Approach Considerations
The American Academy of Pediatrics Safe and Healthy Beginnings Project was established to facilitate implementation of the 2004 guidelines for management of hyperbilirubinemia using a systems-based approach. The three key aspects of this project include (1) assessment of risk for severe hyperbilirubinemia before hospital discharge, (2) breastfeeding support, and (3) care coordination between the nursery and primary care. [29]
Transfer infants with pathologic jaundice or bilirubin levels greater than 20 mg/dL to a center capable of performing exchange transfusions.
If the infant is treated on an outpatient basis, measure serum bilirubin levels either daily in the clinic or in the home with home-health nurses until the bilirubin level is less than 15 mg/dL (260 µmol/L).
Provide gravidas with excellent breastfeeding education. Refer them to a lactation consultant or La Leche League.
Medical Care
Medication is not currently a component of care for breast milk jaundice (BMJ).
Treatment recommendations in this section apply only to healthy term infants with no signs of pathologic jaundice and are based on the severity of the hyperbilirubinemia. In preterm, anemic, or ill infants and those with early (< 24 hours) or extreme jaundice (>25 mg/dL or 430 µmol/L), different treatment protocols should be pursued (see the Medscape Drugs and Diseases article Neonatal Jaundice). [30]
For healthy term infants with breast milk or breastfeeding jaundice who have bilirubin levels of 12 mg/dL (170 µmol/L) to 17 mg/dL, the following options are acceptable:
-
Increase breastfeeding to 8-12 times per day, and recheck the serum bilirubin level in 12-24 hours. Reassure the mother about the relatively benign nature of breast milk jaundice . This recommendation assumes that effective breastfeeding is occurring, including milk production, effective latching, and effective sucking with resultant letdown of milk. Breastfeeding can also be supported with manual or electric pumps and the pumped milk then given as a supplement to the baby.
-
Continue breastfeeding and supplement with formula.
-
Temporary interruption of breastfeeding is rarely needed and is not recommended unless serum bilirubin levels reach 20 mg/dL (340 µmol/L). [31]
For infants with serum bilirubin levels in the range of 17-25 mg/dL (294-430 µmol/L), add phototherapy to any of the previously stated treatment options. The American Academy of Pediatrics (AAP) issued updated practice parameters on the management of hyperbilirubinemia in healthy full-term newborn infants in 2022. These guidelines incorporate gestational age-based phototherapy and exchange transfusion thresholds, neurotoxicity risk factors, use of transcutaneous bilirubin measurements, and follow up after hospital discharge based on the difference between bilirubin level and phototherapy threshold. [32] See Guidelines.
The most rapid way to reduce the bilirubin level is to interrupt breastfeeding for 24 hours, feed with formula, and use phototherapy; however, in most infants, interrupting breastfeeding is not necessary or advisable.
Phototherapy can be administered with standard phototherapy units and fiberoptic blankets. See the image below.
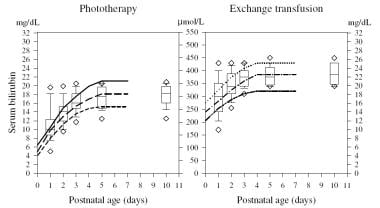 Breast Milk Jaundice. The graph represents indications for phototherapy and exchange transfusion in infants (with a birthweight of 3500 g) in 108 neonatal ICUs. The left panel shows the range of indications for phototherapy, whereas the right panel shows the indications for exchange transfusion. Numbers on the vertical axes are serum bilirubin concentrations in mg/dL (lateral) and mmol/L (middle). In the left panel, the solid line refers to the current recommendation of the American Academy of Pediatrics (AAP) for low-risk infants, the line consisting of long dashes (- - - - -) represents the level at which the AAP recommends phototherapy for infants at intermediate risk, and the line with short dashes (-----) represents the suggested intervention level for infants at high risk. In the right panel, the dotted line (......) represents the AAP suggested intervention level for exchange transfusion in infants considered at low risk, the line consisting of dash-dot-dash (-.-.-.-.) represents the suggested intervention level for exchange transfusion in infants at intermediate risk, and the line consisting of dash-dot-dot-dash (-..-..-..-) represents the suggested intervention level for infants at high risk. Intensive phototherapy is always recommended while preparations for exchange transfusion are in progress. The box-and-whisker plots show the following values: lower error bar = 10th percentile; lower box margin = 25th percentile; line transecting box = median; upper box margin = 75th percentile; upper error bar = 90th percentile; and lower and upper diamonds = 5th and 95th percentiles, respectively.
Breast Milk Jaundice. The graph represents indications for phototherapy and exchange transfusion in infants (with a birthweight of 3500 g) in 108 neonatal ICUs. The left panel shows the range of indications for phototherapy, whereas the right panel shows the indications for exchange transfusion. Numbers on the vertical axes are serum bilirubin concentrations in mg/dL (lateral) and mmol/L (middle). In the left panel, the solid line refers to the current recommendation of the American Academy of Pediatrics (AAP) for low-risk infants, the line consisting of long dashes (- - - - -) represents the level at which the AAP recommends phototherapy for infants at intermediate risk, and the line with short dashes (-----) represents the suggested intervention level for infants at high risk. In the right panel, the dotted line (......) represents the AAP suggested intervention level for exchange transfusion in infants considered at low risk, the line consisting of dash-dot-dash (-.-.-.-.) represents the suggested intervention level for exchange transfusion in infants at intermediate risk, and the line consisting of dash-dot-dot-dash (-..-..-..-) represents the suggested intervention level for infants at high risk. Intensive phototherapy is always recommended while preparations for exchange transfusion are in progress. The box-and-whisker plots show the following values: lower error bar = 10th percentile; lower box margin = 25th percentile; line transecting box = median; upper box margin = 75th percentile; upper error bar = 90th percentile; and lower and upper diamonds = 5th and 95th percentiles, respectively.
Note the following:
-
Fiberoptic phototherapy can often be safely administered at home, which may allow for improved infant-maternal bonding.
-
Although sunlight provides sufficient irradiance in the 425-nm to 475-nm band to provide phototherapy, practical difficulties involved in safely exposing a naked newborn to sunlight, either indoors or outdoors (and avoiding sunburn), preclude the use of sunlight as a reliable phototherapy tool; therefore, it is not recommended.
-
Phototherapy can be discontinued when serum bilirubin levels drop below 15 mg/dL (260 µmol/L).
-
The average bilirubin level rebound has been shown to be less than 1 mg/dL (17 µmol/L); therefore, rechecking the level after discontinuation of phototherapy is not necessary unless the hyperbilirubinemia is due to a hemolytic process. [33]
For an in-depth discussion of phototherapy, see the Medscape Drugs and Diseases article Neonatal Jaundice.
If the infant has not been discharged with the parent, it is important to monitor the baby's daily weights and serum bilirubin concentration for the need for phototherapy as well as assess the caloric intake. Once the serum bilirubin concentration is determined to be within a safe range (< 20 mg/dL) and is not rapidly rising, home phototherapy is an option to consider as long as thorough outpatient follow-up (home visiting nursing assessment or office check-up and bilirubin level monitoring) are feasible.
Weight monitoring is very important in breastfed infants to avoid prolonged and severe jaundice, as well as to avoid hypernatremic dehydration. The general standard indicates that the loss of 10% of the birth weight is considered to be significant.
van Dommelen proposed a reference chart for relative weight change to detect hypernatremic dehydration. [34]
A number of smart phone apps, such as PediTools, BiliBuddy, and BiliCalc, are available to facilitate quick decision making regarding management and follow up.
Consultations
The following consultations may be indicated:
-
Consider consultation with a neonatologist when serum bilirubin levels approach 20 mg/dL (430 µmol/L) or when signs and symptoms suggest pathologic jaundice and the rate of rise in the serum bilirubin level is over 0.5 mg/dL/h.
-
A consultation with a lactation specialist is recommended in any breastfed baby who has jaundice. The expertise of lactation consultants can be extremely helpful, especially in situations in which inadequate breastfeeding is contributing to the jaundice.
Diet and Activity
Diet
Continue breastfeeding, if possible, and increase the frequency of feeding to 8-12 times per day. Depending on maternal preference, breastfeeding can be supplemented or replaced by formula at the same frequency. Supplementation with dextrose solution is not recommended, because it may decrease caloric intake and milk production and may consequently delay the drop in serum bilirubin concentration. Breastfeeding can also be supplemented by pumped breast milk.
Activity
No activity restrictions are necessary. Encourage parents to remove the child from the warmer or infant crib for feeding and bonding. Fiberoptic blankets allow holding and breastfeeding without interruption in treatment.
Prevention
Keys to deterrence and prevention of breast milk jaundice (BMJ) include the following:
-
Poor caloric intake associated with insufficient breastfeeding contributes to the development of severe breast milk jaundice. The first step toward successful breastfeeding is to make sure that mothers nurse their infants at least 8-12 times per day for the first several days, starting from the first hour of life. The whey portion of human milk contains a feedback inhibitory peptide of lactogenesis; hence, effective emptying of the breast with each feeding results in successful lactation.
-
Infants who are nursed more than 8 times during the first 24 hours have earlier meconium passage, reduced maximum weight loss, increased breast milk intake on days 3 and 5, lower serum bilirubin levels and, thus, a significantly lower incidence of severe hyperbilirubinemia (>15 mg/dL) on day 6.
-
Gourley et al demonstrated that beta-glucuronidase inhibition with L-aspartic acid and enzymatically hydrolyzed casein in exclusively breastfed babies resulted in a reduction in the peak serum bilirubin level by 70% in first week of life. [35]
-
According to the American Academy of Pediatrics clinical practice guidelines for the management of hyperbilirubinemia in the newborn aged 35 or more weeks' gestation, exclusive breastfeeding is a major risk factor for severe hyperbilirubinemia; thus, all infants should be evaluated for the risk of subsequent hyperbilirubinemia by plotting their discharge serum bilirubin levels on an hour-specific nomogram. [36]
-
Transcutaneous bilirubinometry is a measurement of yellow color of the blanched skin and subcutaneous tissue, and it can be used as a screening tool. This tool has been shown to be fairly reliable, with good correlation between total serum bilirubin (TSB) and transcutaneous bilirubin (TcB) levels obtained using instruments available in the United States. The TcB measurement tends to underestimate the TSB at higher levels. [37] Confirmation with TSB measurement is indicated in all patients with TcB levels above the 75th percentile and in those in whom therapeutic intervention is considered.
-
Studies have suggested that combining clinical risk factors with predischarge measurement of TSB or TcB levels improves the accuracy of risk assessment for subsequent hyperbilirubinemia. [38] The factors most predictive included predischarge TSB or TcB levels above the 75th percentile, lower gestational age, and exclusive breastfeeding. [39]
-
Newborns who are exclusively breastfed and who have elevated predischarge TcB or TSB levels do not qualify for discharge before 48 hours and should be evaluated for phototherapy in 24 hours. Newborns with TcB and TSB levels in the high-intermediate range and newborns who were born at less than 38 weeks' gestation should undergo repeat TcB and TSB measurements within 24 hours of discharge, or they should receive follow-up within 2 days. [40]
-
Breast Milk Jaundice. The graph represents indications for phototherapy and exchange transfusion in infants (with a birthweight of 3500 g) in 108 neonatal ICUs. The left panel shows the range of indications for phototherapy, whereas the right panel shows the indications for exchange transfusion. Numbers on the vertical axes are serum bilirubin concentrations in mg/dL (lateral) and mmol/L (middle). In the left panel, the solid line refers to the current recommendation of the American Academy of Pediatrics (AAP) for low-risk infants, the line consisting of long dashes (- - - - -) represents the level at which the AAP recommends phototherapy for infants at intermediate risk, and the line with short dashes (-----) represents the suggested intervention level for infants at high risk. In the right panel, the dotted line (......) represents the AAP suggested intervention level for exchange transfusion in infants considered at low risk, the line consisting of dash-dot-dash (-.-.-.-.) represents the suggested intervention level for exchange transfusion in infants at intermediate risk, and the line consisting of dash-dot-dot-dash (-..-..-..-) represents the suggested intervention level for infants at high risk. Intensive phototherapy is always recommended while preparations for exchange transfusion are in progress. The box-and-whisker plots show the following values: lower error bar = 10th percentile; lower box margin = 25th percentile; line transecting box = median; upper box margin = 75th percentile; upper error bar = 90th percentile; and lower and upper diamonds = 5th and 95th percentiles, respectively.








