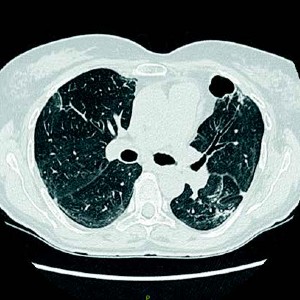
Acinetobacter cavitations in COVID-19 interstitial pneumonia: a case report and review of the literature
Accepted: 10 March 2023
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Acinetobacter baumannii is commonly known to cause infection in immunocompromised patients. During COVID-19 pandemic, outbreaks of multidrug-resistant organisms, including Acinetobacter, have been well documented in acute care hospitals, particularly among critically ill patients. In the case reported, a woman was admitted to our ICU because of a severe COVID-19 pneumonia. During her stay, she worsened due to Acinetobacterrelated lung cavitations and only after proper antibiotic treatment she eventually recovered. To our knowledge, very few cases have been reported pointing to Acinetobacter as a causal agent for the acute development of lung cavities, especially in COVID-19 patients.
How to Cite

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
PAGEPress has chosen to apply the Creative Commons Attribution NonCommercial 4.0 International License (CC BY-NC 4.0) to all manuscripts to be published.

 https://doi.org/10.4081/amsa.2023.10
https://doi.org/10.4081/amsa.2023.10 


