period of 12 weeks or more.
Risk of bias
The quality assessment method of the 19 selected literatures is shown in Figure 2. 16 literatures (25–27, 29, 30, 32–42) described specific randomization methods, and 3 literatures (28, 31, 43) adopted a semi-randomization method combined with patients' wishes, and 5 literatures (30, 31, 37–39) implemented the allocation concealment; Considering the risk associated with exercise, patients are required to give and informed consent, so only one literature (31) implemented blind method for patients, five literatures (31, 37–39, 42) adopted the blinded outcome assessors; 13 (31–43) literatures recorded the circumstances and reasons for subjects who were lost to follow-up and dropped out of the trial. There were no selective reporting of outcome indicators, and no significant bias was identified in risk assessment.
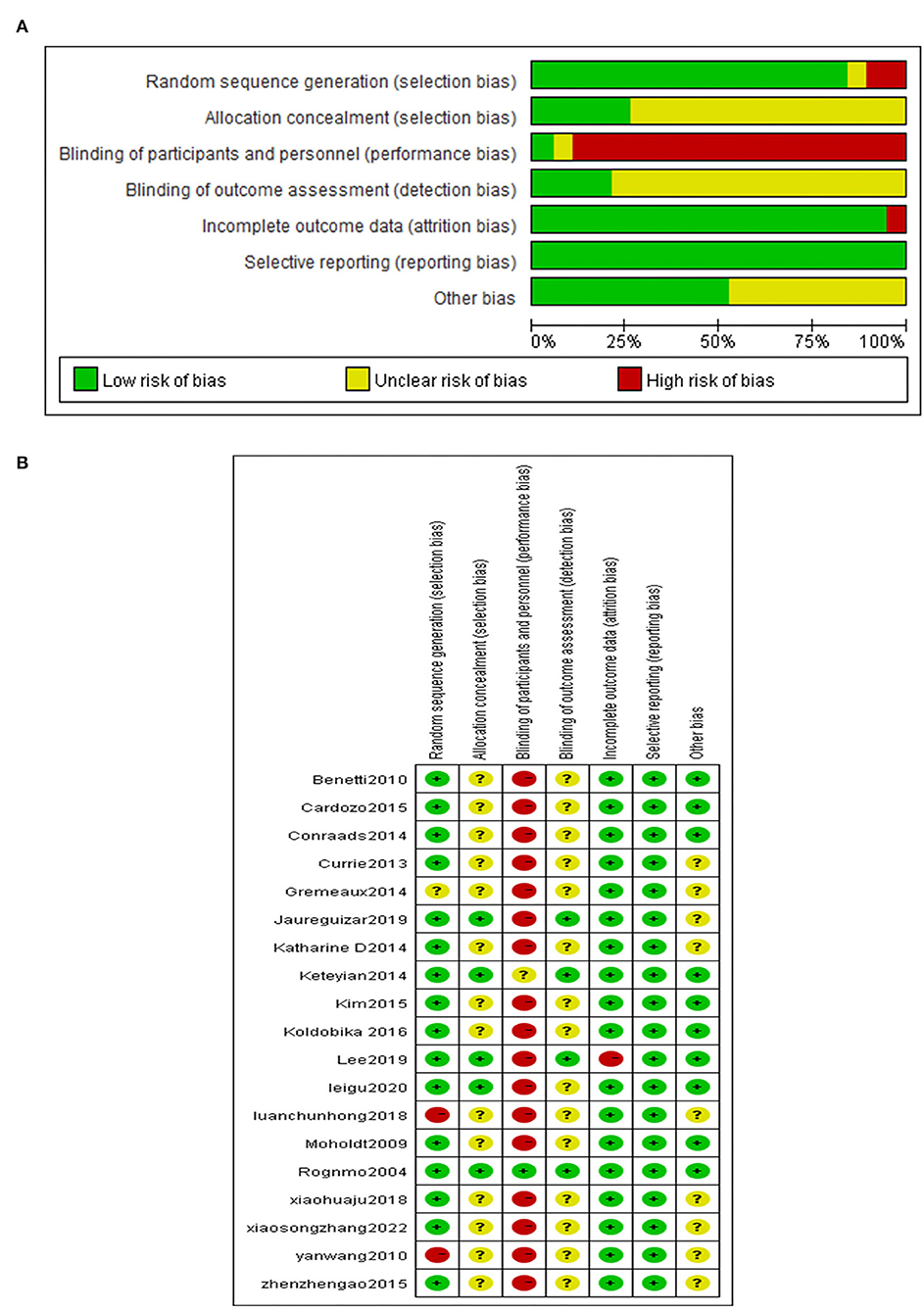
Figure 2. (A) Overall analysis diagram. (B) Single literature analysis diagram. “+” is low risk. “?” is unclear, and “–” is high risk.
Results of meta-analysis
Peak oxygen uptake (peak VO2)
Peak VO2 is reported in all the 19 included literatures (25–43) high-intensity exercise training on Peak VO2 showed significantly better effects than that of moderate-intensity exercise training [MD = 2.67, 95% CI (2.24, 3.09), P < 0.00001, I2 = 19%] (Figure 3).
Anaerobic threshold
Five literatures (25–27, 29, 30) reported anaerobic threshold (AT), and the results showed that there are no statistically significant difference in the improvement effect of two types of exercise intensity on AT [MD = 0.49, 95%CI (−0.12, 1.10), P = 0.11, I2 = 18%] (Figure 4).
Left ventricular ejection fraction
Six articles were reported on left ventricular ejection fraction (LVEF) (25–27, 29, 30, 32), and the result shows that high-intensity exercise training has a significantly better effect on LVEF than moderate-intensity exercise training [MD = 3.60, 95% CI (2.17, 5.03), P < 0.00001, I2 = 0%] (Figure 5).
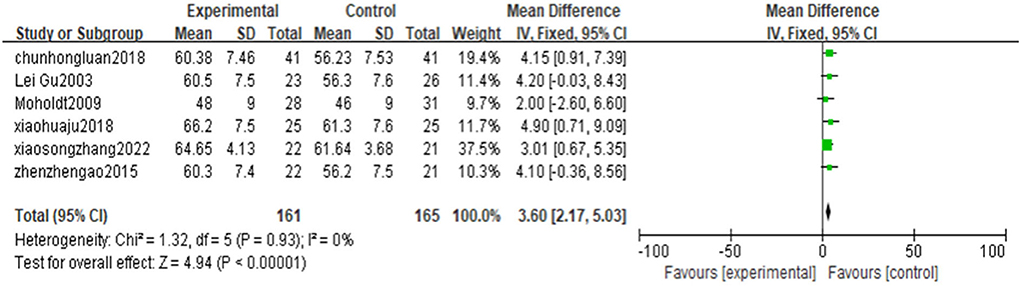
Figure 5. Forest plot of the effects of high-intensity and moderate-intensity exercise on LVEF in CAD patients.
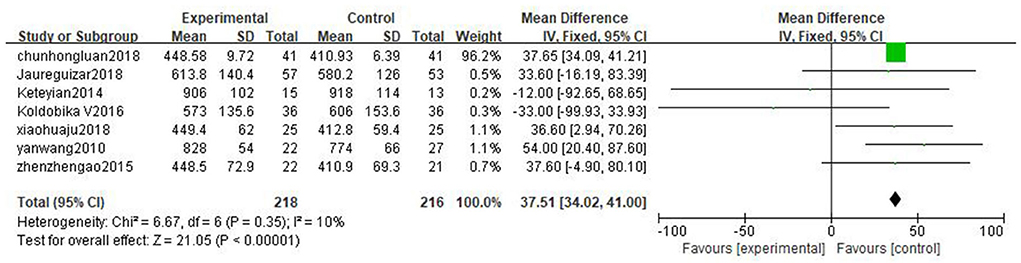
Exercise duration
Seven literatures (25–28, 36, 38, 39) reported exercise duration (ED). The result shows that high-intensity exercise has significant effects on ED compared to moderate-intensity exercise training [MD = 37.51, 95%CI (34.02, 41.00), P < 0.00001, I2 = 10%] (Figure 6).
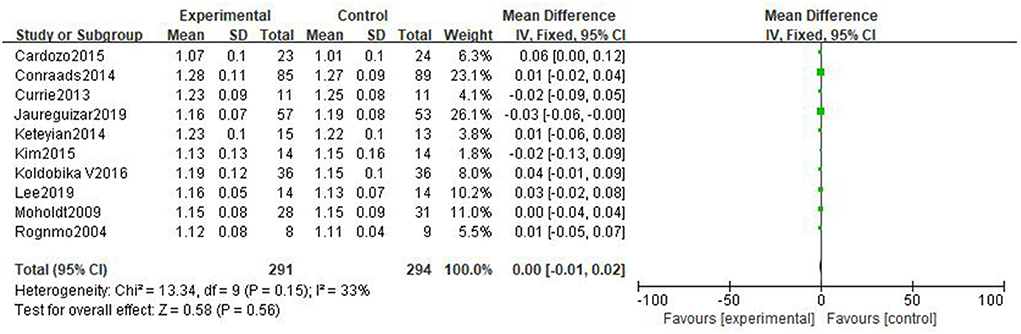
Respiratory exchange ratio
Ten studies (31, 32, 34, 36–42) reported respiratory exchange ratio (RER) with little heterogeneity. The result shows that there is no significant difference in the improvement effect of the two exercise intensities on RER [MD = 0.00, 95%CI (−0.01, 0.02), P = 0.56, I2 = 33%] (Figure 7).
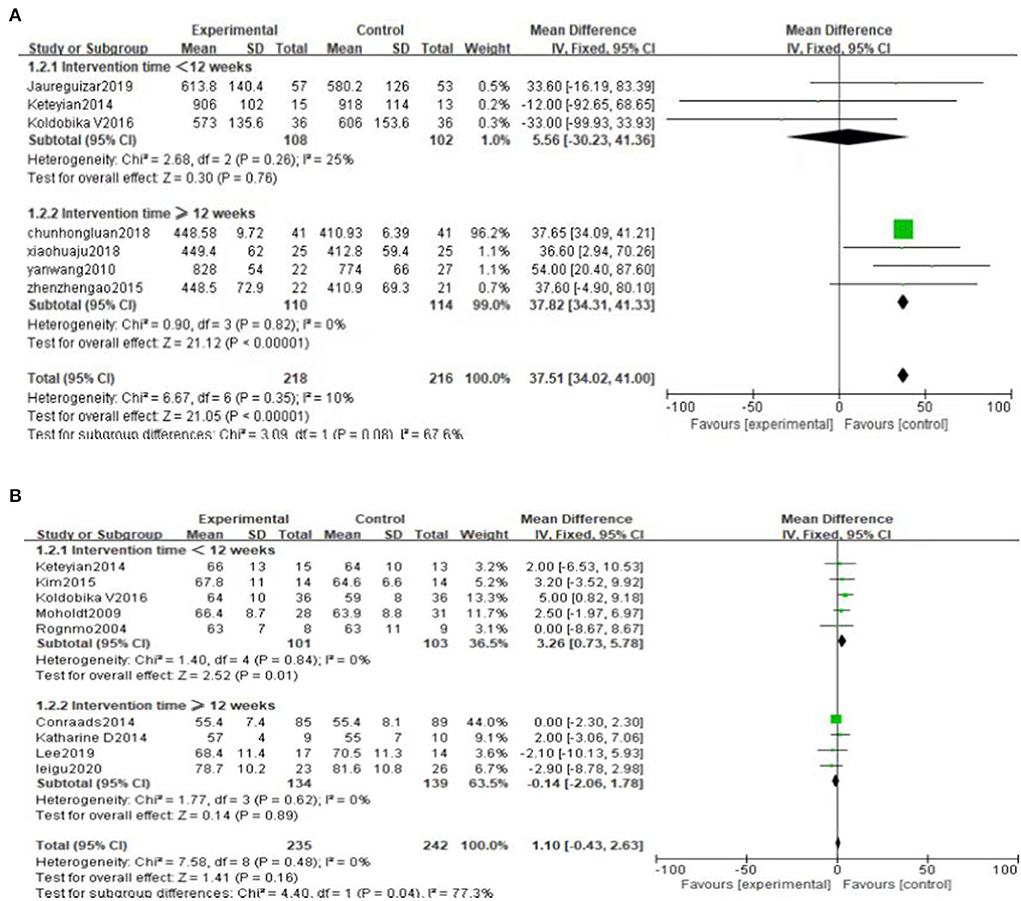
Resting heart rate
Nine literatures (30–32, 34–37, 39, 42) reported resting heart rate (RHR), and the results shows that there is no significant difference in the improvement effect of RHR between the two exercise intensities [MD = 1.10, 95% CI (−0.43, 2.63), P = 0.16, I2 = 0%] (Figure 8).
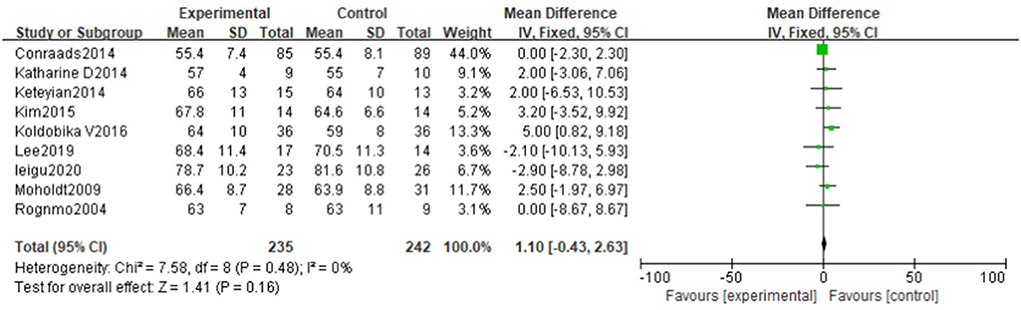
Figure 8. Forest plot of the effects of high-intensity and moderate-intensity exercise on RHR in CAD patients.
Peak heart rate
Twelve studies (28, 30, 31, 34–42) reported peak heart rate (PHR). The result showed that high-intensity exercise training has a significantly effect on PHR compared with moderate-intensity exercise training [MD = 6.86, 95% CI (4.49, 9.24), P < 0.00001, I2 = 0%] (Figure 9A).
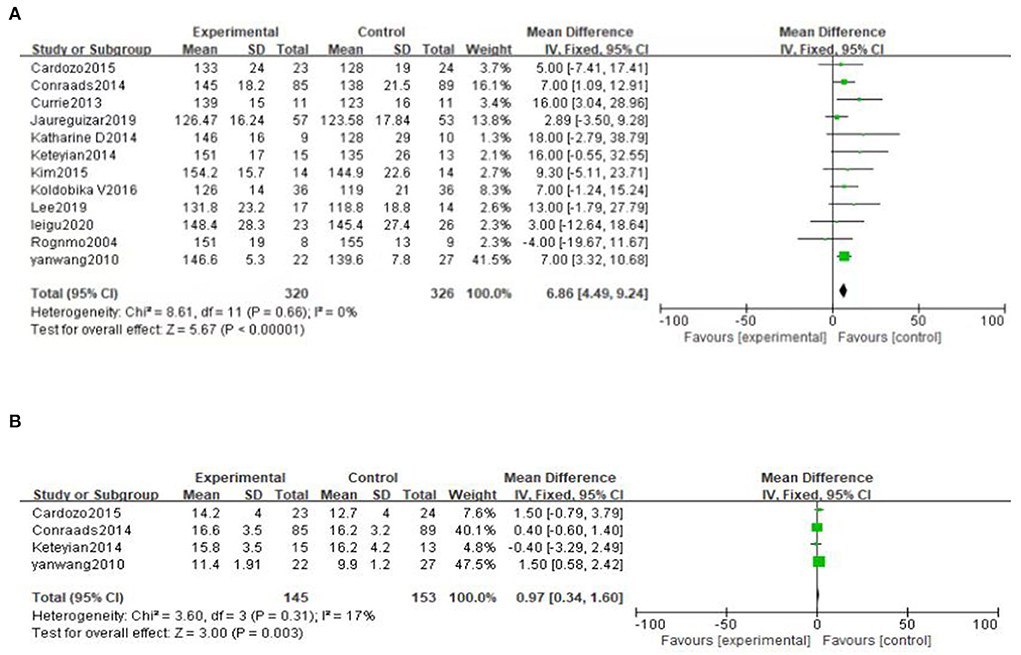
Figure 9. (A) Forest plot of the effects of high-intensity and moderate-intensity exercise on PHR in CAD patients. (B) Forest plot comparing the improvement effect of two exercise modes on O2 pulse.
Oxygen pulse
O2 pulse is reported in 4 literatures (28, 34, 39, 41). The result shows that high-intensity exercise training has a significant improvement on O2 pulse compared to moderate-intensity exercise training [MD = 0.97, 95%CI (0.34, 1.60), P = 0.003, I2 = 17%] (Figure 9B).
Subgroup analysis
Subgroup analysis was performed based on the duration of the intervention. We set 12 weeks as the boundary (one group was <12 weeks, the other group was ≥12 weeks). The results of subgroup analysis showed no significant difference in the influence of intervention time on Peak VO2, RER and PHR, and the results of subgroup analysis were consistent with the results of overall analysis (Figure 10). Interestingly, the subgroup analysis of ED showed no statistically significant difference when intervention duration was <12 weeks [MD = 5.56, 95%CI (−30.23, 41.36), P = 0.76]. However, when intervention time was ≥12 weeks, the difference was statistically significant [MD = 37.82, 95%CI (34.31, 41.33), P < 0.00001] (Figure 11A). Subgroup analysis of RHR showed that the difference was statistically significant when intervention time was <12 weeks, and high-intensity was better than moderate-intensity [MD = 3.26, 95%CI (0.73, 5.78), P = 0.01]. However, there was no significant difference when intervention time was ≥12 weeks [MD = −0.14, 95%CI (−2.06, 1.78), P = 0.89] (Figure 11B).
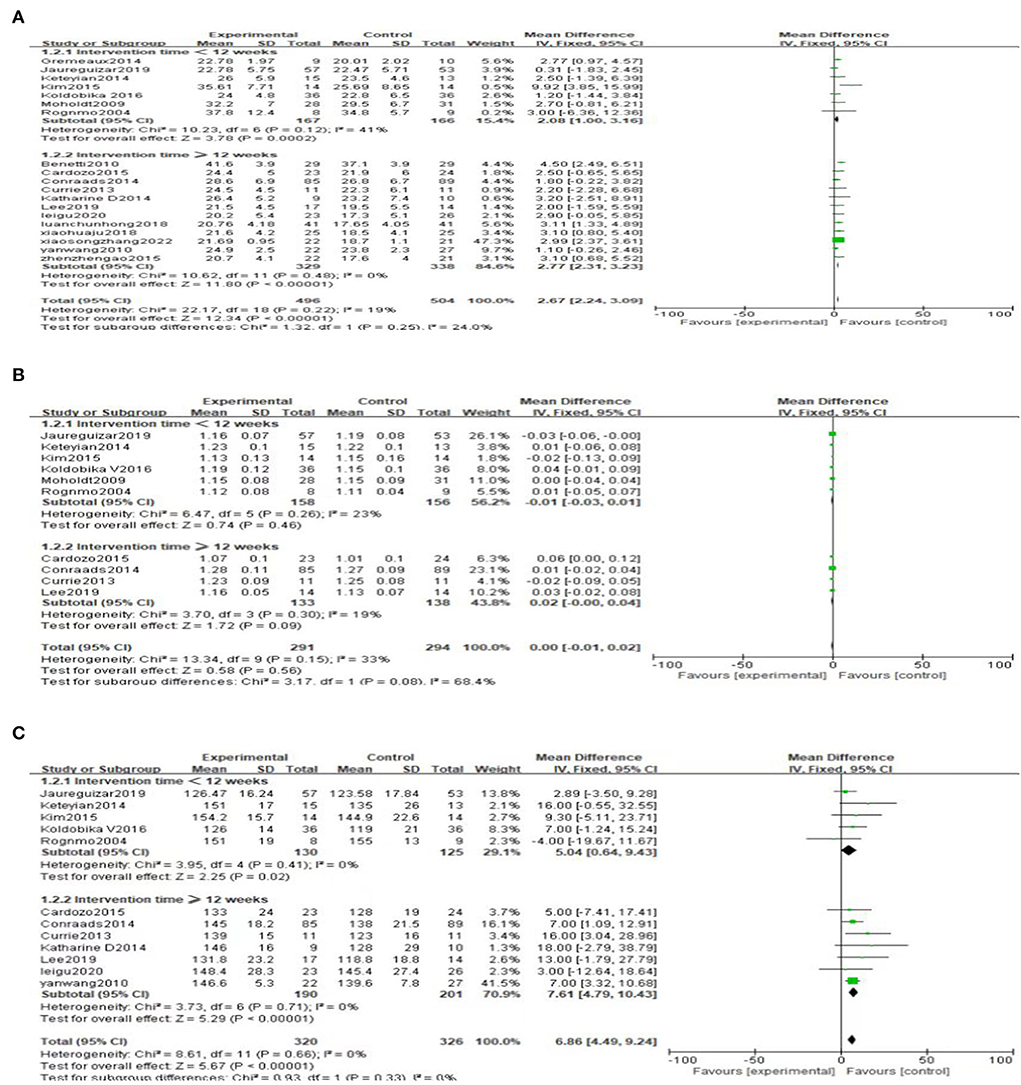
Figure 10. (A) Subgroup analysis of peak VO2. (B) Subgroup analysis of RER. (C) Subgroup analysis of PHR.
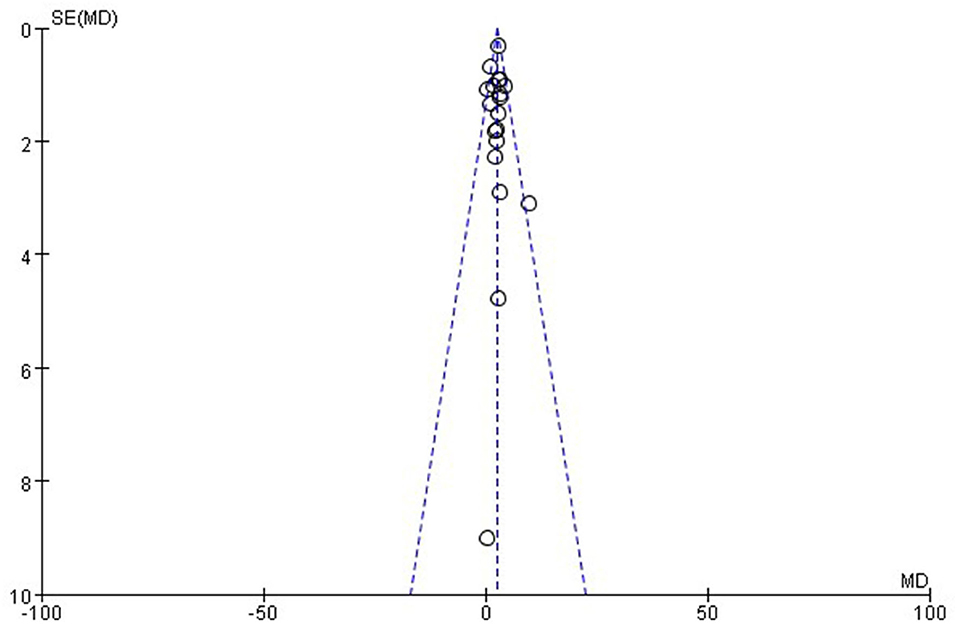
Publication bias
The funnel plot (Figure 12) was generated to reflect the publication bias. It can be seen from the figure that the distribution of all included studies is relatively concentrated and basically all data are located in the funnel plot. Therefore the possibility of publication bias of this study is small.
Sensitivity analysis
We performed sensitivity analysis to evaluate the influence of any individual study on the overall effect. For AT, the difference was statistically significant when Zhang et al. (29) was removed, and high-intensity was better than moderate-intensity [MD = 1.12, 95%CI (0.19, 2.06), P = 0.02, I2 = 0%]. For RHR, the difference was statistically significant when Conraads et al. (34) was removed, and high-intensity group showed slightly better than moderate-intensity group [MD = 2.10, 95%CI (0.13, 4.07), P = 0.04, I2 = 0%]. However, there is no significant difference in the improvement effect of the two exercise intensities on O2 pulse when Wang et al. (28) was removed [MD = 0.49, 95%CI (−0.38, 1.36), P = 0.27, I2 = 0%].
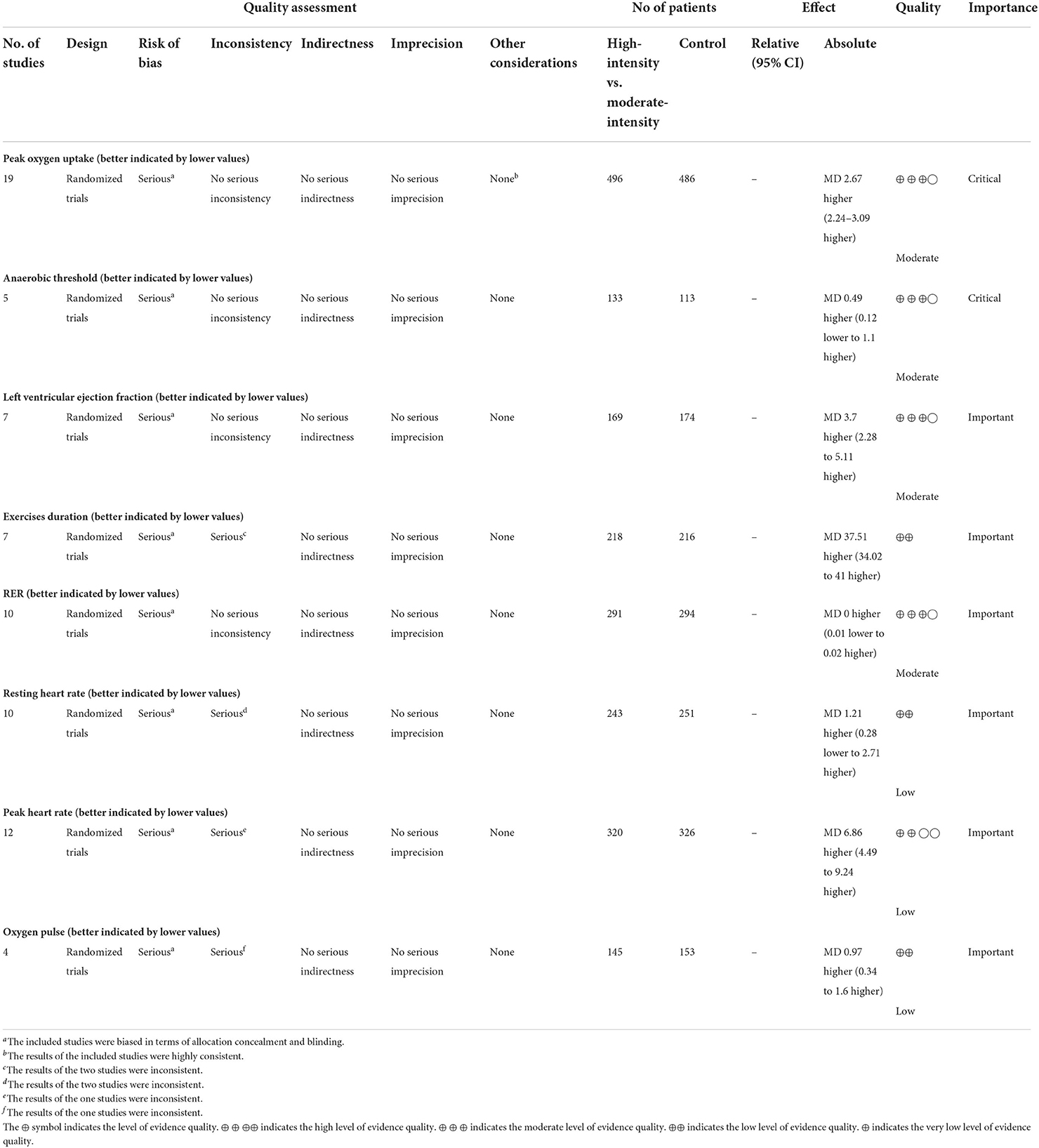
GRADE assessment
Table 3 shows the GRADE assessment of the certainty on the effect of exercise intensity in patients with CAD. Peak VO2, AT, LVEF, and RER were rated as moderate, while ED, RHR, PHR, and O2 pulse were rated as low-quality evidence. Reasons for downgrading: (1) For the risk of bias, only three literatures (28, 31, 43) refer to patients' wishes using a semi-randomized method; most studies do not specify whether allocation concealment is implemented; Considering the risk associated with exercise, patients are required to give and informed consent, so only one literature (31) implemented blind method for patients. (2) In terms of inconsistency: the results of two studies (36, 39) were inconsistent for the effect of exercise intensity on ED. For RHR, two studies (30, 37) had inconsistent results. For PHR, there was one study (31) with different results. For O2 pulse, one study (39) showed different results from others. And these may be due to differences in study population, gender, and duration of intervention.
Discussion
Summary of the evidence
In this study, we selected 19 RCTs with a total of 1,036 patients. Our results show that compared with moderate-intensity exercise training, high-intensity exercise training has better improvement effects on Peak VO2, LVEF, ED, PHR and O2 pulse in patients with CAD. However, there are no significant differences in the effects of AT, RER and RHR. Furthermore, our subgroup analysis showed that there is no statistical difference in the influence of intervention time on peak VO2, RER and PHR. The effect of exercise intensity on ED and RHR was influenced by the intervention time. For the ED outcome, high-intensity exercise was superior to moderate-intensity exercise only when the intervention time was ≥12 weeks. For the outcome of RHR, when the intervention time was <12 weeks, high-intensity exercise has better improvement effects than moderate-intensity exercise. But when the intervention time was ≥12 weeks, the difference was not statistically significant.
Results in relation to other studies
There were some relevant meta-analysis articles published lately, such as the recently published one by Gomes-Neto (44). However, the retrieval deadline of the study mentioned above was in November 2016. Only 12 literatures were selected in that study and the efficacy indicators of cardiopulmonary function were very limited (only peak VO2). On the contrary, our study screened all qualified literature from the establishment of the relevant databases to April 2022, and 19 RCTs were selected. We also analyzed more indicators related to cardiopulmonary function (peak VO2, AT, LVEF, ED, RER, RHR, PHR, and O2 pulse). Hence, our study provided more robust and comprehensive evidence for evaluating the effect of moderate and high exercise intensity on cardiopulmonary function.
Potential mechanism
The underlying mechanism of high-intensity exercise improving peak VO2 in patients with CAD may be related to the fact that high-intensity exercise can stimulate muscle vascularization, improve blood circulation, and enhance blood oxygen-carrying capacity (45); In addition, studies (46) have shown that higher intensity exercise can stimulate the pumping capacity of the heart to a greater extent, increase blood flow, increase endothelial shear stress, activate endothelial nitric oxide synthase, and increase antioxidant status. Thus, nitric oxide synthesis is improved and its bioavailability is increased, which consequently improves the vascular endothelial function (47–49). High-intensity exercise can also increase oxisome proliferator-activated receptor γ coactivator 1α (a regulator of mitochondrial biogenesis) to improve mitochondrial function and enhance rapid adaptation and metabolic capacity in skeletal muscles (50). Therefore, high-intensity exercise is more effective in increasing Peak VO2 than moderate-intensity exercise training. LVEF is a major indicator of the pumping capacity of the heart. An elevated LVEF level indicates improved cardiac function. The mechanism of which exercise intensity improves LVEF is not clear, but it may be related to the ability of higher intensity exercise reduces left ventricular end-diastolic volume (EDV) and left ventricular end-systolic volume (ESV), improves ventricular remodeling and myocardial contractility. The PHR improvement in the high-intensity exercise group is better than that in the moderate-intensity exercise group, which can be attribute to the fact that higher exercise intensity can increase stroke volume, enhance myocardial contractility, increase the ejection fraction during extreme exercise, and improve exercise tolerance (51). ED is the duration of exercise from the beginning to the end of the evaluation in the Cardiopulmonary Exercise Test (CPET). The overall analysis showed that high-intensity exercise prolongs ED better than moderate-intensity exercise. However, our subgroup analysis results shows that when ≥12 weeks, the duration of high-intensity continuous exercise is longer than that of moderate-intensity. This implies that high-intensity exercise results in a better improvement in the exercise endurance of patients over time. Since PHR is affected by multiple factors such as age, gender, body size, muscle volume, daily activity level and exercise type (52), their specific mechanisms need to be further explored through more detailed and high-quality clinical trials. High-intensity exercise training is beneficial to anaerobic glycolysis and increases the lactic acid content in the blood. Lactate is converted back to glucose in the liver, thus AT is related to the gluconeogenic capacity of the liver. An experimental study in animal has shown that high-intensity exercise training can enhance the hepatic gluconeogenesis of lactate and increase the lactate threshold (53). However, this study shows that there is no significant difference in the effect of exercise intensity on AT, which may be due to the difference in lactic acid metabolism of human bodies. In addition, the concept of AT is still controversial, and the calculation methods, equipment used and detection personnel under various concepts will also have a significant impact on the results (54). RER expresses the relationship between carbon dioxide produced (CO2) and oxygen consumed (O2) which can be used to determine the rate of lipid oxidation (55). Studies showed that a reduction in the levels of RER levels after high-intensity exercise compared to moderate-intensity exercise (56, 57). However, our study did not find differences in the effect of exercise intensity on RER, which may be due to the lack of consideration for the effect of related gene expression on RER. Furthermore, some studies found that differences in exercise performance and muscle metabolic activity are associated with ACTN3 gene polymorphisms (58–60). RER decreases in subjects with only X allele after high-intensity exercise training, while there is no significant change in RER in RR homozygous subjects (61). High-intensity exercise has an advantage over moderate-intensity exercise in reducing RHR (62). And our study found that when the intervention time is <12 weeks, the RHR of high-intensity is slower than that of moderate-intensity, but there is no difference in intensity between the two exercises when it is ≥12 weeks. This may be attribute to the fact that high-intensity exercise is better at slowing PHR for a short period of time, but when patients keep exercising for longer time, the advantage of high-intensity exercise disappears.
Limitations
Due to time and funding constraints, most of the current studies only observed the impact of exercise training on cardiopulmonary function indicators in patients. But there are few reports regarding long-term follow-up and clinical endpoint events as the salient endpoint indicators, which offers us a direction worthy of in-depth research in the future; The 19 studies adopted different exercise programs, and there are differences in race, gender and age among the subjects. In addition, exercise time (morning/ afternoon/ evening) and the total calorie consumption during exercise was not uniform, which may be responsible for the bias in our study. And there were large differences in the quality of the literature and the sample size of each study.
Future directions
Due to the limitation of the sample size of the included studies, for patients with severe disease or patients with multi-vessel coronary artery disease, whether it is possible to continue to recommend high-intensity exercise programs is an interesting direction for future research. With the extension of exercise time, there are special changes in cardiopulmonary function indicators, which also provides an interesting direction for the design of future research duration. Given the limitations mentioned above, further high-quality studies are still needed to provide more reliable and higher-level evidence-based evidence on this subject matter in the future.
Conclusion
Compared with moderate-intensity exercise training, high-intensity exercise training is more effective in improving peak VO2, LVEF, ED, PHR and, O2 pulse in patients with CAD. Nonetheless, there is no statistical difference in the effects of the two exercise intensities on AT, RER, and RHR. Among them, high-intensity exercise did not show an advantage in prolonging ED until intervention time reached 12 weeks. Also, high-intensity exercise is better at slowing RHR within 12 weeks, but this advantage disappeared with increased exercise duration.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
LZ, DP, and YG designed the study and assessed the risk of bias. LZ and DP analyzed the data and wrote the first and revised version of the manuscript. RW and YW screened and extracted the data. LZ, DP, and MX modified the final manuscript. All authors read and approved the final manuscript, contributed to the conceptualization of the research questions, interpretation of the results, and article writing.
Funding
This work was supported by the National Key Programme for Research and Development from the Ministry of Science and Technology, China (No. 2019YFC0840608), National Natural Science Foundation of China (No. 81973686), and Major research project of scientific and technological innovation project of Chinese Academy of Chinese Medicine Sciences (No. CI2021A00913).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Members WG, Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, et al. Heart disease and stroke statistics-2016 update: a report from the American Heart Association. Circulation. (2016) 133:e38–360. doi: 10.1161/CIR.0000000000000350
2. Roth GA, Johnson C, Abajobir A, Abd-Allah F, Abera SF, Abyu G, et al. Global, regional, and national burden of cardiovascular diseases for 10 causes, 1990 to 2015. J Am Coll Cardiol. (2017) 70:1–25. doi: 10.1016/j.jacc.2017.04.052
3. Prabhakaran D, Jeemon P, Sharma M, Roth GA, Johnson C, Harikrishnan S, et al. The changing patterns of cardiovascular diseases and their risk factors in the states of India: the Global Burden of Disease Study 1990–2016. Lancet Glob Health. (2018) 6:e1339–51. doi: 10.1016/S2214-109X(18)30407-8
4. Ambrosetti M, Abreu A, Corrà U, Davos CH, Hansen D, Frederix I, et al. Secondary Prevention through Comprehensive Cardiovascular Rehabilitation: From Knowledge to Implementation. 2020 Update. A Position Paper from the Secondary Prevention and Rehabilitation Section of the European Association of Preventive Cardiology. Eur J Prev Cardiol. (2021) 28:460–95. doi: 10.1177/2047487320913379
5. Grace F, Herbert P, Elliott AD, Richards J, Beaumont A, Sculthorpe NF. High Intensity interval training (HIIT) improves resting blood pressure, metabolic (Met) capacity and heart rate reserve without compromising cardiac function in sedentary aging men. Exp Gerontol. (2018) 109:75–81. doi: 10.1016/j.exger.2017.05.010
6. Higgins TP, Baker MD, Evans SA, Adams RA, Cobbold C. Heterogeneous responses of personalised high intensity interval training on type 2 diabetes mellitus and cardiovascular disease risk in young healthy adults. Clin Hemorheol Microcirc. (2015) 59:365–77. doi: 10.3233/CH-141857
7. Maillard F, Pereira B, Boisseau N. Effect of high-intensity interval training on total, abdominal and visceral fat mass: a meta-analysis. Sports Med (Auckland, NZ). (2018) 48:269–88. doi: 10.1007/s40279-017-0807-y
8. Kessler HS, Sisson SB, Short KR. The potential for high-intensity interval training to reduce cardiometabolic disease risk. Sports Med. (2012) 42:489–509. doi: 10.2165/11630910-000000000-00000
9. Fernández-Rubio H, Becerro-de-Bengoa-Vallejo R, Rodríguez-Sanz D, Calvo-Lobo C, Vicente-Campos D, Chicharro JL. Exercise training and interventions for coronary artery disease. J Cardiovasc Dev Dis. (2022) 9:131. doi: 10.3390/jcdd9050131
10. Angadi SS, Mookadam F, Lee CD, Tucker WJ, Haykowsky MJ, Gaesser GA. High-intensity interval training vs. moderate-intensity continuous exercise training in heart failure with preserved ejection fraction: a pilot study. J Appl Physiol. (2015) 119:753–78. doi: 10.1152/japplphysiol.00518.2014
11. Pelliccia A, Sharma S, Gati S, Bäck M, Börjesson M, Caselli S, et al. 2020 ESC guidelines on sports cardiology and exercise in patients with cardiovascular disease. Eur Heart J. (2021) 42:17–96. doi: 10.1093/eurheartj/ehaa605
12. Piepoli MF, Hoes AW, Agewall S, Albus C, Brotons C, Catapano AL, et al. 2016 European guidelines on cardiovascular disease prevention in clinical practice: the sixth joint task force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (Constituted by Representatives of 10 Societies and by Invited Experts): developed with the special contribution of the European Association for Cardiovascular Prevention and Rehabilitation (EACPR). Eur J Prev Cardiol. (2016) 74:821–936. doi: 10.1177/2047487316653709
13. Price KJ, Gordon BA, Bird SR, Benson AC. A review of guidelines for cardiac rehabilitation exercise programmes: is there an international consensus? Eur J Prev Cardiol. (2016) 23:1715–33. doi: 10.1177/2047487316657669
14. Piepoli MF, Hoes AW, Agewall S, Albus C, Brotons C, Catapano AL, et al. 2016 European guidelines on cardiovascular disease prevention in clinical practice: the Sixth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (Constituted by Representatives of 10 Societies and by Invited Experts) developed with the special contribution of the european association for cardiovascular prevention and rehabilitation (EACPR). Atherosclerosis. (2016) 252:207–74. doi: 10.1016/j.atherosclerosis.2016.05.037
15. Weston KS, Wisløff U, Coombes JS. High-intensity interval training in patients with lifestyle-induced cardiometabolic disease: a systematic review and meta-analysis. Br J Sports Med. (2014) 48:1227–34. doi: 10.1136/bjsports-2013-092576
16. Marijon E, Uy-Evanado A, Reinier K, Teodorescu C, Narayanan K, Jouven X, et al. Sudden cardiac arrest during sports activity in middle age. Circulation. (2015) 131:1384–91. doi: 10.1161/CIRCULATIONAHA.114.011988
17. Chugh SS, Weiss JB. Sudden cardiac death in the older athlete. J Am Coll Cardiol. (2015) 65:493–502. doi: 10.1016/j.jacc.2014.10.064
18. Palermo P, Corrà U. Exercise prescriptions for training and rehabilitation in patients with heart and lung disease. Ann Am Thorac Soc. (2017) 14:59–66. doi: 10.1513/AnnalsATS.201702-160FR
19. Lee D-c, Artero EG, Sui X, Blair SN. Mortality trends in the general population: the importance of cardiorespiratory fitness. J Psychopharmacol. (2010) 24:27–35. doi: 10.1177/1359786810382057
20. Kodama S, Saito K, Tanaka S, Maki M, Yachi Y, Asumi M, et al. Cardiorespiratory fitness as a quantitative predictor of all-cause mortality and cardiovascular events in healthy men and women: a meta-analysis. JAMA. (2009) 301:2024–35. doi: 10.1001/jama.2009.681
21. Fihn SD, Blankenship JC, Alexander KP, Bittl JA, Byrne JG, Fletcher BJ, et al. 2014 ACC/AHA/AATS/PCNA/SCAI/STS focused update of the guideline for the diagnosis and management of patients with stable ischemic heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines, and the American Association for Thoracic Surgery, Preventive Cardiovascular Nurses Association, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. J Thorac Cardiovasc Surg. (2015) 149:e5–e23. doi: 10.1016/j.jtcvs.2014.11.002
22. Li B, Tian Z. Research progress on exercise intervention in ischemic heart disease and its mechanism. Life Sci. (2020) 32:864–77. doi: 10.13376/j.cbls/2020108
23. Achttien RJ, Staal JB, van der Voort S, Kemps HMC, Koers H, Jongert MWA, et al. Exercise-based cardiac rehabilitation in patients with coronary heart disease: a practice guideline. Netherlands Heart J. (2013) 21:429–38. doi: 10.1007/s12471-013-0467-y
24. Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 327:557–60. doi: 10.1136/bmj.327.7414.557
25. Luan CH, Yang XL, Luan LP. Effects of intermittent aerobic exercise of different intensities on cardiac function, exercise tolerance and quality of life in patients with coronary heart disease after PCI. Guizhou Med. (2019) 43:277–9. doi: 10.3969/j.issn.1000-744X.2019.02.038
26. Ju XH. Effects of intermittent aerobic exercise of different intensities on cardiac function, exercise tolerance and quality of life in patients with coronary heart disease after PCI. Heilongjiang Med. (2018) 31:675–6. doi: 10.14035/j.cnki.hljyy.2018.03.105
27. Gao ZZ Ji P, Xia YQ, Wang L. Effects of different intensities of aerobic exercise on cardiac function and exercise tolerance in patients after percutaneous coronary intervention. Chin J Rehabil Med. (2015) 30:344–8. doi: 10.3969/j.issn.1001-1242.2015.04.007
28. Wang Y, Zhu LY, Ren AH. Effects of different intensities of exercise on cardiopulmonary function in elderly patients with coronary heart disease who lack exercise. Chin J Phys Med Rehabil. (2010) 2010:845–8. doi: 10.3760/cma.j.issn.0254-1424.2010.11.012
29. Zhang XS, Zhong JP, Tang YX, Song BT, Deng SP, Hu SS, et al. Effects of high-intensity intermittent and moderate-intensity continuous aerobic training on stratified low-risk patients with exercise rehabilitation after percutaneous coronary intervention. Chin J Phys Med. (2022) 44:47–51. doi: 10.3760/cma.j.issn.0254-1424.2022.01.009
30. Gu L, Wu L, Li Y, Wan L, A. comparative study of different exercise intensities for cardiac rehabilitation in patients after percutaneous coronary intervention. Hebei Med. (2020) 42:853–6. doi: 10.3969/j.issn.1002-7386.2020.06.012
31. Rognmo Ø, Hetland E, Helgerud J, Hoff J, Slørdahl SA. High intensity aerobic interval exercise is superior to moderate intensity exercise for increasing aerobic capacity in patients with coronary artery disease. Eur J Cardiovasc Prev Rehab. (2004) 11:216–22. doi: 10.1097/01.hjr.0000131677.96762.0c
32. Moholdt TT, Amundsen BH, Rustad LA, Wahba A, Løvø KT, Gullikstad LR, et al. Aerobic interval training versus continuous moderate exercise after coronary artery bypass surgery: a randomized study of cardiovascular effects and quality of life. Am Heart J. (2009) 158:1031–7. doi: 10.1016/j.ahj.2009.10.003
33. Benetti M, Araujo CL, Santos RZ. Cardiorespiratory fitness and quality of life at different exercise intensities after myocardial infarction. Arquivos Bras Cardiol. (2010) 95:399–404. doi: 10.1590/s0066-782x2010005000089
34. Conraads VM, Pattyn N, De Maeyer C, Beckers PJ, Coeckelberghs E, Cornelissen VA, et al. Aerobic interval training and continuous training equally improve aerobic exercise capacity in patients with coronary artery disease: the SAINTEX-CAD study. Int J Cardiol. (2015) 179:203–10. doi: 10.1016/j.ijcard.2014.10.155
35. Currie KD, Bailey KJ, Jung ME, McKelvie RS, MacDonald MJ. Effects of resistance training combined with moderate-intensity endurance or low-volume high-intensity interval exercise on cardiovascular risk factors in patients with coronary artery disease. J Sci Med Sport. (2015) 18:637–42. doi: 10.1016/j.jsams.2014.09.013
36. Jaureguizar KV, Vicente-Campos D, Bautista LR, de la Peña CH, Gómez MJ, Rueda MJ, et al. Effect of high-intensity interval versus continuous exercise training on functional capacity and quality of life in patients with coronary artery disease: a randomized clinical trial. J Cardiopulm Rehabil Prev. (2016) 36:96–105. doi: 10.1097/HCR.0000000000000156
37. Lee LS, Tsai M-C, Brooks D, Oh PI. Randomised controlled trial in women with coronary artery disease investigating the effects of aerobic interval training versus moderate intensity continuous exercise in cardiac rehabilitation: cat versus mice study. BMJ Open Sport Exerc Med. (2019) 5:e000589. doi: 10.1136/bmjsem-2019-000589
38. Villelabeitia-Jaureguizar K, Vicente-Campos D, Berenguel Senen A, Hernández Jiménez V, Ruiz Bautista L, Barrios Garrido-Lestache ME, et al. Mechanical efficiency of high versus moderate intensity aerobic exercise in coronary heart disease patients: a randomized clinical trial. Cardiol J. (2019) 26:130–7. doi: 10.5603/CJ.a2018.0052
39. Keteyian SJ, Hibner BA, Bronsteen K, Kerrigan D, Aldred HA, Reasons LM, et al. Greater improvement in cardiorespiratory fitness using higher-intensity interval training in the standard cardiac rehabilitation setting. J Cardiopulm Rehabil Prev. (2014) 34:98–105. doi: 10.1097/HCR.0000000000000049
40. Currie KD, Dubberley JB, McKelvie RS, MacDonald MJ. Low-volume, high-intensity interval training in patients with Cad. Med Sci Sports Exerc. (2013) 45:1436–42. doi: 10.1249/MSS.0b013e31828bbbd4
41. Cardozo GG, Oliveira RB, Farinatti PT. Effects of high intensity interval versus moderate continuous training on markers of ventilatory and cardiac efficiency in coronary heart disease patients. Sci World J. (2015) 2015:192479. doi: 10.1155/2015/192479
42. Kim C, Choi HE, Lim MH. Effect of high interval training in acute myocardial infarction patients with drug-eluting stent. Am J Phys Med Rehabil. (2015) 94:879–86. doi: 10.1097/phm.0000000000000290
43. Gremeaux M, Hannequin A, Laurent Y, Laroche D, Casillas JM, Gremeaux V. Usefulness of the 6-minute walk test and the 200-metre fast walk test to individualize high intensity interval and continuous exercise training in coronary artery disease patients after acute coronary syndrome: a pilot controlled clinical study. Clin Rehabil. (2011) 25:844–55. doi: 10.1177/0269215511403942
44. Gomes-Neto M, Durães AR, Reis H, Neves VR, Martinez BP, Carvalho VO. High-intensity interval training versus moderate-intensity continuous training on exercise capacity and quality of life in patients with coronary artery disease: a systematic review and meta-analysis. Eur J Prev Cardiol. (2017) 24:1696–707. doi: 10.1177/2047487317728370
45. Wisløff U, Støylen A, Loennechen JP, Bruvold M, Rognmo Ø, Haram PM, et al. Superior cardiovascular effect of aerobic interval training versus moderate continuous training in heart failure patients: a randomized study. Circulation. (2007) 115:3086–94. doi: 10.1161/CIRCULATIONAHA.106.675041
46. Tinken TM, Thijssen DHJ, Hopkins N, Black MA, Dawson EA, Minson CT, et al. Impact of shear rate modulation on vascular function in humans. Hypertension (Dallas, Tex: 1979) (2009) 54:278–85. doi: 10.1161/HYPERTENSIONAHA.109.134361
47. Johnson BD, Mather KJ, Wallace JP. Mechanotransduction of shear in the endothelium: basic studies and clinical implications. Vasc Med. (2011) 16:365–77. doi: 10.1177/1358863X11422109
48. Tucker WJ, Lijauco CC, Hearon CM Jr, Angadi SS, Nelson MD, Sarma S, et al. Mechanisms of the improvement in peak VO2 with exercise training in heart failure with reduced or preserved ejection fraction. Heart Lung Circ. (2018) 27:9–21. doi: 10.1016/j.hlc.2017.07.002
49. Lavier J, Beaumann M, Menétrey S, Bouzourène K, Rosenblatt-Velin N, Pialoux V, et al. High-intensity exercise in hypoxia improves endothelial function via increased nitric oxide bioavailability in C57bl/6 mice. Acta Physiologica (Oxford, England). (2021) 233:e13700. doi: 10.1111/apha.13700
50. Haykowsky MJ, Timmons MP, Kruger C, McNeely M, Taylor DA, Clark AM. Meta-analysis of aerobic interval training on exercise capacity and systolic function in patients with heart failure and reduced ejection fractions. Am J Cardiol. (2013) 111:1466–9. doi: 10.1016/j.amjcard.2013.01.303
51. Huang SC, Wong MK, Lin PJ, Tsai FC, Fu TC, Wen MS, et al. Modified high-intensity interval training increases peak cardiac power output in patients with heart failure. Eur J Appl Physiol. (2014) 114:1853–62. doi: 10.1007/s00421-014-2913-y
52. Oberman A, Fletcher GF, Lee J, Nanda N, Fletcher BJ, Jensen B, et al. Efficacy of high-intensity exercise training on left ventricular ejection fraction in men with coronary artery disease (the training level comparison study). Am J Cardiol. (1995) 76:643–7. doi: 10.1016/s0002-9149(99)80189-1
53. Itoh H, Ajisaka R, Koike A, Makita S, Omiya K, Kato Y, et al. Heart rate and blood pressure response to ramp exercise and exercise capacity in relation to age, gender, and mode of exercise in a healthy population. J Cardiol. (2013) 61:71–8. doi: 10.1016/j.jjcc.2012.09.010
54. Muller GY, Matos FdO, Perego Junior JE, Kurauti MA, Diaz Pedrosa MM. High-intensity interval resistance training (HIIRT) improves liver gluconeogenesis from lactate in Swiss mice. Appl Physiol Nutr Metab. (2022) 47:439–46. doi: 10.1139/apnm-2021-0721
55. Rogers B, Giles D, Draper N, Mourot L, Gronwald T. Detection of the anaerobic threshold in endurance sports: validation of a new method using correlation properties of heart rate variability. J Funct Morphol Kinesiol. (2021) 6:38. doi: 10.3390/jfmk6020038
56. Farinatti P, Castinheiras Neto AG, Amorim PR. Oxygen consumption and substrate utilization during and after resistance exercises performed with different muscle mass. Int J Exerc Sci. (2016) 9:77–88.
57. Islam H, Townsend LK, Hazell TJ. Modified sprint interval training protocols. Part I Physiological responses. Appl Physiol Nutr Metab. (2017) 42:339–46. doi: 10.1139/apnm-2016-0478
58. McGarvey W, Jones R, Petersen S. Excess post-exercise oxygen consumption following continuous and interval cycling exercise. Int J Sport Nutr Exerc Metab. (2005) 15:28–37. doi: 10.1123/ijsnem.15.1.28
59. MacArthur DG, North KN, A. Gene for speed? The evolution and function of alpha-actinin-3. BioEssays. (2004) 26:786–95. doi: 10.1002/bies.20061
60. Papadimitriou ID, Lucia A, Pitsiladis YP, Pushkarev VP, Dyatlov DA, Orekhov EF, et al. Actn3 R577x and Ace I/D gene variants influence performance in elite sprinters: a multi-cohort study. BMC Genom. (2016) 17:1–8. doi: 10.1186/s12864-016-2462-3
61. Quinlan KG, Seto JT, Turner N, Vandebrouck A, Floetenmeyer M, Macarthur DG, et al. Alpha-actinin-3 deficiency results in reduced glycogen phosphorylase activity and altered calcium handling in skeletal muscle. Hum Mol Genet. (2010) 19:1335–46. doi: 10.1093/hmg/ddq010
Keywords: coronary artery disease, exercise intensity, peak oxygen uptake, anaerobic threshold, meta-analysis
Citation: Zheng L, Pan D, Gu Y, Wang R, Wu Y and Xue M (2022) Effects of high-intensity and moderate-intensity exercise training on cardiopulmonary function in patients with coronary artery disease: A meta-analysis. Front. Cardiovasc. Med. 9:961414. doi: 10.3389/fcvm.2022.961414
Received: 04 June 2022; Accepted: 24 August 2022;
Published: 20 September 2022.
Edited by:
Leonardo Roever, Federal University of Uberlandia, BrazilReviewed by:
Alice Bonomi, Monzino Cardiology Center (IRCCS), ItalyMohanad Alkhodari, Khalifa University, United Arab Emirates
Copyright © 2022 Zheng, Pan, Gu, Wang, Wu and Xue. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mei Xue, meiar@126.com
 Liying Zheng
Liying Zheng Deng Pan
Deng Pan Yimeng Gu1
Yimeng Gu1  Rumeng Wang
Rumeng Wang Mei Xue
Mei Xue