Abstract
Background
The rapid development of COVID-19 vaccines in the wake of the COVID-19 pandemic has led to an equally expediently deployed vaccination campaign with more than 12 billion vaccinations administered worldwide. Reports of vaccine-associated adverse reactions (VAARs) have ranged from headaches and pain at the injection site to potentially life-threatening events such as cerebral venous sinus thrombosis. The heart has also not been spared of VAARs, as vaccine-associated myocardial infarction and more commonly, albeit still rare, myocarditis and perimyocarditis have been reported in predominantly young male recipients.
Methodological innovations
Cardiac magnetic resonance imaging findings of vaccine-associated myocarditis such as prolonged T1 and T2 relaxation times, increased T2 signal intensity ratio, and subepicardial late gadolinium enhancement have been demonstrated to be similar to those in virus-induced myocarditis, enabling the use of the modified 2018 Lake Louise Criteria for diagnostic purposes to confirm vaccination-associated myocardial inflammation. Other reported cardiac findings such as cardiomyopathies and arrhythmias were confined to case reports. The incidence of myocardial infarction was not noted to be higher than in the overall population.
Conclusion
The overall preliminary prognosis of vaccine- associated myocarditis seems to be good as suggested by initial reports, but long-term follow-up is needed to sufficiently assess possible sequelae and consequences.
Zusammenfassung
Hintergrund
Die rasche Entwicklung von COVID-19-Impfstoffen im Rahmen der COVID-19-Pandemie hat zu einer zügigen Impfkampagne geführt, im Rahmen derer mehr als 12 Mrd. Impfungen weltweit durchgeführt wurden. Die Berichte über Impfnebenwirkungen („vaccine-associated adverse reactions“, VAAR) reichen dabei von Kopfschmerzen und Schmerzen an der Injektionsstelle bis hin zu potenziell lebensbedrohlichen Ereignissen wie zerebrale Venen- und Sinusthrombosen. Auch kardiale Impfnebenwirkungen wurden beschrieben. Solche kardialen VAAR scheinen überwiegend junge Männer zu betreffen. Obwohl diese kardialen Impfnebenwirkungen sehr selten sind, gibt es einige Berichte über Myokarditiden und Perimyokarditiden nach Impfung.
Methodische Innovationen
Die Magnetresonanztomographie(MRT)-Befunde der impfassoziierten Myokarditis, wie verlängerte T1- und T2-Relaxationszeiten, fokale T2-Signalerhöhungen und ein subepikardiales Late-Gadolinium-Enhancement ähneln nachweislich denen der virusinduzierten Myokarditis, sodass die modifizierten Lake-Louise-Kriterien 2018 für diagnostische Zwecke zum Nachweis einer impfassoziierten myokardialen Inflammation verwendet werden können. Sonstige kardiale Befunde wie Kardiomyopathien und Arrhythmien beschränken sich aktuell auf Fallberichte. Berichte über Myokardinfarkte nach Impfung sind ebenfalls sehr selten. Die Inzidenz von Myokardinfarkten ist nicht höher als in der Gesamtbevölkerung.
Schlussfolgerung
Die vorläufige Gesamtprognose der impfstoffassoziierten Myokarditis scheint den ersten Berichten zufolge gut zu sein, doch sind langfristige Nachuntersuchungen erforderlich, um mögliche Folgeerkrankungen und Konsequenzen ausreichend bewerten zu können.
Similar content being viewed by others
Introduction
As of August 2022, there have been approximately 591 million confirmed cases of coronavirus disease 2019 (COVID-19) and 6.4 million confirmed deaths worldwide, according to the World Health Organization [1]. The severe acute respiratory syndrome coronavirus 2 (SARS-CoV‑2) was initially described as an infection of the lower airways resulting in atypical pneumonia, but it has since been recognized as a multiorgan disease, with the potential to affect the skin, the brain, and the heart [2]. The development of COVID-19 vaccines cumulated in a total of 12.4 billion doses administered worldwide [1]. This rapidly deployed vaccination campaign has helped to contain the spread of SARS-CoV 2 as well as to prevent many unwanted effects of COVID-19, with studies estimating the overall efficacy of all available vaccines at over 70%, and even over 94% for mRNA-based vaccines [3]. In the 1990s, a database called “Vaccine Adverse Event Reporting System” (VAERS) was set up by the Centers for Disease Control and Prevention (CDC) and the U.S. Food and Drug Administration (FDA) to document possible side effects after the administration of U.S. licensed vaccines. This has been a vital tool in the current pandemic and has allowed healthcare providers to independently report all vaccine-associated adverse reactions (VAARs). While there is no doubt about the benefits of COVID-19 vaccines, a number of reports have emerged detailing VAARs, which usually range from headaches, pain at the injection site, or chills to potentially life-threatening events such as sinus venous thrombosis or myocarditis [3,4,5,6]. Cardiovascular VAARs tend to manifest mainly as myocarditis, pericarditis, or both (perimyocarditis) in predominantly young males. Arrhythmias have also been frequently described. To date, reports of myocardial infarction have been confined to case reports [7]. As the COVID-19 pandemic is currently still ongoing, only long-term follow-up studies will be able to show the true extent of the effects of the pandemic.
Imaging-based assessment of cardiac vaccine-associated adverse events
Myocarditis or pericarditis
By far the most commonly reported, yet still rare, cardiovascular VAAR after COVID-19 vaccination is an acute myocarditis or pericarditis, which has an estimated incidence of 0.48 cases per 100,000 vaccinations [8]. After the widespread adoption of COVID-19 vaccines, reports of myocarditis in predominantly young males usually after the second-dose vaccination started to emerge [5, 9,10,11]. The VEARS noted 94 cases of myocarditis for the Ad26.COV2‑S [recombinant] (Janssen) vaccine, 980 for the mRNA-1273 (Moderna) vaccine, and 1897 cases for the BNT162b2 (Pfizer/BioNTech) vaccine [12]. Acute-onset myocarditis after vaccination is not a new phenomenon and has been previously described for influenza and smallpox vaccines [13]. The main clinical findings are usually dyspnea or chest pain but can also include arrhythmias [9]. Elevated troponin T and other cardiac enzymes have been observed in most cases of myocarditis [5, 8]. Although the definitive pathomechanism is not fully understood, hyperimmunity has been proposed to play a key role: Parts of the vaccines, for example, the mRNA itself or the viral spike protein might be seen as antigens by the body, resulting in an inflammatory cascade inside cardiomyocytes [14, 15].
While endomyocardial biopsy remains the reference standard for diagnosing myocarditis, it has been largely superseded due to its invasive nature by cardiac magnetic resonance imaging (MRI), especially in uncomplicated cases. The modified 2018 Lake Louise criteria have been validated to be a reliable diagnostic tool for the diagnosis of acute myocarditis on cardiac MRI. Utilizing T1-based imaging (prolonged native T1 relaxation times, increased extracellular volume, or positive late gadolinium enhancement [LGE]) and T2-based imaging (prolonged T2 relaxation times or regional or global increased T2 signal intensity ratio), cardiac MRI has the ability to visualize inflammatory cardiac changes [16,17,18]. Recent studies have shown that cardiac MRI changes in vaccine-associated myocarditis are similar to those of viral-induced myocarditis, thus enabling the application of the modified Lake Louise criteria to vaccine-associated myocarditis, as demonstrated in Fig. 1 [5, 17, 18]. Typical cardiac MRI findings include subepicardial LGE of the lateral wall, which tends to correlate with the degree of troponin T elevation. Other common findings are prolonged T1 and T2 relaxation times as well as increased focal or global T2 signal intensity ratios. Some researchers have noted that septal and midmyocardial segments were less commonly involved on LGE imaging in vaccine-associated myocarditis compared to acute viral induced myocarditis [19, 20], as well as a higher overall left ventricular ejection fraction was observed. Isolated vaccine-associated pericarditis has been previously described, but so far there are few imaging-based publications on this topic as most tend to report myocarditis and pericarditis as one event [21]. Inflammation of the pericardium is sometimes observed accompanying acute myocarditis resulting in perimyocarditis.
Cardiac magnetic resonance imaging (MRI) of a 27-year-old male patient with acute vaccine-associated myocarditis 4 days after receiving the second dose of the mRNA-1273 (Moderna) vaccine. Elevated high-sensitive troponin T was noted during the laboratory work-up (579 ng/nL, laboratory reference: < 12 ng/nL). a T2 short tau inversion recovery (STIR) sequence in short-axis view demonstrating elevated subepicardial T2 signal, in keeping with focal edema (arrows). b A corresponding prolonged T2 relaxation time (global T2: 60 ms; site specific cut-off value: ≥ 55.9 ms) is noted on the short-axis T2 parametric map (arrows). c Axial fat-suppressed T2-weighted imaging demonstrates axillary lymph node swelling in the ipsilateral side of the injection arm up to 1.5 cm in short-axis diameter (dashed circle). d Short-axis late gadolinium enhancement (LGE) imaging reveals a corresponding subepicardial contrast enhancement (arrows). e T1 parametric map shows prolonged focal subepicardial T1 relaxation times (global T1: 1050 ms; site specific cut-off value: ≥ 1000 ms; arrows). f Axial LGE imaging showing subepicardial contrast enhancement along the basal and midmyocardial lateral wall
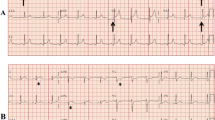
Clinical symptoms of acute vaccine-associated myocarditis or pericarditis as well as cardiac MRI findings tend to be self-limiting and resolve within a few weeks of onset [11]. There is currently a sparsity of literature concerning the natural history of vaccine-associated myocarditis. New research suggests vaccine-associated myocarditis demonstrates rapid improvement of cardiac MRI findings within 3 months of onset, although focal fibrotic changes were still appreciable on follow-up [22]. Figure 2 shows the natural history of a 25-year-old male patient with acute myocarditis at initial cardiac MRI and the resolution of active inflammation at the 7‑month follow-up.
Magnetic resonance imaging (MRI) demonstrating the natural history of acute vaccine-associated myocarditis in a young 25-year-old male patient after receiving the second dose of the BNT162b2 (Pfizer/BioNTech) vaccine at baseline (MRI was performed 4 days after vaccination) and at the 7‑month follow-up. T2 short tau inversion recovery (STIR) imaging demonstrates increased signal intensity at the midmyocardial, subepicardial lateral wall (a, d thick arrows) corresponding to focal edema with associated contrast enhancement in the late gadolinium enhancement (LGE) imaging (thin arrows) in short-axis (b, e) and four-chamber views (c, f). Note the resolution of myocardial edema from baseline to follow-up indicating a resolution of active myocardial inflammation. A decrease of LGE without complete resolution is also seen on follow-up, most likely reflection persistent myocardial scarring after myocardial remodeling and scar shrinkage
Although these preliminary findings are promising, only long-term follow-up examinations will be able to show the true extent of myocardial injury and long-lasting clinical effects. Currently there are at least 96 registered studies, including some large multicenter studies, on the clinicaltrials.gov website pertaining to the effects of the COVID-19 vaccines on myocytes [23]. A selection of currently published literature is highlighted in Table 1.
Myocardial infarction
Even less common than vaccine-associated myocarditis is vaccine-associated myocardial infarction, with no conclusive data available to date. A few case reports have emerged describing myocardial infarcts after COVID-19 vaccination but other than a temporal relationship between symptom onset and vaccination, no clear causation could be attributed [7, 24, 25]. Thrombotic events are known to be precipitated by SARS-CoV2 infections and a similar pathomechanism might be at play for vaccine-associated myocardial infarction [26]. Alternative pathomechanisms such as vasospasms or atherosclerotic plaque rupture have also been proposed [25]. Systematic studies are required to further elucidate whether there is indeed a causal relationship between myocardial infarction and COVID-19 vaccination. Coronary computed tomography–angiography or coronary angiography should be performed for patients presenting with chest pain with elevated cardiac troponin levels and abnormal electrocardiograms so as to directly demonstrate the potentially underlying filling defect. Vaccines have been shown to reduce the risk of acute myocardial infarction after COVID-19, outweighing the potential risks of vaccine-associated acute coronary syndrome [27].
Summary and outlook
Physicians should be aware of the potential risk factors that current COVID-19 vaccines introduce. While rare (estimated incidence of 0.48 per 100,000 vaccinations), vaccine-associated myocarditis should be suspected in young patients with a recent history of COVID-19 vaccination and symptom onset, especially if presenting with electrocardiogram abnormalities and/or elevated cardiac troponin T levels. Cardiac MRI findings are typically similar to those found in viral-induced acute infarct-like myocarditis including subepicardial LGE, edema, and prolonged T1 and T2 relaxation times. Symptom resolution tends to be within weeks, with preliminary findings suggesting no relevant sequelae. However, vaccine-associated myocardial infarction should also be suspected and ruled out if typical symptoms of myocardial infarction such as acute chest pain and dyspnea present shortly after vaccination. As the COVID-19 pandemic is ongoing, we are still learning a great deal about the virus, the disease it causes, and potential VAARs. Only long-term follow-ups can reveal the true extent of the long-term effects of COVID-19 vaccines.
The importance of reporting VAARs of COVID-19 vaccinations should not be underestimated as it is vital for raising awareness among physicians of the potential risk factors that vaccines entail for their patients. This ensures that patients get the proper timely treatment they need. But this does not diminish the benefits COVID-19 vaccines have afforded us. Currently, vaccines are the most effective tool at our disposal to mitigate the COVID-19 pandemic and people should not be discouraged to undergo vaccination by rare possible adverse reactions.
Practical conclusion
Vaccine-induced myocarditis is rarely observed after COVID-19 vaccination but should be considered in patients with an acute symptom onset after vaccination, especially after mRNA vaccination.
Cardiac magnetic resonance imaging findings of vaccine-induced perimyocarditis have been reported to be similar to virus-induced myocarditis, allowing for the use of the Lake Louise criteria for diagnostic assessment of patients with suspected vaccine-induced perimyocarditis.
The occurrence of other cardiac side effects such as cardiomyopathies or myocardial infarctions is currently confined to case reports.
References
WHO Coronavirus (COVID-19) Dashboard (2022) WHO Coronavirus (COVID-19) dashboard with vaccination data. https://covid19.who.int/. Accessed 22 Aug 2022
Thakur V, Ratho RK, Kumar P, Bhatia SK, Bora I, Mohi GK et al (2021) Multi-organ involvement in COVID-19: Beyond pulmonary manifestations. JCM 10(3):446
Cai C, Peng Y, Shen E, Huang Q, Chen Y, Liu P et al (2021) A comprehensive analysis of the efficacy and safety of COVID-19 vaccines. Mol Ther 29(9):2794–2805
Schulz JB, Berlit P, Diener H‑C, Gerloff C, Greinacher A, Klein C et al (2021) COVID-19 vaccine-associated cerebral venous thrombosis in Germany. Ann Neurol 90(4):627–639
Kravchenko D, Isaak A, Mesropyan N, Endler C, Bischoff L, Vollbrecht T et al (2022) Cardiac MRI in Suspected Acute Myocarditis After COVID-19 mRNA Vaccination. Rofo 194(09):1003–1011. https://doi.org/10.1055/a-1752-0951
Sharifian-Dorche M, Bahmanyar M, Sharifian-Dorche A, Mohammadi P, Nomovi M, Mowla A (2021) Vaccine-induced immune thrombotic thrombocytopenia and cerebral venous sinus thrombosis post COVID-19 vaccination; a systematic review. J Neurol Sci 428:117607
Sung JG, Sobieszczyk PS, Bhatt DL (2021) Acute myocardial infarction within 24 hours after COVID-19 vaccination. Am J Cardiol 156:129–131
Witberg G, Barda N, Hoss S, Richter I, Wiessman M, Aviv Y et al (2021) Myocarditis after Covid-19 vaccination in a large health care organization. N Engl J Med 385(23):2132–2139
Bozkurt B, Kamat I, Hotez PJ (2021) Myocarditis with COVID-19 mRNA vaccines. Circulation 144(6):471–484
Isaak A, Feisst A, Luetkens JA (2021) Myocarditis following COVID-19 vaccination. Radiology 301(1):E378–E379
Kim HW, Jenista ER, Wendell DC, Azevedo CF, Campbell MJ, Darty SN et al (2021) Patients with acute myocarditis following mRNA COVID-19 vaccination. JAMA Cardiol 6(10):1196–1201
United States Department of Health and Human Services (DHHS), Public Health Service (PHS), Centers for Disease Control (CDC), Food and Drug Administration (FDA) Vaccine Adverse Event Reporting System (VAERS) 1990–07/22/2022, CDC WONDER on-line database. http://wonder.cdc.gov/vaers.html. Accessed 2 Aug 2022
Kuntz J, Crane B, Weinmann S, Naleway AL (2018) Myocarditis and pericarditis are rare following live viral vaccinations in adults. Vaccine 36(12):1524–1527
Heymans S, Cooper LT (2022) Myocarditis after COVID-19 mRNA vaccination: clinical observations and potential mechanisms. Nat Rev Cardiol 19(2):75–77
Segal Y, Shoenfeld Y (2018) Vaccine-induced autoimmunity: the role of molecular mimicry and immune crossreaction. Cell Mol Immunol 15(6):586–594
Luetkens JA, Faron A, Isaak A, Dabir D, Kuetting D, Feisst A et al (2019) Comparison of original and 2018 Lake Louise criteria for diagnosis of acute myocarditis: results of a validation cohort. Radiol Cardiothorac Imaging 1(3):e190010
Ferreira VM, Schulz-Menger J, Holmvang G, Kramer CM, Carbone I, Sechtem U et al (2018) Cardiovascular magnetic resonance in nonischemic myocardial inflammation: expert recommendations. J Am Coll Cardiol 72(24):3158–3176
Lurz P, Luecke C, Eitel I, Föhrenbach F, Frank C, Grothoff M et al (2016) Comprehensive cardiac magnetic resonance imaging in patients with suspected myocarditis: the myoracer-trial. J Am Coll Cardiol 67(15):1800–1811
Fronza M, Thavendiranathan P, Chan V, Karur GR, Udell JA, Wald RM et al (2022) Myocardial injury pattern at MRI in COVID-19 vaccine-associated myocarditis. Radiology. https://doi.org/10.1148/radiol.212559
Patel YR, Shah NR, Lombardi K, Agarwal S, Has P, Patel R et al (2022) Cardiac MRI findings in male patients with acute myocarditis in the presence or absence of COVID-19 vaccination. Radiol Cardiothorac Imaging 4(3):e220008
Wong H‑L, Hu M, Zhou CK, Lloyd PC, Amend KL, Beachler DC et al (2022) Risk of myocarditis and pericarditis after the COVID-19 mRNA vaccination in the USA: a cohort study in claims databases. Lancet 399(10342):2191–2199
Alhussein MM, Rabbani M, Sarak B, Dykstra S, Labib D, Flewitt J et al (2022) Natural history of myocardial injury following COVID-19 vaccine associated myocarditis. Can J Cardiol. https://doi.org/10.1016/j.cjca.2022.07.017
ClinicalTrials.gov Incidence, patient characteristics and outcome of myocarditis after COVID-19 mRNA vaccine. https://clinicaltrials.gov/ct2/show/NCT05438472?term=COVID-19+AND+myocarditis&draw=2&rank=1. Accessed 1 Aug 2022
Iqbal S, Adnan G, Farhad A, Ahmed I, Rahman MN (2022) Acute myocardial infarction after Coronavirus vaccine: a rare adverse effect. Cureus 14(1):e21544
Tajstra M, Jaroszewicz J, Gąsior M (2021) Acute coronary tree thrombosis after vaccination for COVID-19. JACC Cardiovasc Interv 14(9):e103–e104
McFadyen JD, Stevens H, Peter K (2020) The emerging threat of (micro)thrombosis in COVID-19 and its therapeutic implications. Circ Res 127(4):571–587
Kim Y‑E, Huh K, Park Y‑J, Peck KR, Jung J (2022) Association between vaccination and acute myocardial infarction and ischemic stroke after COVID-19 infection. JAMA 328(9):887
Ahmed SK (2022) Myocarditis after BNT162b2 and mRNA-1273 COVID-19 vaccination: A report of 7 cases. Ann Med Surg 77:103657
Abellan C, Vivekanantham H, Mahmoudi A, Cook S, Doll S, Arroyo D (2021) A case series of acute myocarditis associated with SARS-CoV‑2 mRNA vaccination. Cardiovasc Med. 24:w10103. https://doi.org/10.4414/cvm.2021.w10103
Diaz GA, Parsons GT, Gering SK, Meier AR, Hutchinson IV, Robicsek A (2021) Myocarditis and pericarditis after vaccination for COVID-19. JAMA 326(12):1210–1212
Larson KF, Ammirati E, Adler ED, Cooper LT, Hong KN, Saponara G et al (2021) Myocarditis after BNT162b2 and mRNA-1273 vaccination. Circulation 144(6):506–508
Marshall M, Ferguson ID, Lewis P, Jaggi P, Gagliardo C, Collins JS et al (2021) Symptomatic acute myocarditis in 7 adolescents after Pfizer-bioNtech COVID-19 vaccination. Pediatrics. https://doi.org/10.1542/peds.2021-052478
Montgomery J, Ryan M, Engler R, Hoffman D, McClenathan B, Collins L et al (2021) Myocarditis following immunization with mRNA COVID-19 vaccines in members of the US military. JAMA Cardiol 6(10):1202–1206
Abu Mouch S, Roguin A, Hellou E, Ishai A, Shoshan U, Mahamid L et al (2021) Myocarditis following COVID-19 mRNA vaccination. Vaccine 39(29):3790–3793
Rosner CM, Genovese L, Tehrani BN, Atkins M, Bakhshi H, Chaudhri S et al (2021) Myocarditis temporally associated with COVID-19 vaccination. Circulation 144(6):502–505
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
D. Kravchenko declares that he has no competing interests. J.A. Luetkens received payments from Philips Healthcare for lectures and from Bayer HealthCare for activities related to the scientific advisory board.
For this article no studies with human participants or animals were performed by any of the authors. All studies mentioned were in accordance with the ethical standards indicated in each case.
The supplement containing this article is not sponsored by industry.
Additional information

Scan QR code & read article online
Rights and permissions
About this article
Cite this article
Kravchenko, D., Luetkens, J.A. Cardiac adverse reactions of COVID-19 vaccination: cardiac MRI findings. Radiologie 62 (Suppl 1), 22–27 (2022). https://doi.org/10.1007/s00117-022-01090-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00117-022-01090-8