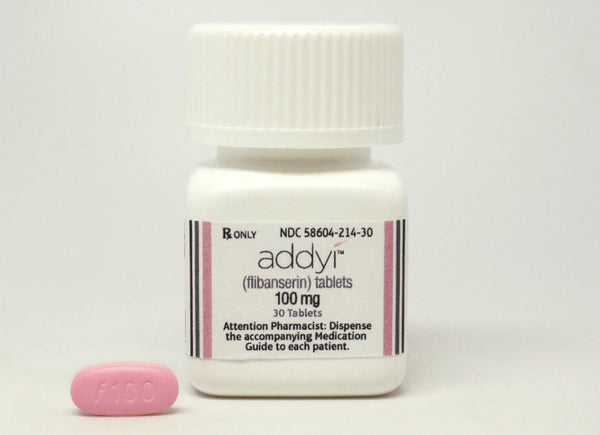
Addyi, the first prescription medication approved to boost female libido, hits the market today. The U.S. Food and Drug Administration has approved marketing the drug to premenopausal women whose low libido doesn’t stem from a medical or psychiatric condition, medication or other substances, but from a lack of desire characterized as hypoactive sexual desire disorder, or HSDD.
The so-called “female Viagra”—something of a misnomer because Addyi does not affect arousal as Viagra does but rather increases libido—was mired in controversy prior to its approval, in large part because clinical studies did not show dramatic improvements in sexual desire and used measures that many experts criticized as inadequate. Despite such concerns, Addyi’s drugmaker, Sprout Pharmaceuticals, was purchased by Valeant Pharmaceuticals International for $1 billion once the drug received approval.
With about 10 percent of women suffering from HSDD, Valeant projects a healthy market for this once-a-day pill, and that does not include a large group of women who are likely to be prescribed the drug for another kind of desire problem: the low libido that is a common side effect of antidepressants.
On supporting science journalism
If you're enjoying this article, consider supporting our award-winning journalism by subscribing. By purchasing a subscription you are helping to ensure the future of impactful stories about the discoveries and ideas shaping our world today.
Although Addyi has not been approved by the FDA for antidepressant-induced libido problems, once a drug hits the market, doctors can prescribe it off-label for other uses other than its approved indication. Nearly one in five women in the U.S. takes an antidepressant, and as many as 70 percent report dampened sexual desire as a result.
Selective serotonin (SSRI) and certain serotonin and noradrenaline (SNRI) reuptake inhibitor antidepressants are particularly likely to cause sexual dysfunction. The exact mechanisms are not well understood but likely stem from boosting serotonin activity in the brain. Serotonin is thought to dampen libido and arousal, and also to inhibit two other neurotransmitters, norepinephrine and dopamine, that promote sexual function. Doctors have tried various strategies, including reducing dosages, prescribing “drug holidays,” and adding in other antidepressants like Wellbutrin or drugs like Ritalin, to counteract these sexual side effects, but have not found a reliable antidote. “There’s nothing really phenomenal out there to treat SSRI-induced dysfunction,” says Christina Dording, a psychiatrist who directs sexual behavior studies at Massachusetts General Hospital’s depression research division. “Clinically we use a variety of different strategies but none of them are perfect.”
Dording and many colleagues point out that no one knows whether Addyi would be effective for women whose low libido stems from antidepressants. In theory, Addyi might work, says Anita Clayton, a University of Virginia psychiatrist who is an expert in antidepressant-induced sexual dysfunction, because it inhibits the sex-dampening effects of serotonin.
In clinical trials measuring the drug’s effectiveness the manufacturer excluded subjects who were taking an antidepressant or other drugs likely to harm sexual functioning.
Despite protocols, a few women in those efficacy studies did take an antidepressant. But because the study was not designed to measure how effective Addyi was for antidepressant users or for women whose low libido stemmed from antidepressant use, any data gleaned for would be “pretty much uninterpretable,” says Leonard Derogatis, a professor of psychiatry at Johns Hopkins University who has advised the drug’s manufacturer for a decade and who conducted many of the clinical trials. Representatives from the manufacturer, Sprout, declined to comment.
Cherry-picking patients to minimize confounding variables is a common strategy in drug trials but it doesn’t reflect the reality of clinical practice, says Rosemary Basson, director of the sexual medicine program at the University of British Columbia. Because many women with HSDD also have mood disorders and take an antidepressant, it is difficult to tease out whether a woman’s libido problems stem from her depression or other mood disorder, or from her antidepressants, relationship or other issues or from HSDD—itself a controversial diagnosis. “What’s very important is to document the level of sexual function prior to treatment with the antidepressant,” says Shari Lusskin, psychiatrist and professor at Icahn School of Medicine at Mount Sinai in New York City who specializes in women’s mental health. Unfortunately, she notes, “that’s not something that’s routinely done.”
The drug’s original developer, Boehringer Ingelheim, which later sold Addyi to Sprout, did conduct a 2010 study of depressed women with low libido to gauge whether it was safe to take Addyi with an antidepressant. The data, says Clayton, who helped plan the study, showed Addyi didn’t worsen anxiety or depression, although combining the drugs slightly increased the risk of some side effects including insomnia and dizziness.
Basson, Dording and others say they would hold off on prescribing Addyi to their patients with antidepressant-induced low libido until there is promising data to support its use—especially because even in women with HSDD, libido improvement was not dramatic and there was a risk of serious side effects like fainting and very low blood pressure, especially when combined with alcohol.
But not all doctors will be so cautious. “It will be used off-label—absolutely,” says Lusskin, who also says she would not do so herself in the absence of promising data for this subgroup. “People will ask for it, and doctors will prescribe it. It’s really the doctor’s responsibility to tell patients whether something is appropriate for them or not, but I’m afraid doctors are often willing to do what patients ask.”
Sprout would not comment on whether they plan to seek additional marketing approval to treat antidepressant-induced low libido, and the new parent company, Valeant, did not respond to requests for comment. But Derogatis and Clayton, who both served as scientific advisors to the manufacturer, think it might make sense to seek additional approvals, given the large number of women suffering from antidepressant-induced low libido and the dearth of truly effective treatment.
“I know [Sprout] was considering it,” Derogatis says, although he doesn’t know whether Valeant feels the same way. “It’s a natural to start looking at what marketing population would be beneficial. And depressed women [with antidepressant-induced low libido] jump right out.”