Background
Middle East respiratory syndrome (MERS) is a respiratory disease caused by MERS-CoV. It was first reported in 2012 in Saudi Arabia and is thus far linked to countries in or near the Arabian Peninsula. Laboratory-confirmed MERS has now been identified in Bahrain, Iran, Jordan, Kuwait, Lebanon, Oman, Qatar, Saudi Arabia, United Arab Emirates (UAE), and Yemen.
A large MERS outbreak occurred in the Republic of South Korea linked to a traveler from the Arabian Peninsula in 2015. Travel-associated cases have been identified in Algeria, Austria, China, Egypt, France, Germany, Greece, Italy, Malaysia, Netherlands, Philippines, Republic of Korea, Thailand, Tunisia, Turkey, United Kingdom (UK), and United States (US). Only two cases have been reported in the United States, both in men who had recently returned from Saudi Arabia. Only two of over 800 cases screened have tested positive for MERS-CoV since 2012. [1, 2]
MERS is considered an international threat to public health. CDC has published guidance for health departments and healthcare infection-control programs for investigating potential cases of MERS and preventing its spread. Tools and guidance for recognizing and reporting ill travelers have been issued to US flight crews, Emergency Medical Service (EMS) units at airports, and US Customs and Border Protection (CBP) officers. CDC maintains ongoing close partnerships in the international public health community to monitor risk and to inform US preventive measures. [2]
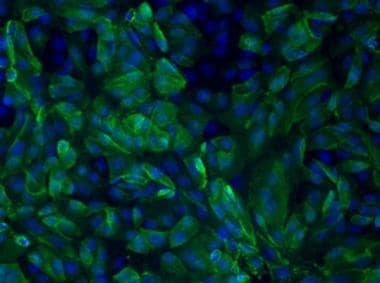 Vero cells infected with Middle East respiratory syndrome coronavirus (MERS-CoV). Image courtesy of the Centers for Disease Control and Prevention (Jennifer L. Harcourt).
Vero cells infected with Middle East respiratory syndrome coronavirus (MERS-CoV). Image courtesy of the Centers for Disease Control and Prevention (Jennifer L. Harcourt).
See 11 Travel Diseases to Consider Before and After the Trip, a Critical Images slideshow, to help identify and manage several infectious travel diseases.
Also, see the Ebola: Care, Recommendations, and Protecting Practitioners slideshow to review treatment, recommendations, and safeguards for healthcare personnel working with infectious diseases, as well as the Acute Respiratory Distress Syndrome: A Complex Clinical Condition slideshow for more information on ARDS, a condition characterized by acute respiratory failure, hypoxemia, and pulmonary edema.
Most individuals with confirmed MERS have developed acute respiratory illness. Illness may be complicated by pneumonitis and multiorgan failure. More than 800 MERS-CoV–associated deaths have occurred since September 2012. [3] MERS-CoV has been shown to spread from person to person via close contact but without sustained community transmission. Transmission has occurred via close contact with infected persons, including from patients to healthcare personnel. Potentially at-risk individuals include caregivers and close contacts of people with suspected or confirmed MERS-CoV infection. [4]
Laboratory testing for MERS-CoV is not routinely available, although polymerase chain reaction (PCR) for MERS-CoV is available via state health departments, CDC, and some international laboratories. Some commercial tests are available, but none has received approval from the US Food and Drug Administration (FDA). [2]
No vaccine exists for MERS, and no specific treatment has been recommended. Management is supportive. [5] At least one group has recommended consideration of interferon alfa 2b plus ribavirin in the management of MERS-CoV cases because of the combination’s efficacy seen in rhesus macaques with MERS. [6]
Standard contact and airborne precautions are recommended for management of hospitalized patients with known or suspected MERS-CoV infection. The complete CDC guidance can be found on the CDC website (Interim Infection Prevention and Control Recommendations for Hospitalized Patients with Middle East Respiratory Syndrome Coronavirus (MERS-CoV).
Etiology
Coronaviruses are the largest of all RNA viruses, with positive-sense single-stranded RNA genomes of 26-32 kb. They are classified into 4 phylogenetic subgroups: alphacoronavirus, betacoronavirus, gammacoronavirus, and deltacoronavirus. [7] SARS-CoV belongs to the lineage B betacoronavirus and was responsible for the 2002-2003 severe acute respiratory syndrome (SARS) outbreaks, which first highlighted the potentially high pathogenicity of human coronaviruses.
MERS-CoV is a betacoronavirus of lineage C that was first reported in Saudi Arabia in 2012. The exact origin of this novel coronavirus is still unknown. MERS-CoV is closely related to two coronaviruses of the same lineage found in bats, which may indeed be its wild reservoir. [8] However, it is also found in dromedary (single-humped) camels, and domesticated herds have been a principal link to zoonotic infection in humans. [9, 10, 11, 12]
The specific transmission mechanisms between humans and the possible source animals are unknown, [5] and, although human-to-human transmission has been demonstrated, the chain of transmission is not self-sustaining, making early identification and isolation a feasible strategy to limit the spread of the virus. The virus tends not to spread beyond one individual to others. [13]
Pathophysiology
One of the most important cells of the innate immune system is the macrophage. Its function is to eliminate pathogens, to present antigens to T cells, to produce cytokines and chemokines to maintain homeostasis, and to modulate the immune response in tissues. [14]
Compared with severe acute respiratory syndrome coronavirus (SARS-Cov), MERS-CoV can establish infection in monocyte-derived macrophages (MDMs) and macrophages. The virus induces release of proinflammatory cytokines, leading to severe inflammation and tissue damage, which may manifest clinically as severe pneumonia and respiratory failure. [15] Vascular endothelial cells located in the pulmonary interstitium also may be infected by MERS-CoV, and, because MERS-CoV receptor DPP4 is expressed in different human cells and tissues, dissemination of the infection may occur. [15] This may explain the increased severity and higher fatality rate compared with SARS-CoV infection.
Interestingly, lymphopenia has been noted in most patients infected with MERS-CoV, as was noted in SARS infections. This is due to cytokine-induced immune cell sequestration and release and induction of monocyte chemotactic protein-1 (MCP-1) and interferon-gamma-inducible protein-10 (IP-10), which suppresses proliferation of human myeloid progenitor cells. [16]
Epidemiology
Since 2012, 2,374 laboratory-confirmed cases of infection with MERS-CoV have been reported to the World Health Organization (WHO), including at least 823 related deaths. [3]
Twenty-seven countries have reported MERS cases. On the Arabian Peninsula, countries include Bahrain, Iran, Jordan, Kuwait, Lebanon, Oman, Qatar, Saudi Arabia, United Arab Emirates (UAE), and Yemen. Other countries reporting travel-associated MERS include Algeria, Austria, China, Egypt, France, Germany, Greece, Italy, Malaysia, Netherlands, Philippines, Republic of Korea, Thailand, Tunisia, Turkey, United Kingdom (UK), and the United States. The vast majority of these cases have so far occurred in the Kingdom of Saudi Arabia. [17]
The largest MERS outbreak outside of Saudi Arabia occurred in 2015 in the Republic of Korea. The outbreak involved 186 confirmed cases and caused 36 deaths. The outbreak sparked quarantine of more than 5,000 individuals and the closure of 2,000 schools before ending. [18] The index case was a 35-year-old man exposed to a laboratory-confirmed case on May 27 while visiting Bahrain. He visited four hospitals before being admitted and testing positive for MERS-CoV on June 7. He recovered and was discharged on October 1 after confirmation of two negative test results. [3, 19] Most of the subsequent cases were related to healthcare-associated exposures of those caring for infected patients, and most deaths occurred in those already hospitalized, with a case fatality rate of only 10%. No cases were found to be community-acquired. South Korean officials enacted an aggressive campaign of isolating contacts in the community and hospitals for 14 days after exposure, which likely contained the outbreak to nosocomial settings. [20]
The first case of MERS in the United States was reported to the CDC by the Indiana State Department of Health on May 1, 2014, and confirmed by the CDC on May 2. The patient was a male who lived and worked in Saudi Arabia as a healthcare provider in a facility that had patients infected with MERS. He became ill around April 18, traveled by commercial airline from Saudi Arabia to Chicago, and then traveled by bus to Indiana. His initial symptoms included low-grade fever, myalgias, and rhinorrhea that later progressed to dyspnea and nonproductive cough. Chest radiography and CT scanning revealed bilateral infiltrates. The patient recovered uneventfully, and no secondary cases were reported. [1]
The second imported case was reported to the CDC by the Florida Department of Health on May 11, 2014. The patient was a healthcare worker who resided and worked in Saudi Arabia and had contact with a patient infected with MERS-CoV prior to presentation. He traveled by commercial airlines from Saudi Arabia to the United Kingdom, the United Kingdom to Boston, Boston to Atlanta, and finally from Atlanta to Orlando, where he was visiting family. His initial symptoms included myalgias, chills, and fever without cough. Because of persistent symptoms, he sought medical attention, and, soon after admission, he developed cough. Thoracic CT scans showed patchy nodular infiltrates bilaterally without mediastinal lymphadenopathy. Two healthcare workers developed a respiratory illness within the incubation period after they were exposed to the patient, but PCR testing of both showed negative results. The rest of the healthcare workers who were potentially in contact with the patient were furloughed, and none tested positive for MERS-CoV. [2, 1]
The virus is not readily transmissible between humans, requiring close contact for prolonged periods with an acutely ill individual. Close contact is defined by prolonged presence within 6 feet (2 meters) of the infected individual, such as during household contact or provision of health care.
In experiments controlling for temperature and relative humidity, tissue infectious quantities of MERS-CoV have been found to survive on surfaces for up to 48 hours under conditions that might approximate most air-conditioned indoor environments; higher temperatures and humidity reduced viability. Aerosolized virus remained most viable at lower relative humidities. These data and the frequent association of hospital visitation or healthcare-associated contact with infection suggest a significant role for inhalation and fomites. Association of infection with household contact appears low. [21, 22] Cough or sneezing and performance of aerosol-generating procedures such as intubation or bronchoscopy without respiratory droplet precautions increases the risk for exposure to infectious respiratory secretions. Extrapolating from other coronaviruses and experience during epidemics, transmission requires direct inhalation of respiratory droplets or contact with mucosa of respiratory secretions. The latter may be indirect, by contact with contaminated surfaces or fomites. [23, 24]
Specific mechanisms for transmission from animals are unclear but appear to involve contact with dromedary camels or their urine, as well as consumption of their undercooked meat or unpasteurized dairy products. [10, 23] Experimental studies have demonstrated that MERS-CoV inoculated into dromedary, cow, and goat milk remains stable and viable for up to 72 hours. [25] While MERS-CoV antibodies have been found in dromedary camels in the Middle East, the virus has not been detected in camel milk, nor have camels outside of the Arabian Peninsula been found to have antibodies to MERS–CoV. In one case of a man who died of MERS in Saudi Arabia, his camel herd was serially tested for MERS–CoV. Of samples, including nasal secretions, urine, milk, blood, and rectal swabs, the virus was detected only in nasal swabs for a transient period. [26] An outbreak investigation linked dromedary camels from a farm in Qatar to two human cases of infection in October 2013. MERS-CoV was virologically confirmed in nose swabs from 3 camels by 3 independent RT-PCR and sequencing assays. [27]
Prognosis
Many individuals with confirmed MERS have developed severe acute respiratory illness, and some have developed multiorgan dysfunction. The case fatality rate is approximately 30-40% and may depend on the underlying health of the individual. Hospital-acquired infection has accounted for the highest number of deaths. Associated comorbidities, including end-stage renal disease on hemodialysis, diabetes, and chronic cardiopulmonary disease, have been associated with increased mortality rates. Delayed diagnosis and supportive care may also play a role. In the second largest outbreak in Korea, most cases involved limited transmission to presumably healthy healthcare workers, and none in the general community. The overall mortality rate was only 10%. [2, 19, 20]
Patient Education
Thus far, the global experience with MERS-CoV substantiates a very low risk to the general population. The US population is not considered to be at risk in the absence of close contact with individuals infected with MERS-CoV or travel to countries where the infection is actively occurring.
CDC issues travel notices when MERS is reported, with enhanced precautions for travelers who plan to work in healthcare settings in involved countries and in or near the Arabian Peninsula. [4] Travelers to an affected region who develop fever, cough, shortness of breath, or myalgias during their trip or within 14 days after returning to the United States are strongly encouraged to seek medical attention. [4]
The CDC advises that people observe the following tips to help prevent respiratory illnesses:
-
Wash hands often with soap and water for 20 seconds; if water and soap are not available, use an alcohol-based hand sanitizer.
-
Practice respiratory etiquette. Cover nose and mouth with a tissue or the inner elbow when coughing or sneezing.
-
Avoid touching eyes, nose, and mouth with unwashed hands.
-
Avoid close contact with sick individuals, such as kissing, sharing cups, or sharing eating utensils.
-
Clean and disinfect frequently touched surfaces, such as toys and doorknobs.
-
Vero cells infected with Middle East respiratory syndrome coronavirus (MERS-CoV). Image courtesy of the Centers for Disease Control and Prevention (Jennifer L. Harcourt).
-
MERS-CoV virion on electron microscopy, illustrating ultrastructural detail. Image courtesy of the Centers for Disease Control and produced by the National Institute of Allergy and Infectious Diseases (NIAID), 2014.





