Therapeutic Anticoagulation with Heparin in Noncritically Ill Patients with Covid-19
Abstract
Background
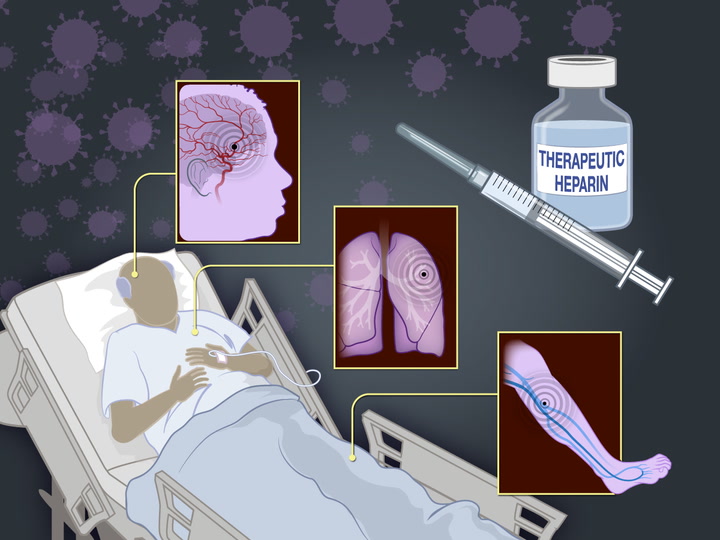
Thrombosis and inflammation may contribute to the risk of death and complications among patients with coronavirus disease 2019 (Covid-19). We hypothesized that therapeutic-dose anticoagulation may improve outcomes in noncritically ill patients who are hospitalized with Covid-19.
Methods
In this open-label, adaptive, multiplatform, controlled trial, we randomly assigned patients who were hospitalized with Covid-19 and who were not critically ill (which was defined as an absence of critical care–level organ support at enrollment) to receive pragmatically defined regimens of either therapeutic-dose anticoagulation with heparin or usual-care pharmacologic thromboprophylaxis. The primary outcome was organ support–free days, evaluated on an ordinal scale that combined in-hospital death (assigned a value of −1) and the number of days free of cardiovascular or respiratory organ support up to day 21 among patients who survived to hospital discharge. This outcome was evaluated with the use of a Bayesian statistical model for all patients and according to the baseline d-dimer level.

Results
The trial was stopped when prespecified criteria for the superiority of therapeutic-dose anticoagulation were met. Among 2219 patients in the final analysis, the probability that therapeutic-dose anticoagulation increased organ support–free days as compared with usual-care thromboprophylaxis was 98.6% (adjusted odds ratio, 1.27; 95% credible interval, 1.03 to 1.58). The adjusted absolute between-group difference in survival until hospital discharge without organ support favoring therapeutic-dose anticoagulation was 4.0 percentage points (95% credible interval, 0.5 to 7.2). The final probability of the superiority of therapeutic-dose anticoagulation over usual-care thromboprophylaxis was 97.3% in the high d-dimer cohort, 92.9% in the low d-dimer cohort, and 97.3% in the unknown d-dimer cohort. Major bleeding occurred in 1.9% of the patients receiving therapeutic-dose anticoagulation and in 0.9% of those receiving thromboprophylaxis.
Conclusions
In noncritically ill patients with Covid-19, an initial strategy of therapeutic-dose anticoagulation with heparin increased the probability of survival to hospital discharge with reduced use of cardiovascular or respiratory organ support as compared with usual-care thromboprophylaxis. (ATTACC, ACTIV-4a, and REMAP-CAP ClinicalTrials.gov numbers, NCT04372589, NCT04505774, NCT04359277, and NCT02735707.)
In some patients, the clinical course of coronavirus disease 2019 (Covid-19) is characterized by an initial period of mild-to-moderate symptoms, followed by progressive respiratory failure leading to cardiovascular or respiratory organ support or death.1,2 However, the majority of patients who are hospitalized with Covid-19 are moderately ill and do not initially require organ support in an intensive care unit (ICU).3-5 Limited therapies are available to prevent progression to organ failure and death among moderately ill patients.
Patients who are hospitalized with Covid-19 frequently have macrovascular and microvascular thrombosis and inflammation, which are associated with a poor clinical outcome.6,7 Given the antithrombotic, antiinflammatory, and possibly antiviral properties of heparins,8-10 it has been hypothesized that anticoagulation with heparin administered at doses higher than conventionally used for venous thromboprophylaxis may improve outcomes.11 Furthermore, an elevated d-dimer level has been associated with vascular thrombosis and a poor clinical outcome.6,12 Thus, some practitioners have advocated an evaluation of d-dimer levels to guide anticoagulant administration. In the absence of data from randomized trials, clinical-guideline recommendations13 and practice14 vary widely.
We conducted an international, adaptive, multiplatform, randomized, controlled trial to determine whether an initial strategy of therapeutic-dose anticoagulation with unfractionated or low-molecular-weight heparin improves in-hospital survival and reduces the duration of ICU-level cardiovascular or respiratory organ support among hospitalized patients with Covid-19 who are not critically ill.
Methods
Trial Design and Oversight
To accelerate evidence generation, we integrated three platforms evaluating therapeutic-dose anticoagulation with heparin in patients hospitalized with Covid-19 into a single multiplatform, randomized, controlled trial. The participating platforms were Antithrombotic Therapy to Ameliorate Complications of Covid-19 (ATTACC),15 A Multicenter, Adaptive, Randomized Controlled Platform Trial of the Safety and Efficacy of Antithrombotic Strategies in Hospitalized Adults with COVID-19 (ACTIV-4a), and Randomized, Embedded, Multifactorial Adaptive Platform Trial for Community-Acquired Pneumonia (REMAP-CAP).16 During the trial period, patients with moderate Covid-19 disease were enrolled at 121 sites in 9 countries (the United States, Canada, the United Kingdom, Brazil, Mexico, Nepal, Australia, the Netherlands, and Spain). We prospectively aligned eligibility criteria, interventions, outcome measures, and data collection. (Comparisons of the three platforms are provided in the Supplementary Appendix, available with the full text of this article at NEJM.org.) Independent data and safety monitoring boards oversaw the platforms on the basis of a collaborative cross-platform interaction plan. The trial protocols and unified statistical analysis plan are also available at NEJM.org.
The trial was approved by the relevant ethics committees and conducted in accordance with the Good Clinical Practice guidelines of the International Council for Harmonisation. All the patients or their surrogates provided written or oral informed consent, in accordance with regional regulations. The trial was supported by multiple international funding organizations, which had no role in the design, analysis, or reporting of trial results, apart from the ACTIV-4a protocol, which received input on design from professional staff members at the National Institutes of Health and from peer reviewers. The members of the writing committees vouch for the accuracy and completeness of the data and for the fidelity of the trials to the protocols.
Patients
The multiplatform trial enrolled patients who were hospitalized with Covid-19. The investigators hypothesized that the benefits and risks of therapeutic-dose anticoagulation would vary according to disease severity. As such, the design prospectively stratified patients according to whether they had severe disease (ICU-level care or critically ill) or moderate disease (hospitalized but noncritically ill) at enrollment. This report describes the results of the analyses involving patients with moderate Covid-19; the results of analyses involving patients with severe Covid-19 are reported separately.17
Moderate disease severity was defined as hospitalization for Covid-19 without the need for ICU-level care. ICU-level care was defined as the use of respiratory or cardiovascular organ support (oxygen delivered by high-flow nasal cannula, noninvasive or invasive mechanical ventilation, or the use of vasopressors or inotropes) in an ICU. In ACTIV-4a, in which investigators found that ICU-level care was challenging to define during the pandemic, receipt of organ support, regardless of hospital setting, was used to define ICU-level care. Patients who were admitted to an ICU but without receiving qualifying organ support were considered to be moderately ill.
Patients with moderate disease were further stratified according to their baseline d-dimer level as follows: a high d-dimer level (≥2 times the upper limit of the normal range [ULN], according to local laboratory criteria), a low d-dimer level (<2 times the ULN), and an unknown d-dimer level. Patients were ineligible for enrollment in the ATTACC and ACTIV-4a platforms if 72 hours had elapsed since hospital admission for Covid-19 or since in-hospital confirmation of the presence of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2); in the REMAP-CAP platform, patients were ineligible if 14 days had elapsed since admission. Patients were also excluded if hospital discharge was expected within 72 hours or if they had a clinical indication for therapeutic anticoagulation, a high risk of bleeding, receipt of dual antiplatelet therapy, or a known heparin allergy, including heparin-induced thrombocytopenia (HIT). (Details regarding eligibility are provided in the Supplementary Appendix.)
Randomization
We used central Internet-based systems to randomly assign patients to receive either therapeutic-dose anticoagulation with unfractionated or low-molecular-weight heparin or usual-care pharmacologic thromboprophylaxis in an open-label fashion. Therapeutic-dose anticoagulation was administered according to local protocols for the treatment of acute venous thromboembolism for up to 14 days or until recovery; the latter was defined as hospital discharge or a discontinuation of supplemental oxygen for at least 24 hours. Thromboprophylaxis was provided at a dose and duration determined by the treating clinician according to local practice. The anticoagulation and thromboprophylaxis regimens are detailed in the Supplementary Appendix.
Treatments were initially randomly assigned in a 1:1 ratio. The ATTACC and REMAP-CAP designs specified the possibility of response-adaptive randomization, in which group-assignment ratios could be modified in a blinded fashion during the trial on the basis of response-adaptive interim analyses to favor the assignment of patients to the treatment group showing greater benefit. (Details regarding the methods used in adaptive randomization are provided in the Supplementary Appendix.) A subset of patients in the REMAP-CAP platform underwent randomization to other platform domains, including an antiplatelet domain.
Outcome Measures
The primary outcome was organ support–free days, evaluated on an ordinal scale that combined in-hospital death and the number of days free of cardiovascular or respiratory organ support up to day 21 among patients who survived to hospital discharge. Patients who were discharged from the hospital before day 21 were assumed to be alive and free of organ support through day 21. Any death during the index hospitalization through 90 days was assigned the worst score on the outcome scale (–1). This end point reflects both the use of ICU-level interventions and survival, with higher values indicating better outcomes.
Secondary efficacy outcomes included survival until hospital discharge, survival without receipt of organ support, survival without receipt of invasive mechanical ventilation, survival without mechanical respiratory support, length of hospital stay, a major thrombotic event or death (a composite of myocardial infarction, pulmonary embolism, ischemic stroke, systemic arterial embolism, or in-hospital death), and any thrombotic event including deep venous thrombosis. Secondary safety outcomes that were assessed during the treatment period were major bleeding (as defined according to the criteria of the International Society on Thrombosis and Haemostasis18) and laboratory-confirmed HIT. All reported bleeding and thrombotic events were adjudicated in a blinded fashion by clinical end-points committees using consensus definitions (as described in the Supplementary Appendix).
Statistical Analysis
We performed the primary analysis using a Bayesian cumulative logistic model that calculated the posterior probability distribution for the proportional odds ratio for therapeutic-dose anticoagulation as compared with usual-care thromboprophylaxis with respect to organ support–free days in patients with confirmed SARS-CoV-2 infection. Although REMAP-CAP enrolled patients with suspected or confirmed Covid-19, only patients who had infection that was confirmed by laboratory testing were included in the main analyses. The primary model incorporated weakly informative Dirichlet prior distributions for the number of days without organ support and was adjusted for age, sex, trial site, d-dimer cohort, and enrollment period (in 2-week intervals). The model was fitted with the use of a Markov chain Monte Carlo algorithm with 100,000 samples from the joint posterior distribution, which allowed for calculation of the posterior distributions for the proportional odds ratios, including medians and 95% credible intervals, and the posterior probabilities of superiority and futility for the comparison between therapeutic-dose anticoagulation and usual-care thromboprophylaxis.
The primary model estimated treatment effects for each of the groups according to disease severity (severe or moderate, with the latter stratified according to the baseline d-dimer level) by means of a Bayesian hierarchical method. The treatment effects of anticoagulation for the groups were nested in a hierarchical prior distribution centered on an overall intervention effect estimated with a neutral prior distribution, but distinct group-specific effects were estimated. With regard to the primary outcome of organ support–free days, when consistent effects were observed for the groups, the posterior distribution for each intervention group effect was shrunk toward the overall estimate (dynamic borrowing).19 Secondary end points were modeled without dynamic borrowing. The stopping criteria for treatment superiority (>99% probability of an odds ratio of >1.0) and futility (<5% probability of an odds ratio of >1.2) were evaluated monthly by an independent statistical analysis committee and could be reached separately in the low and high d-dimer subgroups at each adaptive analysis; no stopping criteria were defined for the cohort with an unknown d-dimer level. Several sensitivity analyses of the primary model are also reported. (Details regarding the sensitivity analyses are provided in the Supplementary Appendix.) In addition, we present analyses involving patients with moderate disease that assume a single treatment effect regardless of the d-dimer level.
Subgroup analyses assessed the treatment effect according to age, sex, baseline respiratory support, and dose of thromboprophylactic drugs. Protocol adherence was defined according to the anticoagulant dose equivalent administered within the first 24 to 48 hours after randomization. The receipt of doses that were categorized as therapeutic or subtherapeutic heparin qualified as adherence in the therapeutic-dose anticoagulation group, and the receipt of low-dose or intermediate-dose thromboprophylactic drugs qualified as adherence in the usual-care thromboprophylaxis group.
Results
Characteristics of the Patients
The first patients underwent randomization on April 21, 2020. On January 22, 2021, enrollment was discontinued on the advice of the data and safety monitoring boards after a planned adaptive analysis of data from 1398 patients showed that the prespecified stopping criteria for superiority of therapeutic-dose anticoagulation had been reached in both the high and low d-dimer cohorts (Table S1 in the Supplementary Appendix). By that time, 2244 patients with moderate disease had undergone randomization. The primary analysis population consisted of 2219 patients (Figure 1). Parallel enrollment of patients with severe Covid-19 ran through December 19, 2020, as reported separately.17
Figure 1

Screening, Enrollment, and Randomization, According to Trial Group.
Trial sites used varying screening and documentation practices during the coronavirus disease 2019 (Covid-19) pandemic to identify eligible patients, as described in the protocol. Of the 13,373 patients who underwent screening, 7202 were assessed for eligibility in the ATTACC platform, 3799 in the ACTIV-4a platform, and 2372 in the REMAP-CAP platform. Under reasons for exclusion from the trial, “other” includes not meeting an inclusion criterion (including a lack of diagnosis of Covid-19), an anticipated duration of hospital stay of less than 72 hours, or meeting an exclusion criterion that is not specified here. Data for patients who had severe disease at baseline could be used for covariate adjustment and dynamic borrowing calculations in the primary analysis. The numbers of patients who were randomly assigned to the treatment groups were imbalanced owing to the use of response-adaptive randomization.
Baseline characteristics were similar in the two treatment groups (Table 1), including within each d-dimer cohort (Table S2). Patients in the high and unknown d-dimer cohorts were generally older and had a higher prevalence of coexisting illnesses than those in low d-dimer cohort. Concomitant baseline therapies included antiplatelet agents (in 12% of the patients), glucocorticoids (in 62%), and remdesivir (in 36%).
Table 1

| Characteristic | Therapeutic-Dose Anticoagulation (N=1181) |
Usual-Care Thromboprophylaxis (N=1050) |
|---|---|---|
| Age ±SD — yr | 59.0±14.1 | 58.8±13.9 |
| Male sex — no. (%) | 713 (60.4) | 597 (56.9) |
| Race or ethnic group — no./total no. (%)† | ||
| White | 622/994 (62.6) | 564/845 (66.7) |
| Asian | 41/994 (4.1) | 43/845 (5.1) |
| Black | 219/994 (22.0) | 162/845 (19.2) |
| First Nations or American Indian | 118/965 (12.2) | 82/819 (10.0) |
| Other | 17/1109 (1.5) | 16/968 (1.7) |
| Hispanic or Latino | 574/1004 (57.2) | 537/879 (61.1) |
| Median body-mass index (IQR)‡ | 29.8 (26.3–34.7) | 30.3 (26.7–34.9) |
| Preexisting condition — no./total no. (%) | ||
| Hypertension | 546/1023 (53.4) | 447/892 (50.1) |
| Diabetes mellitus | 352/1181 (29.8) | 311/1049 (29.6) |
| Severe cardiovascular disease§ | 123/1165 (10.6) | 121/1038 (11.7) |
| Chronic kidney disease | 83/1173 (7.1) | 69/1037 (6.7) |
| Chronic respiratory disease¶ | 249/1132 (22.0) | 212/988 (21.5) |
| Immunosuppressive disease | 105/1143 (9.2) | 103/1005 (10.2) |
| Treatment — no./total no. (%) | ||
| Antiplatelet agent‖ | 148/1140 (13.0) | 111/1013 (11.0) |
| Remdesivir | 428/1178 (36.3) | 383/1048 (36.5) |
| Glucocorticoid | 479/791 (60.6) | 415/656 (63.3) |
| Tocilizumab | 6/1178 (0.5) | 7/1048 (0.7) |
| Respiratory support — no. (%) | ||
| None | 156 (13.2) | 123 (11.7) |
| Low-flow nasal cannula or face mask | 789 (66.8) | 696 (66.3) |
| High-flow nasal cannula | 25 (2.1) | 28 (2.7) |
| Noninvasive mechanical ventilation | 21 (1.8) | 24 (2.3) |
| Unspecified** | 190 (16.1) | 179 (17.0) |
| Median laboratory value (IQR) | ||
| Median d-dimer level relative to ULN at trial site | 1.6 (0.9–2.6) | 1.5 (1.0–2.7) |
| Platelets — per mm3 | 221,000 (171,000–290,000) | 218,000 (172,500–289,000) |
| Lymphocytes — per mm3 | 900 (700–1300) | 1000 (700–1400) |
| Creatinine — mg/dl | 0.9 (0.7–1.1) | 0.9 (0.7–1.1) |
| Platform of enrollment — no. (%)†† | ||
| ATTACC‡‡ | 650 (55.0) | 509 (48.5) |
| ACTIV-4a | 387 (32.8) | 392 (37.3) |
| REMAP-CAP | 144 (12.2) | 149 (14.2) |
| Country of enrollment — no./total no. (%) | ||
| United Kingdom | 95/1181 (8.0) | 103/1050 (9.8) |
| United States | 573/1181 (48.5) | 507/1050 (48.3) |
| Canada | 102/1181 (8.6) | 83/1050 (7.9) |
| Brazil | 234/1181 (19.8) | 209/1050 (19.9) |
| Other§§ | 177/1181 (15.0) | 148/1050 (14.1) |
Demographic and Clinical Characteristics of the Patients at Baseline.*
*
Listed are data that were included in the analysis involving patients with moderate severity of coronavirus disease 2019 (Covid-19). The denominators of patients in the anticoagulation group and the thrombophylaxis group are unequal owing to response-adaptive randomization. The baseline characteristics of the patients according to d-dimer level are provided in Table S2 in the Supplementary Appendix. To convert the values for creatinine to micromoles per liter, multiply by 88.4. ULN denotes upper limit of the normal range.
†
Race or ethnic group was reported by the patients.
‡
The body-mass index is the weight in kilograms divided by the square of the height in meters.
§
Severe cardiovascular disease was defined as a baseline history of heart failure, myocardial infarction, coronary artery disease, peripheral arterial disease, or cerebrovascular disease (stroke or transient ischemic attack) in the ATTACC (Antithrombotic Therapy to Ameliorate Complications of Covid-19) and ACTIV-4a (A Multicenter, Adaptive, Randomized Controlled Platform Trial of the Safety and Efficacy of Antithrombotic Strategies in Hospitalized Adults with COVID-19) platforms and as a baseline history of New York Heart Association class IV symptoms in the REMAP-CAP platform (Randomized, Embedded, Multifactorial Adaptive Platform Trial for Community-Acquired Pneumonia).
¶
Chronic respiratory disease was defined as a baseline history of asthma, chronic obstructive pulmonary disease, bronchiectasis, interstitial lung disease, primary lung cancer, pulmonary hypertension, active tuberculosis, or the receipt of home oxygen therapy.
‖
Not listed are 74 patients who were coenrolled in the REMAP-CAP Antiplatelet Domain (39 in the anticoagulation group and 35 in the thromboprophylaxis group).
**
In REMAP-CAP, levels of oxygen support (including no support) below the level of high-flow nasal cannula were not reported.
††
The relative proportion of patients who were randomly assigned in each platform was imbalanced owing to implementation of response-adaptive randomization in ATTACC on December 15, 2020.
‡‡
A total of 215 patients who were enrolled in the ATTACC platform were funded by the ACTIV4a platform by the National Heart, Lung, and Blood Institute.
§§
Other participating countries were Mexico, Nepal, Australia, the Netherlands, and Spain.
Initial adherence to the protocol-assigned anticoagulation dose after randomization was 88.3% in the therapeutic-dose anticoagulation group and 98.3% in the thromboprophylaxis group (Table S3). Of the 1093 patients in the therapeutic-dose anticoagulation group with available data, 1035 (94.7%) received a low-molecular-weight heparin, most commonly enoxaparin. Among the 855 patients in the thromboprophylaxis group with available data, 613 (71.7%) received a low dose of a thromboprophylactic drug and 227 (26.5%) received an intermediate dose.
Primary Outcome
Among 2219 participants with moderate disease, the posterior probability that therapeutic-dose anticoagulation increased organ support–free days as compared with usual-care thromboprophylaxis was 98.6% (median adjusted odds ratio, 1.27; 95% credible interval, 1.03 to 1.58) (Table 2). Of the 1048 patients in the usual-care thromboprophylaxis group, 801 (76.4%) survived until hospital discharge without receipt of organ support during the first 21 days, as compared with 939 of 1171 patients (80.2%) in the therapeutic-dose anticoagulation group. The median adjusted absolute difference in this value was 4.0 percentage points (95% credible interval, 0.5 to 7.2), favoring the anticoagulation group. Because the majority of patients in the two treatment groups survived until hospital discharge without receipt of ICU-level organ support, the median value for organ support–free days was 22 in both groups (Figure 2 and Fig. S1). Accordingly, the proportion of patients in each treatment group who survived until hospital discharge without receipt of organ support (22 on the ordinal scale) is reported.
Figure 2

Days without Organ Support among All the Patients with Moderate Disease.
Panel A shows the distribution of organ support–free days among all the patients with moderate disease. The ordinal scale includes a score of –1 (in-hospital death, the worst possible outcome), a score of 0 to 21 (the numbers of days alive without organ support), and a score of 22 (survival until hospital discharge without receipt of organ support, the best possible outcome). The difference in the height of the two curves at any point represents the difference in the cumulative probability of having a value for days without organ support of less than or equal to that point on the x axis. Panel B shows the number of days without organ support as horizontally stacked proportions of patients in the two treatment groups, with the following possible outcomes: in-hospital death with or without the receipt of organ support (dark red, the worst possible outcome, corresponding to a score of −1 on the ordinal scale); survival with organ support provided in an intensive care unit (ICU) (red-to-blue gradient shading based on the number of days alive without organ support; intermediate outcome, corresponding to a score of 0 to 21 on the ordinal scale); and survival until hospital discharge without ICU-level organ support (dark blue, the best possible outcome, corresponding to a score of 22 on the ordinal scale).
Table 2

| Variable | Therapeutic-Dose Anticoagulation | Usual-Care Thrombo-prophylaxis | Adjusted Difference in Risk (95% Credible Interval)† |
Adjusted Odds Ratio (95% Credible Interval)‡ |
Probability of Superiority of Therapeutic-Dose Anticoagulation |
|---|---|---|---|---|---|
| no. of patients/total no. (%) | percentage points | % | |||
| Patients with moderate disease | |||||
| Overall group§ | 939/1171 (80.2) | 801/1048 (76.4) | 4.0 (0.5 to 7.2) |
1.27 (1.03–1.58) |
98.6 |
| d-dimer cohort¶ | |||||
| High level | 264/339 (77.9) | 210/291 (72.2) | 5.1 (0.0 to 9.9) |
1.31 (1.00–1.76) |
97.3 |
| Low level | 463/570 (81.2) | 403/505 (79.8) | 3.0 (−1.2 to 6.3) |
1.22 (0.93–1.57) |
92.9 |
| Unknown level | 212/262 (80.9) | 188/252 (74.6) | 4.9 (0.00 to 9.9) |
1.32 (1.00–1.86) |
97.3 |
Primary Outcome of Organ Support–Free Days.*
*
The primary outcome was organ support–free days, evaluated on an ordinal scale that combined in-hospital death and the number of days free of cardiovascular or respiratory organ support up to day 21 among patients who survived to hospital discharge. Because the majority of patients in the two treatment groups survived until hospital discharge without receipt of critical care–level organ support, the median value for organ support–free days was 22 in both groups. Accordingly, the proportion of patients in each treatment group who survived until hospital discharge without receipt of organ support (22 on the ordinal scale) is reported.
†
The adjusted difference in risk is based on the event frequency in the usual-care thromboprophylaxis group and the odds ratio after adjustment for age, sex, site, d-dimer group, and enrollment period.
‡
The odds ratio is for the therapeutic-dose anticoagulation group as compared with the usual-care thromboprophylaxis group. The odds ratios are adjusted for age, sex, trial site, d-dimer cohort, and enrollment period, which may be imbalanced due to the use of response-adaptive randomization.
§
This model assumes a single treatment effect in all the patients with moderate disease regardless of the baseline d-dimer level. Dynamic borrowing of information on the treatment effect from patients who had severe illness at baseline was permitted, in which similar treatment effects were grouped together on the basis of their degree of similarity. Results from a sensitivity analysis assuming independent treatment effects between disease-severity cohorts are provided in Table S5 in the Supplementary Appendix.
¶
The primary adaptive model estimated treatment effects with the use of a Bayesian hierarchical approach in the following groups: patients with severe disease and those with moderate disease stratified according to their baseline high d-dimer level (≥2 times the ULN, low d-dimer level (<2 times the ULN), or unknown d-dimer level. This model permitted dynamic borrowing across illness-severity and d-dimer cohorts, in which similar treatment effects are grouped together on the basis of their degree of similarity. Accordingly, observations about treatment effect are shared between groups. Results from a sensitivity analysis assuming independent treatment effects among d-dimer–defined cohorts are also provided in Table S5.
In the primary adaptive analysis groups, the final posterior probability for superiority of therapeutic-dose anticoagulation as compared with usual-care thromboprophylaxis was 97.3% in the high d-dimer cohort, 92.9% in the low d-dimer cohort, and 97.3% in the cohort with an unknown d-dimer level (Table 2 and Fig. S1). The results were consistent in sensitivity analyses (Tables S4 and S5).
Among all the patients with moderate disease, the treatment effect did not vary meaningfully according to age, level of respiratory support at enrollment, or dose of thromboprophylactic drugs. There was a 95.2% probability that the odds ratio associated with therapeutic-dose anticoagulation was higher in men than in women (Fig. S2).
Secondary Outcomes
Secondary outcomes are shown in Table 3, Table S6, and Figure S3. In the overall cohort of patients with moderate disease, the posterior probability that therapeutic-dose anticoagulation increased survival until hospital discharge as compared with thromboprophylaxis was 87.1% (median adjusted odds ratio, 1.21; 95% credible interval, 0.87 to 1.68), for a median adjusted between-group difference of 1.3 percentage points (95% credible interval, −1.1 to 3.2). The posterior probabilities that patients in the therapeutic-dose anticoagulation group were more likely to survive without organ support or survive without invasive mechanical ventilation at 28 days were 99.1% and 92.2%, respectively.
Table 3

| Outcome | Therapeutic-Dose Anticoagulation | Usual-Care Thromboprophylaxis |
Adjusted Difference in Risk (95% Credible Interval)† |
Adjusted Odds Ratio (95% Credible Interval)‡ |
Probability of Effect of Therapeutic-Dose Anticoagulation |
|---|---|---|---|---|---|
| no. of patients/total no. (%) | percentage points | % | |||
| Survival until hospital discharge | 1085/1171 (92.7) | 962/1048 (91.8) | 1.3 (−1.1 to 3.2) |
1.21 (0.87 to 1.68)§ |
87.1¶ |
| Survival without organ support at 28 days‖ | 932/1175 (79.3) | 789/1046 (75.4) | 4.5 (0.9 to 7.7) |
1.30 (1.05 to 1.61) |
99.1¶ |
| Progression to intubation or death** | 129/1181 (10.9) | 127/1050 (12.1) | −1.9 (−4.1 to 0.7) |
0.82 (0.63 to 1.07) |
92.2¶ |
| Major thrombotic event or death | 94/1180 (8.0) | 104/1046 (9.9) | −2.6 (−4.4 to −0.2) |
0.72 (0.53 to 0.98) |
98.0¶ |
| Major thrombotic event | 13/1180 (1.1) | 22/1046 (2.1) | |||
| Death in hospital | 86/1180 (7.3) | 86/1046 (8.2) | |||
| Major bleeding | 22/1180 (1.9) | 9/1047 (0.9) | 0.7 (−0.1 to 2.3) |
1.80 (0.90 to 3.74) |
95.5†† |
Secondary Outcomes among All Patients with Moderate Disease.*
*
Secondary end points were modeled without dynamic borrowing. In these analyses, a single treatment effect was assumed regardless of the d-dimer level. Additional secondary end points, including those categorized according to the d-dimer cohort, are provided in Table S6.
†
The adjusted difference in risk is based on the event rate in the usual-care thromboprophylaxis group and the odds ratio after adjustment for age, sex, site, d-dimer cohort, and enrollment period.
‡
The odds ratio is for the therapeutic-dose anticoagulation group as compared with the usual-care thromboprophylaxis group. The odds ratios are adjusted for age, sex, trial site, d-dimer cohort, and enrollment period, which may be imbalanced due to the use of response-adaptive randomization.
§
In a model that included borrowing of information on treatment effect from patients with severe disease, the median adjusted odds ratio for survival until hospital discharge was 1.18 (95% credible interval, 0.86 to 1.63), with a posterior probability of superiority of 84.4%.
¶
In this category, the probability of superiority is shown.
‖
Survival without organ support at 28 days was modeled as a dichotomous outcome. Similar results were obtained after the exclusion of 52 patients who were receiving organ support at baseline (median adjusted odds ratio, 1.30; 95% credible interval, 1.06 to 1.62), with a posterior probability of superiority of 99.3%.
**
Progression to intubation or death was modeled as an ordinal outcome with death as the worst possible outcome.
††
For major bleeding, the probability of inferiority is shown.
A major thrombotic event or in-hospital death occurred in 94 of 1180 patients (8.0%) in the therapeutic-dose anticoagulation group and in 104 of 1046 patients (9.9%) in the thromboprophylaxis group (Table 3 and Tables S6 and S7). The analysis of the end point incorporating the occurrence of deep venous thrombosis had similar results. Major bleeding occurred in 22 of 1180 patients (1.9%) in the therapeutic-dose anticoagulation group and in 9 of 1047 (0.9%) in the usual-care thromboprophylaxis group (Table S8). Fatal bleeding occurred in 3 patients in the anticoagulation group and in 1 patient in the thromboprophylaxis group. There were no episodes of intracranial bleeding or confirmed HIT.
Discussion
In noncritically ill patients hospitalized with Covid-19, therapeutic-dose anticoagulation with heparin (most commonly, low-molecular-weight heparin) increased the probability of survival until hospital discharge with a reduced need for ICU-level organ support at 21 days as compared with usual-care thromboprophylaxis. Therapeutic-dose anticoagulation was beneficial regardless of the patient’s baseline d-dimer level. Major bleeding occurred more frequently in the anticoagulation group (1.9% vs. 0.9%). On the basis of these findings, for every 1000 hospitalized patients with moderate disease, an initial strategy of therapeutic-dose anticoagulation, as compared with usual-care thromboprophylaxis, would be anticipated to result in the survival of 40 additional patients until hospital discharge without organ support at the expense of 7 additional major bleeding events. Absolute treatment benefits were more apparent in the high d-dimer cohort than in the low d-dimer cohort. Patients in the high d-dimer cohort were generally older and had a higher prevalence of coexisting illnesses than those in the low d-dimer cohort.
Several cohort studies have shown a favorable association between anticoagulant use and survival from Covid-19.20-22 Because SARS-CoV-2 infection incites a dysregulated inflammatory response that may lead to activation of coagulation23 and potentially contribute to organ failure,24-26 heparins may reduce the use of organ support through antithrombotic, antiinflammatory, and potentially antiviral mechanisms.8–10,27
In contrast to the benefit we found in noncritically ill patients, a parallel analysis from the same multiplatform trial showed that empirical therapeutic-dose anticoagulation was not beneficial in critically ill patients (i.e., those receiving ICU-level care at enrollment).19 In a separate randomized trial involving critically ill patients with Covid-19, intermediate-dose heparin was likewise not beneficial.28 It is possible that therapeutic-dose heparin cannot influence the cascade of inflammation, thrombosis, and organ injury in patients with advanced disease.29-31 It is also possible that differences in the patient populations, aside from illness severity, may have contributed to these findings.
In our multiplatform trial, we used an adaptive Bayesian design that allowed for trial conclusions to be reached simultaneously or sequentially in groups defined according to illness severity and d-dimer level through periodic adaptive analyses. A statistical method of dynamic borrowing was incorporated to enable the investigators to reach conclusions more quickly across the d-dimer stopping cohorts in which the estimates of treatment effect were similar and to mitigate the influence of outlying treatment effects by shrinking similar treatment estimates together. Response-adaptive randomization allowed blinded randomization probabilities to be modified as evidence about treatment effects was accrued throughout the trial. Since response-adaptive randomization may lead to imbalances in baseline covariates between treatment groups over time, the primary models were necessarily adjusted for age, sex, trial site, d-dimer cohort, and enrollment period. Therefore, absolute between-group differences in risk that are based on adjusted treatment effects and the observed frequencies of control events are presented. The adjusted absolute between-group difference in outcomes that is presented is a median, so patients at higher baseline risk may derive greater absolute benefit.
The open-label design of the trial represents a potential limitation, although the primary outcome involving survival and receipt of organ support was selected to minimize bias and to function across a spectrum of illness severity. The potential for ascertainment bias cannot be excluded for the secondary outcomes of major bleeding or thrombosis. This factor, along with the absence of protocol-specified screening for venous thrombosis and the exclusion of patients at increased bleeding risk, may have contributed to a lower incidence of thrombotic events than has been reported previously.32 Although the platforms varied slightly in their classification of illness severity, the majority of patients who were receiving organ support at baseline were included in the analysis involving patients with severe disease.19 Because we did not have detailed screening data, we were not able to specify the most common reasons for exclusion from the trial, other than a high bleeding risk or a clinical indication for anticoagulation. Thus, it is not possible to fully assess the generalizability of our findings. Finally, the treatment effect was attenuated in the final analysis relative to the adaptive stopping results; nevertheless, a high probability of benefit persisted.
Among noncritically ill patients hospitalized with Covid-19, an initial strategy of therapeutic-dose anticoagulation with heparin increased the probability of survival until hospital discharge with reduced use of ICU-level organ support as compared with usual-care thromboprophylaxis.
Notes
The members of the executive writing committee are as follows: Patrick R. Lawler, M.D., M.P.H., Ewan C. Goligher, M.D., Ph.D., Jeffrey S. Berger, M.D., Matthew D. Neal, M.D., Bryan J. McVerry, M.D, Jose C. Nicolau, M.D., Ph.D., Michelle N. Gong, M.D., Marc Carrier, M.D., Robert S. Rosenson, M.D., Harmony R. Reynolds, M.D., Alexis F. Turgeon, M.D., Jorge Escobedo, M.D., David T. Huang, M.D., M.P.H., Charlotte A. Bradbury, M.B., Ch.B., Ph.D., Brett L. Houston, M.D., Lucy Z. Kornblith, M.D., Anand Kumar, M.D., Susan R. Kahn, M.D., Mary Cushman, M.D., Zoe McQuilten, Ph.D., Arthur S. Slutsky, M.D., Keri S. Kim, Pharm.D., Anthony C. Gordon, M.B., B.S., M.D., Bridget-Anne Kirwan, Ph.D., Maria M. Brooks, Ph.D., Alisa M. Higgins, Ph.D., Roger J. Lewis, M.D., Ph.D., Elizabeth Lorenzi, Ph.D., Scott M. Berry, Ph.D., Lindsay R. Berry, Ph.D., Derek C. Angus, M.D., M.P.H., Colin J. McArthur, M.B., Ch.B., Steven A. Webb, M.P.H., Ph.D., Michael E. Farkouh, M.D., Judith S. Hochman, M.D., and Ryan Zarychanski, M.D.
The members of the block writing committee are as follows: Aaron W. Aday, M.D., Farah Al-Beidh, Ph.D., Djillali Annane, M.D., Ph.D., Yaseen M. Arabi, M.D., Diptesh Aryal, M.D., Lisa Baumann Kreuziger, M.D., Abi Beane, Ph.D., Zahra Bhimani, M.P.H., Shailesh Bihari, Ph.D., Henny H. Billett, M.D., Lindsay Bond, H.B.Sc., Marc Bonten, Ph.D., Frank Brunkhorst, M.D., Meredith Buxton, Ph.D., Adrian Buzgau, B.A.S., Lana A. Castellucci, M.D., Sweta Chekuri, M.D., Jen-Ting Chen, M.D., Allen C. Cheng, Ph.D., Tamta Chkhikvadze, M.D., Benjamin Coiffard, M.D., Todd W. Costantini, M.D., Sophie de Brouwer, Ph.D., Lennie P.G. Derde, M.D., Ph.D., Michelle A. Detry, Ph.D., Abhijit Duggal, M.D., M.P.H., Vladimír Džavík, M.D., Mark B. Effron, M.D., Lise J. Estcourt, M.B., B.Chir., D.Phil., Brendan M. Everett, M.D., M.P.H., Dean A. Fergusson, Ph.D., Mark Fitzgerald, Ph.D., Robert A. Fowler, M.D., Jean P. Galanaud, M.D., Benjamin T. Galen, M.D., Sheetal Gandotra, M.D., Sebastian García-Madrona, M.D., Timothy D. Girard, M.D., Lucas C. Godoy, M.D., Andrew L. Goodman, M.D., Herman Goossens, M.D., Cameron Green, M.Sc., Yonatan Y. Greenstein, M.D., Peter L. Gross, M.D., Naomi M. Hamburg, M.D., Rashan Haniffa, Ph.D., George Hanna, M.D., Nicholas Hanna, M.D., Sheila M. Hegde, M.D., M.P.H., Carolyn M. Hendrickson, M.D., R. Duncan Hite, M.D., Alexander A. Hindenburg, M.D., Aluko A. Hope, M.D., James M. Horowitz, M.D., Christopher M. Horvat, M.D., M.H.A., Kristin Hudock, M.D., Beverley J. Hunt, M.D., Mansoor Husain, M.D., Robert C. Hyzy, M.D., Vivek N. Iyer, M.D., M.P.H., Jeffrey R. Jacobson, M.D., Devachandran Jayakumar, M.D., Norma M. Keller, M.D., Akram Khan, M.D., Yuri Kim, M.D., Ph.D., Andrei L. Kindzelski, M.D., Ph.D., Andrew J. King, Ph.D., M. Margaret Knudson, M.D., Aaron E. Kornblith, M.D., Vidya Krishnan, M.D., M.H.S., Matthew E. Kutcher, M.D., Michael A. Laffan, D.M., Francois Lamontagne, M.D., Grégoire Le Gal, M.D., Ph.D., Christine M. Leeper, M.D., Eric S. Leifer, Ph.D., George Lim, M.D., Felipe Gallego Lima, M.D., Kelsey Linstrum, M.S., Edward Litton, Ph.D., Jose Lopez-Sendon, Ph.D., Jose L. Lopez-Sendon Moreno, M.D., Sylvain A. Lother, M.D., Saurabh Malhotra, M.D., M.P.H., Miguel Marcos, Ph.D., Andréa Saud Marinez, Pharm.D., John C. Marshall, M.D., Nicole Marten, R.N., Michael A. Matthay, M.D., Daniel F. McAuley, M.D., Emily G. McDonald, M.D., Anna McGlothlin, Ph.D., Shay P. McGuinness, M.B., Ch.B., Saskia Middeldorp, M.D., Ph.D., Stephanie K. Montgomery, M.Sc., Steven C. Moore, M.D., Raquel Morillo Guerrero, Ph.D., Paul R. Mouncey, M.Sc., Srinivas Murthy, M.D., Girish B. Nair, M.D., Rahul Nair, M.D., Alistair D. Nichol, M.B., Ph.D., Brenda Nunez-Garcia, B.A., Ambarish Pandey, M.D., Pauline K. Park, M.D., Rachael L. Parke, Ph.D., Jane C. Parker, B.N., Sam Parnia, M.D., Ph.D., Jonathan D. Paul, M.D., Yessica S. Pérez González, M.D., Mauricio Pompilio, Ph.D., Matthew E. Prekker, M.D., M.P.H., John G. Quigley, M.D., Natalia S. Rost, M.D., Kathryn Rowan, Ph.D., Fernanda O. Santos, M.D., Marlene Santos, M.D., Mayler Olombrada Santos, M.Sc., Lewis Satterwhite, M.D., Christina T. Saunders, Ph.D., Roger E.G. Schutgens, M.D., Ph.D., Christopher W. Seymour, M.D., Deborah M. Siegal, M.D., Delcio G. Silva, Jr., M.Med., Manu Shankar-Hari, Ph.D., John P. Sheehan, M.D., Aneesh B. Singhal, M.D., Dayna Solvason, Simon J. Stanworth, D.Phil., Tobias Tritschler, M.D., Anne M. Turner, M.P.H., Wilma van Bentum-Puijk, M.Sc., Frank L. van de Veerdonk, M.D., Ph.D., Sean van Diepen, M.D., Gloria Vazquez-Grande, M.D., Lana Wahid, M.D., Vanessa Wareham, H.B.Sc., Bryan J. Wells, M.D., R. Jay Widmer, M.D., Ph.D., Jennifer G. Wilson, M.D., Eugene Yuriditsky, M.D., and Fernando G. Zampieri, M.D., Ph.D.
The views expressed in this article are those of the authors and do not necessarily reflect the view of the National Health Service (in the United Kingdom [U.K.]), the U.K. National Institute for Health Research, the U.K. Department of Health and Social Care, or the National Institutes of Health in the United States.
This article was published on August 4, 2021, at NEJM.org.
A data sharing statement provided by the authors is available with the full text of this article at NEJM.org.
The ATTACC platform was supported by grants from the Canadian Institutes of Health Research, LifeArc Foundation, Thistledown Foundation, Research Manitoba, Ontario Ministry of Health, Peter Munk Cardiac Centre, CancerCare Manitoba Foundation, and Victoria General Hospital Foundation. The ACTIV-4a platform was sponsored by the National Heart, Lung, and Blood Institute, National Institutes of Health (NIH) (grant numbers, OTA-20-011 and 1OT2HL156812-01). The pilot program (PROTECT) was funded in part by a grant (UL1TR001445) from the New York University Clinical and Translational Science Award program, supported by the National Center for Advancing Translational Sciences of the NIH. The REMAP-CAP platform was supported by the European Union through FP7-HEALTH-2013-INNOVATION: the Platform for European Preparedness Against (Re-)emerging Epidemics (PREPARE) consortium (602525) and the Horizon 2020 research and innovation program: the Rapid European Covid-19 Emergency Research response (RECOVER) consortium (101003589); by the Australian National Health and Medical Research Council (APP1101719 and APP1116530), the Health Research Council of New Zealand (16/631), the Canadian Institutes of Health Research (Strategy for Patient-Oriented Research Innovative Clinical Trials Program Grant [158584] and Covid-19 Rapid Research Operating Grant [447335]), the U.K. National Institute for Health Research (NIHR) and the NIHR Imperial Biomedical Research Centre, the Health Research Board of Ireland (CTN 2014-012), the Learning While Doing Program at the University of Pittsburgh Medical Center, the Breast Cancer Research Foundation, the French Ministry of Health (PHRC-20-0147), the Minderoo Foundation, Amgen, Eisai, the Global Coalition for Adaptive Research, and the Wellcome Trust Innovations Project (215522). Dr. Goligher is the recipient of an Early Career Investigator award from the Canadian Institutes of Health Research (grant AR7-162822). Dr. Gordon is supported by an NIHR Research Professorship (RP-2015-06-18), Dr. Shankar-Hari by an NIHR Clinician Scientist Fellowship (CS-2016-16-011), and Dr. Turgeon by a Canada Research Chair (Tier 2). Dr. Zarychanski is the recipient of the Lyonel G. Israels Research Chair in Hematology (University of Manitoba).
Disclosure forms provided by the authors are available with the full text of this article at NEJM.org.
We thank the patients and their families who participated in this trial and the members of the data and safety monitoring board for each platform.
Supplementary Material
Research Summary (nejmoa2105911_research-summary.pdf)
- Download
- 722.42 KB
Protocol (nejmoa2105911_protocol.pdf)
- Download
- 7.49 MB
Supplementary Appendix (nejmoa2105911_appendix.pdf)
- Download
- 1.75 MB
Disclosure Forms (nejmoa2105911_disclosures.pdf)
- Download
- 2.17 MB
Data Sharing Statement (nejmoa2105911_data-sharing.pdf)
- Download
- 70.44 KB
References
1.
Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet 2020;395:1054-1062.
2.
Mody A, Lyons PG, Vazquez Guillamet C, et al. The clinical course of coronavirus disease 2019 in a US hospital system: a multistate analysis. Am J Epidemiol 2021;190:539-552.
3.
Richardson S, Hirsch JS, Narasimhan M, et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City area. JAMA 2020;323:2052-2059.
4.
Lewnard JA, Liu VX, Jackson ML, et al. Incidence, clinical outcomes, and transmission dynamics of severe coronavirus disease 2019 in California and Washington: prospective cohort study. BMJ 2020;369:m1923-m1923.
5.
Garibaldi BT, Fiksel J, Muschelli J, et al. Patient trajectories among persons hospitalized for COVID-19: a cohort study. Ann Intern Med 2021;174:33-41.
6.
Bilaloglu S, Aphinyanaphongs Y, Jones S, Iturrate E, Hochman J, Berger JS. Thrombosis in hospitalized patients with COVID-19 in a New York City health system. JAMA 2020;324:799-801.
7.
Godoy LC, Goligher EC, Lawler PR, Slutsky AS, Zarychanski R. Anticipating and managing coagulopathy and thrombotic manifestations of severe COVID-19. CMAJ 2020;192(40):E1156-E1161.
8.
Clausen TM, Sandoval DR, Spliid CB, et al. SARS-CoV-2 infection depends on cellular heparan sulfate and ACE2. Cell 2020;183(4):1043.e15-1057.e15.
9.
Buijsers B, Yanginlar C, Maciej-Hulme ML, de Mast Q, van der Vlag J. Beneficial non-anticoagulant mechanisms underlying heparin treatment of COVID-19 patients. EBioMedicine 2020;59:102969-102969.
10.
Mycroft-West CJ, Su D, Pagani I, et al. Heparin inhibits cellular invasion by SARS-CoV-2: structural dependence of the interaction of the spike S1 receptor-binding domain with heparin. Thromb Haemost 2020;120:1700-1715.
11.
Chowdhury JF, Moores LK, Connors JM. Anticoagulation in hospitalized patients with Covid-19. N Engl J Med 2020;383:1675-1678.
12.
Short SAP, Gupta S, Brenner SK, et al. d-Dimer and death in critically ill patients with coronavirus disease 2019. Crit Care Med 2021;49(5):e500-e511.
13.
Flaczyk A, Rosovsky RP, Reed CT, Bankhead-Kendall BK, Bittner EA, Chang MG. Comparison of published guidelines for management of coagulopathy and thrombosis in critically ill patients with COVID 19: implications for clinical practice and future investigations. Crit Care 2020;24:559-559.
14.
Rosovsky RP, Sanfilippo KM, Wang TF, et al. Anticoagulation practice patterns in COVID-19: a global survey. Res Pract Thromb Haemost 2020;4:969-983.
15.
Houston BL, Lawler PR, Goligher EC, et al. Anti-Thrombotic Therapy to Ameliorate Complications of COVID-19 (ATTACC): study design and methodology for an international, adaptive Bayesian randomized controlled trial. Clin Trials 2020;17:491-500.
16.
Angus DC, Berry S, Lewis RJ, et al. The REMAP-CAP (Randomized Embedded Multifactorial Adaptive Platform for Community-acquired Pneumonia) study. Rationale and Design. Ann Am Thorac Soc 2020;17:879-891.
17.
The REMAP-CAP, ACTIV-4a, and ATTACC Investigators. Therapeutic anticoagulation with heparin in critically ill patients with Covid-19. N Engl J Med 2021;385:777-789.
18.
Schulman S, Kearon C, the Subcommittee on Control of Anticoagulation of the Scientific and Standardization Committee of the International Society on Thrombosis and Haemostasis. Definition of major bleeding in clinical investigations of antihemostatic medicinal products in non-surgical patients. J Thromb Haemost 2005;3:692-694.
19.
McGlothlin AE, Viele K. Bayesian hierarchical models. JAMA 2018;320:2365-2366.
20.
Nadkarni GN, Lala A, Bagiella E, et al. Anticoagulation, bleeding, mortality, and pathology in hospitalized patients with COVID-19. J Am Coll Cardiol 2020;76:1815-1826.
21.
Ionescu F, Jaiyesimi I, Petrescu I, et al. Association of anticoagulation dose and survival in hospitalized COVID-19 patients: a retrospective propensity score-weighted analysis. Eur J Haematol 2021;106:165-174.
22.
Fröhlich GM, Jeschke E, Eichler U, et al. Impact of oral anticoagulation on clinical outcomes of COVID-19: a nationwide cohort study of hospitalized patients in Germany. Clin Res Cardiol 2021;110:1041-1050.
23.
Connors JM, Levy JH. COVID-19 and its implications for thrombosis and anticoagulation. Blood 2020;135:2033-2040.
24.
Ackermann M, Verleden SE, Kuehnel M, et al. Pulmonary vascular endothelialitis, thrombosis, and angiogenesis in Covid-19. N Engl J Med 2020;383:120-128.
25.
Hanley B, Naresh KN, Roufosse C, et al. Histopathological findings and viral tropism in UK patients with severe fatal COVID-19: a post-mortem study. Lancet Microbe 2020;1(6):e245-e253.
26.
Rapkiewicz AV, Mai X, Carsons SE, et al. Megakaryocytes and platelet-fibrin thrombi characterize multi-organ thrombosis at autopsy in COVID-19: a case series. EClinicalMedicine 2020;24:100434-100434.
27.
Liu J, Li J, Arnold K, Pawlinski R, Key NS. Using heparin molecules to manage COVID-2019. Res Pract Thromb Haemost 2020;4:518-523.
28.
Sadeghipour P, Talasaz AH, Rashidi F, et al. Effect of intermediate-dose vs standard-dose prophylactic anticoagulation on thrombotic events, extracorporeal membrane oxygenation treatment, or mortality among patients with COVID-19 admitted to the intensive care unit: the INSPIRATION randomized clinical trial. JAMA 2021;325:1620-1630.
29.
Xue M, Zeng Y, Qu H-Q, et al. Heparin-binding protein levels correlate with aggravation and multiorgan damage in severe COVID-19. ERJ Open Res 2021;7(1):00741-2020-00741-2020.
30.
White D, MacDonald S, Bull T, et al. Heparin resistance in COVID-19 patients in the intensive care unit. J Thromb Thrombolysis 2020;50:287-291.
31.
Fisher J, Linder A. Heparin-binding protein: a key player in the pathophysiology of organ dysfunction in sepsis. J Intern Med 2017;281:562-574.
32.
Jiménez D, García-Sanchez A, Rali P, et al. Incidence of VTE and bleeding among hospitalized patients with coronavirus disease 2019: a systematic review and meta-analysis. Chest 2021;159:1182-1196.
Information & Authors
Information
Published In
Copyright
Copyright © 2021 Massachusetts Medical Society. All rights reserved.
History
Published online: August 4, 2021
Published in issue: August 26, 2021
Topics
Authors
Affiliations
From the Peter Munk Cardiac Centre at University Health Network (P.R.L., M.E.F., V.D., J.P.G., L.C.G., G.H.), the University of Toronto (P.R.L., E.C.G., A.S.S., M.E.F., V.D., R.A.F., L.C.G., G.H., M.H.), University Health Network (E.C.G., M.H.), St. Michael’s Hospital Unity Health (A.S.S., Z.B., J.C.M., M.S.), Ozmosis Research (L.B., L.P.G.D., V.W.), and Sunnybrook Health Sciences Centre (J.P.G.), Toronto, Ottawa Hospital Research Institute (M. Carrier, L.A.C., D.A.F., G.L.G., D.M.S.), Institut du Savoir Montfort (Marc Carrier, G.L.G.), and the University of Ottawa (L.A.C., D.A.F., D.M.S.), Ottawa, Université Laval (A.F.T.) and CHU de Québec–Université Laval Research Center (A.F.T.), Quebec, QC, the University of Manitoba (B.L.H., A. Kumar, R.Z., S.A.L., D.S., G.V.-G.), CancerCare Manitoba (B.L.H., R.Z.), and St. Boniface Hospital (N.M.), Winnipeg, MB, McGill University, Montreal (S.R.K., E.G.M.), McMaster University (P.L.G.) and the Thrombosis and Atherosclerosis Research Institute (P.L.G.), Hamilton, ON, Université de Sherbrooke, Sherbrooke, QC (F.L.), the University of British Columbia, Vancouver (S. Murthy, K.R.), and the University of Alberta, Edmonton (S.D.) — all in Canada; NYU Grossman School of Medicine (J.S.B., H.R.R., J.S.H., T.C., N.M.K., S.P.), the Icahn School of Medicine at Mount Sinai and Mount Sinai Heart (R.S.R.), NYU Langone Health, NYU Langone Hospital (T.C., J.M.H., E.Y.), and Bellevue Hospital (N.M.K.), New York, Montefiore Medical Center (M.N.G., H.H.B., S.C., J.T.C., R.N.) and Albert Einstein College of Medicine (M.N.G., H.H.B., B.T.G., A. Hope), Bronx, and NYU Langone Long Island, Mineola (R.D.H., A. Hindenburg) — all in New York; the University of Pittsburgh (M.D.N., B.J.M., D.T.H., M.M.B., D.C.A., A.J.K., C.M.L., K.L., S.K.M., C.W.S.), UPMC (M.D.N., B.J.M., D.C.A., K.L., S.K.M.), the Clinical Research, Investigation, and Systems Modeling of Acute Illness (CRISMA) Center, University of Pittsburgh (T.D.G.), and UPMC Children’s Hospital of Pittsburgh (C. Horvat), Pittsburgh, and Emergency Medicine, Penn State Hershey Medical Center, Hershey (S.C.M.) — all in Pennsylvania; Instituto do Coracao, Hospital das Clinicas, Faculdade de Medicina, Universidade de Sao Paulo (J.C.N., L.C.G., F.G.L.), Avanti Pesquisa Clínica (A.S.M.), Hospital de Julho (F.O.S.), and Hospital do Coracao (F.G.Z.), Sao Paulo, Hospital do Coração de Mato Grosso do Sul and the Federal University of Mato Grosso do Sul (M.P.), Hospital Universitário Maria Aparecida Pedrossia (D.G.S.J.), and Hospital Unimed Campo Grande (D.G.S.J.), Campo Grande, and INGOH, Clinical Research Center, Goiânia (M.O.S.) — all in Brazil; Instituto Mexicano del Seguro Social, Mexico City (J.E., Y.S.P.G.); the University of Bristol and University Hospitals Bristol and Weston NHS Foundation Trust (C.A.B.), Bristol, Imperial College London (A.C.G., F.A.-B., M.A.L.), Imperial College Healthcare NHS Trust, St. Mary’s Hospital (A.C.G.), the London School of Hygiene and Tropical Medicine (B.-A.K.), University College London Hospital (R.H.), Kings Healthcare Partners (B.J.H.), the Intensive Care National Audit and Research Centre (P.R.M.), Guy’s and St. Thomas’ NHS Foundation Trust (M.S.-H.), and King’s College London (M.S.-H.), London, Oxford University (A. Beane, S.J.S.) and NHS Blood and Transplant (L.J.E., S.J.S.), Oxford, and Queen’s University Belfast and Royal Victoria Hospital, Belfast (D.F.M.) — all in the United Kingdom; Zuckerberg San Francisco General Hospital, University of California, San Francisco (L.Z.K., C. Hendrickson, M.M.K., A.E.K., M.A.M., B.N.-G.), Harbor–UCLA Medical Center, Torrance (R.J.L., S. Brouwer), Global Coalition for Adaptive Research (M. Buxton) and the University of California Los Angeles (G.L.), Los Angeles, the University of California San Diego School of Medicine, San Diego (T.W.C.), and Stanford University School of Medicine, Palo Alto (J.G.W.) — all in California; Larner College of Medicine at the University of Vermont, Burlington (M. Cushman); Australian and New Zealand Intensive Care Research Centre, Monash University (Z.M., A.M.H., C.J.M., S.A.W., A. Buzgau, C.G., S.P.M., A.D.N., J.C.P., A.C.C.), and Alfred Health (A.C.C., A.D.N.), Melbourne, VIC, St. John of God Subiaco Hospital (S.A.W., E. Litton) and Fiona Stanley Hospital (E. Litton), Perth, WA, and Flinders University, Bedford Park, SA (S. Bihari) — all in Australia; the University of Illinois (K.S.K., J.R.J., J.G.Q.), Cook County Health and Rush Medical College (S. Malhotra), and the University of Chicago (J.D.P.) — all in Chicago; SOCAR Research SA, Nyon (B.-A.K.), and Inselspital, Bern University Hospital, University of Bern (T.T.), Bern — all in Switzerland; Berry Consultants, Austin (R.J.L., E. Lorenzi, S.M.B., L.R.B., M.A.D., M.F., A.M., C.T.S.), University of Texas Southwestern Medical Center, Dallas (A.P.), and Baylor Scott and White Health, Temple (R.J.W.) — all in Texas; Auckland City Hospital (C.J.M., S.P.M., R.L.P.) and the University of Auckland (R.L.P.), Auckland, and the Medical Research Institute of New Zealand, Wellington (C.J.M., A.M.T.) — all in New Zealand; Vanderbilt University Medical Center (A.W.A.) and TriStar Centennial Medical Center (A.L.G.) — both in Nashville; Fédération Hospitalo Universitaire, Raymond Poincaré Hospital, Université de Versailles Saint-Quentin-en-Yvelines, Garches (D. Annane), and Aix-Marseille University, Marseille (B.C.) — both in France; King Saud bin Abdulaziz University for Health Sciences and King Abdullah International Medical Research Center, Riyadh, Saudi Arabia (Y.M.A.); Nepal Mediciti Hospital, Lalitpur, and Nepal Intensive Care Research Foundation, Kathmandu (D. Aryal) — both in Nepal; Versiti Blood Research Institute, Milwaukee (L.B.K., L.J.E.), and the University of Wisconsin School of Medicine and Public Health, Madison (J.P.S.); National Intensive Care Surveillance–Mahidol Oxford Tropical Medicine Research Unit, Colombo, Sri Lanka (A. Beane); the University Medical Center Utrecht, Utrecht University, Utrecht (M. Bonten, R.E.G.S., W.B.-P.), and Radboud University Medical Center, Nijmegen (S. Middeldorp, F.L.V.) — both in the Netherlands; Jena University Hospital, Jena, Germany (F.B.); Cleveland Clinic (A.D.) and Case Western Reserve University, the Metro Health Medical Centre (V.K.) — both in Cleveland; Ochsner Medical Center, University of Queensland–Ochsner Clinical School, New Orleans (M.B.E.); Harvard Medical School (B.M.E., Y.K., N.S.R., A.B.S), Brigham and Women’s Hospital (B.M.E., Y.K., S.M.H.), Boston University School of Medicine and Boston Medical Center (N.M.H.), and Massachusetts General Hospital (A.B.S., N.S.R.) — all in Boston; University of Alabama, Birmingham (S.G.); Hospital Ramón y Cajal (S.G.-M., J.L.L.-S.M., R.M.G.) and IdiPaz Research Institute, Universidad Autonoma (J.L.-S.), Madrid, and University Hospital of Salamanca–University of Salamanca-IBSAL, Salamanca (M.M.) — all in Spain; University of Antwerp, Wilrijk, Belgium (H.G.); Rutgers New Jersey Medical School, Newark (Y.Y.G.); University of Oxford, Bangkok, Thailand (R.H.); Ascension St. John Heart and Vascular Center, Tulsa (N.H.), and the University of Oklahoma College of Medicine, Oklahoma City (N.H.); the University of Cincinnati, Cincinnati (K.H.); University of Michigan, Ann Arbor (R.C.H., P.K.P.), Beaumont Health, Royal Oak, and the OUWB School of Medicine, Auburn Hills (G.B.N.) — all in Michigan; Mayo Clinic, Rochester (V.N.I.), and the Hennepin County Medical Center, Minneapolis (M.E.P.) — both in Minnesota; Apollo Speciality Hospital–OMR, Chennai, India (D.J.); Oregon Health and Science University, Portland (A. Khan, E.S.L.); the National Heart, Lung, and Blood Institute, Bethesda, MD (A.L.K.); University of Mississippi Medical Center, Jackson (M.E.K.); University College Dublin, Dublin (A.D.N.); University of Kansas School of Medicine, Kansas City (L.S.); Duke University Hospital, Durham, NC (L.W.); and Emory University, Atlanta (B.J.W.).
Metrics & Citations
Metrics
Altmetrics
Citations
Export citation
Select the format you want to export the citation of this publication.
Cited by
- Tenecteplase With Concomitant Anticoagulation for Acute Respiratory Failure in Patients With COVID-19: A Randomized Controlled Trial, Cureus, (2024).https://doi.org/10.7759/cureus.54298
- Perspective Chapter: Cardiovascular Post-Acute COVID-19 Syndrome – Definition, Clinical Scenarios, Diagnosis, and Management, New Insights on Cardiomyopathy, (2024).https://doi.org/10.5772/intechopen.109292
- Prophylactic Anticoagulation and Thrombosis in Hospitalized Patients with Clinically Stable COVID-19 at Admission: From the Practice-Based Observational Study, Annals of Vascular Diseases, 17, 1, (1-8), (2024).https://doi.org/10.3400/avd.oa.23-00031
- Small Molecules for the Treatment of Long-COVID-Related Vascular Damage and Abnormal Blood Clotting: A Patent-Based Appraisal, Viruses, 16, 3, (450), (2024).https://doi.org/10.3390/v16030450
- Choice and Duration of Anticoagulation for Venous Thromboembolism, Journal of Clinical Medicine, 13, 1, (301), (2024).https://doi.org/10.3390/jcm13010301
- Special Issue “COVID-19 Coagulopathy: Advances on Pathophysiology and Therapies”, International Journal of Molecular Sciences, 25, 6, (3548), (2024).https://doi.org/10.3390/ijms25063548
- Therapeutic development targeting host heparan sulfate proteoglycan in SARS-CoV-2 infection, Frontiers in Medicine, 11, (2024).https://doi.org/10.3389/fmed.2024.1364657
- Association between loss of hypercoagulable phenotype, clinical features and complement pathway consumption in COVID-19, Frontiers in Immunology, 15, (2024).https://doi.org/10.3389/fimmu.2024.1337070
- Effect of anticoagulation on the incidence of venous thromboembolism, major bleeding, and mortality among hospitalized COVID-19 patients: an updated meta-analysis, Frontiers in Cardiovascular Medicine, 11, (2024).https://doi.org/10.3389/fcvm.2024.1381408
- IL-6 and D-dimer Levels at Admission Predict Cardiac Injury and Early Mortality during SARS-CoV-2 Infection, Cardiovascular Innovations and Applications, 9, 1, (2024).https://doi.org/10.15212/CVIA.2024.0009
- See more
Loading...