Abstract
Background
Application of the immunomodulatory selective cytopheretic device (SCD) to enhance renal replacement therapy and improve outcomes of acute kidney injury in pediatric patients is impeded by safety concerns. Therapy using a pediatric hemodialysis system could overcome these limitations.
Methods
Yucatan minipigs (8–15 kg) with induced septic shock underwent continuous hemodiafiltration with the CARPEDIEM™ pediatric hemodialysis system using regional citrate anticoagulation (RCA) with or without SCD (n = 5 per group). Circuit function plus hemodynamic and hematologic parameters were assessed for 6 h.
Results
SCD was readily integrated into the CARPEDIEM™ system and treatment delivered for 6 h without interference with pump operation. SCD-treated pigs maintained higher blood pressure (p = 0.009) commensurate with lesser degree of lactic acidosis (p = 0.008) compared to pigs only receiving hemodiafiltration. Renal failure occurred in untreated pigs while urine output was sustained with SCD therapy. Neutrophil activation levels and ss-SOFA scores at 6 h trended lower in the SCD-treated cohort.
Conclusions
SCD therapy under RCA was safely administered using the CARPEDIEM™ pediatric hemodialysis system for up to 6 h and no circuit compatibility issues were identified. Sepsis progression and organ dysfunction was diminished with SCD treatment in this model supportive of therapeutic benefit of this immunomodulatory therapy.
Impact
SCD therapy with regional citrate anticoagulation has the potential to be administered safely to patients weighing <20 kg using the Carpediem renal replacement therapy platform.
Use of a renal replacement therapy platform designed specifically for neonates/infants overcomes safety concerns for delivery of SCD treatment in this population.
SCD therapy using the Carpediem renal replacement therapy platform retained the suggestive efficacy seen in larger children and adults to reduce organ injury and dysfunction from sepsis.
Similar content being viewed by others
Introduction
Acute kidney injury (AKI) is common in critically ill children and is associated with increased morbidity and mortality.1 Primary kidney disease accounts for <10% of all AKI in hospitalized children receiving renal replacement therapy (RRT), thus, AKI results most often from another organ illness or its treatment.2,3 Similar to sepsis, AKI contributes to a systemic inflammatory response syndrome (SIRS), and in children with sepsis, AKI is independently associated with higher mortality.4 Clinical manifestations of SIRS and sepsis are due to dysregulation of the host response to infection or injury rather than direct consequences of the invading pathogen or tissue damage.5,6 Central to this initial immunologic response is activation of leukocytes, predominantly neutrophils, and the microvascular endothelium leading to increased vascular permeability with fluid leakage from intravascular space to the interstitium with resulting cardiovascular collapse, ischemic damage to vital organs, and multiorgan dysfunction (MOD).7,8 Organ injury during SIRS is compounded by aggregation of activated neutrophils within microvasculature of vital organs and release of additional inflammatory mediators and destructive enzymes from these defensive cells.9
Since activated leukocytes are central to the pathogenesis and progression of SIRS, therapeutic approaches to limit deleterious effects of these cells are being sought. The selective cytopheretic device (SCD) is an immune cell-processing system that has been evaluated in three separate clinical trials in adults10,11,12 and recently in pediatric patients up to 22 years of age.13,14 The adult studies have demonstrated that SCD treatment is associated with a reduction in mortality and improved renal outcomes in intensive care unit (ICU) patients with AKI and MODs compared to continuous RRT (CRRT) alone. The pediatric study demonstrated that SCD was safe and had a potential benefit with respect to morbidity and mortality compared to a historical registry (although we cannot make efficacy claims). SCD therapy is comprised of tubing, connectors, and a cartridge containing thousands of bundled fibers of a synthetic biomimetic membrane that adheres and sequesters activated leukocytes from systemic circulation. Administered with regional citrate anticoagulation (RCA) to reduce ionized calcium (iCa) levels to <0.4 mM to inhibit the coagulation cascade, the low iCa environment within the SCD produces an inhibitory effect on activated neutrophils,10 thereby combining the SCD effect to simultaneously sequester and deactivate circulating leukocytes. This method of cell processing results in systemic immunomodulatory effects and amelioration of inflammatory sequelae.10,15,16,17
The SCD is readily utilized with conventional CRRT circuits but the extracorporeal circuit blood volume with the SCD, which in its smallest available version, has a prime volume of 117 mL, currently restricts application to patients >20 kg body weight. For SCD technology to be safely applied to the more diminutive pediatric population, the size of the extracorporeal circuit needs to be reduced and a CRRT pump system designed for treatment of small children employed. The Cardio-Renal Pediatric Dialysis Emergency Machine (CARPEDIEM™, Medtronic Inc., Minneapolis, MN) has recently been approved by the United States Food and Drug Association (FDA) to provide CRRT for children weighing between 2.5 and 10 kg. This system allows increased precision in hemodialysis with circuit prime volumes as low as 32 mL (HD 015, 0.15 m2 hemofilter), potentially offering a suitable platform to enable application of SCD therapy to the smallest of patients.18
Herein we aimed to evaluate the feasibility and safety of SCD therapy when administered using the CARPEDIEM™ system with its low volume blood lines and hemofilters under RCA in a miniature pig model of septic shock. If proven safe with retained efficacy signals in preclinical studies, planning will begin for evaluation of SCD therapy with the CARPEDIEM™ pump system within an FDA-approved clinical trial.
Methods
Animal model
Male and female Yucatan miniature pigs (n = 10) aged 2–4 months, weighing 8–15 kg were ventilated under anesthesia with isoflurane in 100% oxygen, propofol (10 mg/kg/h intravenous (IV)) and fentanyl (0.025–0.05 mg/kg/h IV). Arterial and Swan-Ganz pulmonary arterial catheters (Edwards Lifesciences, Irvine, CA) connected to pressure transducers were inserted and a Foley catheter was placed by cystotomy. An 8Fr pediatric double lumen hemodialysis catheter (Teleflex, Wayne, PA) was inserted into a femoral vein for connection to the extracorporeal circuit. Procedures were performed under protocols approved by the institutional animal care and use committee at the University of Michigan and adhered to principles stated in the Guide for the Care and Use of Laboratory Animals.19
Septic shock was induced by instillation of 1.0 × 1011 of Escherichia coli CFU (ATCC® 19138) per kg of body weight into the peritoneal cavity. Initiated at the time of bacterial infusion, continuous venovenous hemodiafiltration (CVVHD) with RCA was provided throughout a 6-h study period. Pigs were assigned to 1 of the 2 treatment cohorts; a control group, in which CVVHD was performed using the standard CARPEDIEM™ tubing set, and a SCD-treated group, whereby the SCD cartridge was incorporated into the CRRT circuit post hemofilter (n = 5 per group). The extracorporeal circuit for each group is depicted in Fig. 1. Identical volume resuscitation with 80 mL/kg crystalloid and 20 mL/kg colloid (HESPAN 6% hydroxyethyl starch, Braun Medical, Bethlehem, PA) plus Cefazolin (1 g IV) was provided to both groups during the first 2 h after bacterial inoculation. Maintenance fluids at 10/mL/kg/h were provided thereafter. Epinephrine (0.1 mg IV bolus) was administered if mean arterial pressure (MAP) dropped below 30 mmHg, but otherwise cardiovascular compromise was allowed to progress without vasopressor or inotropic support. Animals were euthanized at the end of the 6-h treatment period or upon cardiovascular collapse (MAP < 20 mmHg).
a depicts the control circuit and b depicts the circuit with incorporation the SCD. For both cohorts, the CARPEDIEM® circuit was first primed using the automated priming procedure. To deliver SCD therapy, the SCD and its specialized tubing connectors were manually primed with saline separately and then the device was inserted post hemofilter using aseptic technique, in a manner similar to performing a filter exchange. Regional citrate anticoagulation was provided by infusion of ACD-A inline at the connection of the catheter to circuit tubing. If needed, calcium chloride infusion was provided by a separate venous catheter. SCD selective cytopheretic device, UF ultrafiltrate, RF replacement fluid.
Continuous venovenous hemodiafiltration
A CARPEDIEM™ blood line set with a 0.25 m2 hemofilter (HD 025, Medtronic, Minneapolis, MN) was used for CVVHD with a bicarbonate-based, calcium-free dialysate (Braun Medical, Bethlehem, PA), which was aseptically divided into 2 L aliquots for compatibility with the CARPEDIEM™ scales. The dialysate contained 136 mEq/L sodium, 2 mEq/L potassium, 1.5 mEq/L magnesium, 107.5 mEq/L chloride, and 32 mEq/L bicarbonate. Treatment parameters were standardized using an extracorporeal blood flow rate of 40 mL/min and dialysate flow of 600 mL/h. Ultrafiltration was maintained at 10 mL/h/kg with fluid replacement at an equal volume for hours 1–3 and a net gain of 10 mL/kg/h after hour 3 using a balanced crystalloid solution in addition to the citrate anticoagulant.
The circuit was primed with 0.9% NaCl and then immediately prior to use re-primed with whole blood from Yorkshire pigs banked at 4 °C for up to 10 days in 450 mL blood bags containing CPD-A (Baxter, Deerfield, IL). Using a protocol adapted from Cincinnati children’s hospital, the donor blood bag was attached to the access line and hemodiafiltration using the prescribed treatment settings was performed for 6–8 min with the venous line attached to a waste bag. Sodium bicarbonate (30 mL) was infused pre hemofilter over 2 min. Once filled with blood, the circuit was then paused for connection to the animal. Administration of calcium gluconate (50 mg/kg) upon starting extracorporeal circulation prevented hypotension or cardiac arrest with the rapid transfusion.
RCA of the circuit during therapy was performed using acid citrate dextrose solution (ACD-A, Baxter, Deerfield, IL) at 40-80 mL/h administered at the catheter connection with the arterial limb of the blood line to achieve iCa levels in the circuit blood of <0.4 mmol/L. A 2% calcium chloride solution was infused into a separate venous catheter as needed to compensate for iCa bound by citrate, targeting maintenance of systemic iCa levels between 0.9 and 1.5 mmol/L. Systemic and circuit iCa levels were monitored using an iSTAT handheld analyzer (Abbott Laboratories, Abbott Park, IL)
Selective cytopheretic device
The SCD is a cartridge with an inlet and outlet for blood flow, containing bundled porous polysulfone hollow fibers. Blood flow is directed to the extracapillary space of the SCD allowing interaction of blood cells with the membrane surface in a low shear environment before being returned to the animal. SCD used for these studies had a calculated fill volume of 117 mL and outer membrane surface area of 0.98 m2 and were supplied by SeaStar Medical, Inc. (Denver, CO). For the treated cohort, the SCD was placed in the extracorporeal circuit post-hemofilter. Special blood line connectors from the blood port of the hemofiltration cartridge to the side port of the SCD from the SCD to the venous blood line were required.
Sampling
Arterial blood gas analysis was performed hourly (iSTAT, Abbott Laboratories, Abbott Park, IL). Complete blood counts (0, 2, 4, and 6 h) comprised of erythrogram, leukogram, and platelet counts were measured with a veterinary analyzer (Hemavet, Drew Scientific, Miami Lakes, FL). Serum chemistries (0, 3, and 6 h) were determined by routine methods at a commercial laboratory (IDEXX BioAnalytics, Columbia, MO).
Fluorescein isothiocyanate-conjugated anti-porcine CD11R3 antibody (clone: 2F4/11 Bio-Rad Laboratories, Hercules, CA) was added to 100 µL pre-chilled hourly blood. Red cells were then lysed and the leukocytes fixed by addition of Becton-Dickinson’s FACS lysing solution (349202, Franklin lakes, NJ). Cells were collected by centrifugation and resuspended in phosphate-buffered saline for cytometric analysis. CD11R3 expression was quantitatively assessed as mean fluorescent intensity (MFI) with an Attune flow cytometer (Avantor, Radnor, PA). At conclusion of therapy, SCD cartridges were removed from the extracorporeal circuit, rinsed, and adherent cells were eluted and quantified as described previously.10
Hemodynamic measurements
Pressure transducer readings displayed on a patient monitor (Marquette Solar 8000 GE Healthcare, Chicago, IL) were recorded every 15 min. Cardiac output was determined hourly using a modified carbon dioxide Fick method with arterial and central venous blood samples and carbon dioxide elimination measured using a Capnostat® CO2 sensor with the Non-Invasive Cardiac Output monitor, NICO2® model 7300 (Novametrix Medical Systems, Wallingford, CT). Body surface area derived using a formula for miniature swine20 was used to calculate cardiac index (CI) for normalization across the weight range.
Sequential Organ Failure Assessment (SOFA) scoring
Sepsis progression was quantitated using a version of the SOFA scoring system previously modified for use in swine models.21 Five organ systems (respiration, cardiovascular, coagulation, liver, and renal) are scored and then summated for an overall swine-specific SOFA (ss-SOFA) score. Each organ system is scored from 0 (normal) to 4 (greatest degree of compromise) with a maximum ss-SOFA score of 20. Relevant data were collected at 0, 3, and 6 h (Fig. 4). Platelet counts collected at hour 2 were used for the hour 3 ss-SOFA. If animals were euthanized prior to hour 6, the last observed scores were carried forward for the hour 6 ss-SOFA.
Statistics
Group comparisons were made by fitting a mixed model as implemented in GraphPad Prism 8.0, which uses a compound symmetry covariance matrix and is fit using Restricted Maximum Likelihood. This method allows for analysis and interpretation similar to repeated-measures analysis of variance even when some values are missing. The Geisser–Greenhouse correction was applied for lack of sphericity. Point comparisons used Student’s t test, paired or unpaired, as appropriate. Statistical significance was defined as p ≤ 0.05.
Results
Extracorporeal circuit
The SCD was integrated into the CARPEDIEM™ system with only minor modifications to the tubing set required. To deliver SCD therapy, the SCD and its connectors were manually primed with saline separately and then, using the principles of a routine filter exchange, were aseptically inserted into the CARPEDIEM™ tubing set, which had already been saline primed according to the instructions for use. Completed circuits (with or without SCD) were then primed with blood immediately prior to connection to the animal. Blood priming, used in both cohorts, was necessary to prevent dilutional anemia and loss of circulating volume with the increased extracorporeal prime volume of the SCD, which resulted in a total circuit volume of approximately 158 mL.
RCA, a requirement for SCD therapy, was performed based upon published clinical protocols employing a relatively fixed citrate to blood flow rate ratio22 in children. RCA in both groups and was effective in reducing blood iCa levels in the CRRT circuit to <0.4 mmol/L and circuit patency was maintained throughout treatment in all but one untreated animal. This pig had sudden cardiac arrest at hour 5 causing the blood pump to stop automatically with the change in line pressure. Despite rapid revival of the animal using epinephrine and chest compressions, high circuit pressures prevented continuation of CRRT. The animal succumbed before a new circuit could be initiated. Systemic iCa levels prior to starting CRRT averaged 1.38 ± 0.05 mmol/L (range 1.32–1.47 mmol/L). A reduction in systemic iCa levels compared to baseline was seen during RCA in both cohorts; however, across all subjects, values remained between 0.93 and 1.44 mmol/L throughout the treatment period and calcium chloride infusion was not necessary in any animal as iCa levels stabilized after a nadir at hour 1 (Table 1).
Cardiovascular parameters
Intraperitoneal administration of E. coli bacteria produced signs of cardiovascular dysfunction associated with acute sepsis, including an early hyperdynamic phase followed a rapid, profound, and ultimately fatal decline in arterial blood pressure (Fig. 2). Significant hemodynamic declines were evident within 2 h after bacteria administration and were progressive with only the modest prescribed volume resuscitation and sparing use of epinephrine. Table 1 provides a summary of relevant vital measurements. Three animals in the untreated cohort required administration of 1–2 doses of epinephrine to support survival beyond 4 h but only one of these animals was successfully maintained to the 6 h endpoint. One pig in the SCD-treated group received one dose of epinephrine 5.5 h into the study period. Average survival time of the control group was 5.1 ± 0.89 h, with 3 of the 5 animals expiring prior to the end of the 6-h observation period at hours 4, 4.5, and 5. Survival time for the SCD group averaged 5.8 ± 0.27 h with 3 animals completing the study and 2 animals expiring just shy of the final time point at 5.5 h. Depicted in Table 1 and Fig. 2, the SCD-treated group had significantly higher arterial blood pressures than that of the control group. Significant timepoints for MAP were at 2 h (75 ± 4 vs 61 ± 4 mmHg, p = 0.036), 3 h (68 ± 6 vs 47 ± 5 mmHg, p = 0.021), and 4 h (52 ± 6 vs 35 ± 5 mmHg, p = 0.049). Observed in the control group but not in the SCD-treated animals, an acute increase in pulmonary artery pressures and pulmonary vascular resistance resulted in reduced cardiac output for the control group at hour 1. Cardiac index was significantly higher (1.25 ± 0.16 vs. 0.32 ± 0.01 L/min, p < 0.03) in the SCD-treated group compared to controls at this timepoint (Fig. 2). Limited by the constraints of the modified Fick calculation, cardiac output could not be calculated at every time point in every animal when hemodynamics or carbon dioxide elimination readings were not sufficiently stable. At hour 2, only 2 untreated pigs had usable measurements and no cardiac output measurements were able to be obtained for SCD-treated pigs, therefore this timepoint was not used in the analysis. All subsequent timepoints indicate that the SCD group had no worse reductions in CI than the control group. The trend in mean pulmonary arterial pressure (mPAP) was different for the treatment cohorts (Table 1). mPAP in the control group drastically increased from baseline of 23 ± 3 to 36 ± 4 mmHg by hour 1, followed by modest decline. The SCD group at hour 1 had a significantly lower mPAP (24 ± 2 mmHg, p < 0.03) than the controls followed by a gradual increase through hour 4. Pulmonary vascular resistance remained lower for the SCD-treated group than the controls during sepsis (p = 0.049). Likely reflective of these vasoactive changes, arterial partial pressure of oxygen (PaO2) declined in several animals, primarily within the control group, leading to clearly separate trajectories for the group averages of this parameter. This difference did not reach statistical significance. A discernible decline in arterial pH manifested in the control group with ensuing shock, the difference between groups was significant at hour 4 with a pH of 7.226 ± 0.035 in the control group vs 7.414 ± 0.047 for the SCD group, p = 0.013. Correspondingly, serum lactate in the control group was significantly higher at hour 4 (6.11 ± 1.55 mmol/L vs 2.62 ± 0.13, p = 0.03) and hour 5 (8.22 ± 0.03 mmol/L vs 3.72 ± 0.96, p = 0.04) than the SCD group.
Cardiac index (a), mean arterial blood pressure (MAP) (b), arterial partial pressure of oxygen (PaO2) (c), serum lactate (d), arterial pH (e), and cumulative urine output (f) are reported as mean ± SEM. SCD group is indicated by square data points and control group is indicated by circle data points. Horizontal axis units are hours since bacterial infusion.
Hematologic parameters
The change in hematocrit was assessed as a quantitative measure of systemic vascular capillary leak. After an initial decrease in both groups with the identical volume resuscitation, hematocrit progressively increased over the study for the control group, while the SCD group’s values plateaued just below baseline (Fig. 3). This difference was not statistically significant. Both groups experienced a decrease in circulating white blood cell (WBC) counts from baseline (Fig. 3). Control animals demonstrated a significant decrease in WBC counts at hour 2 (p = 0.002) and hour 4 (p = 0.006), whereas SCD-treated animals were only different at hour 4 (p = 0.044). Though decreased, average platelet counts were not different from baseline in SCD-treated animals at any timepoint but a significant reduction from a baseline value of 531 ± 161 K/µL was noted at hour 2 (248 ± 84 K/µL, p = 0.009) and hour 4 (160 ± K/µL, p = 0.016) in control animals.
Hematocrit (a), platelets (b), white blood cell count (WBC) (c), and neutrophil activation as expressed as CD11R3 mean fluorescence intensity (MFI) (d), reported as mean ± SEM. SCD group is indicated by square data points and control group is indicated by circle data points. Horizontal axis units are hours since bacterial infusion.
The level of neutrophil activation was quantified by measuring the amount of CD11R3 on circulating neutrophils. CD11R3, the ortholog of human CD11b, is a cell surface glycoprotein of the alpha integrin family that is instrumental in cell binding to activated endothelium to promote leukocyte extravasation.23 As shown in Fig. 3, the MFI of CD11R3 of neutrophils in systemic circulation increased with onset of sepsis, overall trending higher for the control group, with the SCD group having lower neutrophil activation at hour 4 (MFI 7,466 ± 1253) compared to control (MFI 13,114 ± 1622, p = 0.026).
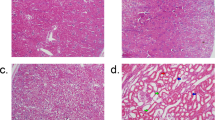
To determine the amount and type of activated leukocytes adhered along the SCD membranes, SCD cartridges were processed to elute adhered cells off the membrane at the end of the study. The average number of cells eluted per SCD was 6.08 ± 2.96 × 107 cells. The distribution of eluted cells was 83 ± 2% neutrophils and 10 ± 3% monocytes with <5% lymphocytes. MFI of CD11R3 on eluted cells exceeded the highest MFI observed on circulating cells in each of the SCD-treated pigs and ranged from 12,242 to 25,046 (data not shown).
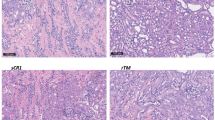
ss-SOFA scoring to assess sepsis progression
Figure 4 depicts the average ss-SOFA score per group at baseline, hour 3, and hour 6. At baseline, there was no difference in ss-SOFA scores between groups. Scores were increased at each subsequent timepoint in this rapidly progressive sepsis model. The average ss-SOFA score for the SCD group at hour 6 was 5.60 ± 1.21 points, trending lower than the 8.80 ± 1.20 points the control group averaged at the same timepoint (p = 0.10). Table 2 details the averaged parameters used to create the ss-SOFA scores for each group. ss-SOFA scores remained low for the liver and renal systems in this model and probably underestimated renal dysfunction since creatinine was continuously removed from systemic circulation via CVVHD. Suggesting preservation of renal function and trending towards significance, the cumulative urine output in the SCD group was greater than the control group (p = 0.10) with all but one of the control animals developing anuric renal failure.
Discussion
This study utilizing a miniature pig (pediatric) sepsis model and a recently FDA-approved pediatric CRRT pump system, the Medtronic Cardio-Renal Pediatric Dialysis Emergency Machine (CARPEDIEM™), serves as an initial step in tailoring SCD therapy to clinical application for small pediatric patients for treatment during sepsis and AKI. The CARPEDIEM™ blood pump is unique in its safety profile featuring a small rotor that allows for lower blood flow rates with reduced risk of clotting and scales accurate to within 1 g/h to help prevent fluid imbalance. Importantly, the CARPEDIEM™ system conserves required blood prime volume with hemofilter and combined tubing sets of just 32 mL (HCD 015) to 41 mL (HCD 025), compared to 52–90 mL for conventional pediatric tubing sets with an additional 7–45 mL for conventional pediatric hemofilters. In this testing, it was determined that the SCD currently utilized in pediatric clinical trials can be integrated into CARPEDIEM™ tubing sets, while not interfering with the proper function of the pump system and continuous performance of the pump system over several hours of SCD therapy was demonstrated. RCA, which is a requirement of SCD therapy, can be safely administered with CARPEDIEM™ circuits using established clinical protocols, achieving desired reductions in circuit iCa to prevent clotting within the circuit with minimal impact on systemic calcium levels as citrate is readily removed by dialysis. Only one test circuit had a clinically recognized clotting issue. This control circuit did not contain the SCD. Thus, the risk of clotting within the circuit did not appear to be increased with use of SCD, even during a period of hemodynamic instability that may cause fluctuations in circuit pressures and flow. The absolute circulating platelet counts observed during the experimental period suggest that the SCD membrane did not have a negative impact on coagulation. In fact, therapeutic benefit may be evidenced by the less substantial reduction from baseline for the SCD-treated pigs compared to the control animals during sepsis, which often causes coagulopathy. Within this 6-h study, which was designed to evaluate safety and feasibility of incorporation of SCD into this new dialysis platform, we did not observe any difference in leukocyte kinetics between groups. This is not surprising given the short observation period compounded by the fact that several animals did not survive to the endpoint. A trend for a reduced activation levels of circulating leukocytes and the binding of highly activated neutrophil and monocytes to the SCD was, however, observed, which is an important mechanistic action resulting in the systemic immunomodulatory effects associated with SCD therapy.10,15,16,17 Longer durations of SCD therapy in a similar sepsis model10 have previously demonstrated modulation of leukocyte recruitment, with WBC returning toward baseline without rebound neutrophilia and reduction in appearance of immature cells, a pattern that has also been observed with clinical use.10,15,16,17
Comparison of pigs treated with the SCD and pigs not given SCD therapy in this septic shock model demonstrated the potential benefit of SCD therapy during sepsis and SIRS similar to that observed in prior work using a larger pig model,10 with SCD-treated animals experiencing better maintenance of hemodynamic parameters, maintenance of renal function, and a reduced level of leukocyte activation. The larger porcine model has been predictive of clinical efficacy. In the current study, tempering of lactic acidosis and a trend for lower average ss-SOFA scores for SCD-treated pigs in four out of five assessed categories suggests that SCD therapy mitigated the progression of septic shock. Unfortunately, AKI was difficult to assess in this short study as serum creatinine levels were not elevated in either group. Renal protection by mitigation of AKI or through preservation of renal perfusion was, however, indicated by the maintenance of urine output of pigs in the SCD-treated group. Improved survival, which has been noted in the previous work, was also suggested for SCD-treated pigs but not clearly demonstrated with the termination of studies at 6 h.
In the current studies, blood priming of the circuit was performed because of the increased circuit volume of the SCD, which, at approximately 117 mL for the smallest SCD currently available, resulted in circuit volumes exceeding 15% of the estimated blood volume for subjects with a body weight of 8–15 kg. While not a clinical necessity when using the CARPEDIEM™ system alone, blood prime was performed in both groups to minimize variables when trying to compare cohorts. This model depicts the current clinical scenario for SCD therapy as blood prime would be indicated for patients of similar size. Recent FDA approval of the SCD as a Humanitarian Use Device for pediatric AKI and sepsis has prompted development efforts toward manufacture of smaller SCD cartridges specifically for pediatric application with the goal of reducing fill volumes while maintaining an effective membrane surface area, potentially obviating the need for blood prime.
Limitations of this study include the relatively small group sizes and the inability to maintain a proportion of these animals to the end of the observation period that limited its statistical power. However, this timeframe and the number of subjects appeared adequate for the main purposes of demonstrating the feasibility and safety of integrating the SCD into the CARPEDIEM™ circuit. The number of subjects did also provide a signal for retained efficacy to impact severity and progression of sepsis with group differences observed in several vital parameters. While we did not encounter technical issues running the circuit or observe any clotting tendency, SCD therapy was only maintained for 6 h in this test system. Thus, not all potential complications may have had time to manifest. Protein deposition, for example, could cause progressively increasing pressures within the device that may impact circuit function. Current IDE approvals require replacement of the SCD every 24 h during treatment. RCA, which has been demonstrated to increase hemofilter longevity,24 has already been successfully used in the clinic to maintain SCD functionality, even at low flows for 24 h in pediatric applications without increased risk of device-related serious adverse events. The manufacturer’s instructions to replace the CARPEDIEM™ tubing set after 24 h of use further minimizes the risk of circuit malfunction over time. We chose circuit settings and treatment parameters suitable for patients weighing 8–15 kg but testing of circuit function with the SCD over the full range of the CARPEDIEM™ settings, which comprises blood pump flow rates from 2 to 50 mL/min, is advisable prior to clinical application. We therefore acknowledge that this study is not necessarily comprehensive but provides meaningful evidence to enable further pursuit of this platform application for SCD therapy to infants. Use of Yucatan miniature pigs to mimic the desired size of a pediatric patient meant that these animals were used at early adult life stages and were not immature animals themselves. Thus, this model may not replicate pediatric-specific responses to AKI or sepsis or the compatibility of SCD therapy with immature immune systems. Nevertheless, the SCD has been clinically tested in pediatric patients 2–22 years of age and as small as 20 kg in a phase 1 safety trial (ClinicalTrials.gov Identifier: NCT02820350) with positive results and a recently FDA-approved trial to investigate safety in patients weighing 10–20 kg is underway (NCT04869787). Results from the preclinical work described here will be considered as potential supporting data for an IDE amendment to enable enrollment of patients of body weight of 8–10 kg for SCD therapy using the CARPEDIEM™ CRRT system, using FDA discretion for a stepwise evaluation for safety in incrementally smaller-sized children as has been done previously.
To date, the ease of incorporation of the SCD into the standard CRRT approach for critically ill adults as well as children weighing >20 kg has allowed for an excellent safety profile and compelling efficacy impact as demonstrated in clinical evaluation of SCD therapy with citrate anticoagulation in ICU patients with AKI and multiorgan failure. The recent FDA approval of the CARPEDIEM™ system as well as development of other CRRT platforms specifically for support of neonates and infants represent a promising pathway to expand therapeutic application of SCD therapy to the smallest of patients with AKI and other inflammatory conditions, a population historically underserved by advancements in renal replacement technology.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Kaddourah, A., Basu, R. K., Bagshaw, S. M., Goldstein, S. L. & AWARE Investigators. Epidemiology of acute kidney injury in critically ill children and young adults. N. Engl. J. Med. 376, 11–20 (2017).
Goldstein, S. L. Advances in pediatric renal replacement therapy for acute kidney injury. Semin. Dial. 24, 187–191 (2011).
Symons, J. M. et al. Demographic characteristics of pediatric continuous renal replacement therapy: a report of the prospective pediatric continuous renal replacement therapy registry. Clin. J. Am. Soc. Nephrol. 2, 732–738 (2007).
Basu, R. K. et al. Identification of candidate serum biomarkers for severe septic shock-associated kidney injury via microarray. Crit. Care 15, R273 (2011).
Hotchkiss, R. S. & Karl, I. E. The pathophysiology and treatment of sepsis. N. Engl. J. Med. 348, 138–150 (2003).
Schouten, M., Wiersinga, W. J., Levi, M. & van der Poll, T. Inflammation, endothelium, and coagulation in sepsis. J. Leukoc. Biol. 83, 536–545 (2008).
Humes, H. D., Fissell, W. H. & Weitzel, W. F. The bioartificial kidney in the treatment of acute renal failure. Kidney Int. 61, S121–S125 (2002).
Humes, H. D. Bioartificial kidney for full renal replacement therapy. Semin. Nephrol. 20, 71–82 (2000).
Brown, K. A. et al. Neutrophils in development of multiple organ failure in sepsis. Lancet 368, 157–169 (2006).
Ding, F. et al. A biomimetic membrane device that modulates the excessive inflammatory response to sepsis. PLoS ONE 6, e18584 (2011).
Tumlin, J. A. et al. The effect of the selective cytopheretic device on acute kidney injury outcomes in the intensive care unit: a multicenter pilot study. Semin. Dial. 26, 616–623 (2013).
Tumlin, J. A. et al. A multi-center, randomized, controlled, pivotal study to assess the safety and efficacy of a selective cytopheretic device in patients with acute kidney injury. PLoS ONE 10, e0132482 (2015).
Goldstein, S. L. et al. Use of the selective cytopheretic device in critically ill children. Kidney Int. Rep. 6, 775–784 (2021).
Selewski, D. T. et al. Immunomodulatory device therapy in a pediatric patient with acute kidney injury and multiorgan dysfunction. Kidney Int. Rep. 2, 1259–1264 (2017).
Pino, C. J., Westover, A. J., Johnston, K. A., Buffington, D. A. & Humes, H. D. Regenerative medicine and immunomodulatory therapy: insights from the kidney, heart, brain, and lung. Kidney Int. Rep. 3, 771–783 (2018).
Pino, C. J. et al. Cell-based approaches for the treatment of systemic inflammation. Nephrol. Dial. Transpl. 28, 296–302 (2013).
Pino, C. J., Yevzlin, A. S., Tumlin, J. & Humes, H. D. Cell-based strategies for the treatment of kidney dysfunction: a review. Blood Purif. 34, 117–123 (2012).
Goldstein, S. L. et al. Survival of infants treated with ckrt: comparing adapted adult platforms with the carpediem. Pediatr. Nephrol. 37, 667–675 (2021).
National Research Council. Guide for the Care and Use of Laboratory Animals: Eighth Edition (The National Academies Press, 2011).
Swindle, M. M., Makin, A., Herron, A. J., Clubb, F. J. Jr. & Frazier, K. S. Swine as models in biomedical research and toxicology testing. Vet. Pathol. 49, 344–356 (2012).
Waterhouse, A. et al. Modified clinical monitoring assessment criteria for multi-organ failure during bacteremia and sepsis progression in a pig model. Adv. Crit. Care Med. 1, 002 (2018).
Yessayan, L. et al. Regional citrate anticoagulation “non-shock” protocol with pre-calculated flow settings for patients with at least 6 l/hour liver citrate clearance. BMC Nephrol. 22, 244 (2021).
Dominguez, J. et al. Workshop studies on monoclonal antibodies in the myeloid panel with Cd11 specificity. Vet. Immunol. Immunopathol. 80, 111–119 (2001).
Zarbock, A. et al. Effect of regional citrate anticoagulation vs systemic heparin anticoagulation during continuous kidney replacement therapy on dialysis filter life span and mortality among critically ill patients with acute kidney injury: a randomized clinical trial. JAMA 324, 1629–1639 (2020).
Funding
This work was generously funded through the Frankel Innovation Initiative at the University of Michigan and private donation by Stuart and Maxine Frankel and the National Institutes of Health (NIH) Small Business for Innovative Research (SBIR) program through the National Center for Advancing Translational Sciences (NCATS) award R44TR001324-02A1.
Author information
Authors and Affiliations
Contributions
Study design: K.A.J., C.J.P., S.L.G., H.D.H. Data collection and manuscript preparation: K.A.J., C.J.P., G.C., S.K.K. Approval: K.A.J., S.L.G., H.D.H.
Corresponding author
Ethics declarations
Competing interests
K.A.J., C.J.P., S.K.K., and H.D.H. are employees of Innovative BioTherapies (IBT). H.D.H. is a shareholder, an officer, and a director of IBT. K.A.J., C.J.P., and H.D.H. are shareholders of SeaStar Medical, Inc. C.J.P. and H.D.H. are inventors on patents held by SeaStar Medical. H.D.H. is a scientific advisor, a director, and a consultant to SeaStar Medical. S.L.G. receives consulting fees from SeaStar Medical. G.C. has no competing interests. SeaStar Medical was not involved in the execution of this study.
Ethics approval and consent to participate
No patient consent was required for this pre-clinical research study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Johnston, K.A., Pino, C.J., Chan, G. et al. Immunomodulatory therapy using a pediatric dialysis system ameliorates septic shock in miniature pigs. Pediatr Res 93, 89–96 (2023). https://doi.org/10.1038/s41390-022-02061-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-022-02061-4