Abstract
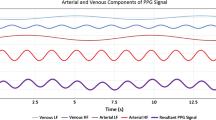
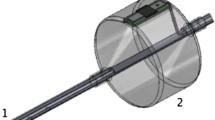
This study proposes to evaluate an innovative device consisting of an indwelling urinary catheter equipped with a photoplethysmography (PPG) sensor in contact with the urethral mucosa that provides a continuous index called urethral perfusion index (uPI). The goal of this study was to determine if the uPI could bring out tissue perfusion modifications induced by hypotension and vasopressors in a porcine model. Twelve piglets were equipped for heart rate, MAP, cardiac index, stroke volume index, systemic vascular resistance index and uPI monitoring. The animals were exposed to different levels of mean arterial pressure (MAP), ranging from low to high values. Friedman tests with a posteriori multiple comparison were performed and a generalized linear mixed model (GLMM) was used to assess the relationship between uPI and MAP. Urethral Perfusion Index and other haemodynamic parameters varied significantly at the different time-points of interest. There was a positive correlation between MAP and uPI below a specific MAP value, called dissociation threshold (DT). Above this threshold, uPI and MAP were negatively correlated. This relationship, assessed with the GLMM, yielded a significant positive fixed effect coefficient (+ 0.2, P < 0.00001) below the DT and a significant negative fixed effect (− 0.14, P < 0.00001) above DT. In an experimental setting, the PPG device and its index uPI permitted the detection of urethral mucosa perfusion alterations associated with hypotension or excessive doses of vasopressors. Further studies are needed to evaluate this device in a clinical context.






Similar content being viewed by others
Data Availability
All data generated or analysed during this study are included in this published article.
Abbreviations
- AC:
-
Alternate current
- CI:
-
Cardiac index
- CRI:
-
Intravenous constant rate infusion
- DAP:
-
Diastolic arterial pressure
- DC:
-
Direct current
- DT:
-
Dissociation threshold
- GLMM:
-
Generalized linear mixed model
- HR:
-
Heart rate,
- IM:
-
Intramuscular
- IV:
-
Intravenous
- MAC:
-
Minimal alveolar concentration
- MAP:
-
Mean arterial pressure
- NE:
-
Norepinephrine
- PPG:
-
Photoplethysmography
- PPV:
-
Pulse pressure variation
- SAP:
-
Systolic arterial pressure
- SVI:
-
Stroke volume index,
- SVRI:
-
Systemic vascular resistance index,
- SVV:
-
Stroke volume variation,
- uPI:
-
Urethral perfusion index
References
Trzeciak S, McCoy JV, Phillip Dellinger R, et al. Early increases in microcirculatory perfusion during protocol-directed resuscitation are associated with reduced multi-organ failure at 24 h in patients with sepsis. Intensive Care Med. 2008;34:2210–7. https://doi.org/10.1007/s00134-008-1193-6.
De Backer D, Creteur J, Dubois M-J, et al. Microvascular alterations in patients with acute severe heart failure and cardiogenic shock. Am Heart J. 2004;147:91–9. https://doi.org/10.1016/j.ahj.2003.07.006.
Jhanji S, Lee C, Watson D, et al. Microvascular flow and tissue oxygenation after major abdominal surgery: association with post-operative complications. Intensive Care Med. 2009;35:671–7. https://doi.org/10.1007/s00134-008-1325-z.
Otero RM, Nguyen HB, Huang DT, et al. Early goal-directed therapy in severe sepsis and septic shock revisited: concepts, controversies, and contemporary findings. Chest. 2006;130:1579–95. https://doi.org/10.1378/chest.130.5.1579.
Sakr Y, Dubois M-J, De Backer D, et al. Persistent microcirculatory alterations are associated with organ failure and death in patients with septic shock. Crit Care Med. 2004;32:1825–31. https://doi.org/10.1097/01.CCM.0000138558.16257.3F.
Annane D, Sebille V, Duboc D, et al. Incidence and prognosis of sustained arrhythmias in critically ill patients. Am J Respir Crit Care Med. 2008;178:20–5. https://doi.org/10.1164/rccm.200701-031OC.
Varpula M, Tallgren M, Saukkonen K, et al. Hemodynamic variables related to outcome in septic shock. Intensive Care Med. 2005;31:1066–71. https://doi.org/10.1007/s00134-005-2688-z.
Bateman RM, Walley KR. Microvascular resuscitation as a therapeutic goal in severe sepsis. Crit Care. 2005;9(Suppl 4):S27–32. https://doi.org/10.1186/cc3756.
Trzeciak S, Cinel I, Phillip Dellinger R, et al. Resuscitating the microcirculation in sepsis: the central role of nitric oxide, emerging concepts for novel therapies, and challenges for clinical trials. Acad Emerg Med. 2008;15:399–413. https://doi.org/10.1111/j.1553-2712.2008.00109.x.
Greenwood JC, Orloski CJ. End points of sepsis resuscitation. Emerg Med Clin North Am. 2017;35:93–107. https://doi.org/10.1016/j.emc.2016.09.001.
Ince C. Hemodynamic coherence and the rationale for monitoring the microcirculation. Crit Care. 2015;19(Suppl 3):S8. https://doi.org/10.1186/cc14726.
De Backer D, Ospina-Tascon G, Salgado D, et al. Monitoring the microcirculation in the critically ill patient: current methods and future approaches. Intensive Care Med. 2010;36:1813–25. https://doi.org/10.1007/s00134-010-2005-3.
Jacquet-Lagrèze M, Bonnet-Garin J-M, Allaouchiche B, et al. A new device for continuous assessment of gut perfusion: proof of concept on a porcine model of septic shock. Crit Care. 2014;18:R153. https://doi.org/10.1186/cc13992.
Dubin A, Pozo MO, Casabella CA, et al. Increasing arterial blood pressure with norepinephrine does not improve microcirculatory blood flow: A prospective study. Crit Care. 2009. https://doi.org/10.1186/cc7922.
Allen J. Photoplethysmography and its application in clinical physiological measurement. Physiol Meas. 2007;28:R1–39. https://doi.org/10.1088/0967-3334/28/3/R01.
Berardesca E, Lévêque J-L, Masson P, European Group for Efficacy Measurements on Cosmetics and Other Topical Products (EEMCO Group). EEMCO guidance for the measurement of skin microcirculation. Skin Pharmacol Appl Skin Physiol. 2002;15:442–56. https://doi.org/10.1159/000066451.
Budidha K, Abay TY, Kyriacou PA (2015) Investigation of photoplethysmography, laser Doppler flowmetry and near infrared spectroscopy during induced thermal stress. In: 2015 37th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC). IEEE, pp 6417–6420.
Pearce WH, Jones DN, Warren GH, et al. The use of infrared photoplethysmography in identifying early intestinal ischemia. Arch Surg. 1987;122:308–10. https://doi.org/10.1001/archsurg.1987.01400150062012.
Akl TJ, Wilson MA, Ericson MN, Coté GL. Intestinal perfusion monitoring using photoplethysmography. J Biomed Opt. 2013;18:87005. https://doi.org/10.1117/1.JBO.18.8.087005.
Abay TY, Kyriacou PA. Photoplethysmography for blood volumes and oxygenation changes during intermittent vascular occlusions. J Clin Monit Comput. 2018;32:447–55. https://doi.org/10.1007/s10877-017-0030-2.
Manohar M, Parks CM. Porcine systemic and regional organ blood flow during 1.0 and 1.5 minimum alveolar concentrations of sevoflurane anesthesia without and with 50% nitrous oxide. J Pharmacol Exp Ther. 1984;231:640–8. https://doi.org/10.1002/(ISSN)2052-1707.
Hecker KE, Baumert JH, Horn N, et al. Minimum anesthetic concentration of sevoflurane with different xenon concentrations in swine. Anesth Analg. 2003;97:1364–9. https://doi.org/10.1213/01.ane.0000081062.20894.d1.
Allaouchiche B, Duflo F, Tournadre JP, et al. Influence of sepsis on sevoflurane minimum alveolar concentration in a porcine model. Br J Anaesth. 2001;86:832–6.
Kelley KW, Curtis SE, Marzan GT, et al. Body surface area of female swine. J Anim Sci. 1973;36:927–30.
Clavijo JA, van Bastelaar J, Pinsky MR, et al. Minimally invasive real time monitoring of mitochondrial NADH and tissue blood flow in the urethral wall during hemorrhage and resuscitation. Med Sci Monit. 2008;14:175–82.
Mayevsky A, Tolmasov M, Kutai-Asis H, Mandelbaum M. Oxygen balance homeostasis and tissue metabolic score (TMS) of patients in emergency and critical care medicine. J Emerg Med Care. 2018;1:204.
Mayevsky A, Walden R, Pewzner E, et al. Mitochondrial function and tissue vitality: bench-to-bedside real-time optical monitoring system. J Biomed Opt. 2011;16:067004. https://doi.org/10.1117/1.3585674.
Swindle MM, Makin A, Herron AJ, et al. Swine as models in biomedical research and toxicology testing. Vet Pathol. 2012;49:344–56. https://doi.org/10.1177/0300985811402846.
Torri G, Casati A. Cardiovascular homeostasis during inhalational general anesthesia: a clinical comparison between sevoflurane and isoflurane. J Clin Anesth. 2000;12:117–22. https://doi.org/10.1016/S0952-8180(00)00123-9.
Ma D, Sapsed-Byrne SM, Chakrabarti MK, Whitwam JG. Effect of sevoflurane on spontaneous sympathetic activity and baroreflexes in rabbits. Br J Anaesth. 1998;80:68–72.
Alexander SPH, Mathie A, Peters JA. Guide to receptors and channels (GRAC), 5th edition. Br J Pharmacol. 2011;164:S1–S324. https://doi.org/10.1111/j.1476-5381.2011.01649_1.x.
Piehl M, Manning J, McCurdy S, et al. Pulse contour cardiac output analysis in a piglet model of severe hemorrhagic shock*. Crit Care Med. 2008;36:1189–95. https://doi.org/10.1097/CCM.0B013E31816592A3.
Bouattour K, Teboul J-L, Varin L, et al. Preload dependence is associated with reduced sublingual microcirculation during major abdominal surgery. Anesthesiol. 2019;130:541–9. https://doi.org/10.1097/ALN.0000000000002631.
LeDoux D, Astiz ME, Carpati CM, Rackow EC. Effects of perfusion pressure on tissue perfusion in septic shock. Crit Care Med. 2000;28:2729–32.
Talja M, Schröder T, Lehtola A, et al. Blood circulation in the urethra during hypovolemia–an experimental study. Urol Res. 1986;14:267–70.
Kroužecký A, Matějovič M, Raděj J, et al. Perfusion pressure manipulation in porcine sepsis: effects on intestinal hemodynamics. Physiol Res. 2006;55:527–33.
Rhodes A, Evans LE, Alhazzani W, et al. Surviving sepsis campaign: international guidelines for management of sepsis and septic shock: 2016. Intensive Care Med. Berlin Heidelberg: Springer; 2017. p. 304–377.
Boyd JH, Forbes J, Nakada T-A, et al. Fluid resuscitation in septic shock: a positive fluid balance and elevated central venous pressure are associated with increased mortality. Crit Care Med. 2011;39:259–65. https://doi.org/10.1097/CCM.0b013e3181feeb15.
Tigabu BM, Davari M, Kebriaeezadeh A, Mojtahedzadeh M. Fluid volume, fluid balance and patient outcome in severe sepsis and septic shock: A systematic review. J Crit Care. 2018;48:153–9. https://doi.org/10.1016/j.jcrc.2018.08.018.
Annane D, Ouanes-Besbes L, De Backer D, et al. A global perspective on vasoactive agents in shock. Intensive Care Med. 2018;44:833–46. https://doi.org/10.1007/s00134-018-5242-5.
Acknowledgements
Rémi Bonidal, Benjamin Delcroix and Dominique Falcon (Advanced Perfusion Diagnostics) for their technical support.
Funding
Funded research by APD (funds covered the material, the animals, the location of the veterinary operative room, the drugs and surgical and anaesthetic materials). APD did not take part in collection, analysis and interpretation of neither in the data or the writing of the manuscript. There was no clause of publication in the contract between our institution and APD.
Author information
Authors and Affiliations
Contributions
The first draft of the manuscript was written by MC. MC, MM, CP, J-YA and SJ performed the experimentation and data collection. SJ designed the study and performed the statistical analysis and helped to draft the manuscript. JB and BA contributed to the study design and coordination and helped to draft the manuscript. MM, CP, J-YA also revised the manuscript critically for important intellectual content. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflicts of interest
B. Allaouchiche: Consultant for APD, The other authors declare that they have no conflict of interest.
Ethics approval
The study was approved by our local ethical board for animal research and care (Vet Agro Sup, Marcy l’Etoile, France, authorization number: 1819) in accordance with European regulations (Directive 2010/63/EU).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Cardinali, M., Magnin, M., Bonnet-Garin, JM. et al. A new photoplethysmographic device for continuous assessment of urethral mucosa perfusion: evaluation in a porcine model. J Clin Monit Comput 35, 585–598 (2021). https://doi.org/10.1007/s10877-020-00515-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-020-00515-w