Overview
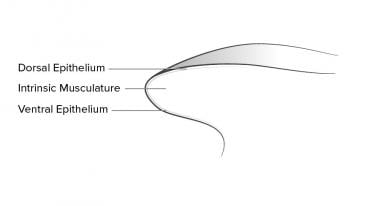
The tongue is a muscular organ that sits on the floor of the oropharynx. It is enveloped by mucosa and contains glands, sensory organs, and four pairs of extrinsic muscles. The tongue is essential for several important functions, including jaw articulation, taste, manipulation of food, swallowing, and the production of speech. See image below.
From anterior to posterior, the tongue has 3 surfaces: tip, body, and base. The tip is the highly mobile, pointed anterior portion of the tongue. Posterior to the tip lies the body of the tongue, which has dorsal (superior) and ventral (inferior) surfaces. For more information about the relevant anatomy, see Tongue Anatomy.
Injuries to the tongue are often treated in the emergency department or other acute care settings. A tongue laceration is often the result of a fall, seizure, psychogenic nonepileptic seizure, or other blunt or penetrating force mechanism. [1, 2, 3] Piercings, intoxication, and iatrogenic cause are also commonly associated with tongue injury. [4, 5, 6, 7, 8, 9, 10, 11, 12] Case studies have also implicated dystonia, self-mutilation, anesthesia, and exploding electronic cigarettes. [13, 14, 15, 16] Lacerations secondary to seizures are most often found to the side of the tongue. [17, 18]
Because of the tongue’s generous blood supply, most tongue lacerations do not become infected and many heal well without repair. The tongue hypertrophies to rebulk itself in a period of 6 months, so even loss of lateral tongue and tip often produces no permanent deficit. [19] However, repair is required when the injury has certain characteristics (see Indications).
The goals of laceration repair of the tongue are to attain adequate closure, stop bleeding, minimize complications, preserve mobility, and optimize articulation and deglutition.
While uncommon, practitioners should keep in mind that such injuries can be the result of physical abuse. [20, 21, 22] Oral and facial trauma occur in 50% of abused children. [23]
Indications
Characteristics of tongue lacerations that require repair include the following [24, 25, 26, 27] :
-
Bisecting wounds
-
Large flaps
-
Persistent bleeding
-
Wounds larger than 1-2 cm
-
Wounds to tip of tongue
-
Gaping wounds
-
U-shaped lacerations
-
Avulsion or amputation injuries (The tongue may be primarily closed if the defect is less than 30% of the tongue.)
Contraindications
Most tongue lacerations do not require sutures. Small flaps may be simply excised. Tongue lacerations in children are known to heal well without intervention. [28] Simple linear lacerations, especially if centrally located, heal with minimal risk of infection. Mouth protectors and tooth guards are also noninvasive modalities to assist tongue healing. [29]
Amputations or avulsions of more than 30% require a flap procedure, which should be performed by a specialist. [30, 31, 32]
Case reports have demonstrated the efficacy of using 2-octyl cyanoacrylate (Dermabond) for a pediatric tongue laceration. [19, 33, 34]
Anesthesia
The following anesthesia techniques may be used:
-
Topical anesthesia with lidocaine 4% on gauze for 5 minutes (See Anesthesia, Topical for more information.)
-
Local infiltration with lidocaine 1% (See Local Anesthetic Agents, Infiltrative Administration for more information.)
-
Lingual nerve block for the anterior two thirds of the tongue
-
Procedural sedation, especially in children
The pain associated with local anesthesia injections can be diminished if the practitioner uses a smaller-gauge needle and administers the anesthetic slowly. [35]
Equipment
Personal protective equipment is as follows:
-
Gloves
-
Face shield
-
Gown
Anesthesia equipment is as follows:
-
Lidocaine
-
Syringe, 10 mL
-
Needle, 27 gauge (ga)
-
Needle, 18 ga
-
Topical anesthetic
Irrigation equipment is as follows:
-
Saline or water
-
Syringe or irrigation device
-
Splash shield
-
Basin
Suture material is as follows:
-
Absorbable sutures (eg, plain gut, chromic gut), 4-0
-
Suture tray
-
Suture kit
-
Towel clip
Other equipment is as follows:
-
Side mouth gag (eg, Denhardt, Dingman)
-
Bite block
-
Towel clip
-
Gauze, 4 X 4 in
Positioning
The supine position is preferable for most repairs. The patient may sit in an ENT chair, if available.
Technique
Preparation
Once the patient is anesthetized, inspect the wound carefully. Some through-and-through lacerations may not be obvious without gentle probing.
Always check for chipped, missing, or mobile teeth in mouth injuries. Tooth fragments may be lodged inside the wound and, if not removed, may serve as a nidus for infection. Consider obtaining radiographic imaging to locate missing tooth fragments.
Intraoral wounds are prone to considerable contamination, and thorough irrigation is necessary.
The major difficulty in closing a tongue laceration is maintaining control of the area being sutured. To stabilize and hold in protrusion for repair, the tip of the tongue can be grasped with gauze or a towel clip or punctured and withdrawn with a large suture.
A bite block may be used to protect both the patient and physician, as necessary.
The recommendations on technique for repair are largely based on anecdotal literature. [19] Through-and-through lacerations can be closed in one, two, or three layers, as described below.
If the muscular layer is closed, bleeding is sufficiently controlled, and motor function is returned, then the superficial mucosal layers will heal rapidly.
The frequent movements of the tongue often untie the sutures. This can be avoided by burying the stitches or tying many knots. Avoid nylon in the mouth and tongue.
Three-layer technique
Using 4-0 absorbable sutures, first close the muscular mucosa.
The inferior mucosa is then sutured.
The repair is then extended up and around the lateral aspect of the tongue to close the superior mucosa. See images below.
Two-layer technique
Use one stitch to approximate half the thickness of the tongue superiorly.
Use another stitch to approximate half the thickness inferiorly.
Close the edges of the tongue.
Sutures do not have to be buried. See image below.
One-layer technique
Some suggest using a deep absorbable suture to close only the muscular layer, leaving the other layers open to heal without sutures.
This technique is successful because of the rapidly healing superficial mucosa. See image below.
Aftercare
After repair, the patient should eat a soft diet for 2-3 days.
Daily dilute peroxide or chlorohexidine mouth rinses may be used.
Healing occurs very rapidly.
Pearls
Update the patient's tetanus vaccination, if necessary.
Do not forget to evaluate for broken teeth and embedded foreign bodies.
The use of prophylactic antibiotics for tongue injury is controversial, but they should be considered in any contaminated wound. [36] A 2008 review on this topic concluded, "treatment decisions must be guided by clinical and scientific rationale rather than evidence-based medicine." [37] For more information, see Medscape article Human Bite Infections.
It may be suggested a patient use a mouthguard to prevent future lacerations if they are at high risk of reoccurrence or engaged in high-risk activities such as contact sports. [11, 38, 39, 40]
Complications
Complications can include the following:
-
Infection
-
Hemorrhage
-
Disfigurement
-
Impaired articulation
-
Impaired deglutition
-
Swelling
-
Airway compromise
In patients with coagulopathy or severe arterial bleeding, specialty consultation and interventional assistance for arterial ligature may be necessary. [41]
-
Bisected tongue.
-
Tongue anatomy in cross-section. The epithelial surfaces comprise the mucosa.
-
Cross-section: Three-layer closure technique.
-
Cross-section: Two-layer closure technique.
-
Cross-section: One-layer closure technique.
-
Closure of the superior mucosa of a bisected tongue.
-
Closure of the lateral aspect of the tongue.
-
Closure of the superior mucosa of a tongue laceration not involving the lateral margin.
-
Closure of the muscular mucosa as the first step of a three-layer technique.