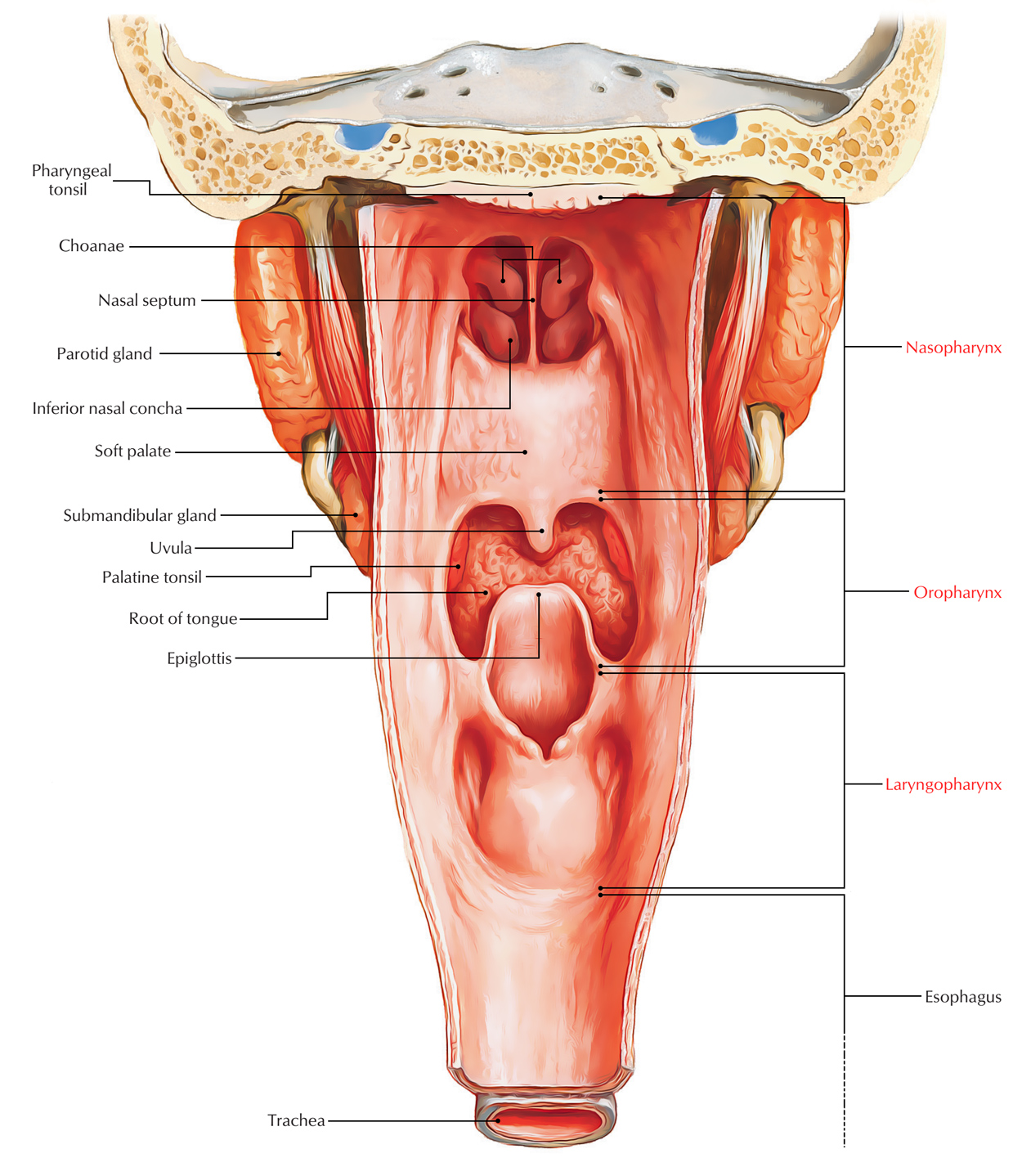
Stretching from the base of the skull to the esophagus, the pharynx is a funnel-shaped fibromuscular tube. It’s lined throughout with mucous membrane. For both food (deglutition) and air (respiration,) the pharynx functions as a mutual channel.
Measurements
- Length: 12-14 cm
- Width: 3.5 cm at its base and
- cm at pharyngoesophageal junction
Pharynx
Location
It’s situated behind the cavities of nose, mouth and the larynx with which it interacts
Borders and Relationships
Superior: Base of skull consisting of the posterior part of the body of sphenoid and basilar part of occipital bone in front of pharyngeal tubercle.
Inferior: Constant with the esophagus in the level of lower border of cricoid cartilage anteriorly and lower border of C6 vertebra posteriorly.
Posterior: Prevertebral fascia in front of cervical spine. The pharynx is divided from prevertebral fascia only by a layer of loose areolar tissue, which enables the pharynx to slip freely on this particular fascia during consuming.
Anterior: Opens into nasal cavities, mouth and larynx.
Lateral: Neurovascular bundle of neck and styloid process with its connected muscles and ligaments.
Subdivisions
The pharynx is split into 3 parts. From above downwards these are as follows:
- Nasopharynx, being located behind the nose.
- Oropharynx, being located behind the oral cavity.
- Laryngopharynx, being located behind the larynx.
You can study every section on individual post
Pharyngeal Wall
The wall of the pharynx is composed of 4 layers; from withinoutwards these are as follows:
Mucous membrane/mucous layer.
Pharyngobasilar fascia (pharyngeal aponeurosis).
Muscular coating (pharyngeal muscles).
Buccopharyngeal fascia (loose areolar sheath).
Mucous membrane/mucous layer: The mucous membranelining the pharynx includes a substantial amount ofelastic tissue and is constant with the mucous lining of eustachian tubes, nasal cavities, mouth, larynx and esophagus. It’s lined by non-keratinized stratified squamous epithelium with the exception of in the region of the nasopharynx, where it’s lined by ciliated columnar epithelium (respiratory epithelium).
There are lots of subendothelial collections of lymphoid tissue around the commencement of food and air passages, into which epithelium tends to invaginate in the create of narrow clefts (crypts).
These collections of lymphoid tissue create pharyngeal and tubal tonsils in the nasopharynx and palatine and lingual tonsils in the oropharynx.
Pharyngobasilar fascia: It’s a fibrous thickening of the submucosa. It lines the muscular layer and is thick near the base of the skull but thin and indistinct inferiorly. The pharyngobasilar fascia is thickest: in the upper part where it fills the gap between the upper border of superior constrictor and the base of the skull and posteriorly where it creates the pharyngeal raphe.
Muscular coating: The muscular layer includes the subsequent 2 layers of striated muscles:
The outer layer consists of 3 pairs of circular muscles termed constrictors.
The inner layer consists of 3 pairs of longitudinal muscles.
Buccopharyngeal fascia: It’s an inconspicuous fascia, which covers the outer surface of constrictor muscles. In the upper part, it’s also prolonged forwards to cover the buccinator muscles, for this reason the name buccopharyngeal fascia. Above the upper border of the superior constrictor, it mixes with the pharyngobasilar fascia.
Clinical Significance
Waldeyer’s ring: The aggregations of lymphoid tissue underneath the epithelial lining of pharyngeal wall referred to as tonsils, surround the commencement of air and food passages. These aggregations jointly make up an interrupted circle termed Waldeyer’s ring, which creates the specific attribute of the inside of the pharynx.
The Waldeyer’s ring is composed by:
- Pharyngeal tonsil (nasopharyngeal tonsil), postero superiorly.
- Lingual tonsil, anteriorly.
- Tubal and palatine tonsils, laterally.
It’s believed that, Waldeyer’s ring prevents the invasion of microorganisms from going into the air and food passages and this helps in the defense mechanism of the respiratory and alimentary systems.
Muscles of the Pharynx
Constrictor Muscles
The 3 constrictor muscles of the pharynx (superior, middle and inferior) are ordered like a flowerpot without base, set 1 above the other and open in front for communication together with the nasal, oral and laryngeal cavities. So inferior constrictor overlaps the middle, which in turn overlaps the superior constrictor.
The constrictor muscles create majority of the muscular layer of the pharyngeal wall. They originate in front from the margins of posterior openings of the nasal, oral and laryngeal cavities. The fibres pass backwards, in a fan-shaped way into the lateral and posterior walls of the pharynx to be added into the median fibrous raphe on the posterior aspect of the pharynx, going from the base of the skull (pharyngeal tubercle of occipital bone) to the esophagus.
Origin, Insertion, Nerve Supply and Activities of the Constrictor Muscles of the Pharynx
| MuscleMedian fibrous raphe | Origin | Insertion | Nerve supply | Action |
|---|---|---|---|---|
| Superior constrictor (Quadrilateral in shape) | Pterygoid hamulus Pterygomandibular raphe. Medial surface of the mandible at the upper end of mylohyoid line. Side of the posterior part of the tongue |
Pharyngeal tubercle on the base of skull Median fibrous raphe | Pharyngeal branch of the vagus nerve carrying fibres of cranial root of the accessory nerve | Helps in deglutition |
| Middle constrictor (Fan shaped | Lower part of the stylohyoid ligament Lesser cornu of hyoid Upper border of greater cornu of hyoid | Median fibrous raphe | Pharyngeal branch of the vagus nerve carrying fibres of cranial root of the accessory nerve | Helps in deglutition |
| Inferior constrictor (a)Thyropharyngeus | Oblique line on lamina of the thyroid cartilage Tendinous band between the thyroid (inferior) tubercle and cricoid cartilage | Median fibrous raphe | Pharyngeal plexus and External laryngeal nerve | Helps in deglutition |
| (b)Cricopharyngeus | Cricoid cartilage | Median fibrous raphe | Recurrent laryngeal nerve | |
Clinical Significance
Pharyngeal Pouch (also referred to as Zenker’s diverticulum).
Inferior constrictor muscle has 2 parts: thyropharyngeus created from oblique fibres and cricopharyngeus composed of transverse fibres.
The potential gap posteriorly between the thyropharyngeus and cricopharyngeus is referred to as pharyngeal dimple or Killian’s dehiscence. The mucosa and submucosa of the pharynx may bulge via this feeble area to create a pharyngeal pouch or diverticulum.
The formation of pharyngeal pouch in the region of Killian’s dehiscence is credited to the neuromuscular incoordination in this region, which might be because the 2 parts of the inferior constrictor have distinct Nerve Supply. The propulsive thyropharyngeus is supplied by the pharyngeal plexus and the sphincteric cricopharyngeus is supplied by the recurrent laryngeal nerve. If the cricopharyngeus doesn’t loosen when the thyropharyngeus contracts, the bolus of food is shoved backwards and tends to generate a diverticulum.
Gaps In The Pharyngeal Wall
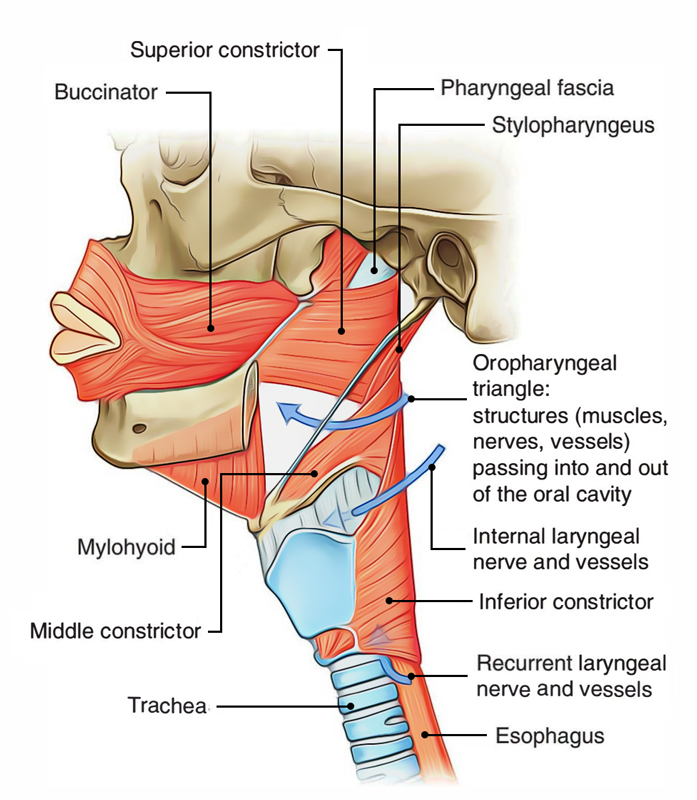
Pharynx: Muscles
| Gap | Structures passing through them |
|---|---|
| Between the base of skull and the upper concave border of superior constrictor (sinus of Morgagni) | Auditory tube Levator palati muscle Ascending palatine artery Palatine branch of the ascending pharyngeal artery |
| Between the superior and middle constrictors | Stylopharyngeus muscle Glossopharyngeal nerve |
| Between the middle and inferior constrictors | Internal laryngeal nerve Superior laryngeal vessels |
| Between the lower border of inferior constrictor and the esophagus (in the tracheo¬esophageal groove) | Recurrent laryngeal nerve Inferior laryngeal vessels |
Longitudinal Muscles
These muscles run longitudinally from above downwards to create the longitudinal muscle jacket.
Origin, Insertion and Nerve Supply of The Longitudinal Muscles of The Pharynx
| Muscle | Origin | Insertion | Nerve supply |
|---|---|---|---|
| Stylopharyngeus | Medial surface of the base of styloid process | Posterior border of the lamina of thyroid cartilage | Glossopharyngeal (IX) nerve |
| Palatopharyngeus | By two fasciculi (anterior and posterior) from the upper surface of the palatine aponeurosis | Posterior border of the lamina of thyroid cartilage | Cranial root of 11th cranial nerve by pharyngeal plexus |
| Salpingopharyngeus | Lower part of the cartilage of the Posterior border of the lamina of Cranial root of 11th cranial nerve by auditory tube thyroid cartilage pharyngeal plexus | ||
Activities of The Longitudinal Muscles
They elevate the larynx and shorten the pharynx during swallowing. At exactly the same time palatopharyngeal sphincter created by some fibres of the palatophayngeus muscle shuts the nasopharyngeal isthmus.
Nerve Supply of the Pharynx
Motor:
- All the pharyngeal muscles are supplied by the cranial root of accessory nerve (via pharyngeal branch of vagus and pharyngeal plexus), with the exception of the stylopharyngeus that is supplied by the glossopharyngeal nerve.
Sensory:
- Nasopharynx, by pharyngeal branch of the pterygo-palatine ganglion taking fibres from maxillary division of the trigeminal nerve.
- Oropharynx, by glossopharyngeal nerve.
- Laryngopharynx, by the internal laryngeal nerve.
Pharyngeal Plexus of the Nerves
It is located on the posterolateral aspect of the pharynx over the middle constrictor underneath the buccopharyngeal fascia.
It’s created by:
- Pharyngeal branch of the vagus nerve taking fibres from cranial part of the accessory nerve.
- Pharyngeal branch of the glossopharyngeal nerve.
- Pharyngeal branch from superior cervical sympathetic ganglion.
Arterial Supply of the Pharynx
The branches of these arteries supply the pharynx:
- Ascending pharyngeal artery (from external carotid artery).
- Ascending palatine and tonsillar artery (from facial artery).
- Greater palatine and pharyngeal artery (from maxillary artery).
- Lingual artery (from external carotid artery).
Venous Drainage of the Pharynx
The venous blood from pharynx is mainly emptied into pharyngeal venous plexus, which, such as the pharyngeal nerve plexus, is situated on the posterolateral aspect of the pharynx over the middle constrictor. It drains into the internal jugular vein.
Lymphatic Drainage of The Pharynx
The lymph from pharynx is drained into the upper and lower deep cervical lymph nodes directly and via retropharyngeal lymph nodes.
Deglutition (Consuming)
The deglutition is a process or action by which the food is transferred from the mouth to the stomach. It is composed of the following 3 consecutive stages/phases:
- First phase (in the mouth) voluntary.
- Second phase (in the pharynx) involuntary.
- Third phase (in the esophagus) involuntary.
First Period
In this phase the mouth is closed, the anterior part of tongue is lifted against the hard palate anterior to the bolus of food to shove the masticated food increasingly in the posterior part of the oral cavity. The soft palate closes down onto the rear of the tongue to help create bolus of food. Now the hyoid bone moves up and food is shoved from oral cavity to the oropharynx via oropharyngeal isthmus.
Second Period
This phase is extremely accelerated. The nasopharyngeal isthmus is closed by the elevation of the soft palate and contraction of Passavant’s ridge to stop entrance of food into the nasopharynx. The laryngeal inlet is closed by approximation of the aryepiglottic folds to stop entrance of food into the larynx. Now the pharynx and larynx are elevated behind the hyoid bone by the longitudinal muscles of the pharynx and the bolus of food is shoved down over the posterior surface of the epiglottis by gravity and contraction of superior and middle constrictors. So food enters from the oropharynx to the laryngopharynx. This is followed by quick downward displacement of the larynx and pharynx (by infrahyoid muscles), which reopens the laryngeal orifice.
Third Period
In this phase, propulsive activity of thyropharyngeus followed by relaxation of cricopharyngeus shoves food, which enters from laryngopharynx to the esophagus. From here it enters into the stomach by peristaltic movements in the esophageal wall.
Pharyngeal Spaces
All these are potential spaces in regard to pharynx, viz.
Retropharyngeal space: It’s situated behind the pharynx and goes from the base of the skull above to the bifurcation of trachea below.
Parapharyngeal space: It’s situated on the side of the pharynx. It includes carotid vessels, internal jugular vein, last 4 cranial nerves and cervical sympathetic chain.
Palatine Tonsils
There are 2 palatine tonsils (usually named tonsils). Every tonsil is an almond shaped mass of lymphoid tissue situated in the triangular fossa (tonsillar fossa) of the lateral wall of the oropharynx between the anterior and posterior columns of fauces. The anterior column is composed by palatoglossal arch and posterior column is composed by palatopharyngeal arch.
The genuine size of tonsil is a lot bigger than it seems on oropharyngeal evaluation because parts of tonsil go upwards into the soft palate, downwards in the base of the tongue and anteriorly underneath the palatoglossal arch.
Observe PALATINE TONSILS for details.

 (53 votes, average: 4.89 out of 5)
(53 votes, average: 4.89 out of 5)