Abstract
Purpose
To compare sleep disturbance from 5 years pre- to 5 years post-diagnosis between breast cancer survivors (BCS) and women without cancer over the same period and to identify BCS subgroups exhibiting different sleep trajectories.
Methods
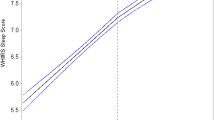
Analyses included data from 152 BCS and 2163 controls from 20 years of follow-up in the longitudinal Study of Women’s Health Across the Nation (SWAN), a multi-racial/ethnic cohort study. SWAN participants were assessed approximately annually from 1995 to 2015 using a standardized protocol. Pink SWAN focused on women who reported no cancer at SWAN enrollment and developed incident breast cancer after enrollment or did not develop breast cancer. Nonparametric locally weighted scatterplot smoothing plots and linear mixed models were used to compare the prevalence of the most frequently reported sleep problem, frequently waking several times a night (a sleep maintenance problem) during the previous 2 weeks, between BCS and controls in the 5 years pre- to 5 years post-diagnosis. We characterized heterogeneity among BCS on this sleep problem using group-based trajectories and examined pre-diagnosis variables as predictors of group membership.
Results
No differences were found between BCS and controls in prevalence of frequent nighttime awakenings either before or after diagnosis. Among BCS, three trajectory groups were identified. Thirty-seven percent of BCS had consistently low prevalence of waking several times per night, 30% had high prevalence, and 33% had increasing prevalence which started 2 years pre-diagnosis. Prevalence of pre-diagnosis vasomotor symptoms, anxiety, depressive symptoms, and smoking differed among these groups.
Conclusion
Among mid-aged women diagnosed with breast cancer, this diagnosis did not trigger/amplify a sleep maintenance problem. The majority of BCS had similar levels of this sleep problem from pre- to post-diagnosis.
Implications for Cancer Survivors
Although sleep maintenance problems were not amplified by a cancer diagnosis, a subset of BCS may have sleep issues that should be monitored and treated, as indicated.


Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Howlader N, Noone AM, Krapcho M, Miller D, Brest A, Yu M, et al. (Eds). SEER cancer statistics review, 1975–2016. Bethesda: National Cancer Institute. https://seer.cancer.gov/csr/1975_2016/, based on November 2018 SEER data submission, posted to the SEER web site, April 2019.
Miller KD, Nogueira L, Mariotto AB, et al. Cancer treatment and survivorship statistics, 2019. CA Cancer J Clin. 2019;69(5):363–85. https://doi.org/10.3322/caac.21565.
Whisenant M, Wong B, Mitchell SA, et al. Distinct trajectories of fatigue and sleep disturbance in women receiving chemotherapy for breast cancer. Oncol Nurs Forum. 2017;44(6):739–50. https://doi.org/10.1188/17.ONF.739-750.
Dhruva A, Paul SM, Cooper BA, et al. A longitudinal study of measures of objective and subjective sleep disturbance in patients with breast cancer before, during, and after radiation therapy. J Pain Symptom Manage. 2012;44(2):215–28.
Grayson S, Sereika S, Harpel C, et al. Factors associated with sleep disturbances in women undergoing treatment for early-stage breast cancer. Support Care Cancer. 2022;30(1):157–66. https://doi.org/10.1007/s00520-021-06373-9.
Costa AR, Fontes F, Pereira S, et al. Impact of breast cancer treatments on sleep disturbances - a systematic review. Breast. 2014;23(6):697–709. https://doi.org/10.1016/j.breast.2014.09.003.
Leysen L, Lahousse A, Nijs J, et al. Prevalence and risk factors of sleep disturbances in breast cancer survivors: systematic review and meta-analyses. Support Care Cancer. 2019;27(12):4401–33. https://doi.org/10.1007/s00520-019-04936-5.
Accortt EE, Bower JE, Stanton AL, et al. Depression and vasomotor symptoms in young breast cancer survivors: the mediating role of sleep disturbance. Arch Womens Ment Health. 2015;18(3):565–8. https://doi.org/10.1007/s00737-015-0504-5.
Fortner BV, Stepanski EJ, Wang SC, et al. Sleep and quality of life in breast cancer patients. J Pain Symptom Manage. 2002;24(5):471–80.
Beverly CM, Naughton MJ, Pennell ML, et al. Change in longitudinal trends in sleep quality and duration following breast cancer diagnosis: results from the Women’s Health Initiative. NPJ Breast Cancer. 2018;4:15–15. https://doi.org/10.1038/s41523-018-0065-7.
Van OC, Cooper BA, Lee K, et al. Identification of distinct subgroups of breast cancer patients based on self-reported changes in sleep disturbance. Support Care Cancer. 2012;20(10):2611–9. https://doi.org/10.1007/s00520-012-1381-3.
Fontes F, Severo M, Gonçalves M, et al. Trajectories of sleep quality during the first three years after breast cancer diagnosis. Sleep Med. 2017;34:193–9. https://doi.org/10.3390/healthcare10040661.
Zhang B, Wing YK. Sex differences in insomnia: a meta-analysis. Sleep. 2006;29(1):85–93. https://doi.org/10.1093/sleep/29.1.85.
Lampio L, Polo-Kantola P, Polo O, et al. Sleep in midlife women: effects of menopause, vasomotor symptoms, and depressive symptoms. Menopause. 2014;21(11):1217–24. https://doi.org/10.1097/gme.0000000000000239.
Ancoli-Israel S, Liu L, Rissling M, et al. Sleep, fatigue, depression, and circadian activity rhythms in women with breast cancer before and after treatment: a 1-year longitudinal study. Support Care Cancer. 2014;22(9):2535–45. https://doi.org/10.1007/s00520-014-2204-5.
Mandelblatt JS, Zhai W, Ahn J, et al. Symptom burden among older breast cancer survivors: the Thinking and Living With Cancer (TLC) study. Cancer. 2020;126(6):1183–92. https://doi.org/10.1002/cncr.32663.
Kravitz HM, Janssen I, Bromberger JT, et al. Sleep trajectories before and after the final menstrual period in the Study of Women’s Health Across the Nation (SWAN). Curr sleep Med Rep. 2017;3(3):235–50. https://doi.org/10.1007/s40675-017-0084-1.
Wang Y, Zhu X, Li L, et al. What factors affect the insomnia symptom trajectories in women with nonmetastatic breast cancer? J Pain Symptom Manage. 2016;52(6):850–8. https://doi.org/10.1016/j.jpainsymman.2016.07.001.
Bean HR, Diggens J, Ftanou M, et al. Insomnia and fatigue symptom trajectories in breast cancer: a longitudinal cohort study. Behav Sleep Med. 2021;19(6):814–27. https://doi.org/10.1080/15402002.2020.1869005.
Kocevska D, Lysen TS, Dotinga A, et al. Sleep characteristics across the lifespan in 1.1 million people from the Netherlands, United Kingdom and United States: a systematic review and meta-analysis. Nat Hum Behav. 2021;5(1):113–22. https://doi.org/10.1038/s41562-020-00965-x.
Baker FC, Lampio L, Saaresranta T, et al. Sleep and sleep disorders in the menopausal transition. Sleep Med Clin. 2018;13(3):443–56. https://doi.org/10.1016/j.jsmc.2018.04.011.
Sowers M, Crawford S, Sternfeld B, et al. SWAN: a multicenter, multiethnic, community-based cohort study of women and the menopausal transition. In: Lobo RA, Kelsey J, Marcus R, editors., et al., Menopause: biology and pathology. San Diego: Academic Press; 2000. p. 175–88.
Bromberger JT, Kravitz HM, Chang Y, et al. Does risk for anxiety increase during the menopausal transition? Study of Women’s Health Across the Nation. Menopause (New York, NY). 2013;20(5):488–95. https://doi.org/10.1097/GME.0b013e3182730599.
Radloff LS. The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1(3):385–401.
Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24(4):385–96.
Cleveland WS, Devlin SJ. Locally weighted regression: an approach to regression analysis by local fitting. J Am Stat Assoc. 1988;83(403):596–610. https://doi.org/10.2307/2289282.
Fitzmaurice GM, Laird NM, Ware JH. Applied longitudinal analysis. Hoboken, NJ: Wiley; 2004.
Nagin D. Group-based modeling of development. Cambridge: Harvard University Press; 2005. https://doi.org/10.4159/9780674041318
Savard J, Villa J, Ivers H, et al. Prevalence, natural course, and risk factors of insomnia comorbid with cancer over a 2-month period. J Clin Oncol. 2009;27(31):5233–9. https://doi.org/10.1200/jco.2008.21.6333.
Berrett-Abebe J, Cadet T, Pirl W, et al. Exploring the relationship between fear of cancer recurrence and sleep quality in cancer survivors. J Psychosoc Oncol. 2015;33(3):297–309. https://doi.org/10.1080/07347332.2015.1020586.
Palesh OG, Collie K, Batiuchok D, et al. A longitudinal study of depression, pain, and stress as predictors of sleep disturbance among women with metastatic breast cancer. Biol Psychol. 2007;75(1):37–44. https://doi.org/10.1016/j.biopsycho.2006.11.002.
Ma Y, Hall DL, Ngo LH, et al. Efficacy of cognitive behavioral therapy for insomnia in breast cancer: a meta-analysis. Sleep Med Rev. 2021;55:101376. https://doi.org/10.1016/j.smrv.2020.101376.
Kwak A, Jacobs J, Haggett D, et al. Evaluation and management of insomnia in women with breast cancer. Breast Cancer Res Treat. 2020;181(2):269–77. https://doi.org/10.1007/s10549-020-05635-0.
Funding
The Study of Women’s Health Across the Nation (SWAN) is supported by the National Institutes of Health (NIH), DHHS, through the National Institute on Aging (NIA), the National Institute of Nursing Research (NINR), and the Office of Research on Women’s Health (ORWH) (Grants U01NR004061, U01AG012505, U01AG012535, U01AG012531, U01AG012539, U01AG012546, U01AG012553, U01AG012554, U01AG012495, and U19AG063720). Pink SWAN was supported by the National Cancer Institute R01CA199137. The content of this article is solely the responsibility of the authors and does not necessarily represent the official views of the NCI, NIA, NINR, ORWH, or the NIH. Dr. Goyal was supported by the National Cancer Institute R25 CA122061.
Author information
Authors and Affiliations
Contributions
Nancy E. Avis: conceptualization, formal analysis, funding acquisition, writing—original draft. Beverly Levine: formal analysis, writing—original draft. Sybil L. Crawford: funding acquisition, formal analysis, writing—review and editing. Neha Goyal: formal analysis, writing—original draft, review, and editing.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Institutional Board at each site. All participants provided written informed consent.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Goyal, N., Levine, B.J., Crawford, S.L. et al. Sleep disturbance among breast cancer survivors and controls from midlife to early older adulthood: Pink SWAN. J Cancer Surviv 18, 489–498 (2024). https://doi.org/10.1007/s11764-022-01247-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11764-022-01247-3