Laboratory Studies
A complete laboratory evaluation is required not only to diagnose exocrine pancreatic insufficiency (EPI) but also to determine the extent of the malabsorption and assess manifestations of the underlying disease, if present.
Blood tests
A complete blood count (CBC) may reveal microcytic anemia due to iron deficiency or macrocytic anemia due to vitamin B-12 or folate malabsorption. Serum iron, vitamin B-12, and folate concentrations may help establish the diagnosis of EPI. Prothrombin time (PT) may be prolonged because of malabsorption of vitamin K, a fat-soluble vitamin. A study by Lindkvist et al found that serum nutritional markers (eg, magnesium, albumin, prealbumin) can be used to determine the probability of EPI in patients with chronic pancreatitis. [27]
Malabsorption can involve electrolyte imbalances such as hypokalemia, hypocalcemia, hypomagnesemia, and metabolic acidosis. Protein malabsorption may cause hypoproteinemia and hypoalbuminemia. Fat malabsorption can lead to low serum levels of triglycerides, cholesterol, and alpha- and beta-carotene. The Westergren erythrocyte sedimentation rate (ESR) may provide a clue to an underlying autoimmune disease.
Serum levels of antigliadin and antiendomysial antibodies can be used to help diagnose celiac sprue. The serum immunoglobulin A (IgA) level can be assessed to rule out IgA deficiency.
Stool tests
Determination of fecal elastase (a protease that is produced by the pancreas and that remains intact in the stool) can be used to support the clinical diagnosis of EPI.
Tests of malabsorption
A full malabsorption workup is required to differentiate EPI from other causes of malabsorption. Such a workup may include a number of tests, as follows.
Fat absorption tests
A fat absorption test is usually the first one ordered because there are many disease processes that can result in fat malabsorption. For quantitative measurement of fat absorption, a 72-hour fecal fat collection is often performed and is considered the standard. Qualitative tests include the acid steatocrit test and Sudan III stain of stool, but these tests are less reliable.
Patients are instructed to consume a normal amount (80-100 g/day) of fat before and during the collection. On the basis of this level of intake, fecal fat excretion in healthy individuals should be less than 7 g/day.
The current standard for measuring fat malabsorption is the coefficient of fat absorption (CFA), [12] which is the percentage of absorbed fat in the diet. Normally, the CFA is approximately 90%. The various diseases that can give rise to EPI will produce different degrees of pancreatic insufficiency and, hence, different CFAs. For example, cystic fibrosis often results in a CFA lower than 40%, which typically increases to more than 80% with therapy.
D-xylose test
If the 72-hour fecal fat collection results demonstrate fat malabsorption, the D-xylose test is used to document the integrity of the intestinal mucosa.
D-xylose is readily absorbed in the small intestine. Approximately half of the absorbed D-xylose is excreted in urine without being metabolized. If absorption of D-xylose is impaired by either a luminal factor (eg, bacterial overgrowth) or a reduced or damaged mucosal surface area (eg, from surgical resection or celiac disease), urinary excretion will be lower than normal. Cases of pancreatic insufficiency usually result in normal urinary excretion because absorption of D-xylose is still intact.
Carbohydrate absorption test
A simple sensitive test for carbohydrate malabsorption is the hydrogen breath test, in which patients are given an oral solution of lactose. [28, 29] In cases of lactase deficiency, colonic organisms digest the unabsorbed lactose, which results in an elevated hydrogen content in the expired air.
Bacterial overgrowth or rapid transit also can cause an early rise in breath hydrogen, in which case it is necessary to use glucose instead of lactose to make a diagnosis. However, 18% of patients are hydrogen nonexcretors, in whom the hydrogen breath test will yield false-negative test results.
Bile salt absorption test
The bile salt breath test can determine the integrity of bile salt metabolism. The patient is given an oral conjugated bile salt, such as glycine cholic acid with the glycine radiolabeled in the carbon position. The bile salt is deconjugated and subsequently metabolized by bacteria. If interrupted enterohepatic circulation (eg, from bacterial overgrowth, ileal resection, or disease), a radioactively labeled elevated breath carbon dioxide level will be noted.
Schilling test
Malabsorption of vitamin B-12 may occur as a consequence of an intrinsic factor deficiency (eg, from pernicious anemia or gastric resection), pancreatic insufficiency, bacterial overgrowth, ileal resection, or disease. The 3-stage Schilling test can often help differentiate these conditions.
13C-D-xylose breath test
A study by Hope et al suggested that small intestinal malabsorption in chronic alcoholism may be identified by means of a13 C-D-xylose breath test. [30] The investigators evaluated this test in 14 alcoholics, compared the results with those obtained from untreated celiac disease patients and healthy control subjects, and correlated the breath test findings with the morphologic findings from the duodenal mucosa.
In this study, absorption of13 C-D-xylose was significantly less in the alcoholic patients than in healthy control subjects, whereas the time curve of13 C-D-xylose absorption in the alcoholics was similar to that in the untreated celiac patients. [30] In addition, although few changes were observed on light microscopy in the alcoholics, morphologic pathology (primarily reduced surface area of microvilli) was observed on electron microscopy in the majority of the patients.
Pancreatic Function Tests
Pancreatic function can be measured directly by using endoscopy or the Dreiling tube method after stimulation with secretin or cholecystokinin (CCK). Direct pancreatic function testing is the most sensitive approach to assessment of exocrine pancreatic function and is usually performed at specialized centers. [6] Various methods have been developed. [31]
Direct testing
Whereas the CCK test measures the ability of the acinar cells to secrete digestive enzymes, the secretin test measures the ability of the ductal cells to secrete bicarbonate. Although both tests yield abnormal results in advanced EPI, it is not known which of the 2 secretagogues offers better sensitivity for early EPI. In uncertain cases, both CCK and secretin tests may be ordered.
Secretin test
In the secretin test, porcine or human synthetic secretin is given in doses ranging from 0.5 to 5 clinical units (CU)/kg. Duodenal fluid is continuously collected in 15-minute aliquots for 1 hour. The fluid is analyzed for bicarbonate concentration, volume, and total bicarbonate output.
A bicarbonate concentration lower than 80 mEq/L in all 4 aliquots represents exocrine insufficiency. A peak bicarbonate cutoff of 90 mEq/L has been advocated by some investigators. A peak bicarbonate concentration lower than 50 mEq/L is indicative of severe exocrine insufficiency. When the bicarbonate concentration is equivocal, volume and total bicarbonate output are used as secondary diagnostic parameters.
CCK test
Use of a CCK receptor agonist (eg, cerulein) as a hormonal stimulant provides information on pancreatic enzyme-secreting capacity. Two endoscopic tubes are placed: (1) a single-lumen gastric tube and (2) a double-lumen duodenal tube. The gastric tube continuously collects and discards gastric fluid to prevent acidification of the duodenum. One duodenal lumen continuously collects duodenal drainage fluid, whereas the other is used for administration of a mannitol-saline solution containing a nonabsorbable marker (polyethylene glycol [PEG]).
An accurate determination is made of enzyme concentration, enzyme output, and fluid volume on the basis of recovery of the PEG marker. Measurement of perfusion markers requires a specialized laboratory.
Secretin-CCK test
Many pancreatic research centers use the combined secretin-CCK test, which allows simultaneous assessment of ductal and acinar secretory capacity. Many dosing regimens have been used for this test. The 2 hormones are administered, and the concentration and output of both bicarbonate and pancreatic enzymes are evaluated.
Indirect testing
Pancreatic function can also be measured indirectly. Qualitative fecal fat analysis via microscopic examination of random stool samples is used as a screening test only. [32] In addition, measurement of fecal elastase levels may serve as an indirect indicator of pancreatic function; however, sensitivity is limited to moderate or severe disease, and the result can be falsely positive owing to dilution by watery stools. [6] The typical findings in EPI are increased fecal fat and decreased enzymes.
A prospective study by González-Sánchez et al suggested that with regard to sensitivity, specificity, and positive and negative predictive values, results from the fecal elastase-1 (FE-1) test are similar to those from the 13C-mixed triglyceride breath test (TGBT) in the diagnosis of EPI in chronic pancreatitis. However, the TGBT appeared to be more accurate than the FE-1 test in operated patients with chronic pancreatitis. [33]
Abdominal Imaging
Abdominal imaging (see the image below) can help in identifying features of chronic pancreatitis, which is the most common cause of EPI. Because fat maldigestion is not evident until pancreatic lipase secretion falls below 10% of normal, some patients with confirmed chronic pancreatitis may not have the signs and symptoms of EPI.
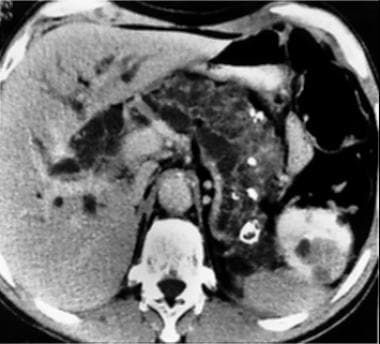 Complete replacement of the pancreas with cystic disease and intrahepatic biliary dilation caused by extrinsic compression of the common bile duct. Note also the renal cysts and masses. This patient had exocrine pancreatic insufficiency. Image courtesy of Wikimedia Commons.
Complete replacement of the pancreas with cystic disease and intrahepatic biliary dilation caused by extrinsic compression of the common bile duct. Note also the renal cysts and masses. This patient had exocrine pancreatic insufficiency. Image courtesy of Wikimedia Commons.
A study by Saad et al indicated that in pediatric patients, a smaller pancreas parenchymal volume on magnetic resonance imaging (MRI) serves as a marker for exocrine and endocrine pancreatic dysfunction. The likelihood that exocrine pancreatic dysfunction would be diagnosed by endoscopic pancreatic function testing (ePFT) or fecal elastase testing was found to be greater in children whose pancreas parenchymal volume was reduced by 5 mL, the odds ratios (ORs) for such diagnosis in ePFT and fecal elastase testing both being 1.16. For the subset of patients without acute pancreatitis, the ORs were 1.29 and 1.23, respectively. [34]
-
Complete replacement of the pancreas with cystic disease and intrahepatic biliary dilation caused by extrinsic compression of the common bile duct. Note also the renal cysts and masses. This patient had exocrine pancreatic insufficiency. Image courtesy of Wikimedia Commons.
-
Residual islets in dense fibrous stroma secondary to loss of exocrine pancreatic tissue in chronic pancreatitis (hematoxylin-eosin stain, medium magnification). Image courtesy of Dr. Rose Anton.
-
Pancreas anatomy.
-
The duodenum and pancreas.
-
The pancreas and duodenum, posterior view.
-
Factors controlling release of pancreatic secretions. Image courtesy of Wikimedia Commons.
-
Defective protein transmembrane conductance regulator (CFTR) in cystic fibrosis.







