Dosing & Uses
Dosage Forms & Strengths
heparin lock solution
- 1unit/mL
- 2units/mL
- 10units/mL
- 100units/mL
injectable solution
- 1000units/mL
- 2500units/mL
- 5000units/mL
- 10,000units/mL
- 20,000units/mL
premixed IV solution
- 12,500units/250mL
- 20,000units/500mL
- 25,000units/250mL
- 25,000units/500mL
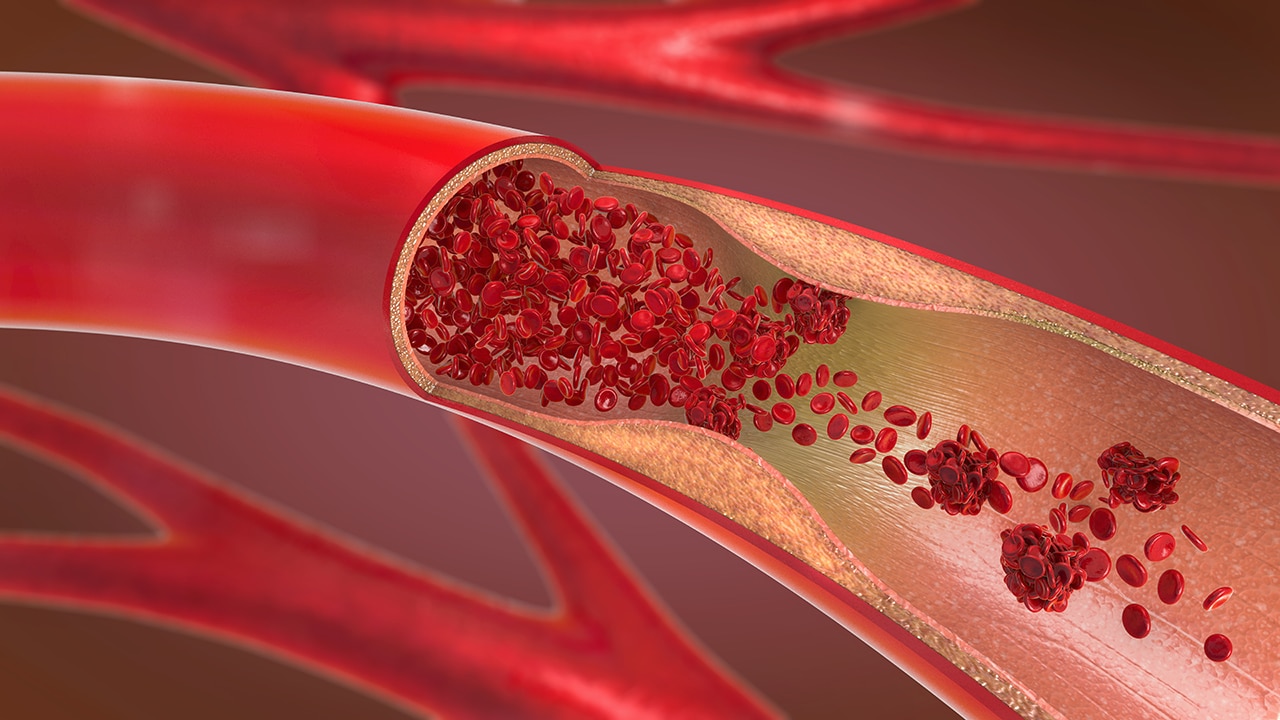
DVT & PE
Prophylaxis
- 5000 units SC q8-12hr, OR
- 7500 units SC q12hr
Treatment
- 80 units/kg IV bolus, THEN continuous infusion of 18 units/kg/hr, OR
- 5000 units IV bolus, THEN continuous infusion of 1300 units/hr, OR
- 250 units/kg (alternatively, 17,500 units) SC, THEN 250 units/kg q12hr
Dosing considerations
- Numerous concentrations available; extreme caution is required to avoid medication error
Acute Coronary Syndromes
PCI
- Without GPIIb/IIIa inhibitor: Initial IV bolus of 70-100 units/kg (target ACT 250-300 sec)
- With GPIIb/IIIa inhibitor: Initial IV bolus of 50-70 units/kg (target ACT >200 sec)
STEMI
- Patient on fibrinolytics: IV bolus of 60 units/kg (max: 4000 units), THEN 12 units/kg/hr (max 1000 units/hr) as continuous IV infusion
- Dose should be adjusted to maintain aPTT of 50-70 sec
Unstable Angina/NSTEMI
- Initial IV bolus of 60-70 units/kg (max: 5000 units), THEN initial IV infusion of 12-15 units/kg/hr (max: 1000 units/hr)
- Dose should be adjusted to maintain aPTT of 50-70 sec
Dosing considerations
- Numerous concentrations available; extreme caution is required to avoid medication error
Anticoagulation
Intermittent IV injection
Continuous IV infusion
- 5000 units IV injection, followed by continuous IV infusion of 20,000-40,000 units/24 hr
Dosing considerations
- Numerous concentrations available; extreme caution is required to avoid medication error
- Heparin sodium may prolong one-stage prothrombin time; when heparin sodium is given with dicumarol or warfarin sodium, a period of at least 5 hr after last intravenous dose or 24 hr after last subcutaneous dose should elapse before blood is drawn if a valid prothrombin time is to be obtained
Catheter Patency
Prevention of clot formation within venous and arterial catheters
Use 100 units/mL; instill enough volume to fill lumen of catheter
Dosing considerations
- Numerous concentrations available; extreme caution is required to avoid medication error
- Amount and frequency depends on catheter volume and type
- Peripheral heparin locks typically are flushed q6-8hr
Dosing Modifications
Hepatic impairment: Caution is advised; dosage adjustment may be required
Dosage Forms & Strengths
heparin lock solution
- 10units/mL
- 100units/mL
injectable solution
- 1000units/mL
- 5000units/mL
- 10,000units/mL
Venous Thromboembolic Prophylaxis (Off-label)
Venous Thromboembolic Treatment (Off-label)
<1 year
>1 year
- Loading dose of 75 units/kg IV, THEN 20 units/kg/hr IV as initial maintenance dose
Intermittent IV injection
- Initially give 50-100 units/kg IV infusion, THEN 100 units/kg IV infusion q4hr as a maintenance dose
Catheter Patency (Off-label)
Initially give 50-100 units/kg IV infusion, THEN 100 units/kg IV infusion q4hr as maintenance dose
Infants under 10 kg: 10 units/mL; instill enough volume to fill lumen of catheter
Children and infants over 10 kg: 10-100 units/mL; instill enough volume to fill lumen of catheter
Dosing Considerations
Numerous concentrations available; extreme caution is required to avoid medication error
When prescribing in infants, consider combined daily metabolic load of benzyl alcohol from all sources including heparin sodium injection (contains 9.45 mg of benzyl alcohol) and other drugs containing benzyl alcohol; the minimum amount of benzyl alcohol at which serious adverse reactions may occur is not known
There are no adequate, well-controlled studies on heparin use in pediatric patients; pediatric dosing recommendations are based on clinical experience
Use preservative-free heparin in neonates and infants; benzyl alcohol preservative has been associated with serious adverse effects (ie, gasping syndrome, which is characterized by central nervous system depression, metabolic acidosis, and gasping respirations) and death in pediatric patients
Venous thromboembolic treatment (off-label)
- Adjust heparin dose based on desired aPTT
Catheter patency (off-label)
- Dosage amount and frequency depend on catheter volume and type
- Peripheral heparin locks typically are flushed q6-8hr
Interactions
Interaction Checker
No Results

Contraindicated
Serious - Use Alternative
Significant - Monitor Closely
Minor

Contraindicated (4)
- corticorelin
heparin increases toxicity of corticorelin by unknown mechanism. Contraindicated. Do not use heparin to maintain IV cannula patency during corticorelin test; may lead to severe hypot'n.
- defibrotide
defibrotide increases effects of heparin by pharmacodynamic synergism. Contraindicated. Coadministration of defibrotide is contraindicated with antithrombotic/fibrinolytic drugs. This does not include use for routine maintenance or reopening of central venous lines.
- mifepristone
mifepristone, heparin. Other (see comment). Contraindicated. Comment: Mifepristone may lead to excessive post abortion bleeding in pts. on anticoagulant therapy.
- prothrombin complex concentrate, human
heparin, prothrombin complex concentrate, human. pharmacodynamic antagonism. Contraindicated.
Serious - Use Alternative (65)
- abciximab
heparin, abciximab. Either increases effects of the other by pharmacodynamic synergism. Contraindicated. Enhanced risk of hemorrhage.
- amobarbital
amobarbital decreases effects of heparin by increasing metabolism. Avoid or Use Alternate Drug.
- anagrelide
heparin, anagrelide. Either increases effects of the other by pharmacodynamic synergism. Contraindicated. Enhanced risk of hemorrhage.
- antithrombin alfa
antithrombin alfa and heparin both increase anticoagulation. Avoid or Use Alternate Drug.
- antithrombin III
antithrombin III and heparin both increase anticoagulation. Avoid or Use Alternate Drug.
- apixaban
heparin and apixaban both increase anticoagulation. Avoid or Use Alternate Drug.
- argatroban
argatroban and heparin both increase anticoagulation. Avoid or Use Alternate Drug.
- azithromycin
azithromycin increases effects of heparin by decreasing metabolism. Avoid or Use Alternate Drug.
- bazedoxifene/conjugated estrogens
bazedoxifene/conjugated estrogens decreases effects of heparin by pharmacodynamic antagonism. Contraindicated. Risk of thromboembolic disorders.
- bemiparin
bemiparin and heparin both increase anticoagulation. Avoid or Use Alternate Drug.
- bivalirudin
bivalirudin and heparin both increase anticoagulation. Avoid or Use Alternate Drug.
- butabarbital
butabarbital decreases effects of heparin by increasing metabolism. Avoid or Use Alternate Drug.
- butalbital
butalbital decreases effects of heparin by increasing metabolism. Avoid or Use Alternate Drug.
- caplacizumab
caplacizumab, heparin. Either increases effects of the other by anticoagulation. Avoid or Use Alternate Drug.
- cefamandole
cefamandole increases effects of heparin by pharmacodynamic synergism. Avoid or Use Alternate Drug.
- cefazolin
cefazolin increases effects of heparin by pharmacodynamic synergism. Avoid or Use Alternate Drug.
- cefdinir
cefdinir increases effects of heparin by anticoagulation. Avoid or Use Alternate Drug. cephalosporins may decrease prothrombin activity.
- cefditoren
cefditoren will increase the level or effect of heparin by anticoagulation. Avoid or Use Alternate Drug. cephalosporins may decrease prothrombin activity
- cefotetan
cefotetan increases effects of heparin by anticoagulation. Avoid or Use Alternate Drug. cephalosporins may decrease prothrombin activity.
- cefoxitin
cefoxitin will increase the level or effect of heparin by anticoagulation. Avoid or Use Alternate Drug. cephalosporins may decrease prothrombin activity
- cefpodoxime
cefpodoxime will increase the level or effect of heparin by anticoagulation. Avoid or Use Alternate Drug. cephalosporins may decrease prothrombin activity
- ceftriaxone
ceftriaxone will increase the level or effect of heparin by anticoagulation. Avoid or Use Alternate Drug. cephalosporins may decrease prothrombin activity
- cefuroxime
cefuroxime will increase the level or effect of heparin by anticoagulation. Avoid or Use Alternate Drug. cephalosporins may decrease prothrombin activity
- cilostazol
heparin, cilostazol. Either increases effects of the other by pharmacodynamic synergism. Contraindicated. Enhanced risk of hemorrhage.
- clarithromycin
clarithromycin increases effects of heparin by decreasing metabolism. Avoid or Use Alternate Drug.
- conjugated estrogens
conjugated estrogens decreases effects of heparin by pharmacodynamic antagonism. Contraindicated. Risk of thromboembolic disorders.
- dabigatran
dabigatran and heparin both increase anticoagulation. Avoid or Use Alternate Drug. Both drugs have the potential to cause bleeding. Concomitant use may increase risk of bleeding.
- dalteparin
dalteparin and heparin both increase anticoagulation. Avoid or Use Alternate Drug.
- dipyridamole
heparin, dipyridamole. Either increases effects of the other by pharmacodynamic synergism. Contraindicated. Enhanced risk of hemorrhage.
- edoxaban
edoxaban, heparin. Either increases toxicity of the other by anticoagulation. Avoid or Use Alternate Drug. Both drugs have the potential to cause bleeding, monitor closely. Promptly evaluate any signs or symptoms of blood loss. Long-term concomitant treatment with edoxaban and other anticoagulants is not recommended. Short-term coadministration may be needed for patients transitioning to or from edoxaban.
- enoxaparin
enoxaparin and heparin both increase anticoagulation. Avoid or Use Alternate Drug.
- eptifibatide
heparin, eptifibatide. Either increases effects of the other by pharmacodynamic synergism. Contraindicated. Enhanced risk of hemorrhage.
- erythromycin base
erythromycin base increases effects of heparin by decreasing metabolism. Avoid or Use Alternate Drug.
- erythromycin ethylsuccinate
erythromycin ethylsuccinate increases effects of heparin by decreasing metabolism. Avoid or Use Alternate Drug.
- erythromycin lactobionate
erythromycin lactobionate increases effects of heparin by decreasing metabolism. Avoid or Use Alternate Drug.
- erythromycin stearate
erythromycin stearate increases effects of heparin by decreasing metabolism. Avoid or Use Alternate Drug.
- estradiol
estradiol decreases effects of heparin by pharmacodynamic antagonism. Contraindicated. Risk of thromboembolic disorders.
- estrogens conjugated synthetic
estrogens conjugated synthetic decreases effects of heparin by pharmacodynamic antagonism. Contraindicated. Risk of thromboembolic disorders.
- estropipate
estropipate decreases effects of heparin by pharmacodynamic antagonism. Contraindicated. Risk of thromboembolic disorders.
- ethinylestradiol
ethinylestradiol decreases effects of heparin by pharmacodynamic antagonism. Contraindicated. Risk of thromboembolic disorders.
- Factor X, human
heparin will decrease the level or effect of Factor X, human by pharmacodynamic antagonism. Avoid or Use Alternate Drug. Based on the mechanism of action, Factor X is likely to be counteracted by direct and indirect Factor Xa inhibitors.
- fondaparinux
fondaparinux and heparin both increase anticoagulation. Avoid or Use Alternate Drug.
- levonorgestrel intrauterine
levonorgestrel intrauterine, heparin. Either decreases effects of the other by pharmacodynamic antagonism. Avoid or Use Alternate Drug. Risk of thromboembolic disorders.
- levonorgestrel oral
levonorgestrel oral, heparin. Either decreases effects of the other by pharmacodynamic antagonism. Avoid or Use Alternate Drug. Risk of thromboembolic disorders.
- levothyroxine
levothyroxine increases effects of heparin by pharmacodynamic synergism. Avoid or Use Alternate Drug.
- liothyronine
liothyronine increases effects of heparin by pharmacodynamic synergism. Avoid or Use Alternate Drug.
- mestranol
mestranol decreases effects of heparin by pharmacodynamic antagonism. Contraindicated. Risk of thromboembolic disorders.
- pentobarbital
pentobarbital decreases effects of heparin by increasing metabolism. Avoid or Use Alternate Drug.
- phenindione
heparin and phenindione both increase anticoagulation. Avoid or Use Alternate Drug.
- phenobarbital
phenobarbital decreases effects of heparin by increasing metabolism. Avoid or Use Alternate Drug.
- piperacillin
piperacillin will increase the level or effect of heparin by anticoagulation. Avoid or Use Alternate Drug. piperacillin can inhibit platelet aggregation
- prasugrel
heparin, prasugrel. Either increases effects of the other by pharmacodynamic synergism. Contraindicated. Enhanced risk of hemorrhage.
- primidone
primidone decreases effects of heparin by increasing metabolism. Avoid or Use Alternate Drug.
- protamine
heparin and protamine both increase anticoagulation. Avoid or Use Alternate Drug.
- quinine
quinine increases effects of heparin by unknown mechanism. Avoid or Use Alternate Drug.
- roxithromycin
roxithromycin increases effects of heparin by decreasing metabolism. Avoid or Use Alternate Drug.
- secobarbital
secobarbital decreases effects of heparin by increasing metabolism. Avoid or Use Alternate Drug.
- sulfadiazine
sulfadiazine increases effects of heparin by decreasing metabolism. Avoid or Use Alternate Drug.
sulfadiazine increases effects of heparin by plasma protein binding competition. Avoid or Use Alternate Drug. - sulfamethoxazole
sulfamethoxazole increases effects of heparin by decreasing metabolism. Avoid or Use Alternate Drug.
sulfamethoxazole increases effects of heparin by plasma protein binding competition. Avoid or Use Alternate Drug. - sulfisoxazole
sulfisoxazole increases effects of heparin by decreasing metabolism. Avoid or Use Alternate Drug.
sulfisoxazole increases effects of heparin by plasma protein binding competition. Avoid or Use Alternate Drug. - thyroid desiccated
thyroid desiccated increases effects of heparin by pharmacodynamic synergism. Avoid or Use Alternate Drug.
- tibolone
tibolone increases effects of heparin by pharmacodynamic synergism. Avoid or Use Alternate Drug.
- ticlopidine
heparin, ticlopidine. Either increases effects of the other by pharmacodynamic synergism. Contraindicated. Enhanced risk of hemorrhage.
- tirofiban
heparin, tirofiban. Either increases effects of the other by pharmacodynamic synergism. Contraindicated. Enhanced risk of hemorrhage.
- warfarin
heparin increases effects of warfarin by anticoagulation. Avoid or Use Alternate Drug. Avoid combined use once INR is established in the desired therapeutic range.
Monitor Closely (149)
- acalabrutinib
acalabrutinib increases effects of heparin by anticoagulation. Use Caution/Monitor. Coadministration of acalabrutinib with antiplatelets or anticoagulants may further increase risk of hemorrhage. Monitor for signs of bleeding and consider the benefit-risk of withholding acalabrutinib for 3-7 days presurgery and postsurgery depending upon the type of surgery and the risk of bleeding.
- aceclofenac
heparin and aceclofenac both increase anticoagulation. Modify Therapy/Monitor Closely.
- acemetacin
heparin and acemetacin both increase anticoagulation. Modify Therapy/Monitor Closely.
- agrimony
heparin and agrimony both increase anticoagulation. Modify Therapy/Monitor Closely.
- alfalfa
heparin and alfalfa both increase anticoagulation. Modify Therapy/Monitor Closely.
- alteplase
heparin and alteplase both increase anticoagulation. Modify Therapy/Monitor Closely.
- American ginseng
heparin and American ginseng both increase anticoagulation. Modify Therapy/Monitor Closely.
- amiloride
amiloride, heparin. Either increases toxicity of the other by serum potassium. Use Caution/Monitor. Both drugs may increase serum potassium levels.
- anamu
heparin and anamu both increase anticoagulation. Use Caution/Monitor.
- antithrombin III
antithrombin III increases effects of heparin by pharmacodynamic synergism. Use Caution/Monitor. Use reduced dose of heparin during antithrombin III therapy to avoid bleeding.
- aspirin
heparin and aspirin both increase anticoagulation. Modify Therapy/Monitor Closely.
aspirin, heparin. Either increases toxicity of the other by anticoagulation. Use Caution/Monitor. The need for simultaneous use of low-dose aspirin and anticoagulant or antiplatelet agents are common for patients with cardiovascular disease; monitor closely. - aspirin rectal
heparin and aspirin rectal both increase anticoagulation. Modify Therapy/Monitor Closely.
- aspirin/citric acid/sodium bicarbonate
aspirin/citric acid/sodium bicarbonate, heparin. Either increases toxicity of the other by anticoagulation. Use Caution/Monitor. The need for simultaneous use of low-dose aspirin and anticoagulant or antiplatelet agents are common for patients with cardiovascular disease; monitor closely.
heparin and aspirin/citric acid/sodium bicarbonate both increase anticoagulation. Modify Therapy/Monitor Closely. - azapropazone
azapropazone increases effects of heparin by plasma protein binding competition. Use Caution/Monitor.
- azathioprine
azathioprine decreases effects of heparin by unknown mechanism. Use Caution/Monitor.
- azficel-T
azficel-T, heparin. Other (see comment). Use Caution/Monitor. Comment: Coadministration with anticoagulants or antiplatelets may increase bruising or bleeding at biopsy and/or injection sites; concomitant use not recommended. Decisions regarding continued use or cessation of anticoagulants or antiplatelets should be made by a physician.
- azilsartan
heparin increases toxicity of azilsartan by Other (see comment). Use Caution/Monitor. Comment: Low molecular weight heparins may suppress adrenal aldosterone secretion, which can potentially cause hyperkalemia.
- benazepril
heparin increases toxicity of benazepril by Other (see comment). Use Caution/Monitor. Comment: Low molecular weight heparins may suppress adrenal aldosterone secretion, which can potentially cause hyperkalemia.
- betrixaban
heparin, betrixaban. Either increases levels of the other by anticoagulation. Use Caution/Monitor.
- budesonide
budesonide, heparin. Other (see comment). Use Caution/Monitor. Comment: Corticosteroids may decrease anticoagulant effects by increasing blood coagulability; conversely, they may impair vascular integrity, thus increasing bleeding risk. Monitor INR closely.
- canagliflozin
heparin and canagliflozin both increase serum potassium. Use Caution/Monitor.
- candesartan
heparin increases toxicity of candesartan by Other (see comment). Use Caution/Monitor. Comment: Low molecular weight heparins may suppress adrenal aldosterone secretion, which can potentially cause hyperkalemia.
- capecitabine
capecitabine increases effects of heparin by unspecified interaction mechanism. Use Caution/Monitor.
- captopril
heparin increases toxicity of captopril by Other (see comment). Use Caution/Monitor. Comment: Low molecular weight heparins may suppress adrenal aldosterone secretion, which can potentially cause hyperkalemia.
- carbamazepine
carbamazepine decreases levels of heparin by increasing metabolism. Use Caution/Monitor.
- celecoxib
heparin and celecoxib both increase anticoagulation. Modify Therapy/Monitor Closely.
- chitosan
chitosan increases effects of heparin by Other (see comment). Use Caution/Monitor. Comment: Chitosan can decrease GI absorption of vitamin K, enhancing anticoagulant effects.
- choline magnesium trisalicylate
heparin and choline magnesium trisalicylate both increase anticoagulation. Modify Therapy/Monitor Closely.
- cinnamon
heparin and cinnamon both increase anticoagulation. Modify Therapy/Monitor Closely.
- citalopram
citalopram increases effects of heparin by pharmacodynamic synergism. Use Caution/Monitor. Combination may increase risk of bleeding.
- clopidogrel
heparin, clopidogrel. Either increases effects of the other by pharmacodynamic synergism. Modify Therapy/Monitor Closely. Enhanced risk of hemorrhage; additive effects are intended when both drugs are prescribed as indicated for ACS.
- collagenase clostridium histolyticum
heparin increases toxicity of collagenase clostridium histolyticum by anticoagulation. Use Caution/Monitor. Collagenase clostridium histolyticum has high incidence of ecchymosis/contusion at injection site; avoid concomitant anticoagulants (except for low-dose aspirin, ie, up to 150 mg/day).
- conjugated estrogens, vaginal
conjugated estrogens, vaginal decreases effects of heparin by pharmacodynamic antagonism. Modify Therapy/Monitor Closely. Risk of thromboembolic disorders.
- cordyceps
heparin and cordyceps both increase anticoagulation. Modify Therapy/Monitor Closely.
- cornsilk
cornsilk decreases effects of heparin by pharmacodynamic antagonism. Use Caution/Monitor. Cornsilk contains vitamin K; consume a consistent amount daily.
- cortisone
cortisone, heparin. Other (see comment). Use Caution/Monitor. Comment: Corticosteroids may decrease anticoagulant effects by increasing blood coagulability; conversely, they may impair vascular integrity, thus increasing bleeding risk. Monitor INR closely.
- cyclophosphamide
cyclophosphamide increases effects of heparin by unknown mechanism. Use Caution/Monitor. Due to potential thrombocytopenic effects of cyclophosphamide, an additive risk of bleeding may be seen in patients receiving concomitant anticoagulants.
- danshen
heparin and danshen both increase anticoagulation. Use Caution/Monitor.
- deferasirox
deferasirox, heparin. Other (see comment). Use Caution/Monitor. Comment: Gastric ulceration and GI bleeding have been reported in patients taking deferasirox, use caution when coadministering with other drugs known to increase the risk of peptic ulcers or gastric hemorrhage including anticoagulants.
- deflazacort
deflazacort, heparin. Other (see comment). Use Caution/Monitor. Comment: Corticosteroids may decrease anticoagulant effects by increasing blood coagulability; conversely, they may impair vascular integrity, thus increasing bleeding risk. Monitor INR closely.
- devil's claw
heparin and devil's claw both increase anticoagulation. Use Caution/Monitor.
- dexamethasone
dexamethasone, heparin. Other (see comment). Use Caution/Monitor. Comment: Corticosteroids may decrease anticoagulant effects by increasing blood coagulability; conversely, they may impair vascular integrity, thus increasing bleeding risk. Monitor INR closely.
- diclofenac
heparin and diclofenac both increase anticoagulation. Modify Therapy/Monitor Closely.
- diflunisal
heparin and diflunisal both increase anticoagulation. Modify Therapy/Monitor Closely.
diflunisal increases effects of heparin by plasma protein binding competition. Use Caution/Monitor. - dong quai
heparin and dong quai both increase anticoagulation. Modify Therapy/Monitor Closely.
- enalapril
heparin increases toxicity of enalapril by Other (see comment). Use Caution/Monitor. Comment: Low molecular weight heparins may suppress adrenal aldosterone secretion, which can potentially cause hyperkalemia.
- epoprostenol
heparin and epoprostenol both increase anticoagulation. Modify Therapy/Monitor Closely.
- eprosartan
heparin increases toxicity of eprosartan by Other (see comment). Use Caution/Monitor. Comment: Low molecular weight heparins may suppress adrenal aldosterone secretion, which can potentially cause hyperkalemia.
- ethanol
ethanol increases effects of heparin by unknown mechanism. Use Caution/Monitor. Acute EtOH intoxication.
- ethotoin
heparin increases levels of ethotoin by unknown mechanism. Use Caution/Monitor.
ethotoin, heparin. Other (see comment). Use Caution/Monitor. Comment: Hydantoin anticonvulsants increase anticoagulant effects at first, then decrease those effects with continued use (2+ wks). There are multiple mechanisms involved, including enzyme induction, plasma protein binding site competition, and additive effects on prothrombin time. - etodolac
heparin and etodolac both increase anticoagulation. Modify Therapy/Monitor Closely.
- fenbufen
heparin and fenbufen both increase anticoagulation. Modify Therapy/Monitor Closely.
- fennel
heparin and fennel both increase anticoagulation. Modify Therapy/Monitor Closely.
- fenoprofen
heparin and fenoprofen both increase anticoagulation. Modify Therapy/Monitor Closely.
- feverfew
heparin and feverfew both increase anticoagulation. Modify Therapy/Monitor Closely.
- finerenone
heparin and finerenone both increase serum potassium. Modify Therapy/Monitor Closely. Finerenone dose adjustment based on current serum potassium concentration. Monitor serum potassium and adjust finerenone dose as described in the prescribing information as necessary.
- fish oil
fish oil, heparin. Other (see comment). Use Caution/Monitor. Comment: Patients taking fish oil and an anticoagulant or other drug affecting coagulation should be monitored periodically due to potential increased risk of bleeding. .
- fish oil triglycerides
fish oil triglycerides will increase the level or effect of heparin by anticoagulation. Use Caution/Monitor. Prolonged bleeding reported in patients taking antiplatelet agents or anticoagulants and oral omega-3 fatty acids. Periodically monitor bleeding time in patients receiving fish oil triglycerides and concomitant antiplatelet agents or anticoagulants.
- fludrocortisone
fludrocortisone, heparin. Other (see comment). Use Caution/Monitor. Comment: Corticosteroids may decrease anticoagulant effects by increasing blood coagulability; conversely, they may impair vascular integrity, thus increasing bleeding risk. Monitor INR closely.
- fluorouracil
fluorouracil increases effects of heparin by unspecified interaction mechanism. Use Caution/Monitor. Due to the thrombocytopenic effects of fluorouracil, an additive risk of bleeding may be seen in patients receiving concomitant anticoagulants.
- flurbiprofen
heparin and flurbiprofen both increase anticoagulation. Modify Therapy/Monitor Closely.
- forskolin
heparin and forskolin both increase anticoagulation. Modify Therapy/Monitor Closely.
- fosinopril
heparin increases toxicity of fosinopril by Other (see comment). Use Caution/Monitor. Comment: Low molecular weight heparins may suppress adrenal aldosterone secretion, which can potentially cause hyperkalemia.
- fosphenytoin
heparin increases levels of fosphenytoin by unknown mechanism. Use Caution/Monitor.
fosphenytoin, heparin. Other (see comment). Use Caution/Monitor. Comment: Hydantoin anticonvulsants increase anticoagulant effects at first, then decrease those effects with continued use (2+ wks). There are multiple mechanisms involved, including enzyme induction, plasma protein binding site competition, and additive effects on prothrombin time. - garlic
heparin and garlic both increase anticoagulation. Modify Therapy/Monitor Closely.
- gemcitabine
gemcitabine increases effects of heparin by unspecified interaction mechanism. Use Caution/Monitor. Due to the thrombocytopenic effects of gemcitabine, an additive risk of bleeding may be seen in patients receiving concomitant anticoagulants.
- ginger
heparin and ginger both increase anticoagulation. Modify Therapy/Monitor Closely.
- ginkgo biloba
heparin and ginkgo biloba both increase anticoagulation. Modify Therapy/Monitor Closely.
- glucagon intranasal
glucagon intranasal increases effects of heparin by unknown mechanism. Use Caution/Monitor.
- green tea
green tea, heparin. Other (see comment). Use Caution/Monitor. Comment: Combination may increase risk of bleeding, caution is advised.
- hemin
heparin, hemin. Either increases effects of the other by anticoagulation. Use Caution/Monitor. Hemin degradation product (ie, hematin) may produce coagulopathy (eg, thrombocytopenia, platelet degranulation) and cause mild anticoagulant effects.
- horse chestnut seed
heparin and horse chestnut seed both increase anticoagulation. Modify Therapy/Monitor Closely.
- hydrocortisone
hydrocortisone, heparin. Other (see comment). Use Caution/Monitor. Comment: Corticosteroids may decrease anticoagulant effects by increasing blood coagulability; conversely, they may impair vascular integrity, thus increasing bleeding risk. Monitor INR closely.
- ibrutinib
ibrutinib, heparin. Either increases effects of the other by anticoagulation. Use Caution/Monitor. Ibrutinib may potentiate the effects of anticoagulant agents such as warfarin may increase the risk of bleeding; monitor for signs of bleeding.
heparin, ibrutinib. Either increases effects of the other by anticoagulation. Use Caution/Monitor. Ibrutinib may potentiate the effects of anticoagulant agents such as warfarin may increase the risk of bleeding; monitor for signs of bleeding. - ibuprofen
heparin and ibuprofen both increase anticoagulation. Modify Therapy/Monitor Closely.
- ibuprofen IV
heparin and ibuprofen IV both increase anticoagulation. Modify Therapy/Monitor Closely.
- icosapent
icosapent, heparin. Either increases effects of the other by pharmacodynamic synergism. Use Caution/Monitor. Icosapent may prolong bleeding time; monitor periodically if coadministered with other drugs that affect bleeding.
- imatinib
imatinib, heparin. Either increases toxicity of the other by Other (see comment). Modify Therapy/Monitor Closely. Comment: Imatinib may cause thrombocytopenia; bleeding risk increased when imatinib is coadministered with anticoagulants, NSAIDs, platelet inhibitors, and thrombolytic agents; patients requiring anticoagulation while on imatinib should receive LMWH or unfractionated heparin instead of warfarin because of multiple interaction mechanisms of imatinib with warfarin.
- indomethacin
heparin and indomethacin both increase anticoagulation. Modify Therapy/Monitor Closely.
- iodine (radioactive)
iodine (radioactive) decreases effects of heparin by pharmacodynamic antagonism. Use Caution/Monitor.
- irbesartan
heparin increases toxicity of irbesartan by Other (see comment). Use Caution/Monitor. Comment: Low molecular weight heparins may suppress adrenal aldosterone secretion, which can potentially cause hyperkalemia.
- ketoprofen
heparin and ketoprofen both increase anticoagulation. Modify Therapy/Monitor Closely.
- ketorolac
heparin and ketorolac both increase anticoagulation. Modify Therapy/Monitor Closely.
- ketorolac intranasal
heparin and ketorolac intranasal both increase anticoagulation. Modify Therapy/Monitor Closely.
- lisinopril
heparin increases toxicity of lisinopril by Other (see comment). Use Caution/Monitor. Comment: Low molecular weight heparins may suppress adrenal aldosterone secretion, which can potentially cause hyperkalemia.
- lofepramine
lofepramine increases levels of heparin by decreasing metabolism. Use Caution/Monitor.
- lornoxicam
heparin and lornoxicam both increase anticoagulation. Modify Therapy/Monitor Closely.
- losartan
heparin increases toxicity of losartan by Other (see comment). Use Caution/Monitor. Comment: Low molecular weight heparins may suppress adrenal aldosterone secretion, which can potentially cause hyperkalemia.
- meclofenamate
heparin and meclofenamate both increase anticoagulation. Modify Therapy/Monitor Closely.
- mefenamic acid
heparin and mefenamic acid both increase anticoagulation. Modify Therapy/Monitor Closely.
- melatonin
melatonin increases effects of heparin by anticoagulation. Use Caution/Monitor. Melatonin may decrease prothrombin time.
- meloxicam
heparin and meloxicam both increase anticoagulation. Modify Therapy/Monitor Closely.
- methimazole
methimazole decreases effects of heparin by pharmacodynamic antagonism. Use Caution/Monitor.
- methylprednisolone
methylprednisolone, heparin. Other (see comment). Use Caution/Monitor. Comment: Corticosteroids may decrease anticoagulant effects by increasing blood coagulability; conversely, they may impair vascular integrity, thus increasing bleeding risk. Monitor INR closely.
- mipomersen
mipomersen, heparin. Either increases toxicity of the other by Other (see comment). Use Caution/Monitor. Comment: Both drugs have potential to increase hepatic enzymes; monitor LFTs.
- mistletoe
heparin increases and mistletoe decreases anticoagulation. Effect of interaction is not clear, use caution. Modify Therapy/Monitor Closely.
- moexipril
heparin increases toxicity of moexipril by Other (see comment). Use Caution/Monitor. Comment: Low molecular weight heparins may suppress adrenal aldosterone secretion, which can potentially cause hyperkalemia.
- nabumetone
heparin and nabumetone both increase anticoagulation. Modify Therapy/Monitor Closely.
- naproxen
heparin and naproxen both increase anticoagulation. Modify Therapy/Monitor Closely.
- nettle
heparin increases and nettle decreases anticoagulation. Effect of interaction is not clear, use caution. Modify Therapy/Monitor Closely.
- nintedanib
nintedanib increases effects of heparin by anticoagulation. Use Caution/Monitor. Nintedanib is a VEGFR inhibitor, and may increase the risk of bleeding; monitor patients on full anticoagulation therapy; monitor closely for bleeding and adjust therapy as needed .
- nitroglycerin rectal
nitroglycerin rectal decreases effects of heparin by Other (see comment). Use Caution/Monitor. Comment: Although an interaction has been reported between IV heparin and nitroglycerin (resulting in a decrease in anticoagulant effect of heparin), the data are not consistent. If patients are to receive IV heparin and nitroglycerin concurrently, the anticoagulation status of the patient must be checked.
- olmesartan
heparin increases toxicity of olmesartan by Other (see comment). Use Caution/Monitor. Comment: Low molecular weight heparins may suppress adrenal aldosterone secretion, which can potentially cause hyperkalemia.
- omega 3 carboxylic acids
omega 3 carboxylic acids, heparin. Other (see comment). Use Caution/Monitor. Comment: Patients taking omega-3 acids and an anticoagulant or other drug affecting coagulation should be monitored periodically due to potential increased risk of bleeding.
- omega 3 fatty acids
omega 3 fatty acids, heparin. Other (see comment). Use Caution/Monitor. Comment: Patients taking omega-3-fatty acids and an anticoagulant or other drug affecting coagulation should be monitored periodically due to potential increased risk of bleeding. .
- oxaprozin
heparin and oxaprozin both increase anticoagulation. Modify Therapy/Monitor Closely.
- panax ginseng
heparin and panax ginseng both increase anticoagulation. Modify Therapy/Monitor Closely.
- parecoxib
heparin and parecoxib both increase anticoagulation. Modify Therapy/Monitor Closely.
- pau d'arco
heparin and pau d'arco both increase anticoagulation. Modify Therapy/Monitor Closely.
- pegaspargase
pegaspargase increases effects of heparin by pharmacodynamic synergism. Use Caution/Monitor. Increased risk of bleeding events.
- perindopril
heparin increases toxicity of perindopril by Other (see comment). Use Caution/Monitor. Comment: Low molecular weight heparins may suppress adrenal aldosterone secretion, which can potentially cause hyperkalemia.
- phenytoin
heparin increases levels of phenytoin by unknown mechanism. Use Caution/Monitor.
phenytoin, heparin. Other (see comment). Use Caution/Monitor. Comment: Hydantoin anticonvulsants increase anticoagulant effects at first, then decrease those effects with continued use (2+ wks). There are multiple mechanisms involved, including enzyme induction, plasma protein binding site competition, and additive effects on prothrombin time. - phytoestrogens
heparin and phytoestrogens both increase anticoagulation. Modify Therapy/Monitor Closely.
- piroxicam
heparin and piroxicam both increase anticoagulation. Modify Therapy/Monitor Closely.
- porfimer
heparin decreases effects of porfimer by pharmacodynamic antagonism. Use Caution/Monitor.
- potassium citrate/citric acid
heparin and potassium citrate/citric acid both increase serum potassium. Use Caution/Monitor.
- prednisolone
prednisolone, heparin. Other (see comment). Use Caution/Monitor. Comment: Corticosteroids may decrease anticoagulant effects by increasing blood coagulability; conversely, they may impair vascular integrity, thus increasing bleeding risk. Monitor INR closely.
- prednisone
prednisone, heparin. Other (see comment). Use Caution/Monitor. Comment: Corticosteroids may decrease anticoagulant effects by increasing blood coagulability; conversely, they may impair vascular integrity, thus increasing bleeding risk. Monitor INR closely.
- propafenone
propafenone increases effects of heparin by decreasing metabolism. Use Caution/Monitor.
- propylthiouracil
propylthiouracil decreases effects of heparin by pharmacodynamic antagonism. Use Caution/Monitor.
- quinapril
heparin increases toxicity of quinapril by Other (see comment). Use Caution/Monitor. Comment: Low molecular weight heparins may suppress adrenal aldosterone secretion, which can potentially cause hyperkalemia.
- ramipril
heparin increases toxicity of ramipril by Other (see comment). Use Caution/Monitor. Comment: Low molecular weight heparins may suppress adrenal aldosterone secretion, which can potentially cause hyperkalemia.
- reishi
heparin and reishi both increase anticoagulation. Modify Therapy/Monitor Closely.
- reteplase
heparin and reteplase both increase anticoagulation. Modify Therapy/Monitor Closely.
- rifabutin
rifabutin decreases levels of heparin by increasing metabolism. Use Caution/Monitor.
- rivaroxaban
rivaroxaban, heparin. Either increases effects of the other by anticoagulation. Use Caution/Monitor. Avoid concurrent use of rivaroxaban with other anticoagulants due to increased bleeding risk other than during therapeutic transition periods where patients should be observed closely. Monitor for signs/symptoms of blood loss.
- sacubitril/valsartan
heparin increases toxicity of sacubitril/valsartan by Other (see comment). Use Caution/Monitor. Comment: Heparin may suppress adrenal aldosterone secretion, which can potentially cause hyperkalemia.
- salicylates (non-asa)
heparin and salicylates (non-asa) both increase anticoagulation. Modify Therapy/Monitor Closely.
- salsalate
heparin and salsalate both increase anticoagulation. Modify Therapy/Monitor Closely.
- saw palmetto
saw palmetto increases toxicity of heparin by unspecified interaction mechanism. Use Caution/Monitor. May increase risk of bleeding.
- Siberian ginseng
heparin and Siberian ginseng both increase anticoagulation. Modify Therapy/Monitor Closely.
- spironolactone
spironolactone, heparin. Either increases toxicity of the other by serum potassium. Use Caution/Monitor. Both drugs may increase serum potassium levels.
- sulfasalazine
heparin and sulfasalazine both increase anticoagulation. Modify Therapy/Monitor Closely.
- sulindac
heparin and sulindac both increase anticoagulation. Modify Therapy/Monitor Closely.
- telmisartan
heparin increases toxicity of telmisartan by Other (see comment). Use Caution/Monitor. Comment: Low molecular weight heparins may suppress adrenal aldosterone secretion, which can potentially cause hyperkalemia.
- tenecteplase
heparin and tenecteplase both increase anticoagulation. Modify Therapy/Monitor Closely.
- ticagrelor
ticagrelor, heparin. Either increases effects of the other by anticoagulation. Use Caution/Monitor. Increased risk of bleeding during concomitant use of medications that increase potential for bleeding.
- tipranavir
tipranavir increases effects of heparin by pharmacodynamic synergism. Use Caution/Monitor. Tipranavir has mild antiplatelet activity that may incr bleeding risk.
- tolfenamic acid
heparin and tolfenamic acid both increase anticoagulation. Modify Therapy/Monitor Closely.
- tolmetin
heparin and tolmetin both increase anticoagulation. Modify Therapy/Monitor Closely.
- trandolapril
heparin increases toxicity of trandolapril by Other (see comment). Use Caution/Monitor. Comment: Low molecular weight heparins may suppress adrenal aldosterone secretion, which can potentially cause hyperkalemia.
- triamcinolone acetonide injectable suspension
triamcinolone acetonide injectable suspension, heparin. Other (see comment). Use Caution/Monitor. Comment: Corticosteroids may decrease anticoagulant effects by increasing blood coagulability; conversely, they may impair vascular integrity, thus increasing bleeding risk. Monitor INR closely.
- triamterene
triamterene, heparin. Either increases toxicity of the other by serum potassium. Use Caution/Monitor. Both drugs may increase serum potassium levels.
- triclofos
triclofos increases effects of heparin by unspecified interaction mechanism. Use Caution/Monitor.
- valsartan
heparin increases toxicity of valsartan by Other (see comment). Use Caution/Monitor. Comment: Low molecular weight heparins may suppress adrenal aldosterone secretion, which can potentially cause hyperkalemia.
- voclosporin
voclosporin and heparin both increase serum potassium. Use Caution/Monitor.
- vorapaxar
heparin, vorapaxar. Either increases effects of the other by anticoagulation. Use Caution/Monitor. Coadministration of anticoagulants, antiplatelets, or other drug affecting coagulation should be monitored periodically due to potential increased risk of bleeding.
- vortioxetine
vortioxetine and heparin both increase anticoagulation. Use Caution/Monitor.
- zanubrutinib
heparin, zanubrutinib. Either increases effects of the other by anticoagulation. Modify Therapy/Monitor Closely. Zanubrutinib-induced cytopenias increases risk of hemorrhage. Coadministration of zanubritinib with antiplatelets or anticoagulants may further increase this risk.
Minor (22)
- acetaminophen
acetaminophen increases effects of heparin by unknown mechanism. Minor/Significance Unknown.
- acetaminophen IV
acetaminophen IV increases effects of heparin by unknown mechanism. Minor/Significance Unknown.
- acetaminophen rectal
acetaminophen rectal increases effects of heparin by unknown mechanism. Minor/Significance Unknown.
- alprostadil intracavernous/urethral
alprostadil intracavernous/urethral increases effects of heparin by pharmacodynamic synergism. Minor/Significance Unknown.
- aprotinin
aprotinin increases effects of heparin by unspecified interaction mechanism. Minor/Significance Unknown.
- ceftaroline
ceftaroline increases effects of heparin by Other (see comment). Minor/Significance Unknown. Comment: Cephalosporins with a methylthiotetrazole (MTT) side ring (eg, cefotetan, cefoperazone) are more frequently associated with hypoprothrombinemic activity.
- chlorella
chlorella decreases effects of heparin by pharmacodynamic antagonism. Minor/Significance Unknown. Theoretical, due to vitamin K content.
- demeclocycline
demeclocycline increases effects of heparin by pharmacodynamic synergism. Minor/Significance Unknown.
- dexmethylphenidate
dexmethylphenidate increases effects of heparin by decreasing metabolism. Minor/Significance Unknown.
- doxycycline
doxycycline increases effects of heparin by pharmacodynamic synergism. Minor/Significance Unknown.
- glyburide
glyburide increases effects of heparin by unspecified interaction mechanism. Minor/Significance Unknown.
- mineral oil
mineral oil decreases levels of heparin by inhibition of GI absorption. Applies only to oral form of both agents. Minor/Significance Unknown.
- minocycline
minocycline increases effects of heparin by pharmacodynamic synergism. Minor/Significance Unknown.
- nitroglycerin IV
nitroglycerin IV decreases effects of heparin by unspecified interaction mechanism. Minor/Significance Unknown.
- oxytetracycline
oxytetracycline increases effects of heparin by pharmacodynamic synergism. Minor/Significance Unknown.
- protamine
protamine decreases effects of heparin by Other (see comment). Minor/Significance Unknown. Comment: This combination produces an insoluble salt.
- quinidine
quinidine increases effects of heparin by decreasing metabolism. Minor/Significance Unknown.
- serdexmethylphenidate/dexmethylphenidate
serdexmethylphenidate/dexmethylphenidate increases effects of heparin by decreasing metabolism. Minor/Significance Unknown.
- tetracycline
tetracycline increases effects of heparin by pharmacodynamic synergism. Minor/Significance Unknown.
- vasopressin
heparin decreases effects of vasopressin by pharmacodynamic antagonism. Minor/Significance Unknown.
- verteporfin
heparin decreases effects of verteporfin by pharmacodynamic antagonism. Minor/Significance Unknown.
- vitamin E
vitamin E, heparin. Mechanism: pharmacodynamic synergism. Minor/Significance Unknown. Vitamin E at RDA does not change INR in pts. on chronic warfarin therapy; megadoses (~10x RDA) may enhance anticoagulant effects in vitamin K deficient pts.
Adverse Effects
>10%
Heparin-induced thrombocytopenia, possibly delayed (10-30% )
Frequency Not Defined
Mild pain
Hemorrhage
Injection site ulcer (after deep SC injection)
Increased liver aminotransferase
Anaphylaxis
Immune hypersensitivity reaction
Osteoporosis (long-term, high-dose use)
Postmarketing Reports
Heparin resistance
Gasping syndrome in infants due to benzyl alcohol preservative
Hypersensitivity
Necrosis of skin at site of subcutaneous injection
Local irritation, erythema, mild pain, hematoma or ulceration following deep subcutaneous (intrafat) injection
Risk of serious adverse reactions in infants due to benzyl alcohol
Histamine-like reactions
Vascular disorders, including contusion, vasospastic reactions (including episodes of painful, ischemic, and cyanosed limbs)
Hyperkalemia
Delayed transient alopecia
Priapism
Rebound hyperlipemia on discontinuation of heparin
Warnings
Contraindications
History of pentosan polysulfate-induced thrombocytopenia (HIT) (with or without thrombosis)
Uncontrollable active bleeding state except when this is due to disseminated intravascular coagulation (DIC)
In whom suitable blood coagulation tests – eg, whole blood clotting time, partial thromboplastin time, etc, – cannot be performed at appropriate intervals (contraindication refers to full-dose heparin; there is usually no need to monitor coagulation parameters in patients receiving low-dose heparin)
Cases where the administration of sodium or chloride could be clinically detrimental (large volume heparin 2 unit/mL IV solutions only)
Known hypersensitivity to heparin or pork products
Cautions
Any risk factor for hemorrhage (eg, subacute bacterial endocarditis, blood dyscrasias, menorrhagia, dissecting aneurysm, major surgery, spinal anesthesia, hemophilia, GI ulcerative lesions, liver disease, impaired hemostasis)
When using a full-dose heparin regimen, adjust heparin dose based on frequent blood coagulation tests; if coagulation test is unduly prolonged or if hemorrhage occurs, heparin sodium should be discontinued promptly; periodic platelet counts, hematocrits are recommended during entire course of heparin therapy
Monitor therapy with aPTT
Heparin may prolong PT
Do not use heparin sodium injection as a catheter lock-flush product; heparin sodium injection is supplied in vials containing various strengths of heparin; these include vials containing a highly concentrated solution of 10,000 units in 1 mL, which have been mistaken for 1 mL low-concentration catheter lock-flush vials; Fatal hemorrhages have occurred due to medication errors; carefully examine all heparin products to confirm correct container choice prior to administration of drug
Geriatric dosing: Lower doses may be necessary; patients over 60 years may have enhanced serum levels and response compared with patients under 60 years receiving similar dosages
Heparin sodium may prolong one-stage prothrombin time; when heparin sodium is given with dicumarol or warfarin sodium, a period of at least 5 hr after last intravenous dose or 24 hr after last subcutaneous dose should elapse before blood is drawn if a valid prothrombin time is to be obtained
If preserved with benzyl alcohol, do not administer to neonates, infants, pregnant women, or breastfeeding women; benzyl alcohol has been associated with serious adverse events and death, particularly in pediatric patients (gasping syndrome)
Anticoagulant effect of heparin is enhanced by concurrent treatment with antithrombin III (human) in patients with hereditary antithrombin III deficiency; to reduce risk of bleeding, reduce heparin dose during concomitant treatment with antithrombin III (human)
Osteoporosis may occur with prolonged ( >6 months) use due to a reduction in mineral bone density
Some preparations may contain sulfite which may cause allergic reactions
Serious and fatal adverse reactions including “gasping syndrome” can occur in neonates and infants treated with benzyl alcohol-preserved drugs; consider combined daily metabolic load of benzyl alcohol from all sources including heparin sodium injection multiple-dose vials and other drugs containing benzyl alcohol hen prescribing multiple-dose vials in infants; minimum amount of benzyl alcohol at which toxicity may occur is not known
Significant elevations of aspartate aminotransferase (AST) and alanine aminotransferase (ALT) levels have occurred in patients who have received heparin; elevation of these enzymes in patients receiving heparin should be interpreted with caution; these elevations typically resolve upon heparin discontinuation
Heparin-induced thrombocytopenia and heparin-induced thrombocytopenia with thrombosis
- Heparin-induced thrombocytopenia (HIT) is a serious immune-mediated reaction resulting from irreversible aggregation of platelets; heparin-induced thrombocytopenia (HIT) is a serious immune-mediated reaction; HIT occurs in patients treated with heparin due to development of antibodies to a platelet Factor 4-heparin complex that induce in vivo platelet aggregation
- HIT may progress to development of venous and arterial thromboses, a condition referred to as heparin-induced thrombocytopenia with thrombosis (HITT) Thrombotic events may also be the initial presentation for HITT
- These serious thromboembolic events include deep vein thrombosis, pulmonary embolism, cerebral vein thrombosis, limb ischemia, stroke, myocardial infarction, mesenteric thrombosis, renal arterial thrombosis, skin necrosis, gangrene of the extremities that may lead to amputation, and possibly death
- Once HIT or HITT is diagnosed or strongly suspected, discontinue all heparin sources (including heparin flushes) and use an alternative anticoagulant
- Immune-mediated HIT is diagnosed based on clinical findings supplemented by laboratory tests confirming the presence of antibodies to heparin, or platelet activation induced by heparin
- Obtain platelet counts at baseline and periodically during heparin administration. A drop in platelet count greater than 50% from baseline is considered indicative of HIT
- Platelet counts begin to fall 5 to 10 days after exposure to heparin in heparin–naive individuals and reach a threshold by days 7 to 14
- In contrast, “rapid onset” HIT can occur very quickly (within 24 hours following heparin initiation), especially in patients with a recent exposure to heparin (eg, previous 3 months); thrombosis development shortly after documenting thrombocytopenia is a characteristic finding in almost half of all patients with HIT
- Monitor any degree of thrombocytopenia closely; if platelet count falls below 100,000/mm^3 or if recurrent thrombosis develops, promptly discontinue heparin, evaluate for HIT and HITT, and, if necessary, administer an alternative anticoagulant. HIT or HITT can occur up to several weeks after the discontinuation of heparin therapy
- Evaluate patients presenting with thrombocytopenia or thrombosis after discontinuation of heparin sodium for HIT or HITT
Thrombocytopenia
- Thrombocytopenia in patients receiving heparin has been reported at frequencies up to 30%; it can occur 2 to 20 days (average 5 to 9) following onset of heparin therapy
- Obtain platelet counts before and periodically during heparin therapy; mild thrombocytopenia (count greater than 100,000/mm3) may remain stable or reverse even if heparin is continued;
- However, monitor thrombocytopenia of any degree closely; if count falls below 100,000/mm3 or if recurrent thrombosis develops, promptly discontinue heparin, evaluate for HIT and HITT, and, if necessary, administer an alternative anticoagulant
Heparin resistance
- Increased resistance to heparin may be observed in patients with antithrombin deficiency, increased heparin clearance, elevations of heparin-binding proteins, elevations of in factor VIII and/or fibrinogen and may require doses >35,000 units/24hr to maintain therapeutic aPTT; frequently encountered in fever, thrombosis, thrombophlebitis, infections with thrombosing tendencies, myocardial infarction, cancer, in postsurgical patients, and patients with anti-thrombin deficiency
- Consider measurement of anti-thrombin levels if heparin resistance is suspected; monitor coagulation tests frequently in such patients; it may be necessary to adjust dose of heparin based on coagulation test monitoring, such as anti-Factor Xa levels and/or partial thromboplastin time
Hypersensitivity
- Hypersensitivity reactions with chills, fever and urticaria as the most usual manifestations and also asthma, rhinitis, lacrimation, and anaphylactoid reactions have been reported
- Patients with documented hypersensitivity to heparin should be given the drug only in clearly life-threatening situations; because heparin sodium in sodium chloride injection is derived from animal tissue, it should be used with caution in patients with a history of allergy to pork products
- This product contains sodium metabisulfite, a sulfite that may cause allergic-type reactions including anaphylactic symptoms and life-threatening or less severe asthmatic episodes in certain susceptible people; the overall prevalence of sulfite sensitivity in the general population is unknown and probably low; sulfite sensitivity is seen more frequently in asthmatic than in nonasthmatic people
Hyperkalemia
- Heparin can suppress adrenal secretion of aldosterone leading to hyperkalemia, particularly in patients with diabetes mellitus, chronic renal failure, pre-existing metabolic acidosis, a raised plasma potassium, or taking potassium sparing drugs; the risk of hyperkalemia appears to increase with duration of therapy but is usually reversible upon discontinuation of heparin
- Measure plasma potassium in patients at risk of hyperkalemia before starting heparin therapy and periodically in all patients treated for more than 5 days or earlier as deemed fit by the clinician
Hemorrhage
- Hemorrhage, including fatal events, has occurred; hemorrhage can occur at virtually any site in patients receiving heparin; avoid using heparin in presence of major bleeding, except when benefits of heparin therapy outweigh potential risks
- Hemorrhage can occur at virtually any site in patients receiving heparin; adrenal hemorrhage (with resultant acute adrenal insufficiency), ovarian hemorrhage, and retroperitoneal hemorrhage have occurred during anticoagulant therapy with heparin
- Higher incidence of bleeding reported in patients, particularly women, >60 years of age; an unexplained fall in hematocrit or fall in blood pressure should lead to serious consideration of hemorrhagic event
Pregnancy & Lactation
Pregnancy
There are no available data on heparin sodium injection use in pregnant women to inform a drug-associated risk of major birth defects and miscarriage; in published reports, in published reports, heparin exposure during pregnancy did not show evidence of increased risk of adverse maternal or fetal outcomes in humans
There are no known adverse outcomes associated with fetal exposure to preservative benzyl alcohol through maternal drug administration; however, preservative benzyl alcohol can cause serious adverse events and death when administered intravenously to neonates and infants
Animal data
- No teratogenicity, but early embryo-fetal death reported in animal reproduction studies with administration of heparin sodium to pregnant rats and rabbits during organogenesis at doses approximately 10 times maximum recommended human dose (MRHD) of 45,000 units/ day; consider benefits and risks of heparin sodium Injection for mother and possible risks to fetus when prescribing heparin sodium injection to pregnant women
Lactation
There is no information regarding presence of heparin sodium injection in human milk, effects on breastfed infant, or on milk production; developmental and health benefits of breastfeeding should be considered along with mother's clinical need for heparin sodium injection and potential adverse effects on breastfed infant from therapy or from the underlying maternal condition
If available, preservative-free heparin sodium injection is recommended when heparin therapy is needed during lactation; benzyl alcohol present in maternal serum is likely to cross into human milk and may be orally absorbed by a breastfed infant
There is no information regarding presence of heparin sodium injection in human milk, effects on breastfed infant, or on milk production; due to its large molecular weight, heparin is not likely to be excreted in human milk, and any heparin in milk would not be orally absorbed by a breastfed infant
Pregnancy Categories
A: Generally acceptable. Controlled studies in pregnant women show no evidence of fetal risk.
B: May be acceptable. Either animal studies show no risk but human studies not available or animal studies showed minor risks and human studies done and showed no risk. C: Use with caution if benefits outweigh risks. Animal studies show risk and human studies not available or neither animal nor human studies done. D: Use in LIFE-THREATENING emergencies when no safer drug available. Positive evidence of human fetal risk. X: Do not use in pregnancy. Risks involved outweigh potential benefits. Safer alternatives exist. NA: Information not available.Pharmacology
Mechanism of Action
Mechanism for low dose: Inactivates factor Xa and inhibits conversion of prothrombin to thrombin
Mechanism for high dose: Inactivates factors IX, X, XI, and XII and thrombin and inhibits conversion of fibrinogen to fibrin
Also inhibits activation of factor VIII
Absorption
Bioavailability: 22-40%
Onset: IV (immediate); SC (20-30 min)
Peak plasma time: 2-4 hr
Distribution
Protein bound: Extensive
Metabolism
Metabolized in the liver (partial) and reticuloendothelial system (partial)
Metabolites: None
Elimination
Half-life: 60-90 min average (longer at higher doses)
Dialyzable: No
Excretion: Urine
Administration
IV Incompatibilities
Additive
- Dobutamine
- Erythromycin
- Gentamicin
- Haloperidol
- Hydrocortisone
- Meperidine
- Morphine
- Vancomycin
Syringe
- Amiodarone
- Diazepam
- Erythromycin
- Gentamicin
- Haloperidol
- Meperidine
- Morphine(?)
- Vancomycin
Y-site
- Amiodarone
- Diazepam
- Dobutamine
- Gentamicin
- Haloperidol
- Vancomycin
Not spec
- Hydroxyzine
- Tetracycline
IV Compatibilities
Additive
- Aminophylline
- Ampho B
- Ampicillin
- Ca gluconate
- Clindamycin
- Dopamine
- Esmolol
- Furosemide
- Lidocaine
- Norepinephrine
- KCl
- Na bicarbonate
- Verapamil
- Vitamins B/C
Syringe
- Aminophylline
- Ampho B
- Ampicillin
- Atropine
- Cimetidine
- Clindamycin
- Dobutamine
- Dopamine
- Epinephrine
- Furosemide
- Lidocaine
- Morphine(?)
- Norepinephrine
- Na bicarbonate
- Verapamil
Y-site
- Aminophylline, ampicillin, atropine, Ca gluconate, cimetidine, clindamycin, dopamine, epinephrine, erythromycin, esmolol, furosemide, hydrocortisone, lidocaine, norepinephrine, meperidine, morphine, KCl, Na bicarbonate
IV Preparation
Recommended infusion concentration for most patients is 25,000 units in 500 mL D5W (50 units/mL premixed infusion solution)
IV Administration
IV injection may be given undiluted or diluted in 50-100 mL NS or D5W
Infusion: Dilute in NS, D5W, or other compatible fluid
Continuous IV therapy is preferred because intermittent IV therapy produces a higher incidence of bleeding abnormalities
Invert IV bag at least 6 times to ensure mixing and prevent pooling of medication
Use constant-rate IV infusion pump
Storage
Store heparin solutions at room temperature; do not freeze
Do not use if discolored/precipitates
Autoclavable
Images
| BRAND | FORM. | UNIT PRICE | PILL IMAGE |
|---|---|---|---|
| heparin lock flush (porcine) intravenous
-
|
100 unit/mL vial |  |
|
| heparin lock flush (porcine) intravenous
-
|
100 unit/mL vial | 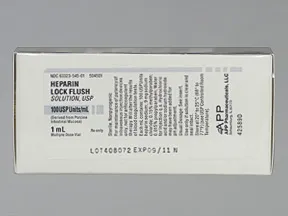 |
|
| heparin lock flush (porcine) intravenous
-
|
10 unit/mL vial |  |
|
| heparin lock flush (porcine) intravenous
-
|
10 unit/mL vial |  |
Copyright © 2010 First DataBank, Inc.
Patient Handout
heparin lock flush (porcine) intravenous
HEPARIN LOCK FLUSH-INJECTION
(HEP-a-rin)
COMMON BRAND NAME(S): Hep-Lock
USES: This medication is used to keep IV catheters open and flowing freely. Heparin helps to keep blood flowing smoothly and from clotting in the catheter by making a certain natural substance in your body (anti-clotting protein) work better. It is known as an anticoagulant.This form of heparin must not be used to treat or prevent blood clots in the body.Some products should not be used for newborns due to an increased risk of side effects. Check with your doctor or pharmacist for more details.
HOW TO USE: This medication is given by injection into the IV catheter as directed by your doctor. Do not inject this medication into the body.Heparin comes in many strengths. Serious (sometimes fatal) injuries have occurred when the wrong strength was used. Check that you are using the correct strength and dose before injecting this medication.Flush the catheter/line with normal saline before and after infusing drugs that interact with heparin such as doxorubicin, droperidol, ciprofloxacin, and mitoxantrone.If you are using this medication at home, learn all preparation and usage instructions from your health care professional. Before using, check this product visually for particles or discoloration. If either is present, do not use the liquid. Learn how to store and discard medical supplies safely.
SIDE EFFECTS: Remember that this medication has been prescribed because your doctor has judged that the benefit to you is greater than the risk of side effects. Many people using this medication do not have serious side effects.Although very unlikely, this medication can cause bleeding if its effect on your clotting proteins is too much. Tell your doctor right away if you develop any signs of serious bleeding, including unusual pain/swelling/discomfort, prolonged bleeding from cuts or gums, frequent nosebleeds, unusually heavy/prolonged menstrual periods, unusual/easy bruising, dark urine, black stools, severe headache, unusual dizziness.Some patients can have certain bad reactions to heparin (heparin-induced thrombocytopenia-HIT or heparin-induced thrombocytopenia and thrombosis-HITT). This can occur during treatment and up to several weeks after treatment with heparin has stopped. You should not use this drug again if you have this type of reaction with heparin.Get medical help right away if you have any very serious side effects, including: pain/loss of feeling in the arms/legs, change in color of the arms/legs, chest pain, trouble breathing, confusion, weakness on one side of the body, trouble speaking, vision changes.A very serious allergic reaction to this drug is rare. However, get medical help right away if you notice any symptoms of a serious allergic reaction, including: rash, itching/swelling (especially of the face/tongue/throat), severe dizziness, trouble breathing.This is not a complete list of possible side effects. If you notice other effects not listed above, contact your doctor or pharmacist.In the US -Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088 or at www.fda.gov/medwatch.In Canada - Call your doctor for medical advice about side effects. You may report side effects to Health Canada at 1-866-234-2345.
PRECAUTIONS: Before using heparin, tell your doctor or pharmacist if you are allergic to it; or to pork products; or to pentosan polysulfate sodium; or if you have any other allergies. This product may contain inactive ingredients (such as benzyl alcohol found in some brands), which can cause allergic reactions or other problems. Talk to your pharmacist for more details.Before using this medication, tell your doctor or pharmacist your medical history.Before having surgery, tell your doctor or dentist about all the products you use (including prescription drugs, nonprescription drugs, and herbal products).Tell your doctor if you are pregnant before using this medication.This medication does not pass into breast milk. Consult your doctor before breastfeeding.
DRUG INTERACTIONS: See also How to Use section.Drug interactions may change how your medications work or increase your risk for serious side effects. This document does not contain all possible drug interactions. Keep a list of all the products you use (including prescription/nonprescription drugs and herbal products) and share it with your doctor and pharmacist. Do not start, stop, or change the dosage of any medicines without your doctor's approval.This medication may interfere with certain lab tests (such as prothrombin time), possibly causing false test results. Make sure lab personnel and all your doctors know you use this drug.
OVERDOSE: If someone has overdosed and has serious symptoms such as passing out or trouble breathing, call 911. Otherwise, call a poison control center right away. US residents can call their local poison control center at 1-800-222-1222. Canada residents can call a provincial poison control center. Symptoms of overdose may include: easy/unusual bruising, easy/unusual bleeding (such as frequent nosebleeds), blood in urine, black stools.
NOTES: Not applicable.
MISSED DOSE: Not applicable.
STORAGE: Consult the product instructions and your pharmacist for storage details. Keep all medications away from children and pets.Do not flush medications down the toilet or pour them into a drain unless instructed to do so. Properly discard this product when it is expired or no longer needed. Consult your pharmacist or local waste disposal company.
Information last revised February 2024. Copyright(c) 2024 First Databank, Inc.
IMPORTANT: HOW TO USE THIS INFORMATION: This is a summary and does NOT have all possible information about this product. This information does not assure that this product is safe, effective, or appropriate for you. This information is not individual medical advice and does not substitute for the advice of your health care professional. Always ask your health care professional for complete information about this product and your specific health needs.
Formulary
Adding plans allows you to compare formulary status to other drugs in the same class.
To view formulary information first create a list of plans. Your list will be saved and can be edited at any time.
Adding plans allows you to:
- View the formulary and any restrictions for each plan.
- Manage and view all your plans together – even plans in different states.
- Compare formulary status to other drugs in the same class.
- Access your plan list on any device – mobile or desktop.