Abstract
Objectives
This study compared the osseointegrative potential of a novel injection molded zirconia dental implant (Neodent Zi ceramic implant, test) and a commercially available titanium implant (Neodent Alvim implant, control) in terms of histomorphometrically derived bone-to-implant contact (BIC), first bone-to-implant contact (fBIC), and the ratio of bone area to total area (BATA) around the implant.
Materials and methods
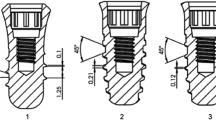
A total of 36 implants, 18 per individual test device, were implanted in a split-mouth arrangement in either side of the edentulous and fully healed mandible of 6 minipigs. Histomorphometric analysis of BIC, fBIC, and BATA were performed 8 weeks post implantation and subjected to statistical non-inferiority testing. Surface characteristics of both implant types were compared in terms of contact angle, surface topography, and elemental composition.
Results
BIC, fBIC, and coronal BATA values of test and control implants were statistically comparable and non-inferior. BIC values of 77.8 ± 6.9% vs. 80.7 ± 6.9% (p = 0.095) were measured for the test and control groups. fBIC lingual values were − 238 ± 328 μm compared with − 414 ± 511 μm (p = 0.121) while buccal values were − 429 ± 648 μm and − 588 ± 550 μm (p = 0.230) for the test and control devices, respectively. BATA in the apical segment was significantly higher in the test group compared with the control group (67.2 ± 11.8% vs. 59.1 ± 11.4%) (p = 0.0103). Surface topographies of both implant types were comparable. Surface chemical analysis indicated the presence of carbonaceous adsorbates which correlated with a comparable and predominantly hydrophobic character of the implants.
Conclusion
The results demonstrate that the investigated zirconia implants, when compared with a commercially available titanium implant, show equivalent and non-inferior bone integration, bone formation, and alveolar bone level maintenance. This qualifies the investigated zirconia implant as a potential candidate for clinical development.
Clinical relevance
This study investigated the osseointegration of a novel zirconia 2-piece dental implant prototype intended for clinical development. With the aim of translating this prototype into clinical development preclinical models, procedures and materials within this study have been selected as close to clinical practice and human physiological conditions as possible.







Similar content being viewed by others
References
Pieralli S, Kohal RJ, Jung RE, Vach K, Spies BC (2017) Clinical outcomes of zirconia dental implants: a systematic review. J Dent Res 96:38–46. https://doi.org/10.1177/0022034516664043
Andreiotelli M, Wenz HJ, Kohal R-J (2009) Are ceramic implants a viable alternative to titanium implants? A systematic literature review. Clin Oral Implants Res 20:32–47. https://doi.org/10.1111/j.1600-0501.2009.01785.x
Garvie RC, Hannink RH, Pascoe RT (1975) Ceramic steel? Nature 258:703–704. https://doi.org/10.1038/258703a0
Kohal R-J, Finke HC, Klaus G (2009) Stability of prototype two-piece zirconia and titanium implants after artificial aging: an in vitro pilot study. Clin Implant Dent Relat Res 11:323–329. https://doi.org/10.1111/j.1708-8208.2008.00116.x
Piconi C, Maccauro G (1999) Zirconia as a ceramic biomaterial. Biomaterials 20:1–25. https://doi.org/10.1016/S0142-9612(98)00010-6
Rimondini L, Cerroni L, Carrassi A, Torricelli P (2002) Bacterial colonization of zirconia ceramic surfaces: an in vitro and in vivo study. Int J Oral Maxillofac Implants 17:793–798
Kohal RJ, Knauf M, Larsson B, Sahlin H, Butz F (2012) One-piece zirconia oral implants: one-year results from a prospective cohort study. 1. Single tooth replacement. J Clin Periodontol 39:590–597. https://doi.org/10.1111/j.1600-051X.2012.01876.x
Oliva J, Oliva X, Oliva JD (2010) Five-year success rate of 831 consecutively placed zirconia dental implants in humans: a comparison of three different rough surfaces. Int J Oral Maxillofac Implants 25:336–344
Cionca N, Hashim D (2000) Mombelli A (2017) Zirconia dental implants: where are we now, and where are we heading? Periodontol 73:241–258. https://doi.org/10.1111/prd.12180
Jank S, Hochgatterer G (2016) Success rate of two-piece zirconia implants: a retrospective statistical analysis. Implant Dent 25:193–198. https://doi.org/10.1097/ID.0000000000000365
Schünemann FH, Galárraga-Vinueza ME, Magini R, Fredel M, Silva F, Souza JCM, Zhang Y, Henriques B (2019) Zirconia surface modifications for implant dentistry. Mater Sci Eng C Mater Biol Appl 98:1294–1305. https://doi.org/10.1016/j.msec.2019.01.062
Hafezeqoran A, Koodaryan R (2017) Effect of zirconia dental implant surfaces on bone integration: a systematic review and meta-analysis. Biomed Res Int 2017:1–12. https://doi.org/10.1155/2017/9246721
Moritz T, Lenk R (2009) Ceramic injection moulding: a review of developments in production technology, materials and applications. Powder Inject Mould Int 3:23–34
Yang YS, Yen Chen C (2016) Effect of injection molding and sintering behaviors on Y-TZP dental implants. J Phys Chem Biophys 6. https://doi.org/10.4172/2161-0398.1000220
Kim H-K, Woo KM, Shon W-J et al (2015) Comparison of peri-implant bone formation around injection-molded and machined surface zirconia implants in rabbit tibiae. Dent Mater J 34:508–515. https://doi.org/10.4012/dmj.2015-024
Park Y-S, Chung S-H, Shon W-J (2013) Peri-implant bone formation and surface characteristics of rough surface zirconia implants manufactured by powder injection molding technique in rabbit tibiae. Clin Oral Impl Res 24:586–591. https://doi.org/10.1111/j.1600-0501.2012.02468.x
Gahlert M, Röhling S, Wieland M, Sprecher CM, Kniha H, Milz S (2009) Osseointegration of zirconia and titanium dental implants: a histological and histomorphometrical study in the maxilla of pigs. Clin Oral Implants Res 20:1247–1253. https://doi.org/10.1111/j.1600-0501.2009.01734.x
Aboushelib MN, Salem NA, Taleb ALA, El Moniem NMA (2013) Influence of surface nano-roughness on osseointegration of zirconia implants in rabbit femur heads using selective infiltration etching technique. J Oral Implantol 39:583–590. https://doi.org/10.1563/AAID-JOI-D-11-00075
Chung SH, Kim H-K, Shon W-J, Park Y-S (2013) Peri-implant bone formations around (Ti,Zr)O2-coated zirconia implants with different surface roughness. J Clin Periodontol 40:404–411. https://doi.org/10.1111/jcpe.12073
Wilson TG, Miller RJ, Trushkowsky R, Dard M (2016) Tapered implants in dentistry: revitalizing concepts with technology: a review. Adv Dent Res 28:4–9. https://doi.org/10.1177/0022034516628868
Pippenger BE, Rottmar M, Kopf BS, Stübinger S, Dalla Torre FH, Berner S, Maniura-Weber K (2019) Surface modification of ultrafine-grained titanium: influence on mechanical properties, cytocompatibility, and osseointegration potential. Clin Oral Impl Res 30:99–110. https://doi.org/10.1111/clr.13396
Benlidayi ME, Gaggl A, Bürger H, Brandner C, Kurkcu M, Ünlügenç H (2011) Comparative study of the osseointegration of dental implants after different bone augmentation techniques: vascularized femur flap, non-vascularized femur graft and mandibular bone graft. Clin Oral Implants Res 22:594–599. https://doi.org/10.1111/j.1600-0501.2010.02013.x
Fuerst G, Gruber R, Tangl S et al (2003) Enhanced bone-to-implant contact by platelet-released growth factors in mandibular cortical bone: a histomorphometric study in minipigs. Int J Oral Maxillofac Implants 18:685–690
Kwon Y-S, Namgoong H, Kim J-H, Cho IH, Kim MD, Eom TG, Koo KT (2013) Effect of microthreads on removal torque and bone-to-implant contact: an experimental study in miniature pigs. J Periodontal Implant Sci 43:41–46. https://doi.org/10.5051/jpis.2013.43.1.41
Meng H-W, Chien EY, Chien H-H (2016) Dental implant bioactive surface modifications and their effects on osseointegration: a review. Biomark Res 4:24. https://doi.org/10.1186/s40364-016-0078-z
Mardas N, Dereka X, Donos N, Dard M (2014) Experimental model for bone regeneration in oral and cranio-maxillo-facial surgery. J Investig Surg 27:32–49. https://doi.org/10.3109/08941939.2013.817628
Berardini M, Trisi P, Sinjari B, Rutjes AWS, Caputi S (2016) The effects of high insertion torque versus low insertion torque on marginal bone resorption and implant failure rates: a systematic review with meta-analyses. Implant Dent 25:532–540. https://doi.org/10.1097/ID.0000000000000422
Trisi P, Todisco M, Consolo U, Travaglini D (2011) High versus low implant insertion torque: a histologic, histomorphometric, and biomechanical study in the sheep mandible. Int J Oral Maxillofac Implants 26:837–849
Ikar M, Grobecker-Karl T, Karl M, Steiner C (2020) Mechanical stress during implant surgery and its effects on marginal bone: a literature review. Quintessence Int 51(2):142–150.
Buser D, Nydegger T, Oxland T, Cochran DL, Schenk RK, Hirt HP, Snétivy D, Nolte LP (1999) Interface shear strength of titanium implants with a sandblasted and acid-etched surface: a biomechanical study in the maxilla of miniature pigs. J Biomed Mater Res 45(2):75–83
dos Santos MV, Elias CN, Cavalcanti Lima JH (2011) The effects of superficial roughness and design on the primary stability of dental implants: primary stability of dental implant. Clin Implant Dent Relat Res 13:215–223. https://doi.org/10.1111/j.1708-8208.2009.00202.x
Tabassum A, Meijer GJ, Wolke JGC, Jansen JA (2009) Influence of the surgical technique and surface roughness on the primary stability of an implant in artificial bone with a density equivalent to maxillary bone: a laboratory study. Clin Oral Implants Res 20:327–332. https://doi.org/10.1111/j.1600-0501.2008.01692.x
Manzano G, Herrero LR, Montero J (2014) Comparison of clinical performance of zirconia implants and titanium implants in animal models: a systematic review. Int J Oral Maxillofac Implants 29:311–320. https://doi.org/10.11607/jomi.2817
Wennerberg A, Albrektsson T, Andersson B, Krol JJ (1995) A histomorphometric and removal torque study of screw-shaped titanium implants with three different surface topographies. Clin Oral Implants Res 6:24–30. https://doi.org/10.1034/j.1600-0501.1995.060103.x
Palmquist A, Omar OM, Esposito M, Lausmaa J, Thomsen P (2010) Titanium oral implants: surface characteristics, interface biology and clinical outcome. J R Soc Interface 7. https://doi.org/10.1098/rsif.2010.0118.focus
Roehling S, Astasov-Frauenhoffer M, Hauser-Gerspach I, Braissant O, Woelfler H, Waltimo T, Kniha H, Gahlert M (2017) In vitro biofilm formation on titanium and zirconia implant surfaces. J Periodontol 88:298–307. https://doi.org/10.1902/jop.2016.160245
Gahlert M, Roehling S, Sprecher CM, Kniha H, Milz S, Bormann K (2012) In vivo performance of zirconia and titanium implants: a histomorphometric study in mini pig maxillae: in vivo performance of zirconia and titanium implants. Clin Oral Impl Res 23:281–286. https://doi.org/10.1111/j.1600-0501.2011.02157.x
Rupp F, Scheideler L, Olshanska N, de Wild M, Wieland M, Geis-Gerstorfer J (2006) Enhancing surface free energy and hydrophilicity through chemical modification of microstructured titanium implant surfaces. J Biomed Mater Res A 76:323–334. https://doi.org/10.1002/jbm.a.30518
Buser D, Broggini N, Wieland M, Schenk RK, Denzer AJ, Cochran DL, Hoffmann B, Lussi A, Steinemann SG (2004) Enhanced bone apposition to a chemically modified SLA titanium surface. J Dent Res 83:529–533. https://doi.org/10.1177/154405910408300704
Acknowledgments
The authors would like to thank Letitia Grace from the Swiss Tropical Institute (Basel) for the support of the statistical analysis and Novonexile AG (Switzerland) for the writing assistance and editorial support in the preparation of the manuscript.
Funding
This research was financially supported by Neodent and Straumann. Neodent is a daughter company of Straumann. This work may potentially lead to the development of products, in which Neodent and Straumann may have a business and/or financial interest. Neodent and Straumann therefore may be affected by the research reported in the enclosed paper.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr. Geninho Thomé declares that he is an employee of Neodent. Mrs. Rebecca Sandgren declares that she has no conflict of interest. Dr. Sergio Bernardes declares that he is an employee of Neodent. Dr. Larissa Trojan declares that she is an employee of Neodent. Dr. Nils Warfving declares that he has no conflict of interest. Dr. Benjamin Pippenger declares that he is an employee of Straumann. Mr. Benjamin Bellón declares that he is an employee of Straumann.
Ethical approval
This article does not contain any studies with human participants performed by any of the authors. Ethical standards related to the research of human subjects are not applicable. All applicable international, national, and/or institutional guidelines for the care and use of animals were followed. This study was conducted at the Biomedical Department of Lund University (Sweden) and approved by the local ethics committee of the university (M-192-14). The study was conducted in accordance with ISO 10993-6 “Biological evaluation of medical devices – Part 6 Tests for local effects after implantation guideline and recommendations.” This study adheres to the ARRIVE guidelines.
Informed consent
For this type of study, formal consent is not required.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 3470 kb)
Rights and permissions
About this article
Cite this article
Thomé, G., Sandgren, R., Bernardes, S. et al. Osseointegration of a novel injection molded 2-piece ceramic dental implant: a study in minipigs. Clin Oral Invest 25, 603–615 (2021). https://doi.org/10.1007/s00784-020-03513-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-020-03513-z