Dosing & Uses
Dosage Forms & Strengths
capsule
- 324mg
Malaria
Uncomplicated (P falciparum)
- 648 mg PO q8hr x 7 days
Chloroquine-resistant (P falciparum)
- 648 mg PO q8hr x 3-7 days with concomitant tetracycline, doxycycline, or clindamycin
Chloroquine-resistant (P vivax)
- 648 mg PO q8hr x 3-7 days with concomitant doxycycline (or tetracycline) and PO primaquine
Babesiosis (Off-label)
648 mg PO q8hr x 7 days, with concomitant PO or IV clindamycin
Dosage Modifications
Renal impairment
- Severe: 648 mg PO once, then 324 mg PO q12hr
Hepatic impairment
- Mild or moderate (Child-Pugh A or B): No dosage adjustment required; monitor closely
- Severe (Child-Pugh C): Do not administer
Limitations of use
Not approved for
- Treatment of severe or complicated P. falciparum malaria
- Prevention of malaria
- Treatment or prevention of nocturnal leg cramps
Dosage Forms & Strengths
capsule
- 324mg
Malaria
Uncomplicated (P falciparum)
Chloroquine-resistant (P falciparum)
- 30 mg/kg/day PO divided TID x3-7 days, with concomitant doxycycline, tetracycline or clindamycin
- Should not exceed the usual adult PO dosage.
Chloroquine-resistant (P vivax)
- 30 mg/kg/day PO TID x 3–7 days, with concomitant doxycyline & PO primaquine
- Should not exceed the usual adult PO dosage.
Babesiosis (Off-label)
25 mg/kg/day PO divided TID x7 days, with concomitant oral clindamycin
Interactions
Interaction Checker
No Results

Contraindicated
Serious - Use Alternative
Significant - Monitor Closely
Minor

Contraindicated (5)
- dronedarone
dronedarone will increase the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Contraindicated. Although quinine levels are not significantly increased, combination is contraindicated because of potential for both drugs to prolong QT interval
dronedarone and quinine both increase QTc interval. Contraindicated. - eliglustat
quinine increases levels of eliglustat by affecting hepatic enzyme CYP2D6 metabolism. Contraindicated. If coadministered with strong or moderate CYP2D6 inhibitors, reduce eliglustat dose from 84 mg BID to 84 mg once daily in extensive and intermediate metabolizers; eliglustat is contraindiated if strong or moderate CYP2D6 inhibitors are given concomitantly with strong or moderate CYP3A inhibitors.
- lefamulin
lefamulin will increase the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Contraindicated. Lefamulin is contraindicated with CYP3A substrates know to prolong the QT interval.
- pimozide
pimozide and quinine both increase QTc interval. Contraindicated.
- thioridazine
thioridazine and quinine both increase QTc interval. Contraindicated.
Serious - Use Alternative (101)
- adagrasib
adagrasib will increase the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Avoid or Use Alternate Drug. Avoid coadministration of adagrasib, a CYP3A4 inhibitor, with sensitive CYP3A substrates unless otherwise recommended in the prescribing information for these substrates.
adagrasib, quinine. Either increases effects of the other by QTc interval. Avoid or Use Alternate Drug. Each drug prolongs the QTc interval, which may increased the risk of Torsade de pointes, other serious arryhthmias, and sudden death. If coadministration unavoidable, more frequent monitoring is recommended for such patients. - afatinib
quinine increases levels of afatinib by P-glycoprotein (MDR1) efflux transporter. Avoid or Use Alternate Drug. Reduce afatinib daily dose by 10 mg if not tolerated when coadministered with P-gp inhibitors.
- alfuzosin
alfuzosin and quinine both increase QTc interval. Avoid or Use Alternate Drug.
- amisulpride
amisulpride and quinine both increase QTc interval. Avoid or Use Alternate Drug. ECG monitoring is recommended if coadministered.
- antithrombin alfa
quinine increases effects of antithrombin alfa by unknown mechanism. Avoid or Use Alternate Drug.
- antithrombin III
quinine increases effects of antithrombin III by unknown mechanism. Avoid or Use Alternate Drug.
- apalutamide
apalutamide will decrease the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Avoid or Use Alternate Drug. Coadministration of apalutamide, a strong CYP3A4 inducer, with drugs that are CYP3A4 substrates can result in lower exposure to these medications. Avoid or substitute another drug for these medications when possible. Evaluate for loss of therapeutic effect if medication must be coadministered. Adjust dose according to prescribing information if needed.
- argatroban
quinine increases effects of argatroban by unknown mechanism. Avoid or Use Alternate Drug.
- aripiprazole
aripiprazole and quinine both increase QTc interval. Avoid or Use Alternate Drug.
- artemether
artemether and quinine both increase QTc interval. Avoid or Use Alternate Drug.
- asenapine transdermal
asenapine transdermal and quinine both increase QTc interval. Avoid or Use Alternate Drug.
- atomoxetine
atomoxetine and quinine both increase QTc interval. Avoid or Use Alternate Drug.
- atracurium
quinine increases effects of atracurium by pharmacodynamic synergism. Contraindicated. Risk of resp. depression.
- bemiparin
quinine increases effects of bemiparin by unknown mechanism. Avoid or Use Alternate Drug.
- bivalirudin
quinine increases effects of bivalirudin by unknown mechanism. Avoid or Use Alternate Drug.
- bremelanotide
bremelanotide will decrease the level or effect of quinine by Other (see comment). Avoid or Use Alternate Drug. Bremelanotide may slow gastric emptying and potentially reduces the rate and extent of absorption of concomitantly administered oral medications. Avoid use when taking any oral drug that is dependent on threshold concentrations for efficacy. Interactions listed are representative examples and do not include all possible clinical examples.
- brigatinib
brigatinib will decrease the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Avoid or Use Alternate Drug. Brigatinib induces CYP3A4 in vitro. Coadministration with CYP3A4 substrates, particularly those with a narrow therapeutic index, can result in decreased concentrations and loss of efficacy. If unable to avoid coadministration, monitor CYP3A4 substrate levels and adjust dose as needed.
- buprenorphine
buprenorphine and quinine both increase QTc interval. Avoid or Use Alternate Drug.
- buprenorphine buccal
buprenorphine buccal and quinine both increase QTc interval. Avoid or Use Alternate Drug.
- buprenorphine subdermal implant
buprenorphine subdermal implant and quinine both increase QTc interval. Avoid or Use Alternate Drug.
- buprenorphine transdermal
buprenorphine transdermal and quinine both increase QTc interval. Avoid or Use Alternate Drug.
- buprenorphine, long-acting injection
buprenorphine, long-acting injection and quinine both increase QTc interval. Avoid or Use Alternate Drug.
- ceritinib
ceritinib and quinine both increase QTc interval. Avoid or Use Alternate Drug.
ceritinib will increase the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Avoid or Use Alternate Drug. - chloroquine
chloroquine increases toxicity of quinine by QTc interval. Avoid or Use Alternate Drug.
- cisatracurium
quinine increases effects of cisatracurium by pharmacodynamic synergism. Contraindicated. Risk of resp. depression.
- colchicine
quinine will increase the level or effect of colchicine by P-glycoprotein (MDR1) efflux transporter. Avoid or Use Alternate Drug. Avoid use of colchicine with P-gp inhibitors. If coadministration is necessary, decrease colchicine dose or frequency as recommended in prescribing information. Use of any colchicine product in conjunction with P-gp inhibitors is contraindicated in patients with renal or hepatic impairment.
- dalteparin
quinine increases effects of dalteparin by unknown mechanism. Avoid or Use Alternate Drug.
- dapsone topical
quinine, dapsone topical. unspecified interaction mechanism. Avoid or Use Alternate Drug. Avoid coadministration of dapsone topical with oral dapsone or antimalarial medications because of the potential for hemolytic reactions.
- desflurane
desflurane and quinine both increase QTc interval. Avoid or Use Alternate Drug.
- donepezil
donepezil and quinine both increase QTc interval. Avoid or Use Alternate Drug.
- doxepin
doxepin and quinine both increase QTc interval. Avoid or Use Alternate Drug.
- edoxaban
quinine will increase the level or effect of edoxaban by P-glycoprotein (MDR1) efflux transporter. Avoid or Use Alternate Drug. Dose adjustment may be required with strong P-gp inhibitors. DVT/PE treatment: Decrease dose to 30 mg PO once daily. NVAF: No dose reduction recommended
- efavirenz
efavirenz and quinine both increase QTc interval. Avoid or Use Alternate Drug.
- eliglustat
eliglustat and quinine both increase QTc interval. Contraindicated.
- encorafenib
encorafenib and quinine both increase QTc interval. Avoid or Use Alternate Drug. Encorafenib is associated with dose-dependent QTc interval prolongation. Avoid with drugs known to prolong QT interval.
- enoxaparin
quinine increases effects of enoxaparin by unknown mechanism. Avoid or Use Alternate Drug.
- entrectinib
quinine and entrectinib both increase QTc interval. Avoid or Use Alternate Drug.
- erdafitinib
erdafitinib, quinine. Other (see comment). Avoid or Use Alternate Drug. Comment: Avoid coadministration during initial dosing adjustment period (ie, first 21 days). Increases in serum phosphate levels are a pharmacodynamic effect of FGFR inhibition. Serum phosphate binders may obscure decisions regarding initial dosage increase.
erdafitinib, quinine. affecting hepatic/intestinal enzyme CYP3A4 metabolism. Avoid or Use Alternate Drug. Avoid coadministration with erdafitinib and sensitive CYP3A4 substrates with narrow therapeutic indices. Erdafitinib may altered plasma concentrations of CYP3A4 substrates, leading to either loss of activity or increased toxicity of the substrate.
erdafitinib will increase the level or effect of quinine by P-glycoprotein (MDR1) efflux transporter. Avoid or Use Alternate Drug. If coadministration unavoidable, separate administration by at least 6 hr before or after administration of P-gp substrates with narrow therapeutic index.
quinine will increase the level or effect of erdafitinib by affecting hepatic enzyme CYP2C9/10 metabolism. Avoid or Use Alternate Drug. If coadministration of a strong CYP2C9 inhibitors is unavoidable, closely monitor adverse reactions and modify dose of erdafitinib accordingly. If strong CYP2C9 inhibitor is discontinued, consider increasing erdafitinib dose in the absence of any drug-related toxicities. - eribulin
eribulin and quinine both increase QTc interval. Avoid or Use Alternate Drug. Potential for enhanced QTc-prolonging effects; if concurrent use is necessary then ECG monitoring is recommended.
- fexinidazole
fexinidazole and quinine both increase QTc interval. Avoid or Use Alternate Drug. Avoid coadministration of fexinidazole with drugs known to block potassium channels and/or prolong QT interval.
fexinidazole will increase the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Avoid or Use Alternate Drug. Fexinidazole inhibits CYP3A4. Coadministration may increase risk for adverse effects of CYP3A4 substrates. - fingolimod
fingolimod and quinine both increase QTc interval. Avoid or Use Alternate Drug.
- fondaparinux
quinine increases effects of fondaparinux by unknown mechanism. Avoid or Use Alternate Drug.
- gadobenate
gadobenate and quinine both increase QTc interval. Avoid or Use Alternate Drug.
- gilteritinib
gilteritinib and quinine both increase QTc interval. Avoid or Use Alternate Drug.
- glasdegib
quinine and glasdegib both increase QTc interval. Avoid or Use Alternate Drug. If coadministration unavoidable, monitor for increased risk of QTc interval prolongation.
- granisetron
granisetron and quinine both increase QTc interval. Avoid or Use Alternate Drug.
- heparin
quinine increases effects of heparin by unknown mechanism. Avoid or Use Alternate Drug.
- hydroxychloroquine sulfate
hydroxychloroquine sulfate and quinine both increase QTc interval. Avoid or Use Alternate Drug.
- hydroxyzine
hydroxyzine and quinine both increase QTc interval. Avoid or Use Alternate Drug.
- idelalisib
idelalisib will increase the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Avoid or Use Alternate Drug. Idelalisib is a strong CYP3A inhibitor; avoid coadministration with sensitive CYP3A substrates
- isoflurane
isoflurane and quinine both increase QTc interval. Avoid or Use Alternate Drug.
- ivosidenib
ivosidenib and quinine both increase QTc interval. Avoid or Use Alternate Drug. Avoid coadministration of QTc prolonging drugs with ivosidenib or replace with alternate therapies. If coadministration of a QTc prolonging drug is unavoidable, monitor for increased risk of QTc interval prolongation.
ivosidenib will decrease the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Avoid or Use Alternate Drug. Avoid coadministration of sensitive CYP3A4 substrates with ivosidenib or replace with alternative therapies. If coadministration is unavoidable, monitor patients for loss of therapeutic effect of these drugs. - lasmiditan
lasmiditan increases levels of quinine by P-glycoprotein (MDR1) efflux transporter. Avoid or Use Alternate Drug.
- lithium
lithium and quinine both increase QTc interval. Avoid or Use Alternate Drug.
- lonafarnib
lonafarnib will increase the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Avoid or Use Alternate Drug. Avoid coadministration with sensitive CYP3A substrates. If coadministration unavoidable, monitor for adverse reactions and reduce CYP3A substrate dose in accordance with product labeling.
quinine will increase the level or effect of lonafarnib by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Avoid or Use Alternate Drug. If coadministration of lonafarnib (a sensitive CYP3A substrate) with weak CYP3A inhibitors is unavoidable, reduce to, or continue lonafarnib at starting dose. Closely monitor for arrhythmias and events (eg, syncope, heart palpitations) since lonafarnib effect on QT interval is unknown. - lopinavir
lopinavir will increase the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Avoid or Use Alternate Drug.
- lorlatinib
lorlatinib will decrease the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Avoid or Use Alternate Drug. Avoid use of lorlatinib with CYP3A substrates, where minimal concentration changes may lead to serious therapeutic failures of the substrate. If concomitant use is unavoidable, increase CYP3A substrate dosage in accordance with approved product labeling.
- lumacaftor/ivacaftor
lumacaftor/ivacaftor will decrease the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Avoid or Use Alternate Drug. Lumacaftor is a strong inducer of CYP3A. Avoid coadministration with sensitive CYP3A substrates or CYP3A substrates with a narrow therapeutic index.
- macimorelin
macimorelin and quinine both increase QTc interval. Avoid or Use Alternate Drug. Macimorelin causes an increase of ~11 msec in the corrected QT interval. Avoid coadministration with drugs that prolong QT interval, which could increase risk for developing torsade de pointes-type ventricular tachycardia. Allow sufficient washout time of drugs that are known to prolong the QT interval before administering macimorelin.
- mefloquine
quinine, mefloquine. Mechanism: pharmacodynamic synergism. Contraindicated. Risk of ECG abnormalities, cardiac arrest.
mefloquine increases toxicity of quinine by QTc interval. Avoid or Use Alternate Drug. Mefloquine may enhance the QTc prolonging effect of high risk QTc prolonging agents. - mifepristone
mifepristone will increase the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Avoid or Use Alternate Drug.
- mirtazapine
mirtazapine and quinine both increase QTc interval. Avoid or Use Alternate Drug.
- mobocertinib
mobocertinib will decrease the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Avoid or Use Alternate Drug. If use is unavoidable, increase CYP3A4 substrate dosage in accordance with its prescribing information.
mobocertinib and quinine both increase QTc interval. Avoid or Use Alternate Drug. If coadministration unavoidable, reduce mobocertinib dose and monitor QTc interval more frequently. - nefazodone
nefazodone will increase the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Avoid or Use Alternate Drug.
- olutasidenib
olutasidenib will decrease the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Avoid or Use Alternate Drug. Avoid coadministration of olutasidenib (a CYP3A4 inducer) with sensitive CYP3A substrates unless otherwise instructed in substrates prescribing information. If unavoidable, monitor for loss of therapeutic effect of sensitive CYP3A4 substrates.
- ondansetron
quinine and ondansetron both increase QTc interval. Avoid or Use Alternate Drug. Avoid with congenital long QT syndrome; ECG monitoring recommended with concomitant medications that prolong QT interval, electrolyte abnormalities, CHF, or bradyarrhythmias.
- oxaliplatin
oxaliplatin and quinine both increase QTc interval. Avoid or Use Alternate Drug.
- pacritinib
pacritinib will increase the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Avoid or Use Alternate Drug.
- pancuronium
quinine increases effects of pancuronium by pharmacodynamic synergism. Contraindicated. Risk of resp. depression.
- pexidartinib
pexidartinib will decrease the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Avoid or Use Alternate Drug. Coadministration of pexidartinib (a CYP3A4 inducer) with sensitive CYP3A substrates may lead to serious therapeutic failures. If concomitant use is unavoidable, increase the CYP3A substrate dosage in accordance with approved product labeling.
- phenindione
quinine increases effects of phenindione by unknown mechanism. Avoid or Use Alternate Drug.
- pitolisant
quinine and pitolisant both increase QTc interval. Avoid or Use Alternate Drug.
- pomalidomide
quinine increases levels of pomalidomide by P-glycoprotein (MDR1) efflux transporter. Avoid or Use Alternate Drug.
- ponesimod
ponesimod, quinine. Either increases effects of the other by QTc interval. Avoid or Use Alternate Drug. Consult cardiologist if considering treatment. Generally, should not be initiated in patients who are concurrently taking QT prolonging drugs with known arrhythmogenic properties, such as HR-lowering calcium channel blockers (eg, verapamil, diltiazem).
- primaquine
primaquine and quinine both increase QTc interval. Avoid or Use Alternate Drug.
- protamine
quinine increases effects of protamine by unknown mechanism. Avoid or Use Alternate Drug.
- rapacuronium
quinine increases effects of rapacuronium by pharmacodynamic synergism. Contraindicated. Risk of resp. depression.
- repotrectinib
quinine will increase the level or effect of repotrectinib by P-glycoprotein (MDR1) efflux transporter. Avoid or Use Alternate Drug.
repotrectinib will decrease the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Avoid or Use Alternate Drug. Repotrectinib is a CYP3A4 inducer. Avoid coadministration with CYP3A substrates where minimal concentration changes can cause reduced efficacy, unless otherwise recommended their prescribing information. - ribociclib
ribociclib increases toxicity of quinine by QTc interval. Avoid or Use Alternate Drug.
- rimegepant
quinine will increase the level or effect of rimegepant by P-glycoprotein (MDR1) efflux transporter. Avoid or Use Alternate Drug.
- riociguat
quinine will increase the level or effect of riociguat by decreasing metabolism. Avoid or Use Alternate Drug. Coadministration of riociguat (substrate of CYP isoenzymes 1A1, 2C8, 3A, 2J2) with strong CYP inhibitors may require a decreased initial dose of 0.5 mg PO TID; monitor for signs of hypotension and reduce dose if needed
- ritonavir
ritonavir will increase the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Avoid or Use Alternate Drug. Prescribing information for quinine recommends avoiding combination
- rocuronium
quinine increases effects of rocuronium by pharmacodynamic synergism. Contraindicated. Risk of resp. depression.
- saquinavir
saquinavir will increase the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Contraindicated.
- sevoflurane
sevoflurane and quinine both increase QTc interval. Avoid or Use Alternate Drug.
- siponimod
quinine will increase the level or effect of siponimod by affecting hepatic enzyme CYP2C9/10 metabolism. Avoid or Use Alternate Drug. Coadministration of siponimod with drugs that cause moderate CYP2C9 AND a moderate or strong CYP3A4 inhibition is not recommended. Caution if siponimod coadministered with moderate CYP2C9 inhibitors alone.
siponimod and quinine both increase QTc interval. Avoid or Use Alternate Drug. - sotorasib
sotorasib will decrease the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Avoid or Use Alternate Drug. If use is unavoidable, refer to the prescribing information of the CYP3A4 substrate for dosage modifications
sotorasib will decrease the level or effect of quinine by P-glycoprotein (MDR1) efflux transporter. Avoid or Use Alternate Drug. If use is unavoidable, refer to the prescribing information of the P-gp substrate for dosage modifications. - succinylcholine
quinine increases effects of succinylcholine by pharmacodynamic synergism. Contraindicated. Risk of resp. depression.
- tepotinib
tepotinib will increase the level or effect of quinine by P-glycoprotein (MDR1) efflux transporter. Avoid or Use Alternate Drug. If concomitant use unavoidable, reduce the P-gp substrate dosage if recommended in its approved product labeling.
- tetrabenazine
tetrabenazine and quinine both increase QTc interval. Avoid or Use Alternate Drug.
- tipranavir
tipranavir will increase the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Avoid or Use Alternate Drug.
- topotecan
quinine will increase the level or effect of topotecan by P-glycoprotein (MDR1) efflux transporter. Avoid or Use Alternate Drug. Product labeling for PO topotecan recommends avoiding concomitant use of P-gp inhibitors; the interaction with IV topotecan may be less severe but is still likely of clinical significance
- tucatinib
quinine will increase the level or effect of tucatinib by Other (see comment). Avoid or Use Alternate Drug. Coadministration of tucatinib (a CYP2C8 substrate) with a strong or moderate CYP2C8 inhibitors increases tucatinib plasma concentrations and risk of toxicities.
tucatinib will increase the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Avoid or Use Alternate Drug. Avoid concomitant use of tucatinib with CYP3A substrates, where minimal concentration changes may lead to serious or life-threatening toxicities. If unavoidable, reduce CYP3A substrate dose according to product labeling. - umeclidinium bromide/vilanterol inhaled
quinine increases toxicity of umeclidinium bromide/vilanterol inhaled by QTc interval. Avoid or Use Alternate Drug. Exercise extreme caution when vilanterol coadministered with drugs that prolong QTc interval; adrenergic agonist effects on the cardiovascular system may be potentiated.
- vandetanib
quinine, vandetanib. Either increases toxicity of the other by QTc interval. Avoid or Use Alternate Drug. Avoid coadministration with drugs known to prolong QT interval; if a drug known to prolong QT interval must be used, more frequent ECG monitoring is recommended.
- vecuronium
quinine increases effects of vecuronium by pharmacodynamic synergism. Contraindicated. Risk of resp. depression.
- vemurafenib
vemurafenib and quinine both increase QTc interval. Avoid or Use Alternate Drug. Concomitant use of vemurafenib with drugs that prolong QT interval is not recommended.
- venetoclax
quinine will increase the level or effect of venetoclax by P-glycoprotein (MDR1) efflux transporter. Avoid or Use Alternate Drug. If a P-gp inhibitor must be used, reduce the venetoclax dose by at least 50%. Monitor more closely for signs of venetoclax toxicities.
- vilanterol/fluticasone furoate inhaled
quinine increases toxicity of vilanterol/fluticasone furoate inhaled by QTc interval. Avoid or Use Alternate Drug. Exercise extreme caution when vilanterol coadministered with drugs that prolong QTc interval; adrenergic agonist effects on the cardiovascular system may be potentiated.
- vortioxetine
quinine increases levels of vortioxetine by affecting hepatic enzyme CYP2D6 metabolism. Avoid or Use Alternate Drug. Decrease vortioxetine dose by 50% when coadministered with strong CYP2D6 inhibitors.
- voxelotor
voxelotor will increase the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Avoid or Use Alternate Drug. Voxelotor increases systemic exposure of sensitive CYP3A4 substrates. Avoid coadministration with sensitive CYP3A4 substrates with a narrow therapeutic index. Consider dose reduction of the sensitive CYP3A4 substrate(s) if unable to avoid.
Monitor Closely (202)
- albuterol
albuterol and quinine both increase QTc interval. Use Caution/Monitor.
- amantadine
quinine will increase the level or effect of amantadine by decreasing renal clearance. Use Caution/Monitor. Coadministration of quinine or quinidine with amantadine was shown to reduce the renal clearance of amantadine by ~30%.
- amiodarone
amiodarone will increase the level or effect of quinine by basic (cationic) drug competition for renal tubular clearance. Use Caution/Monitor.
amiodarone and quinine both increase QTc interval. Use Caution/Monitor. - amitriptyline
amitriptyline and quinine both increase QTc interval. Use Caution/Monitor.
- amoxapine
amoxapine and quinine both increase QTc interval. Use Caution/Monitor.
- anagrelide
anagrelide and quinine both increase QTc interval. Use Caution/Monitor.
- apomorphine
apomorphine and quinine both increase QTc interval. Use Caution/Monitor.
- arformoterol
arformoterol and quinine both increase QTc interval. Use Caution/Monitor.
- arsenic trioxide
arsenic trioxide and quinine both increase QTc interval. Use Caution/Monitor.
- artemether/lumefantrine
artemether/lumefantrine and quinine both increase QTc interval. Use Caution/Monitor.
- asenapine
asenapine and quinine both increase QTc interval. Use Caution/Monitor.
- atogepant
quinine will increase the level or effect of atogepant by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Use Caution/Monitor.
- avapritinib
quinine will increase the level or effect of avapritinib by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Use Caution/Monitor.
- axitinib
quinine increases levels of axitinib by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Use Caution/Monitor.
- azithromycin
azithromycin and quinine both increase QTc interval. Use Caution/Monitor.
- bedaquiline
quinine and bedaquiline both increase QTc interval. Modify Therapy/Monitor Closely. ECG should be monitored closely
- berotralstat
quinine increases levels of berotralstat by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor.
berotralstat will increase the level or effect of quinine by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor. Monitor or titrate P-gp substrate dose if coadministered.
berotralstat will increase the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Use Caution/Monitor. Monitor or titrate substrate dose when berotralstat is coadministered with narrow therapeutic index drugs that are CYP3A substrates. - betrixaban
quinine increases levels of betrixaban by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor. Decrease betrixaban dose to 80 mg PO once, then 40 mg PO qDay if coadministered with a P-gp inhibitor.
- blinatumomab
blinatumomab increases levels of quinine by decreasing metabolism. Modify Therapy/Monitor Closely. Treatment initiation causes transient release of cytokines that may suppress CYP450 enzymes; highest drug-drug interaction risk is during the first 9 days of the first cycle and the first 2 days of the 2nd cycle in patients who are receiving concomitant CYP450 substrates, particularly those with a narrow therapeutic index.
- bosutinib
bosutinib and quinine both increase QTc interval. Use Caution/Monitor.
- brexpiprazole
quinine will increase the level or effect of brexpiprazole by affecting hepatic enzyme CYP2D6 metabolism. Modify Therapy/Monitor Closely. Administer a quarter of brexpiprazole dose if coadministered with a moderate CYP2D6 inhibitor PLUS a strong/moderate CYP3A4 inhibitor.
- brodalumab
brodalumab, quinine. Other (see comment). Use Caution/Monitor. Comment: Formation of CYP450 enzymes can be altered by increased levels of certain cytokines during chronic inflammation; thus, brodalumab could normalize the formation of CYP450 enzymes. Upon initiation or discontinuation of brodalumab in patients who are receiving concomitant CYP450 substrates, particularly those with a narrow therapeutic index, consider monitoring for therapeutic effect.
- bupivacaine implant
quinine, bupivacaine implant. Either increases toxicity of the other by Other (see comment). Use Caution/Monitor. Comment: Local anesthetics may increase the risk of developing methemoglobinemia when concurrently exposed to drugs that also cause methemoglobinemia.
- capecitabine
capecitabine and quinine both increase QTc interval. Use Caution/Monitor.
- carbamazepine
carbamazepine will decrease the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Use Caution/Monitor.
- cenobamate
cenobamate will decrease the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Modify Therapy/Monitor Closely. Increase dose of CYP3A4 substrate, as needed, when coadministered with cenobamate.
- ceritinib
quinine increases levels of ceritinib by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor.
- chlorpromazine
chlorpromazine and quinine both increase QTc interval. Use Caution/Monitor.
- cimetidine
cimetidine will increase the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Use Caution/Monitor.
cimetidine will increase the level or effect of quinine by basic (cationic) drug competition for renal tubular clearance. Use Caution/Monitor. - ciprofloxacin
ciprofloxacin and quinine both increase QTc interval. Use Caution/Monitor. Ciprofloxacin elicits minimal effects on QT interval. Caution if used in combination with other drugs known to affect QT interval or in patients with other risk factors.
- citalopram
quinine and citalopram both increase QTc interval. Use Caution/Monitor. ECG monitoring is recommended, along with drugs that may prolong the QT interval.
- clarithromycin
clarithromycin will increase the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Use Caution/Monitor.
clarithromycin and quinine both increase QTc interval. Use Caution/Monitor. - clomipramine
clomipramine and quinine both increase QTc interval. Use Caution/Monitor.
- clozapine
clozapine and quinine both increase QTc interval. Use Caution/Monitor.
- cobicistat
cobicistat will increase the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Use Caution/Monitor.
- crizotinib
crizotinib increases levels of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Use Caution/Monitor. Dose reduction may be needed for coadministered drugs that are predominantly metabolized by CYP3A. ECG monitoring is recommended, along with drugs that may prolong the QT interval.
crizotinib and quinine both increase QTc interval. Use Caution/Monitor. - crofelemer
crofelemer increases levels of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Use Caution/Monitor. Crofelemer has the potential to inhibit CYP3A4 at concentrations expected in the gut; unlikely to inhibit systemically because minimally absorbed.
- cyclosporine
cyclosporine will increase the level or effect of quinine by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor.
- dabigatran
quinine will increase the level or effect of dabigatran by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor. Atrial fibrillation: Avoid coadministering dabigatran with P-gp inhibitors if CrCl <30 mL/min. DVT/PE treatment: Avoid coadministering dabigatran with P-gp inhibitors if CrCl <50 mL/min
- dabrafenib
dabrafenib will decrease the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Modify Therapy/Monitor Closely.
- danicopan
danicopan will increase the level or effect of quinine by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor. Danicopan increases plasma concentrations of P-gp substrates; consider dose reduction of P-gp substrates where minimal concentration changes may lead to serious adverse reactions.
- dasatinib
dasatinib and quinine both increase QTc interval. Use Caution/Monitor.
- deferasirox
deferasirox will decrease the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Use Caution/Monitor.
- degarelix
degarelix and quinine both increase QTc interval. Use Caution/Monitor.
- desipramine
desipramine and quinine both increase QTc interval. Use Caution/Monitor.
- deutetrabenazine
quinine and deutetrabenazine both increase QTc interval. Use Caution/Monitor. At the maximum recommended dose, deutetrabenazine does not prolong QT interval to a clinically relevant extent. Certain circumstances may increase risk of torsade de pointes and/or sudden death in association with drugs that prolong the QTc interval (eg, bradycardia, hypokalemia or hypomagnesemia, coadministration with other drugs that prolong QTc interval, presence of congenital QT prolongation).
- digoxin
digoxin will increase the level or effect of quinine by basic (cationic) drug competition for renal tubular clearance. Use Caution/Monitor.
- diltiazem
diltiazem will increase the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Use Caution/Monitor.
- disopyramide
disopyramide and quinine both increase QTc interval. Use Caution/Monitor.
- dofetilide
dofetilide will increase the level or effect of quinine by basic (cationic) drug competition for renal tubular clearance. Use Caution/Monitor.
dofetilide and quinine both increase QTc interval. Use Caution/Monitor. - dolasetron
dolasetron and quinine both increase QTc interval. Use Caution/Monitor.
- droperidol
droperidol and quinine both increase QTc interval. Use Caution/Monitor.
- dulaglutide
dulaglutide, quinine. Other (see comment). Use Caution/Monitor. Comment: Dulaglutide slows gastric emptying and may impact absorption of concomitantly administered oral medications; be particularly cautious when coadministered with drugs that have a narrow therapeutic index.
- dupilumab
dupilumab, quinine. Other (see comment). Use Caution/Monitor. Comment: Formation of CYP450 enzymes can be altered by increased levels of certain cytokines during chronic inflammation; thus, dupilumab could normalize the formation of CYP450 enzymes. Upon initiation or discontinuation of dupilumab in patients who are receiving concomitant CYP450 substrates, particularly those with a narrow therapeutic index, consider monitoring for therapeutic effect.
- duvelisib
duvelisib will increase the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Modify Therapy/Monitor Closely. Coadministration with duvelisib increases AUC of a sensitive CYP3A4 substrate which may increase the risk of toxicities of these drugs. Consider reducing the dose of the sensitive CYP3A4 substrate and monitor for signs of toxicities of the coadministered sensitive CYP3A substrate.
quinine will increase the level or effect of duvelisib by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor. - elagolix
elagolix will increase the level or effect of quinine by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor.
elagolix decreases levels of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Modify Therapy/Monitor Closely. Elagolix is a weak-to-moderate CYP3A4 inducer. Monitor CYP3A substrates if coadministered. Consider increasing CYP3A substrate dose if needed. - eliglustat
eliglustat increases levels of quinine by P-glycoprotein (MDR1) efflux transporter. Modify Therapy/Monitor Closely. Monitor therapeutic drug concentrations, as indicated, or consider reducing the dosage of the P-gp substrate and titrate to clinical effect.
- elranatamab
elranatamab will increase the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Use Caution/Monitor. Elranatamab causes cytokine release syndrome (CRS) that may suppress activity of CYP enzymes, resulting in increased exposure of CYP substrates. This is more likely to occur from initiation of elranatamab step-up dosing up to 14 days after the first treatment dose and during and after CRS.
- eluxadoline
eluxadoline increases levels of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Use Caution/Monitor. Caution when CYP3A substrates that have a narrow therapeutic index are coadministered with eluxadoline.
- elvitegravir/cobicistat/emtricitabine/tenofovir DF
elvitegravir/cobicistat/emtricitabine/tenofovir DF increases levels of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Modify Therapy/Monitor Closely. Cobicistat is a CYP3A4 inhibitor; contraindicated with CYP3A4 substrates for which elevated plasma concentrations are associated with serious and/or life-threatening events.
- encorafenib
encorafenib, quinine. affecting hepatic/intestinal enzyme CYP3A4 metabolism. Use Caution/Monitor. Encorafenib both inhibits and induces CYP3A4 at clinically relevant plasma concentrations. Coadministration of encorafenib with sensitive CYP3A4 substrates may result in increased toxicity or decreased efficacy of these agents.
- epcoritamab
epcoritamab, quinine. affecting hepatic/intestinal enzyme CYP3A4 metabolism. Use Caution/Monitor. Epcoritamab causes release of cytokines that may suppress activity of CYP enzymes, resulting in increased exposure of CYP substrates. For certain CYP substrates, minimal changes in their concentration may lead to serious adverse reactions. If needed, modify therapy as recommended in the substrate's prescribing information. .
- erythromycin base
erythromycin base will increase the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Use Caution/Monitor.
erythromycin base and quinine both increase QTc interval. Use Caution/Monitor. - erythromycin ethylsuccinate
erythromycin ethylsuccinate will increase the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Use Caution/Monitor.
erythromycin ethylsuccinate and quinine both increase QTc interval. Use Caution/Monitor. - erythromycin lactobionate
erythromycin lactobionate will increase the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Use Caution/Monitor.
erythromycin lactobionate and quinine both increase QTc interval. Use Caution/Monitor. - erythromycin stearate
erythromycin stearate will increase the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Use Caution/Monitor.
erythromycin stearate and quinine both increase QTc interval. Use Caution/Monitor. - escitalopram
escitalopram and quinine both increase QTc interval. Use Caution/Monitor.
- ezogabine
ezogabine, quinine. Either increases toxicity of the other by QTc interval. Use Caution/Monitor. Slight and transient QT-prolongation observed with ezogabine, particularly when dose titrated to 1200 mg/day. QT interval should be monitored when ezogabine is prescribed with agents known to increase QT interval.
- fedratinib
fedratinib will increase the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Use Caution/Monitor. Adjust dose of drugs that are CYP3A4 substrates as necessary.
- ferric maltol
ferric maltol, quinine. Either increases levels of the other by unspecified interaction mechanism. Modify Therapy/Monitor Closely. Coadministration of ferric maltol with certain oral medications may decrease the bioavailability of either ferric maltol and some oral drugs. For oral drugs where reductions in bioavailability may cause clinically significant effects on its safety or efficacy, separate administration of ferric maltol from these drugs. Duration of separation may depend on the absorption of the medication concomitantly administered (eg, time to peak concentration, whether the drug is an immediate or extended release product).
- finerenone
quinine will increase the level or effect of finerenone by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Modify Therapy/Monitor Closely. Monitor serum potassium during initiation and dosage adjustment of either finererone or weak CYP3A4 inhibitors. Adjust finererone dosage as needed.
- flecainide
flecainide and quinine both increase QTc interval. Use Caution/Monitor.
- flibanserin
flibanserin increases levels of quinine by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor. Increase monitoring of concentrations of drugs transported by P-gp that have a narrow therapeutic index if coadministered with flibanserin.
quinine will increase the level or effect of flibanserin by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Use Caution/Monitor. Increased flibanserin adverse effects may occur if coadministered with multiple weak CYP3A4 inhibitors. - floxuridine
floxuridine and quinine both increase QTc interval. Use Caution/Monitor.
- fluconazole
fluconazole and quinine both increase QTc interval. Use Caution/Monitor.
- fluoxetine
fluoxetine and quinine both increase QTc interval. Use Caution/Monitor.
- fluphenazine
fluphenazine and quinine both increase QTc interval. Use Caution/Monitor.
- formoterol
formoterol and quinine both increase QTc interval. Use Caution/Monitor.
- foscarnet
foscarnet and quinine both increase QTc interval. Use Caution/Monitor.
- fostemsavir
quinine and fostemsavir both increase QTc interval. Use Caution/Monitor. QTc prolongation reported with higher than recommended doses of fostemsavir.
- gemifloxacin
gemifloxacin and quinine both increase QTc interval. Use Caution/Monitor.
- gepirone
gepirone and quinine both increase QTc interval. Modify Therapy/Monitor Closely.
- glecaprevir/pibrentasvir
quinine will increase the level or effect of glecaprevir/pibrentasvir by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor.
glecaprevir/pibrentasvir will increase the level or effect of quinine by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor. - glofitamab
glofitamab, quinine. affecting hepatic/intestinal enzyme CYP3A4 metabolism. Use Caution/Monitor. GlofitamaGlofitamab causes release of cytokines that may suppress activity of CYP enzymes, resulting in increased exposure of CYP substrates. For certain CYP substrates, minimal changes in their concentration may lead to serious adverse reactions. If needed, modify therapy as recommended in the substrate's prescribing information. causes release of cytokines that may suppress activity of CYP enzymes, resulting in increased exposure of CYP substrates. For certain CYP substrates, minimal changes in their concentration may lead to serious adversereactions. If needed, modify therapy as recommended in the substrate's prescribing information. .
- glycerol phenylbutyrate
glycerol phenylbutyrate will decrease the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Use Caution/Monitor. Glycerol phenylbutyrate is a weak inducer of CYP3A4. Monitor for decreased efficacy of CYP3A4 substrates that have a narrow therapeutic index.
- guselkumab
guselkumab, quinine. Other (see comment). Use Caution/Monitor. Comment: Formation of CYP450 enzymes can be altered by increased levels of certain cytokines during chronic inflammation; thus, normalizing the formation of CYP450 enzymes. Upon initiation or discontinuation of guselkumab in patients who are receiving concomitant CYP450 substrates, particularly those with a narrow therapeutic index, consider monitoring for therapeutic effect.
- haloperidol
haloperidol and quinine both increase QTc interval. Use Caution/Monitor.
- ibutilide
ibutilide and quinine both increase QTc interval. Use Caution/Monitor.
- iloperidone
iloperidone increases levels of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Use Caution/Monitor. Iloperidone is a time-dependent CYP3A inhibitor and may lead to increased plasma levels of drugs predominantly eliminated by CYP3A4.
iloperidone and quinine both increase QTc interval. Use Caution/Monitor. - indacaterol, inhaled
indacaterol, inhaled, quinine. QTc interval. Use Caution/Monitor. Drugs that are known to prolong the QTc interval may have an increased the risk of ventricular arrhythmias.
- indapamide
indapamide and quinine both increase QTc interval. Use Caution/Monitor.
- isavuconazonium sulfate
quinine will increase the level or effect of isavuconazonium sulfate by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Use Caution/Monitor.
isavuconazonium sulfate will increase the level or effect of quinine by Other (see comment). Use Caution/Monitor. Isavuconazonium sulfate, an inhibitor of P-gp and CYP3A4, may increase the effects or levels of sensitive P-gp or CYP3A4 substrates, which may require dose adjustment. - isoniazid
isoniazid will increase the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Use Caution/Monitor.
- isradipine
isradipine and quinine both increase QTc interval. Use Caution/Monitor.
- istradefylline
istradefylline will increase the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Use Caution/Monitor. Istradefylline 40 mg/day increased peak levels and AUC of CYP3A4 substrates in clinical trials. This effect was not observed with istradefylline 20 mg/day. Consider dose reduction of sensitive CYP3A4 substrates.
istradefylline will increase the level or effect of quinine by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor. Istradefylline 40 mg/day increased peak levels and AUC of P-gp substrates in clinical trials. Consider dose reduction of sensitive P-gp substrates. - itraconazole
itraconazole will increase the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Use Caution/Monitor.
itraconazole and quinine both increase QTc interval. Use Caution/Monitor. - ixekizumab
ixekizumab, quinine. Other (see comment). Use Caution/Monitor. Comment: Formation of CYP450 enzymes can be altered by increased levels of certain cytokines during chronic inflammation; thus, ixekizumab could normalize the formation of CYP450 enzymes. Upon initiation or discontinuation of ixekizumab in patients who are receiving concomitant CYP450 substrates, particularly those with a narrow therapeutic index, consider monitoring for therapeutic effect.
- ketoconazole
ketoconazole will increase the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Use Caution/Monitor.
- lapatinib
lapatinib and quinine both increase QTc interval. Use Caution/Monitor.
- lemborexant
quinine will increase the level or effect of lemborexant by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Modify Therapy/Monitor Closely. Lower nightly dose of lemborexant recommended if coadministered with weak CYP3A4 inhibitors. See drug monograph for specific dosage modification.
- lenacapavir
lenacapavir will increase the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Use Caution/Monitor. Lencapavir may increase CYP3A4 substrates initiated within 9 months after last SC dose of lenacapavir, which may increase potential risk of adverse reactions of CYP3A4 substrates.
- letermovir
letermovir increases levels of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Use Caution/Monitor.
- levofloxacin
levofloxacin and quinine both increase QTc interval. Use Caution/Monitor.
- levoketoconazole
levoketoconazole will increase the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Use Caution/Monitor.
- lomitapide
quinine increases levels of lomitapide by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Use Caution/Monitor. Lomitapide dose should not exceed 30 mg/day.
- lonafarnib
lonafarnib will increase the level or effect of quinine by P-glycoprotein (MDR1) efflux transporter. Modify Therapy/Monitor Closely. Lonafarnib is a weak P-gp inhibitor. Monitor for adverse reactions if coadministered with P-gp substrates where minimal concentration changes may lead to serious or life-threatening toxicities. Reduce P-gp substrate dose if needed.
- lonapegsomatropin
lonapegsomatropin will decrease the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Use Caution/Monitor. Limited published data indicate that growth hormone treatment increases cytochrome P450 (CYP450)-mediated antipyrine clearance. Caution with sensitive CYP substrates
- lopinavir
lopinavir and quinine both increase QTc interval. Use Caution/Monitor.
- maprotiline
maprotiline and quinine both increase QTc interval. Use Caution/Monitor.
- methadone
methadone and quinine both increase QTc interval. Use Caution/Monitor.
- midazolam intranasal
quinine will increase the level or effect of midazolam intranasal by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Use Caution/Monitor. Coadministration of mild CYP3A4 inhibitors with midazolam intranasal may cause higher midazolam systemic exposure, which may prolong sedation.
- mifepristone
mifepristone, quinine. QTc interval. Modify Therapy/Monitor Closely. Use alternatives if available.
- mitotane
mitotane decreases levels of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Use Caution/Monitor. Mitotane is a strong inducer of cytochrome P-4503A4; monitor when coadministered with CYP3A4 substrates for possible dosage adjustments.
- moxifloxacin
moxifloxacin and quinine both increase QTc interval. Use Caution/Monitor.
- naldemedine
quinine increases levels of naldemedine by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor. Monitor naldemedine for potential adverse effects if coadministered with P-gp inhibitors.
- nilotinib
nilotinib and quinine both increase QTc interval. Use Caution/Monitor.
- nintedanib
quinine increases levels of nintedanib by P-glycoprotein (MDR1) efflux transporter. Modify Therapy/Monitor Closely. If nintedanib adverse effects occur, management may require interruption, dose reduction, or discontinuation of therapy .
- nortriptyline
nortriptyline and quinine both increase QTc interval. Use Caution/Monitor.
- octreotide
octreotide and quinine both increase QTc interval. Use Caution/Monitor.
- ofloxacin
ofloxacin and quinine both increase QTc interval. Use Caution/Monitor.
- olanzapine
olanzapine and quinine both increase QTc interval. Use Caution/Monitor.
- oliceridine
quinine will increase the level or effect of oliceridine by affecting hepatic enzyme CYP2D6 metabolism. Modify Therapy/Monitor Closely. If concomitant use is necessary, may require less frequent oliceridine dosing. Closely monitor for respiratory depression and sedation and titrate subsequent doses accordingly. If inhibitor is discontinued, consider increase oliceridine dosage until stable drug effects are achieved. Monitor for signs of opioid withdrawal.
- olodaterol inhaled
quinine and olodaterol inhaled both increase QTc interval. Use Caution/Monitor. Drugs that prolong the QTc interval and may potentiate the effects of beta2 agonists on the cardiovascular system; increased risk of ventricular arrhythmias
- omaveloxolone
omaveloxolone will decrease the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Use Caution/Monitor. Omaveloxolone may reduce systemic exposure of sensitive CYP3A4 substrates. Check prescribing information of substrate if dosage modification is needed.
- oritavancin
oritavancin will decrease the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Use Caution/Monitor. Oritavancin is a weak CYP3A4 inducer; caution if coadministered with CYP3A4 substrates that have a narrow therapeutic index
- osilodrostat
osilodrostat and quinine both increase QTc interval. Use Caution/Monitor.
- oxaliplatin
oxaliplatin will increase the level or effect of quinine by Other (see comment). Use Caution/Monitor. Monitor for ECG changes if therapy is initiated in patients with drugs known to prolong QT interval.
- ozanimod
ozanimod and quinine both increase QTc interval. Modify Therapy/Monitor Closely. The potential additive effects on heart rate, treatment with ozanimod should generally not be initiated in patients who are concurrently treated with QT prolonging drugs with known arrhythmogenic properties.
- paclitaxel
quinine will increase the level or effect of paclitaxel by Other (see comment). Use Caution/Monitor. Paclitaxel levels/toxicity may increase when coadministered with CYP2C8 inhibitors
- paclitaxel protein bound
quinine will increase the level or effect of paclitaxel protein bound by Other (see comment). Use Caution/Monitor. Paclitaxel levels/toxicity may increase when coadministered with CYP2C8 inhibitors
- palbociclib
palbociclib will increase the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Modify Therapy/Monitor Closely. The dose of sensitive CYP3A substrates with a narrow therapeutic index may need to be reduced if coadministered with palbociclib
- paliperidone
paliperidone and quinine both increase QTc interval. Use Caution/Monitor.
- pasireotide
quinine and pasireotide both increase QTc interval. Modify Therapy/Monitor Closely.
- pazopanib
pazopanib and quinine both increase QTc interval. Use Caution/Monitor.
- pentamidine
pentamidine and quinine both increase QTc interval. Use Caution/Monitor.
- perphenazine
perphenazine and quinine both increase QTc interval. Use Caution/Monitor.
- phenytoin
phenytoin will decrease the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Use Caution/Monitor. Use caution when prescribing phenytoin and quinine together due to a decrease in quinine plasma concentrations and potential lack of efficacy.
- pirtobrutinib
pirtobrutinib will increase the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Use Caution/Monitor. Pirtobrutinib (a CYP3A4 inhibitor) may increase plasma concentrations of sensitive CYP3A4 substrate which may increase the risk of adverse reactions related to these substrates.
- pitolisant
pitolisant will decrease the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Use Caution/Monitor. Pitolisant is a borderline/weak inducer of CYP3A4. Monitor sensitive CYP3A4 substrates for reduced effectiveness if coadministered.
- posaconazole
posaconazole and quinine both increase QTc interval. Use Caution/Monitor.
- procainamide
procainamide will increase the level or effect of quinine by basic (cationic) drug competition for renal tubular clearance. Use Caution/Monitor.
procainamide and quinine both increase QTc interval. Use Caution/Monitor. - propafenone
propafenone and quinine both increase QTc interval. Use Caution/Monitor.
- protriptyline
protriptyline and quinine both increase QTc interval. Use Caution/Monitor.
- quetiapine
quetiapine, quinine. Either increases toxicity of the other by QTc interval. Use Caution/Monitor. Avoid use with drugs that prolong QT and in patients with risk factors for prolonged QT interval. Postmarketing cases show QT prolongation with overdose in patients with concomitant illness or with drugs known to cause electrolyte imbalance or prolong QT.
- quinidine
quinidine will increase the level or effect of quinine by basic (cationic) drug competition for renal tubular clearance. Use Caution/Monitor.
quinidine and quinine both increase QTc interval. Use Caution/Monitor. - quizartinib
quizartinib, quinine. Either increases effects of the other by QTc interval. Modify Therapy/Monitor Closely. Monitor patients more frequently with ECG if coadministered with QT prolonging drugs.
- ranolazine
ranolazine and quinine both increase QTc interval. Use Caution/Monitor.
- ribociclib
ribociclib will increase the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Modify Therapy/Monitor Closely. Caution if ribociclib is coadministered with sensitive CYP3A4 substrates that have a narrow therapeutic index. Dose reduction for sensitive CYP3A4 substrates may be needed.
- rifabutin
rifabutin will decrease the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Use Caution/Monitor.
- rifampin
rifampin will decrease the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Use Caution/Monitor.
- rifaximin
quinine increases levels of rifaximin by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor.
- rilpivirine
rilpivirine increases toxicity of quinine by QTc interval. Use Caution/Monitor. Rilpivirine should be used with caution when co-administered with a drug with a known risk of Torsade de Pointes.
- risperidone
risperidone and quinine both increase QTc interval. Use Caution/Monitor.
- ritlecitinib
ritlecitinib will increase the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Modify Therapy/Monitor Closely. Ritlecitinib inhibits CYP3A4 substrates; coadministration increases AUC and peak plasma concentration sensitive substrates, which may increase risk of adverse reactions. Additional monitoring and dosage adjustment may be needed in accordance with product labeling of CYP3A substrates.
- romidepsin
romidepsin and quinine both increase QTc interval. Use Caution/Monitor.
- rucaparib
rucaparib will increase the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Modify Therapy/Monitor Closely. Adjust dosage of CYP3A4 substrates, if clinically indicated.
- saquinavir
saquinavir and quinine both increase QTc interval. Use Caution/Monitor.
- sarecycline
sarecycline will increase the level or effect of quinine by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor. Monitor for toxicities of P-gp substrates that may require dosage reduction when coadministered with P-gp inhibitors.
- sarilumab
sarilumab, quinine. Other (see comment). Use Caution/Monitor. Comment: Formation of CYP450 enzymes can be altered by increased levels of cytokines such as IL-6. Elevated IL-6 concentration may down-regulate CYP activity, such as in patients with RA, and, hence, increase drug levels compared with subjects without RA. Blockade of IL-6 signaling by IL-6 antagonists (eg, sarilumab) might reverse the inhibitory effect of IL-6 and restore CYP activity, leading to decreased drug concentrations. Caution when initiating or discontinuing sarilumab if coadministered with CYP450 substrates, especially those with a narrow therapeutic index.
- schisandra
schisandra will increase the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Use Caution/Monitor.
- secukinumab
secukinumab, quinine. Other (see comment). Use Caution/Monitor. Comment: Formation of CYP450 enzymes can be altered by increased levels of certain cytokines during chronic inflammation; thus, secukinumab could normalize the formation of CYP450 enzymes. Upon initiation or discontinuation of secukinumab in patients who are receiving concomitant CYP450 substrates, particularly those with a narrow therapeutic index, consider monitoring for therapeutic effect.
- selexipag
quinine will increase the level or effect of selexipag by decreasing metabolism. Modify Therapy/Monitor Closely. Reduce selexipag dose to once daily if coadministered with moderate CYP2C8 inhibitors.
- selpercatinib
selpercatinib increases toxicity of quinine by QTc interval. Use Caution/Monitor.
- sertraline
sertraline and quinine both increase QTc interval. Use Caution/Monitor.
- sodium sulfate/?magnesium sulfate/potassium chloride
sodium sulfate/?magnesium sulfate/potassium chloride increases toxicity of quinine by QTc interval. Use Caution/Monitor. Consider predose and post-colonoscopy ECGs in patients at increased risk of serious cardiac arrhythmias. .
- sodium sulfate/potassium sulfate/magnesium sulfate
sodium sulfate/potassium sulfate/magnesium sulfate increases toxicity of quinine by QTc interval. Use Caution/Monitor. Consider predose and post-colonoscopy ECGs in patients at increased risk of serious cardiac arrhythmias. .
- solifenacin
solifenacin and quinine both increase QTc interval. Use Caution/Monitor.
- somapacitan
somapacitan will decrease the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Use Caution/Monitor. Limited published data indicate that growth hormone treatment increases cytochrome P450 (CYP450)-mediated antipyrine clearance. Caution with sensitive CYP substrates
- somatrogon
somatrogon will decrease the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Use Caution/Monitor. Limited published data indicate that growth hormone treatment increases cytochrome P450 (CYP450)-mediated antipyrine clearance. Caution with sensitive CYP substrates
- somatropin
somatropin will decrease the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Use Caution/Monitor. Limited published data indicate that growth hormone treatment increases cytochrome P450 (CYP450)-mediated antipyrine clearance. Caution with sensitive CYP substrates
- sorafenib
sorafenib and quinine both increase QTc interval. Use Caution/Monitor.
- sotalol
sotalol and quinine both increase QTc interval. Use Caution/Monitor.
- St John's Wort
St John's Wort will decrease the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Use Caution/Monitor.
- stiripentol
stiripentol, quinine. affecting hepatic/intestinal enzyme CYP3A4 metabolism. Modify Therapy/Monitor Closely. Stiripentol is a CYP3A4 inhibitor and inducer. Monitor CYP3A4 substrates coadministered with stiripentol for increased or decreased effects. CYP3A4 substrates may require dosage adjustment.
stiripentol will increase the level or effect of quinine by P-glycoprotein (MDR1) efflux transporter. Modify Therapy/Monitor Closely. Consider reducing the dose of P-glycoprotein (P-gp) substrates, if adverse reactions are experienced when administered concomitantly with stiripentol. - sunitinib
sunitinib and quinine both increase QTc interval. Use Caution/Monitor.
- tacrolimus
tacrolimus and quinine both increase QTc interval. Use Caution/Monitor.
- talazoparib
quinine will increase the level or effect of talazoparib by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor. Talazoparib is a P-glycoprotein (P-gp) substrate; coadministration with P-gp inhibitors may increase talazoparib systemic exposure.
- talquetamab
talquetamab will increase the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Use Caution/Monitor. Talquetamab causes cytokine release syndrome (CRS) that may suppress activity of CYP enzymes, resulting in increased exposure of CYP substrates. This is more likely to occur from initiation of talquetamab step-up dosing up to 14 days after the first treatment dose and during and after CRS.
- tamsulosin
quinine increases levels of tamsulosin by affecting hepatic enzyme CYP2D6 metabolism. Use Caution/Monitor.
- tazemetostat
tazemetostat will decrease the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Use Caution/Monitor.
quinine will increase the level or effect of tazemetostat by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Use Caution/Monitor. - teclistamab
teclistamab will increase the level or effect of quinine by altering metabolism. Use Caution/Monitor. Teclistamab causes release of cytokines that may suppress activity of CYP450 enzymes, resulting in increased exposure of CYP substrates. Monitor for increased concentrations or toxicities of sensitive CYP substrates. Adjust dose of CYP substrate drug as needed.
- tecovirimat
tecovirimat will decrease the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Use Caution/Monitor. Tecovirimat is a weak CYP3A4 inducer. Monitor sensitive CYP3A4 substrates for effectiveness if coadministered.
- telavancin
telavancin and quinine both increase QTc interval. Use Caution/Monitor.
- telotristat ethyl
telotristat ethyl will decrease the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Modify Therapy/Monitor Closely. Telotristat ethyl induces CYP3A4 and may reduce systemic exposure of sensitive CYP3A4 substrates. Monitor for suboptimal efficacy and consider increasing the dose of the CYP3A4 substrate.
- tetracaine
tetracaine, quinine. Other (see comment). Use Caution/Monitor. Comment: Monitor for signs of methemoglobinemia when methemoglobin-inducing drugs are coadministered.
- thiothixene
thiothixene and quinine both increase QTc interval. Use Caution/Monitor.
- tinidazole
quinine will increase the level or effect of tinidazole by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Use Caution/Monitor.
- tobramycin inhaled
tobramycin inhaled and quinine both increase nephrotoxicity and/or ototoxicity. Modify Therapy/Monitor Closely. Avoid concurrent or sequential use to decrease risk for ototoxicity
- toremifene
toremifene and quinine both increase QTc interval. Use Caution/Monitor.
- triclabendazole
triclabendazole and quinine both increase QTc interval. Use Caution/Monitor.
- trimipramine
trimipramine and quinine both increase QTc interval. Use Caution/Monitor.
- trofinetide
trofinetide will increase the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Use Caution/Monitor. Monitor CYP3A4 substrates for which a small increase in plasma concentration may lead to serious toxicities if coadministered with trofinetide (a weak CYP3A4 inhibitor).
- tucatinib
tucatinib will increase the level or effect of quinine by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor. Consider reducing the dosage of P-gp substrates, where minimal concentration changes may lead to serious or life-threatening toxicities.
- turmeric
turmeric will increase the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Use Caution/Monitor.
- ustekinumab
ustekinumab, quinine. Other (see comment). Use Caution/Monitor. Comment: Formation of CYP450 enzymes can be altered by increased levels of certain cytokines during chronic inflammation; thus, normalizing the formation of CYP450 enzymes. Upon initiation or discontinuation of ustekinumab in patients who are receiving concomitant CYP450 substrates, particularly those with a narrow therapeutic index, consider monitoring for therapeutic effect.
- vardenafil
vardenafil and quinine both increase QTc interval. Use Caution/Monitor.
- voclosporin
voclosporin, quinine. Either increases effects of the other by QTc interval. Use Caution/Monitor.
- vonoprazan
vonoprazan will increase the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Use Caution/Monitor. Vonoprazan is weak CYP3A inhibitor. Caution with sensitive CYP3A substrates.
- voriconazole
voriconazole and quinine both increase QTc interval. Use Caution/Monitor.
- vorinostat
vorinostat and quinine both increase QTc interval. Use Caution/Monitor.
- warfarin
quinine will increase the level or effect of warfarin by decreasing metabolism. Use Caution/Monitor. Cinchona alkaloids, including quinine and quinidine, may increase anticoagulant effect of vitamin K antagonists by inhibiting hepatic synthesis of vitamin K-dependent coagulation proteins.
- ziprasidone
ziprasidone and quinine both increase QTc interval. Use Caution/Monitor.
Minor (72)
- acetazolamide
acetazolamide will increase the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Minor/Significance Unknown.
- amobarbital
amobarbital will decrease the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Minor/Significance Unknown.
- anastrozole
anastrozole will increase the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Minor/Significance Unknown.
- aprepitant
aprepitant will increase the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Minor/Significance Unknown.
- armodafinil
armodafinil will decrease the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Minor/Significance Unknown.
- artemether/lumefantrine
artemether/lumefantrine will decrease the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Minor/Significance Unknown.
- atazanavir
atazanavir will increase the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Minor/Significance Unknown.
- bosentan
bosentan will decrease the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Minor/Significance Unknown.
- budesonide
budesonide will decrease the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Minor/Significance Unknown.
- butabarbital
butabarbital will decrease the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Minor/Significance Unknown.
- butalbital
butalbital will decrease the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Minor/Significance Unknown.
- conivaptan
conivaptan will increase the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Minor/Significance Unknown.
- cortisone
cortisone will decrease the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Minor/Significance Unknown.
- cyclophosphamide
cyclophosphamide will increase the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Minor/Significance Unknown.
- danazol
danazol will increase the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Minor/Significance Unknown.
- darifenacin
darifenacin will increase the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Minor/Significance Unknown.
- darunavir
darunavir will increase the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Minor/Significance Unknown.
- dasatinib
dasatinib will increase the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Minor/Significance Unknown.
- dexamethasone
dexamethasone will decrease the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Minor/Significance Unknown.
- DHEA, herbal
DHEA, herbal will increase the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Minor/Significance Unknown.
- drospirenone
drospirenone will increase the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Minor/Significance Unknown.
- efavirenz
efavirenz will decrease the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Minor/Significance Unknown.
- eslicarbazepine acetate
eslicarbazepine acetate will decrease the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Minor/Significance Unknown.
- etravirine
etravirine will decrease the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Minor/Significance Unknown.
- fluconazole
fluconazole will increase the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Minor/Significance Unknown.
- fludrocortisone
fludrocortisone will decrease the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Minor/Significance Unknown.
- fosamprenavir
fosamprenavir will increase the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Minor/Significance Unknown.
- fosaprepitant
fosaprepitant will increase the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Minor/Significance Unknown.
- fosphenytoin
fosphenytoin will decrease the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Minor/Significance Unknown.
- grapefruit
grapefruit will increase the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Minor/Significance Unknown.
- griseofulvin
griseofulvin will decrease the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Minor/Significance Unknown.
- hydrochlorothiazide
hydrochlorothiazide will increase the level or effect of quinine by basic (cationic) drug competition for renal tubular clearance. Minor/Significance Unknown.
- hydrocortisone
hydrocortisone will decrease the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Minor/Significance Unknown.
- indinavir
indinavir will increase the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Minor/Significance Unknown.
- lapatinib
lapatinib will increase the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Minor/Significance Unknown.
- larotrectinib
larotrectinib will increase the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Minor/Significance Unknown.
- lumefantrine
lumefantrine will decrease the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Minor/Significance Unknown.
- marijuana
marijuana will increase the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Minor/Significance Unknown.
- memantine
memantine will increase the level or effect of quinine by basic (cationic) drug competition for renal tubular clearance. Minor/Significance Unknown.
- metformin
metformin will increase the level or effect of quinine by basic (cationic) drug competition for renal tubular clearance. Minor/Significance Unknown.
- methyclothiazide
methyclothiazide will increase the level or effect of quinine by basic (cationic) drug competition for renal tubular clearance. Minor/Significance Unknown.
- methylprednisolone
methylprednisolone will decrease the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Minor/Significance Unknown.
- metronidazole
metronidazole will increase the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Minor/Significance Unknown.
- miconazole vaginal
miconazole vaginal will increase the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Minor/Significance Unknown.
- midodrine
midodrine will increase the level or effect of quinine by basic (cationic) drug competition for renal tubular clearance. Minor/Significance Unknown.
- nafcillin
nafcillin will decrease the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Minor/Significance Unknown.
- nelfinavir
nelfinavir will increase the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Minor/Significance Unknown.
- nevirapine
nevirapine will decrease the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Minor/Significance Unknown.
- nifedipine
nifedipine will increase the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Minor/Significance Unknown.
- nilotinib
nilotinib will increase the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Minor/Significance Unknown.
- ofloxacin
ofloxacin will increase the level or effect of quinine by basic (cationic) drug competition for renal tubular clearance. Minor/Significance Unknown.
- oxcarbazepine
oxcarbazepine will decrease the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Minor/Significance Unknown.
- pentobarbital
pentobarbital will decrease the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Minor/Significance Unknown.
- phenobarbital
phenobarbital will decrease the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Minor/Significance Unknown.
- posaconazole
posaconazole will increase the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Minor/Significance Unknown.
- pramipexole
pramipexole will increase the level or effect of quinine by basic (cationic) drug competition for renal tubular clearance. Minor/Significance Unknown.
- prednisone
prednisone will decrease the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Minor/Significance Unknown.
- primaquine
primaquine, quinine. Mechanism: pharmacodynamic synergism. Minor/Significance Unknown. Risk of hemolysis in G6PD deficient pts.
- primidone
primidone will decrease the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Minor/Significance Unknown.
- quinupristin/dalfopristin
quinupristin/dalfopristin will increase the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Minor/Significance Unknown.
- rifapentine
rifapentine will decrease the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Minor/Significance Unknown.
- rufinamide
rufinamide will decrease the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Minor/Significance Unknown.
- ruxolitinib
quinine will increase the level or effect of ruxolitinib by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Minor/Significance Unknown.
- ruxolitinib topical
quinine will increase the level or effect of ruxolitinib topical by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Minor/Significance Unknown.
- secobarbital
secobarbital will decrease the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Minor/Significance Unknown.
- sulfamethoxazole
sulfamethoxazole will increase the level or effect of quinine by basic (cationic) drug competition for renal tubular clearance. Minor/Significance Unknown.
- topiramate
topiramate will decrease the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Minor/Significance Unknown.
- triamterene
quinine will increase the level or effect of triamterene by basic (cationic) drug competition for renal tubular clearance. Minor/Significance Unknown.
- trimethoprim
quinine will increase the level or effect of trimethoprim by basic (cationic) drug competition for renal tubular clearance. Minor/Significance Unknown.
- verapamil
verapamil will increase the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Minor/Significance Unknown.
quinine will increase the level or effect of verapamil by basic (cationic) drug competition for renal tubular clearance. Minor/Significance Unknown. - voriconazole
voriconazole will increase the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Minor/Significance Unknown.
- zafirlukast
zafirlukast will increase the level or effect of quinine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Minor/Significance Unknown.
Adverse Effects
<1%
Flushing of the skin
Anginal symptoms
Fever
Rash
Pruritus
Hypoglycemia
Epigastric pain
Hemolysis in G6PD deficiency
Thrombocytopenia
Hepatitis
Nightblindness
Diplopia
Optic atrophy
Impaired hearing
Hypersensitivity reaction
Frequency Not Defined
Severe headache
Nausea
Vomiting
Diarrhea
Blurred vision
Tinnituscinchonism (risk of cinchonism is directly related to dose and duration of therapy)
Warnings
Black Box Warnings
Limited or no benefit for treatment/prevention of nocturnal leg cramps
May cause serious and life-threatening hematologic reactions, including thrombocytopenia and hemolytic uremic syndrome/thrombotic thrombocytopenic purpura (HUS/TTP)
Chronic renal impairment associated with the development of TTP has been reported
Contraindications
Prolonged QT interval
Hypersensitivity; cross-sensitivity with mefloquine or quinidine
G6PD deficiency
Optic neuritis, tinnitus, history of quinine-associated blackwater fever and thrombocytopenic purpura
Thrombocytopenia
Idiopathic thrombocytopenia purpura (ITP) and thrombotic thrombocytopenic purpura (TTP)
Hemolytic uremic syndrome
Blackwater fever
Myasthenia gravis
Optic neuritis
Cautions
Acute hemolytic anemia reported in patients receiving quinine for treatment of malaria, including patients with glucose-6-phosphate dehydrogenase (G6PD) deficiency; the cause for acute hemolytic anemia in treated patients with malaria and potential relationship with G6PD deficiency not determined; closely monitor hemoglobin and hematocrit during quinine treatment; discontinue therapy if patients develop acute hemolytic anemia
Use with caution in patients with atrial fibrillation or atrial flutter; a paradoxical increase in ventricular response rate may occur with quinine, similar to that observed with quinidine; if digoxin is used to prevent a rapid ventricular response, serum digoxin levels should be closely monitored, because digoxin levels may be increased with use of quinine
Quinine stimulates release of insulin from the pancreas, and patients, especially pregnant women, may experience clinically significant hypoglycemia
Hypersensitivity
- Serious hypersensitivity reactions reported with therapy include anaphylactic shock, anaphylactoid reactions, urticaria, serious skin rashes, including Stevens-Johnson syndrome and toxic epidermal necrolysis, angioedema, facial edema, bronchospasm, and pruritus
- A number of other serious adverse reactions reported with quinine, including thrombotic thrombocytopenic purpura (TTP) and hemolytic uremic syndrome (HUS), thrombocytopenia, immune thrombocytopenic purpura (ITP), blackwater fever, disseminated intravascular coagulation, leukopenia, neutropenia, granulomatous hepatitis, and acute interstitial nephritis may also be due to hypersensitivity reactions; therapy should be discontinued in case of any signs or symptoms of hypersensitivity
Thrombocytopenia
- Quinine-induced thrombocytopenia is an immune-mediated disorder; severe cases of thrombocytopenia that are fatal or life threatening reported, including cases of hemolytic-uremic syndrome/thrombotic thrombocytopenic purpura (HUS/TTP); chronic renal impairment associated with development of TTP also reported
- Thrombocytopenia usually resolves within a week upon discontinuation of quinine; if quinine is not stopped, a patient is at risk for fatal hemorrhage; upon re-exposure to quinine from any source, a patient with quinine-dependent antibodies could develop thrombocytopenia that is more rapid in onset and more severe than the original episode
Treatment or prevention of leg cramps
- The drug may cause unpredictable serious and life-threatening hematologic reactions including thrombocytopenia and HUS/TTP in addition to hypersensitivity reactions, QT prolongation, serious cardiac arrhythmias including torsades de pointes, and other serious adverse events requiring medical intervention and hospitalization
- Chronic renal impairment associated with development of TTP, and fatalities also reported; the risk associated with therapy in the absence of evidence of its effectiveness for treatment or prevention of nocturnal leg cramps, outweighs any potential benefit in treating and/or preventing this benign, self-limiting condition
QT prolongation
- QT interval prolongation has been a consistent finding in studies evaluating electrocardiographic changes with oral or parenteral quinine administration, regardless of age, clinical status, or severity of disease
- The maximum increase in QT interval has been shown to correspond with peak quinine plasma concentration; quinine sulfate has been rarely associated with potentially fatal cardiac arrhythmias, including torsades de pointes, and ventricular fibrillation
- Therapy has been shown to cause concentration-dependent prolongation of the PR and QRS interval; at particular risk are patients with underlying structural heart disease and preexisting conduction system abnormalities, elderly patients with sick sinus syndrome, patients with atrial fibrillation with slow ventricular response, patients with myocardial ischemia or patients receiving drugs known to prolong the PR interval (eg, verapamil) or QRS interval (eg, flecainide or quinidine)
- Therapy should be avoided in patients with known prolongation of QT interval and in patients with clinical conditions known to prolong the QT interval, such as uncorrected hypokalemia, bradycardia, and certain cardiac conditions
Drug interaction overview
- Drug not recommended for use with other drugs known to cause QT prolongation, including Class IA antiarrhythmic agents (eg, quinidine, procainamide, disopyramide), and Class III antiarrhythmic agents (eg, amiodarone, sotalol, dofetilide)
- The use of macrolide antibiotics such as erythromycin should be avoided in patients receiving therapy; fatal torsades de pointes was reported in an elderly patient who received concomitant quinine, erythromycin, and dopamine
- Quinine may inhibit metabolism of certain drugs that are CYP3A4 substrates and are known to cause QT prolongation, eg, astemizole, cisapride, terfenadine, pimozide, halofantrine and quinidine; Torsades de pointes has been reported in patients who received concomitant quinine and astemizole
- Concomitant administration with antimalarial drugs, mefloquine or halofantrine, may result in electrocardiographic abnormalities, including QT prolongation, and increase the risk for torsades de pointes or other serious ventricular arrhythmias; concurrent use of mefloquine may increase the risk of seizures
- Treatment failures may result from concurrent use of rifampin, due to decreased plasma concentrations of quinine; concomitant use of these medications should be avoided
- The use of neuromuscular blocking agents should be avoided in patients receiving therapy; in one patient who received pancuronium during an operative procedure, subsequent administration of quinine resulted in respiratory depression and apnea; although there are no clinical reports with succinylcholine or tubocurarine, quinine may also potentiate neuromuscular blockade when used with these drugs
Pregnancy & Lactation
Pregnancy
No evidence that quinine causes uterine contractions at doses recommended for malaria treatment
May stimulate the pregnant uterus at doses several-times higher than those used to treat malaria
There are extensive published data but few well-controlled studies of quinine sulfate in pregnant women
Published data on over 1,000 pregnancy exposures to quinine did not show an increase in teratogenic effects over the background rate in the general population; however, the majority of these exposures were not in the first trimester
Used during pregnancy only if the potential benefit justifies the potential risk to the fetus
Clinical considerations
- Treatment of malaria in pregnancy is important
- P falciparum malaria carries a higher risk of morbidity and mortality in pregnant women than in the general population
- Pregnant women with P falciparum malaria have an increased incidence of fetal loss (including spontaneous abortion and stillbirth), preterm labor and delivery, intrauterine growth retardation, low birth weight, and maternal death
- Hypoglycemia, due to increased pancreatic secretion of insulin, associated with quinine use, particularly in pregnant women
Lactation
Low levels of quinine in breastmilk; amounts ingested by infant are small and would not be expected to cause any adverse effects
Dosage in milk is far below those required to treat an infant for malaria
Do not use in mothers with an infant who is glucose-6-phosphate dehydrogenase (G6PD) deficient
Relatively small amounts of quinine in tonic water ingested by breastfeeding women have caused hemolysis in G6PD-deficient infants
Pregnancy Categories
A: Generally acceptable. Controlled studies in pregnant women show no evidence of fetal risk.
B: May be acceptable. Either animal studies show no risk but human studies not available or animal studies showed minor risks and human studies done and showed no risk. C: Use with caution if benefits outweigh risks. Animal studies show risk and human studies not available or neither animal nor human studies done. D: Use in LIFE-THREATENING emergencies when no safer drug available. Positive evidence of human fetal risk. X: Do not use in pregnancy. Risks involved outweigh potential benefits. Safer alternatives exist. NA: Information not available.Pharmacology
Mechanism of action
Unknown; may disrupt Plasmodium DNA transcription/replication
Pharmacokinetics
Absorption: readily, mainly from upper small intestine
Protein Bound: 70-95%
Metabolism: primarily hepatic
Half-life elimination: children: 6-12 hr; adults: 8-14 hr
Peak Plasma Time: 1-3 hr
Excretion: feces & saliva; urine (<5% as unchanged drug)
Administration
Oral Administration
Take with food to minimize gastric upset
Missed dose: Instruct patient not to double the next dose; if >4 hr has elapsed since missed dose, patient should wait and take the next dose as previously scheduled
IV Administration
Was administered by slow IV infusion as the dihydrochloride; however, a parenteral dosage form of the drug no longer is available in the US
Storage
Capsules: Store at 20-25°C (68-77°F)
Images
| BRAND | FORM. | UNIT PRICE | PILL IMAGE |
|---|---|---|---|
| Qualaquin oral
-
|
324 mg capsule | 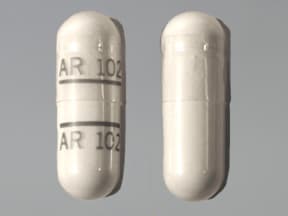 |
|
| quinine oral
-
|
324 mg capsule | 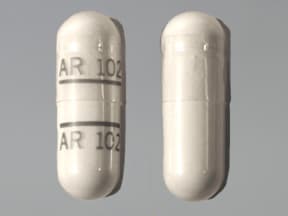 |
|
| quinine oral
-
|
324 mg capsule |  |
|
| quinine oral
-
|
324 mg capsule |  |
Copyright © 2010 First DataBank, Inc.
Patient Handout
quinine oral
QUININE SULFATE (ANTIMALARIAL) - ORAL
(KWEYE-nine SUL-fate)
COMMON BRAND NAME(S): Qualaquin
WARNING: The US Food and Drug Administration (FDA) warns that quinine should not be used to treat leg cramps. It has not been shown to work for this use and may cause serious side effects. Consult your doctor or pharmacist for more details.
USES: This medication is used alone or with other medication to treat malaria caused by mosquito bites in countries where malaria is common. Malaria parasites can enter the body through these mosquito bites, and then live in body tissues such as red blood cells or the liver. This medication is used to kill the malaria parasites living inside red blood cells. In some cases, you may need to take a different medication (such as primaquine) to kill the malaria parasites living in other body tissues. Both drugs may be needed for a complete cure and to prevent the return of infection (relapse). Quinine belongs to a class of drugs known as antimalarials. It is not used for the prevention of malaria.The United States Centers for Disease Control provide updated guidelines and travel recommendations for the prevention and treatment of malaria in different parts of the world. Discuss the most recent information with your doctor before traveling to areas where malaria occurs.
HOW TO USE: Read the Medication Guide and, if available, the Patient Information Leaflet provided by your pharmacist before you start taking quinine and each time you get a refill. If you have any questions, ask your doctor or pharmacist.Take this medication by mouth with food (to decrease upset stomach) as directed by your doctor, usually every 8 hours for 3 to 7 days.Take this medication 2 to 3 hours before or after taking antacids containing aluminum or magnesium. These products bind with quinine, preventing your body from fully absorbing the drug.The dosage and length of treatment are based on your medical condition, country where you were infected, other medications you may be taking for malaria, and your response to treatment. For children, the dosage is also based on weight.It is very important to continue taking this medication (and other malaria medications) exactly as prescribed by your doctor. Do not take more or less of this drug than prescribed. Do not skip any doses. Continue to take this medication until the full prescribed amount is finished, even if symptoms disappear after a few days. Skipping doses or stopping the medication too early may make the infection more difficult to treat and result in a return of the infection.This medication works best when the amount of drug in your body is kept at a constant level. Take this drug at evenly spaced intervals. To help you remember, take it at the same times each day.Tell your doctor if you do not start feeling better after 1 to 2 days of starting this medication. If your fever returns after completing this prescription, contact your doctor so that he/she can determine whether the malaria has returned.
SIDE EFFECTS: Mild headache, flushing, unusual sweating, nausea, ringing in the ears, decreased hearing, dizziness, blurred vision, and temporary changes in color vision may occur. If any of these effects last after your treatment is finished, or if these effects get worse while taking the medication, tell your doctor or pharmacist promptly.Quinine may cause low blood sugar (hypoglycemia), especially during pregnancy. Symptoms of low blood sugar include sudden sweating, shaking, fast heartbeat, hunger, blurred vision, dizziness, or tingling hands/feet. If symptoms of low blood sugar occur, increase your blood sugar by eating a quick source of sugar such as table sugar, honey, or candy, or drink fruit juice or non-diet soda. Tell your doctor right away about the reaction and the use of this product.Remember that this medication has been prescribed because your doctor has judged that the benefit to you is greater than the risk of side effects. Many people using this medication do not have serious side effects.Tell your doctor right away if you have any serious side effects, including: easy bruising/bleeding, unusual purple/brown/red spots on the skin, signs of serious infection (such as sore throat that doesn't go away, high fever, severe chills), signs of a sudden loss of red blood cells called hemolytic anemia (such as severe tiredness, brown urine, pale lips/nails/skin, rapid breathing at rest), signs of severe liver problems (such as nausea/vomiting that doesn't stop, abdominal pain, severe weakness, yellow skin/eyes, unusually dark urine), signs of kidney problems (such as change in the amount of urine).Get medical help right away if you have any very serious side effects, including: chest pain, severe dizziness, fainting, fast/irregular heartbeat, blindness.A very serious allergic reaction to this drug is rare. However, get medical help right away if you notice any symptoms of a serious allergic reaction, including: rash, itching/swelling (especially of the face/tongue/throat), severe dizziness, trouble breathing.This is not a complete list of possible side effects. If you notice other effects not listed above, contact your doctor or pharmacist.In the US -Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088 or at www.fda.gov/medwatch.In Canada - Call your doctor for medical advice about side effects. You may report side effects to Health Canada at 1-866-234-2345.
PRECAUTIONS: Before taking quinine, tell your doctor or pharmacist if you are allergic to it; or to quinidine or mefloquine; or if you have any other allergies. This product may contain inactive ingredients, which can cause allergic reactions or other problems. Talk to your pharmacist for more details.Before using this medication, tell your doctor or pharmacist your medical history, especially of: previous serious side effects with quinine (such as blood problems), family/personal history of a certain enzyme problem (glucose-6-phosphate dehydrogenase deficiency-G6PD), a certain eye nerve problem (optic neuritis), hearing problems (such as ringing in the ears), a certain nerve/muscle disease (myasthenia gravis), heart rhythm problems (such as atrial fibrillation/flutter), kidney problems, liver problems.This drug may make you dizzy or blur your vision. Alcohol or marijuana (cannabis) can make you more dizzy. Do not drive, use machinery, or do anything that needs alertness or clear vision until you can do it safely. Limit alcoholic beverages. Talk to your doctor if you are using marijuana (cannabis).Before having surgery, tell your doctor or dentist about all the products you use (including prescription drugs, nonprescription drugs, and herbal products).Quinine may cause a condition that affects the heart rhythm (QT prolongation). QT prolongation can rarely cause serious (rarely fatal) fast/irregular heartbeat and other symptoms (such as severe dizziness, fainting) that need medical attention right away.The risk of QT prolongation may be increased if you have certain medical conditions or are taking other drugs that may cause QT prolongation. Before using quinine, tell your doctor or pharmacist of all the drugs you take and if you have any of the following conditions: certain heart problems (heart failure, slow heartbeat, QT prolongation in the EKG), family history of certain heart problems (QT prolongation in the EKG, sudden cardiac death).Low levels of potassium or magnesium in the blood may also increase your risk of QT prolongation. This risk may increase if you use certain drugs (such as diuretics/"water pills") or if you have conditions such as severe sweating, diarrhea, or vomiting. Talk to your doctor about using quinine safely.Older adults may be more sensitive to the side effects of this drug, especially QT prolongation (see above).During pregnancy, this medication should be used only when clearly needed. Discuss the risks, benefits, and treatment options with your doctor. Untreated malaria is a serious condition that can harm both a pregnant woman and her unborn baby.This drug passes into breast milk. However, this drug is unlikely to harm some nursing infants. Your doctor will test your infant for a certain enzyme deficiency (glucose-6-phosphate dehydrogenase deficiency-G6PD) before you breastfeed. Consult your doctor before breastfeeding.
DRUG INTERACTIONS: See also How to Use section.Drug interactions may change how your medications work or increase your risk for serious side effects. This document does not contain all possible drug interactions. Keep a list of all the products you use (including prescription/nonprescription drugs and herbal products) and share it with your doctor and pharmacist. Do not start, stop, or change the dosage of any medicines without your doctor's approval.Some products that may interact with this drug include: "blood thinners" (such as warfarin), penicillamine.Other medications can affect the removal of quinine from your body, which may affect how quinine works. Examples include cimetidine, erythromycin, ketoconazole, phenytoin, rifampin, HIV protease inhibitors (such as lopinavir), ritonavir, urinary alkalinizers such as sodium bicarbonate, among others.This medication can slow down the removal of other medications from your body, which may affect how they work. Examples of affected drugs include desipramine, digoxin, certain "statin" drugs (atorvastatin, lovastatin, simvastatin), phenobarbital, among others.Many drugs besides quinine may affect the heart rhythm (QT prolongation), including amiodarone, dofetilide, mefloquine, pimozide, procainamide, quinidine, sotalol, macrolide antibiotics (such as erythromycin), among others. Before using quinine, report all medications you are currently using to your doctor or pharmacist.Quinine is very similar to quinidine. Do not use medications containing quinidine while using quinine.This medication may interfere with certain lab tests (such as certain urine tests for catecholamines, protein, steroids), possibly causing false test results. Make sure lab personnel and all your doctors know you use this drug.
OVERDOSE: If someone has overdosed and has serious symptoms such as passing out or trouble breathing, call 911. Otherwise, call a poison control center right away. US residents can call their local poison control center at 1-800-222-1222. Canada residents can call a provincial poison control center. Symptoms of overdose may include: sudden vision change, confusion, severe trouble hearing, fast/irregular heartbeat, fainting, slow/shallow breathing, seizures, inability to wake up (coma).
NOTES: Do not share this medication with others.Lab and/or medical tests (such as G6PD blood level, vision tests, blood potassium, liver/kidney function, EKG) may be done while you are taking this medication. Keep all medical and lab appointments. Consult your doctor for more details.
MISSED DOSE: If you miss a dose, take it as soon as you remember. If it is more than 4 hours after the missed dose, skip the missed dose. Take your next dose at the regular time. Do not double the dose to catch up.
STORAGE: Store at room temperature away from light and moisture. Do not store in the bathroom. Keep all medications away from children and pets.Do not flush medications down the toilet or pour them into a drain unless instructed to do so. Properly discard this product when it is expired or no longer needed. Consult your pharmacist or local waste disposal company.
Information last revised March 2024. Copyright(c) 2024 First Databank, Inc.
IMPORTANT: HOW TO USE THIS INFORMATION: This is a summary and does NOT have all possible information about this product. This information does not assure that this product is safe, effective, or appropriate for you. This information is not individual medical advice and does not substitute for the advice of your health care professional. Always ask your health care professional for complete information about this product and your specific health needs.
Formulary
Adding plans allows you to compare formulary status to other drugs in the same class.
To view formulary information first create a list of plans. Your list will be saved and can be edited at any time.
Adding plans allows you to:
- View the formulary and any restrictions for each plan.
- Manage and view all your plans together – even plans in different states.
- Compare formulary status to other drugs in the same class.
- Access your plan list on any device – mobile or desktop.





