ADHD, Bipolar Disorder, or Both?
Linda Jo Volness, MS, RN, is a psychiatric clinical nurse specialist who is board certified in child, adolescent, and adult mental illness. At Quality of Life in Fargo, ND, Volness has extensive experience with children who have ADHD and BD. "One of the most common scenarios I encounter in practice," says Volness, "is the child diagnosed with severe ADHD and oppositional defiant disorder, who is not getting better with current treatment, and who probably has BD. These kids need to be screened very closely. They will usually be given the ADHD diagnosis, but the bipolar diagnosis is down the road."
Misdiagnosis and symptom overlap are 2 of the problems resulting from comorbid ADHD and BD.[14] The complex presentation of many of these children can be confusing.[15] Volness adds, "It's difficult because some of these kids won't have classic mood swings. You can have bipolar disorder with chronic mania as the main symptom."
Establishing the correct diagnosis is essential to instituting the correct treatment, and all comorbid conditions must be identified. Individually and combined, these conditions require different medications, psychotherapy, and other aspects of management. A child who is improperly diagnosed may not only receive the wrong treatment needed to alleviate the most severe symptoms, but also valuable educational and developmental time is wasted, and both child and family will suffer needlessly. Moreover, administering the wrong treatment can make the child's condition worse. The nurse can help to establish the correct diagnosis by observing, questioning, and relaying pertinent and appropriate data to the mental health provider.
Distinguishing ADHD and Bipolar Disorder
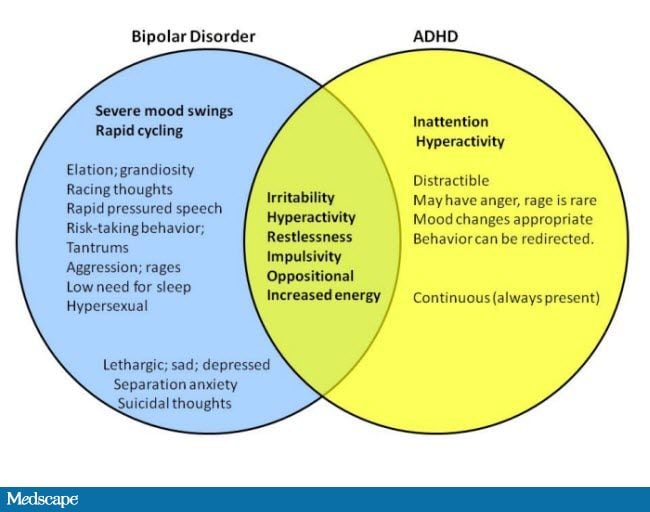
The confusion that often thwarts attempts to differentiate ADHD and BD stems from the high rate of comorbidity between these 2 disorders, as well as the comorbidity between BD or ADHD and a host of other pediatric mental health disorders ( Table 3 ). It can be challenging to establish the correct diagnosis in a child who has symptoms, such as irritability, restlessness, and impulsivity, which are commonly observed in children with comorbid mental health disorders.
However, in spite of the overlap in defining features, it is possible to recognize ADHD or BD when they coexist with each other or with other mental health disorders.[5] The Figure presents a visual depiction of where ADHD and BD often intersect. Some symptoms, such as irritability, that can indicate either disorder, ultimately may not be helpful in establishing a diagnosis.
Figure.
Possible Symptoms of Bipolar Disorder and ADHD in Children, Showing Overlap in Clinical Symptoms
Clues to Primary ADHD
Generally, the symptoms of ADHD are always present and aren't cyclical.[2] A child who has only ADHD doesn't have severe mood swings. Children with ADHD may talk a lot, but not with the same pressured quality and gear-switching seen in BD. And although children with ADHD can exhibit irritability and aggression, these symptoms should not be extreme. Severe, uncontrollable aggression should arouse suspicion for BD.[16]
In a child demonstrating symptoms that could be characteristic of either ADHD or BD, the presentation and pattern of a behavior, such as a high activity level, is important. In children with ADHD, from the time they are walking, they are "wearing the soles off their shoes."[17] In children with BD, the hyperactivity is more episodic.[17]
Clues to Primary Bipolar Disorder
The 5 symptoms with the best discrimination for BD are elated mood, grandiosity, flight of ideas/racing thoughts, decreased need for sleep, and hypersexuality.[18] If these are among the child or adolescent's primary symptoms, the diagnosis is likely BD. To avoid misdiagnosing a child as having BD when in fact, the child has severe ADHD, either elated/euphoric mood or grandiosity should be present. To establish the existence of mania, a prerequisite for a diagnosis of pediatric bipolar disorder, the child should exhibit episodes of a distinct change in mood accompanied by changes in cognition and behavior.[11] Symptoms such as distractibility and agitation indicate BD only if they are markedly increased over the child's baseline symptoms and are concurrent with a distinct change in mood.
The symptoms of BD that don't overlap with ADHD are the mood symptoms and depressive symptoms, such as crying (suggesting depression) and bossiness or cockiness (suggesting grandiosity in a child). Grandiosity is more than an elevated self-esteem, it is when the child believes he or she is smarter or more capable than anyone else, orders peers and adults around, and may even believe he or she has special skills or talents.[15] Similarly, elation in a child is more than situationally appropriate giggling -- it is when a child acts too cheerful or silly, or "on top of the world," in a way that is disturbing and uncomfortable, and can't be redirected by adults.[15] Although both ADHD and BD children can have impaired social skills compared with typical children, children with BD have fewer friends, poorer social skills, and poor sibling relations.
Children and adolescents who demonstrate exaggerated mood swings that range from extreme highs (excited or manic phases) to extreme lows (depression) are more likely to have BD. Periods of moderate mood occur in between the extreme highs and lows. During manic phases, the child may talk nonstop, need very little sleep, and show unusually poor judgment. At the low end of the mood swing, children can experience severe depression, but this low mood may not manifest the same as it would in an adult. Depression in a child can be reflected in irritability, or in anhedonia (a marked lack of interest or pleasure in activities).[15] Chronically hypomanic children are often misdiagnosed as having primary ADHD.
Clues that More Is Going On
Just when it might seem that these 2 disorders can be differentiated, this monkey wrench is thrown into the mix: A large majority (85%) of children and adolescents with BD also qualify for a diagnosis of ADHD. And although ADHD more commonly occurs alone, about 20% also have BD. In the child whose ADHD is superimposed on BD, the symptoms of ADHD are present when the child is in a manic phase.
A lack of response or an unexpected response to treatment should prompt clinicians to assess the accuracy of the diagnosis and consider the possibility of undiagnosed coexisting conditions.[5] A common scenario is the child who is initially diagnosed with ADHD and given stimulants and/or antidepressants. Stimulants given for ADHD that are unopposed by mood stabilizers can worsen bipolar symptoms, increasing mania and aggression. Children with undiagnosed BD will either not respond or may suffer more severe symptoms of mania such as rages, insomnia, agitation, and pressured speech. Parents may describe them as "bouncing off the wall." The exacerbation of mania triggered by stimulants can even lead to hospitalization for suicide attempts.
The Effects of Age and Development on Symptom Presentation
In children, the signs and symptoms of mental illness are superimposed on the processes of normal development, a fact that can make it difficult to determine which behaviors might suggest mental illness. Normal and abnormal development are often separated only by differences of degree.[19] For example, mood swings are a common part of adolescence, and in and of themselves do not suggest pathology.[15] However, when mood swings occur to such a degree that they impair the adolescent's functioning, this might signal more than the stress of being a teenager. The signs and symptoms of a mental disorder can wax and wane in response to unfolding development and changing relationships with family and the broader social environment.[19]
It is more difficult in children than in adults to characterize features such as elation and grandiosity.[20] Normal childhood play behaviors must be separated from potentially significant evidence of mania. McDougall emphasizes that the nurse must be careful in distinguishing the high spirits of childhood from true elation.[1] Children often boast and play act, pretending to be strong and important figures, but this does not necessarily represent grandiosity. The context in which the behaviors occur may offer a clue. In children with BD, a behavior isn't just situation- or environment-dependent (eg, playing a make-believe game with a group of friends), but pervasive and impairing.
The symptoms of BD are known to vary according to the age of the child. Weller reports that in children aged 1-8 years, the predominant symptoms of BD are irritability and psychomotor agitation, while in those aged 6-12 years, the symptoms are divided between an elevated mood and irritability.[17] Symptoms of BD are more likely to be exhibited after age 7 years. Symptoms of ADHD are often apparent in children younger than 7 years.
Topics in Advanced Practice Nursing eJournal. 2009;9(4) © 2009 Medscape, LLC
Cite this: Bipolar Disorder and ADHD in Children: Confusion and Comorbidity - Medscape - Oct 27, 2009.










Comments