Abstract
Purpose
The purpose of this study was to conduct a systematic review to assess the effect of exercise on symptoms and quality of life in lung cancer patients.
Methods
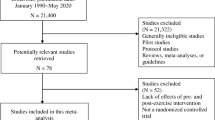
We conducted a systematic review using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines. PubMed, Medline, Embase, Scopus, Web of Science, and SciELO were searched for studies published from January 1998 to January 2019. The review included all randomized controlled trials that evaluated the effect of exercise on symptoms and quality of life of lung cancer patients. Two reviewers independently assessed the quality of all the included studies using the Physiotherapy Evidence Database scale.
Results
In total, ten studies (835 participants) met all inclusion criteria. Three studies investigated the effect of exercise after lung resection, whereas four studies investigated it as a pre-surgery intervention. Two studies investigated the effect of exercise in patients under systemic treatment only, and one study included patients on diverse treatment plans. Exercise protocols consisted of different combinations of strength, aerobic, and inspiratory muscle training. Two trials, including 101 participants, found significant difference in quality of life between groups, favoring the intervention group; and five trials, including 549 participants, found significant inter-group differences in isolated symptoms, also favoring the intervention group.
Conclusions
Exercise can lead to improvements of symptoms and of quality of life in lung cancer survivors. Providing resistance training combined with high-intensity interval aerobic exercise after lung resection seems to be particularly effective. Further studies are warranted to investigate exercise for patients with poor performance status.

Similar content being viewed by others
References
Ferioli M, Zauli G, Martelli AM et al (2018) Impact of physical exercise in cancer survivors during and after antineoplastic treatments. Oncotarget 9:14005–14034. https://doi.org/10.18632/oncotarget.24456
Campbell KL, Winters-Stone KM, Wiskemann J et al (2019) Exercise guidelines for cancer survivors. Med Sci Sport Exerc 51:2375–2390. https://doi.org/10.1249/MSS.0000000000002116
Hayes SC, Newton RU, Spence RR, Galvão DA (2019) The Exercise and Sports Science Australia position statement: exercise medicine in cancer management. J Sci Med Sport 22:1175–1199. https://doi.org/10.1016/j.jsams.2019.05.003
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A (2018) Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 68:394–424. https://doi.org/10.3322/caac.21492
Lu T, Yang X, Huang Y, Zhao M, Li M, Ma K, Yin J, Zhan C, Wang Q (2019) Trends in the incidence, treatment, and survival of patients with lung cancer in the last four decades. Cancer Manag Res 11:943–953. https://doi.org/10.2147/CMAR.S187317
Planchard D, Popat S, Kerr K et al (2018) Metastatic non-small cell lung cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol 29:iv192–iv237. https://doi.org/10.1093/annonc/mdy275
Morgensztern D, Ng SH, Gao F, Govindan R (2010) Trends in stage distribution for patients with non-small cell lung cancer: a National Cancer Database survey. J Thorac Oncol 5:29–33. https://doi.org/10.1097/JTO.0b013e3181c5920c
Herbst RS, Morgensztern D, Boshoff C (2018) The biology and management of non-small cell lung cancer. Nature 553:446–454. https://doi.org/10.1038/nature25183
Temel JS, Greer JA, Muzikansky A, Gallagher ER, Admane S, Jackson VA, Dahlin CM, Blinderman CD, Jacobsen J, Pirl WF, Billings JA, Lynch TJ (2010) Early palliative care for patients with metastatic non–small-cell lung cancer. N Engl J Med 363:733–742. https://doi.org/10.1056/NEJMoa1000678
Postmus PE, Kerr KM, Oudkerk M et al (2017) Early and locally advanced non-small-cell lung cancer (NSCLC): ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol 28:iv1–iv21. https://doi.org/10.1093/annonc/mdx222
Schulte T, Schniewind B, Dohrmann P, Küchler T, Kurdow R (2009) The extent of lung parenchyma resection significantly impacts long-term quality of life in patients with non-small cell lung cancer. Chest 135:322–329. https://doi.org/10.1378/chest.08-1114
Rosero ID, Ramírez-Vélez R, Lucia A, Martínez-Velilla N, Santos-Lozano A, Valenzuela PL, Morilla I, Izquierdo M (2019) Systematic review and meta-analysis of randomized, controlled trials on preoperative physical exercise interventions in patients with non-small-cell lung cancer. Cancers (Basel) 11:944. https://doi.org/10.3390/cancers11070944
Moher D, Liberati A, Tetzlaff J, Altman DG (2009) Preferred Reporting Items for Systematic Reviews and Meta-Analyses: the PRISMA statement. J Clin Epidemiol 62:1006–1012. https://doi.org/10.1016/j.jclinepi.2009.06.005
Booth A, Clarke M, Ghersi D, Moher D, Petticrew M, Stewart L (2011) An international registry of systematic-review protocols. Lancet 377:108–109. https://doi.org/10.1016/S0140-6736(10)60903-8
Blobaum P (2006) Physiotherapy Evidence Database (PEDro). J Med Libr Assoc 94:477–478
Maher CG, Sherrington C, Herbert RD, Moseley AM, Elkins M (2003) Reliability of the PEDro scale for rating quality of randomized controlled trials. Phys Ther 83:713–721
De Morton NA (2009) The PEDro scale is a valid measure of the methodological quality of clinical trials : a demographic study. Aust J Physiother 55:129–133. https://doi.org/10.1016/s0004-9514(09)70043-1
Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA (editors). Cochrane handbook for systematic reviews of interventions version 6.0 (updated July 2019). Session 10-10-1. Cochrane, 2019. Available at www.training.cochrane.org/handbook/current.Available
Lai Y, Huang J, Yang M, Su J, Liu J, Che G (2017) Seven-day intensive preoperative rehabilitation for elderly patients with lung cancer: a randomized controlled trial. J Surg Res 209:30–36. https://doi.org/10.1016/j.jss.2016.09.033
Lai Y, Su J, Qiu P, Wang M, Zhou K, Tang Y, Che G (2017) Systematic short-term pulmonary rehabilitation before lung cancer lobectomy: a randomized trial. Interact Cardiovasc Thorac Surg 25:476–483. https://doi.org/10.1093/icvts/ivx141
Chen H-M, Tsai C-M, Wu Y-C, Lin KC, Lin CC (2015) Randomised controlled trial on the effectiveness of home-based walking exercise on anxiety, depression and cancer-related symptoms in patients with lung cancer. Br J Cancer 112:438–445. https://doi.org/10.1038/bjc.2014.612
Edvardsen E, Skjønsberg OH, Holme I et al (2014) High-intensity training following lung cancer surgery: a randomised controlled trial. Thorax 1–7. https://doi.org/10.1136/thoraxjnl-2014-205944
Morano MTAP, Mesquita R, Da Silva GPF et al (2014) Comparison of the effects of pulmonary rehabilitation with chest physical therapy on the levels of fibrinogen and albumin in patients with lung cancer awaiting lung resection: a randomized clinical trial. BMC Pulm Med 14:121. https://doi.org/10.1186/1471-2466-14-121
Quist M, Sommer MS, Vibe-Petersen J, Stærkind MB, Langer SW, Larsen KR, Trier K, Christensen M, Clementsen PF, Missel M, Henriksen C, Christensen KB, Lillelund C, Langberg H, Pedersen JH (2018) Early initiated postoperative rehabilitation reduces fatigue in patients with operable lung cancer: a randomized trial. Lung Cancer 126:125–132. https://doi.org/10.1016/j.lungcan.2018.10.025
Sebio García R, Yáñez-Brage MI, Giménez Moolhuyzen E, Salorio Riobo M, Lista Paz A, Borro Mate JM (2017) Preoperative exercise training prevents functional decline after lung resection surgery: a randomized, single-blind controlled trial. Clin Rehabil 31:1057–1067. https://doi.org/10.1177/0269215516684179
Zhang LL, Wang SZ, Chen HL, Yuan AZ (2016) Tai Chi exercise for cancer-related fatigue in patients with lung cancer undergoing chemotherapy: a randomized controlled trial. J Pain Symptom Manag 51:504–511. https://doi.org/10.1016/j.jpainsymman.2015.11.020
Brocki BC, Andreasen J, Nielsen LR, Nekrasas V, Gorst-Rasmussen A, Westerdahl E (2014) Short and long-term effects of supervised versus unsupervised exercise training on health-related quality of life and functional outcomes following lung cancer surgery – a randomized controlled trial. Lung Cancer 83:102–108. https://doi.org/10.1016/j.lungcan.2013.10.015
Hwang CL, Yu CJ, Shih JY, Yang PC, Wu YT (2012) Effects of exercise training on exercise capacity in patients with non-small cell lung cancer receiving targeted therapy. Support Care Cancer 20:3169–3177. https://doi.org/10.1007/s00520-012-1452-5
Jastrzębski D, Maksymiak M, Kostorz S et al (2015) Pulmonary rehabilitation in advanced lung cancer patients during chemotherapy. In: Advances in experimental medicine and biology. pp 57–64
Arbane G, Tropman D, Jackson D, Garrod R (2011) Evaluation of an early exercise intervention after thoracotomy for non-small cell lung cancer (NSCLC), effects on quality of life, muscle strength and exercise tolerance: randomised controlled trial. Lung Cancer 71:229–234. https://doi.org/10.1016/j.lungcan.2010.04.025
Stigt JA, Uil SM, van Riesen SJH, Simons FJNA, Denekamp M, Shahin GM, Groen HJM (2013) A randomized controlled trial of postthoracotomy pulmonary rehabilitation in patients with resectable lung cancer. J Thorac Oncol 8:214–221. https://doi.org/10.1097/JTO.0b013e318279d52a
Arbane G, Douiri A, Hart N, Hopkinson NS, Singh S, Speed C, Valladares B, Garrod R (2014) Effect of postoperative physical training on activity after curative surgery for non-small cell lung cancer: a multicentre randomised controlled trial. Physiother (United Kingdom) 100:100–107. https://doi.org/10.1016/j.physio.2013.12.002
Henke CC, Cabri J, Fricke L, Pankow W, Kandilakis G, Feyer PC, de Wit M (2014) Strength and endurance training in the treatment of lung cancer patients in stages IIIA/IIIB/IV. Support Care Cancer 22:95–101. https://doi.org/10.1007/s00520-013-1925-1
Chen H-M, Tsai C-M, Wu Y-C, Lin KC, Lin CC (2016) Effect of walking on circadian rhythms and sleep quality of patients with lung cancer: a randomised controlled trial. Br J Cancer 115:1304–1312. https://doi.org/10.1038/bjc.2016.356
Dhillon HM, Bell ML, van der Ploeg HP, Turner JD, Kabourakis M, Spencer L, Lewis C, Hui R, Blinman P, Clarke SJ, Boyer MJ, Vardy JL (2017) Impact of physical activity on fatigue and quality of life in people with advanced lung cancer: a randomized controlled trial. Ann Oncol 28:1889–1897. https://doi.org/10.1093/annonc/mdx205
Edvardsen E, Skjonsberg OH, Holme I, Nordsletten L, Borchsenius F, Anderssen SA (2015) High-intensity training following lung cancer surgery: a randomised controlled trial. Thorax 70:244–250. https://doi.org/10.1136/thoraxjnl-2014-205944
Oken MM, Creech RH, Tormey DC, Horton J, Davis TE, McFadden ET, Carbone PP (1982) Toxicity and response criteria of the Eastern Cooperative Oncology Group. Am J Clin Oncol 5:649–656. https://doi.org/10.1097/00000421-198212000-00014
Fletcher GF, Ades PA, Kligfield P, Arena R, Balady GJ, Bittner VA, Coke LA, Fleg JL, Forman DE, Gerber TC, Gulati M, Madan K, Rhodes J, Thompson PD, Williams MA, American Heart Association Exercise, Cardiac Rehabilitation, and Prevention Committee of the Council on Clinical Cardiology, Council on Nutrition, Physical Activity and Metabolism, Council on Cardiovascular and Stroke Nursing, and Council on Epidemiology and Prevention (2013) Exercise standards for testing and training: a scientific statement from the American Heart Association. Circulation 128:873–934. https://doi.org/10.1161/CIR.0b013e31829b5b44
Cheville AL, Rhudy L, Basford JR, Griffin JM, Flores AM (2017) How receptive are patients with late stage cancer to rehabilitation services and what are the sources of their resistance? Arch Phys Med Rehabil 98:203–210. https://doi.org/10.1016/j.apmr.2016.08.459
Suetta C, Magnusson SP, Beyer N, Kjaer M (2007) Effect of strength training on muscle function in elderly hospitalized patients. Scand J Med Sci Sports 17:464–472. https://doi.org/10.1111/j.1600-0838.2007.00712.x
Buchheit M, Laursen PB (2013) High-intensity interval training, solutions to the programming puzzle. Sport Med 43:313–338. https://doi.org/10.1007/s40279-013-0029-x
Papadopoulos E, Santa Mina D (2018) Can we HIIT cancer if we attack inflammation? Cancer Causes Control 29:7–11. https://doi.org/10.1007/s10552-017-0983-y
Stamatis G, Leschber G, Schwarz B, Brintrup DL, Ose C, Weinreich G, Passlick B, Hecker E, Kugler C, Dienemann H, Krbek T, Eggeling S, Hatz R, Müller MR, Weder W, Aigner C, Jöckel KH (2019) Perioperative course and quality of life in a prospective randomized multicenter phase III trial, comparing standard lobectomy versus anatomical segmentectomy in patients with non-small cell lung cancer up to 2 cm, stage IA (7th edition of TNM staging system). Lung Cancer 138:19–26. https://doi.org/10.1016/j.lungcan.2019.09.021
Brown JC, Cespedes Feliciano EM, Caan BJ (2018) The evolution of body composition in oncology-epidemiology, clinical trials, and the future of patient care: facts and numbers. J Cachexia Sarcopenia Muscle 9:1200–1208. https://doi.org/10.1002/jcsm.12379
Hardee JP, Counts BR, Carson JA (2019) Understanding the role of exercise in cancer cachexia therapy. Am J Lifestyle Med 13:46–60. https://doi.org/10.1177/1559827617725283
Radbruch L, Strasser F, Elsner F, Gonçalves JF, Løge J, Kaasa S, Nauck F, Stone P, the Research Steering Committee of the European Association for Palliative Care (EAPC) (2008) Fatigue in palliative care patients — an EAPC approach. Palliat Med 22:13–32. https://doi.org/10.1177/0269216307085183
Lorenz D, Morrison S (2015) Current concepts in periodization of strength and conditioning for the sports physical therapist. Int J Sports Phys Ther 10:734–747
Fairman CM, Zourdos MC, Helms ER, Focht BC (2017) A scientific rationale to improve resistance training prescription in exercise oncology. Sport Med 47:1457–1465. https://doi.org/10.1007/s40279-017-0673-7
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Codima, A., das Neves Silva, W., de Souza Borges, A.P. et al. Exercise prescription for symptoms and quality of life improvements in lung cancer patients: a systematic review. Support Care Cancer 29, 445–457 (2021). https://doi.org/10.1007/s00520-020-05499-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-020-05499-6