Abstract
Aims/hypothesis
Although much is known about the pathophysiological processes contributing to diabetic retinopathy (DR), the role of protective pathways has received less attention. The transcription factor nuclear factor erythroid-2-related factor 2 (also known as NFE2L2 or NRF2) is an important regulator of oxidative stress and also has anti-inflammatory effects. The objective of this study was to explore the potential role of NRF2 as a protective mechanism in DR.
Methods
Retinal expression of NRF2 was investigated in human donor and mouse eyes by immunohistochemistry. The effect of NRF2 modulation on oxidative stress was studied in the human Müller cell line MIO-M1. Non-diabetic and streptozotocin-induced diabetic wild-type and Nrf2 knockout mice were evaluated for multiple DR endpoints.
Results
NRF2 was expressed prominently in Müller glial cells and astrocytes in both human and mouse retinas. In cultured MIO-M1 cells, NRF2 inhibition significantly decreased antioxidant gene expression and exacerbated tert-butyl hydroperoxide- and hydrogen peroxide-induced oxidative stress. NRF2 activation strongly increased NRF2 target gene expression and suppressed oxidant-induced reactive oxygen species. Diabetic mice exhibited retinal NRF2 activation, indicated by nuclear translocation. Superoxide levels were significantly increased by diabetes in Nrf2 knockout mice as compared with wild-type mice. Diabetic Nrf2 knockout mice exhibited a reduction in retinal glutathione and an increase in TNF-α protein compared with wild-type mice. Nrf2 knockout mice exhibited early onset of blood–retina barrier dysfunction and exacerbation of neuronal dysfunction in diabetes.
Conclusions/interpretation
These results indicate that NRF2 is an important protective factor regulating the progression of DR and suggest enhancement of the NRF2 pathway as a potential therapeutic strategy.
Similar content being viewed by others
Introduction
Diabetic retinopathy (DR) is the leading cause of blindness in working-age adults worldwide [1]. With an estimated prevalence of 93 million people, including 28 million with vision-threatening retinopathy, DR may become the leading cause of visual impairment in the world [2]. The pathogenesis of DR is multi-faceted, including oxidative stress [3], pro-inflammatory changes [4, 5] and advanced glycation end products [6]. These processes lead to dysfunction of multiple retinal cell types, including the vasculature and neuroretina [4, 5, 7, 8].
Research into DR has largely focused on the identification of pathogenic molecules such as vascular endothelial growth factor (VEGF). There is a growing awareness of the importance of identifying protective pathways, the activity of which could be augmented in patients with DR. It is increasingly appreciated that diabetic vascular complications result from an imbalance between causal (harmful) factors and protective factors [9, 10]. This suggests that new therapeutic strategies for DR, including both vascular and neuronal protection, should focus on enhancing the action of endogenous protective mechanisms in addition to inhibiting pathogenic mechanisms [9, 10].
The involvement of oxidative stress and pro-inflammatory changes in DR leads us to consider nuclear factor erythroid-2-related factor 2 (also known as NFE2L2 or NRF2), since it regulates both processes. NRF2 is a transcription factor that protects cells from endogenous and exogenous stresses [11, 12]. NRF2 is considered to be part of the most important cellular pathway protecting against oxidative stress [11, 12], and it also has an important role as a negative regulator of inflammation, attenuating inflammation-associated pathogenesis in multiple disease conditions [13–15]. Overall, NRF2 has been implicated as an important protective factor, especially in disease processes in which reactive oxygen species (ROS) and inflammation play a critical role.
Importantly, evidence is accumulating regarding a potential protective role for NRF2 in the retina [16, 17]. We found NRF2 to have a cytoprotective role for both neurons and vasculature following retinal ischaemia–reperfusion injury [17]. Intriguingly, NRF2 has been found to be protective in the context of diabetic disease, especially diabetic nephropathy. Nrf2 knockout mice (Nrf2 −/−) displayed significantly greater renal injury compared with wild-type mice (Nrf2 +/+) in a streptozotocin (STZ)-induced model of diabetes [18]. Therapeutic activation of NRF2 had beneficial effects against diabetic kidney disease in rodents [19]. In this study we investigated whether NRF2 might have a beneficial role in suppressing the progression of DR. Using a loss of function strategy with genetic ablation of NRF2, we found evidence supporting the involvement of NRF2 in a protective mechanism against multiple endpoints that model DR in mice.
Methods
Human tissue
Human donor eyes were fixed in 10% neutral buffered formalin for at least 24 h before paraffin embedding and subsequent sectioning. Unstained sections from human donor eyes were obtained from the Wilmer Eye Institute Ophthalmic Pathology laboratory with Institutional Review Board approval. All eyes were fixed within 18 h postmortem.
Immunohistochemistry
Deparaffinised sections were boiled in 1× target retrieval solution (Dako, Carpinteria, CA, USA) for 20 min. Anti-NRF2 antibody (No. 2178-1; Epitomics, Burlingame, CA, USA) and isotype- and concentration-matched IgG control (ISO-2178; Epitomics) were used for incubation at 4°C overnight. Secondary biotinylated goat anti-rabbit IgG and ABC reagent (Vector Labs, Burlingame, CA, USA) were applied to the sections. Vector blue AP substrate kit III (Vector Labs) was used to stain the sections. Sections were also counter-stained with nuclear fast red (Vector Labs).
Cell culture, small interference RNA (siRNA) transfection, quantitative PCR and western blot analysis
The human Müller glial cell line MIO-M1 [20] was cultured in DMEM plus 10% FBS and 1% GlutaMAX-I supplement (Invitrogen, Grand Island, NY, USA). Sub-confluent MIO-M1 cells were transfected with negative control No. 2 siRNA, NRF2 siRNA (s9493) and KEAP1 siRNA (s18983) (Applied Biosystems, Foster city, CA, USA) using Lipofectamine 2000 for 48 h. Total RNA was isolated using the RNeasy mini kit (Qiagen, Valencia, CA, USA) and single-stranded cDNA was synthesised using MMLV Reverse Transcriptase (Invitrogen). Quantitative PCR (qPCR) was performed using the QuantiTect SYBR Green PCR Kit (Qiagen) with a StepOnePlus real-time PCR system (Applied Biosystems). The qPCR primers were as follows: NQO1: (5′-CAGCTCACCGAGAGCCTAGT-3′) and (5′-ACCACCTCCCATCCTTTCTT-3′); GCLC: 5′-ACCATCATCAATGGGAAGGA-3′) and (5′-GCGATAAACTCCCTCATCCA-3′); HO-1: (5′-ATGACACCAAGGACCAGAGC-3′) and (5′-GTGTAAGGACCCATCGGAGA-3′); β-actin: (5′-AGAAAATCTGGCACCACACC-3′) and (5′-GGGGTGTTGAAGGTCTCAAA-3′). For western blot analysis, anti-NRF2 (Epitomics), anti-NQO1 (Cell Signaling Technology, Danvers, MA, USA), anti-HO-1 (Enzo Life Science International, Farmingdale, NY, USA) and anti-β-actin antibodies (Cell Signaling Technology) were used. For analysis of NRF2 nuclear translocation, nuclear extracts from mouse retinas were prepared using NE-PER Nuclear and Cytoplasmic Extraction Reagents (ThermoFisher Scientific, Waltham, MA, USA). Rabbit monoclonal NRF2 antibody (Cell Signaling Technology) and Lamin B antibody (Santa Cruz Biotechnology, Dallas, Texas, USA) were used. The band intensity was quantified using the Image J program (version 1.47, NIH, http://imagej.nih.gov/ij/).
Dichlorofluorescein assay
ROS production was quantified by the dichlorofluorescein (DCF) assay. Forty-eight hours after siRNA transfection, MIO-M1 cells were treated with or without different doses of tert-butyl hydroperoxide (TBH, Sigma, St Louis, MO, USA) and hydrogen peroxide (H2O2, Sigma) for 1 h. CM-H2DCFDA (10 μmol/l, Invitrogen) was then added and the cells were incubated for 30 min. DCF fluorescence was measured with a spectrophotometer (BMG Labtech, Durham, NC, USA).
Animals and treatments
Nrf2 −/− and Nrf2 +/+ mice on a C57BL/6 background [21, 22] were used for all experiments. Experimental diabetes was induced in 8-week-old male mice by intraperitoneal injection of STZ (45 mg/kg body weight in 10 mmol/l of citrate buffer, pH 4.5) for 5 consecutive days, as described [23]. Mice were considered diabetic when the blood glucose level was higher than 13.89 mmol/l. All animal procedures were approved by the Institutional Animal Care and Use Committee of the Johns Hopkins University School of Medicine and conducted in accordance with the Association for Research in Vision and Ophthalmology Statement for the Use of Animals in Ophthalmic and Vision Research.
Immunofluorescence analysis of mouse retinal frozen cryosections
Cryosections (10 μm) of mouse eyes were fixed in 4% paraformaldehyde. Anti-NRF2 (R&D Systems, Minneapolis, MN, USA), anti-glial fibrillary acidic protein (GFAP) (ThermoFisher Scientific) and anti-Vimentin (Sigma) antibodies were used. Alexa fluor 488-, Alexa fluor 594- (Invitrogen) or Cy3- (Jackson ImmunoResearch, West Grove, PA, USA) conjugated IgG were used as secondary antibodies. DAPI (Invitrogen) was used to stain nuclei. Photographs were taken with a Zeiss LSM 710 confocal microscope (Carl Zeiss Microscopy, Thornwood, NY, USA).
Lucigenin assay
Superoxide anion in the retina was quantified by lucigenin assay as described [24]. Fresh retinas were placed in 0.2 ml Krebs/HEPES buffer and incubated in the dark at 37°C under 5% CO2 for 10 min. Lucigenin (Sigma) was added to a final concentration of 0.5 mmol/l and photon emission was measured over 10 s with a luminometer three times (Analytical Luminescence Laboratory, San Diego, CA, USA). Retinas were then sonicated in 200 μl RIPA lysis buffer (Sigma). Protein concentration was measured by DC protein assay (BioRad, Hercules, CA, USA) and used to normalise the final superoxide level.
Glutathione assay
Retinas were sonicated in 0.5 mmol/l PB buffer (pH 6.8 and 1 mmol/l EDTA). The samples were cleared by centrifugation at 10,000 g for 15 min. Retinal protein extract (18 μg) was deproteinised and assayed with a glutathione (GSH) assay kit (Cayman Chemical, Ann Arbor, Michigan, USA). 5,5′-Dithio-bis-2-(nitrobenzoic acid (DTNB) was added to the extract to react with GSH and produce a yellow-coloured 5-thio-2-nitrobenzoic acid (TNB). After incubation for 25 min, the absorbance of TNB was measured at 405 nm using a microplate reader (Epoch BioTek, Winooski, VT, USA).
ELISA for TNF-α
Retinas were sonicated in 0.1% Triton X-100 in PBS supplemented with a mixture of protease inhibitors (Invitrogen). The samples were cleared of debris by centrifugation at 12,000 g for 10 min and then assessed for protein concentration. TNF-α levels were measured using an ELISA kit (R&D Systems). The TNF-α concentration was calculated from a standard curve and corrected for total protein concentration.
Blood–retina barrier assay
The blood–retina barrier (BRB) assay was performed as described [25, 26]. Mice were given an intraperitoneal injection of 37,000 Bq/g body weight of [3H]mannitol. One hour after injection, mice were sedated and retinas rapidly removed and dissected to free the lens, vitreous and retinal-pigment epithelium. Retinal dry weight was measured. One millilitre of NCSII solubilising solution (GE Healthcare, Piscataway, NJ, USA) was added to each sample, and the samples were incubated overnight at 50°C. Solubilised tissue was brought to room temperature and decolourised with 20% benzoyl peroxide in toluene at 50°C. After re-equilibration to room temperature, 5 ml of scintillation fluid cytoscint ES (ThermoFisher Scientific) and 30 μl of glacial acetic acid were added. Samples were stored for several hours in darkness at 4°C to eliminate chemoluminescence. Radioactivity was counted with a scintillation counter (LS 6500 Liquid Scintillation Counter; Beckman-Coulter, Indianapolis, IN, USA). The cpm of retina tissue from Nrf2 −/− and Nrf2 +/+ groups were measured and normalised to the dry weight of each retina.
Behavioural assessment of visual thresholds in mice
A virtual optomotor system [27] (OptomotryTM; Cerebral Mechanics, White Plains, NY, USA) was used to assess visual function in diabetic and non-diabetic mice. The apparatus has four inward-facing LCD panels arranged in a square around an elevated testing platform (7 cm diameter). A moving vertical sine wave grating is displayed on the monitors, creating an illusion of a virtual cylinder rotating at 12°/s around the testing platform. A video camera mounted to the top lid of the apparatus reports to a computer program, enabling the experimenter to score the test animal’s optokinetic reflex response to the moving grating.
The spatial frequency (SF) threshold and contrast sensitivity (CS) were assessed in awake, freely moving mice. When mice were able to see the moving target, their head and upper body tracked the grating pattern. SF (cycles/degree) was always measured at maximum contrast (100%) by using a staircase method beginning with a minimum preset frequency of 0.072 cycles/degree. The contrast threshold (%) was measured at an SF of 0.092 cycles/degree. CS threshold was calculated as the reciprocal of the CS score. The SF threshold and CS were identified as the highest values that still elicited a response in the mouse. Twenty-three mice were used for visual threshold testing. Both SF and CS were averaged over three trials on consecutive days for each mouse.
Retinal thickness and cell count in ganglion cell layer
Cross-sections cut through the optic nerve were prepared and stained with hematoxylin and eosin for retinal morphology examination. Three cryosections from each retina and six locations in the retina from each cryosection (three locations on each side of the optic nerve) were quantified with respect to nuclei in the ganglion cell layer (GCL) (excluding nuclei of blood vessels) and the thickness of the inner nuclear layer (INL) and outer nuclear layer (ONL), under 400× magnification with Zeiss AxioVision software (AxioVS40 V4.7.2.0, Carl Zeiss) [28].
Statistical analysis
Data were presented as means ± SD, and were analysed by using non-parametric Mann–Whitney test for in vivo studies and two-tailed Student’s t test for cell culture studies. A value of p < 0.05 was considered statistically significant.
Results
NRF2 is expressed in human retinas
We first investigated the expression and localisation of NRF2 in human retinas. Immunohistochemical staining for NRF2 was performed using human ocular sections. Retinas showed prominent NRF2 immunoreactivity in Müller cells spanning the retina. There was also prominent immunoreactivity in the nerve fibre layer and GCL in the cells that were morphologically consistent with astrocytes, microglia and ganglion cells (Fig. 1a). Staining was also observed in vascular endothelial cells, although relatively weak (see electronic supplementary material [ESM] Fig. 1). Normal control IgG did not give any positive staining (Fig. 1b). Immunostaining of NRF2 in mouse retina showed co-localisation of NRF2 with Vimentin (Müller glia marker) (Fig. 1c) and GFAP (astrocyte marker) (Fig. 1d), indicating that NRF2 was strongly expressed in retinal glial cells. NRF2 showed similar localisation in diabetic retinas and non-diabetic control retinas (data not shown).
Expression of NRF2 in human and mouse retinas. Paraffin-embedded human retinal sections were immunostained with NRF2 antibody (blue) and counter-stained with nuclear fast red. (a) Retina from donors showed NRF2 immunoreactivity in Müller cells spanning the retina. NRF2 was also expressed in the GCL. Arrows indicate Müller cell processes and asterisks indicate the nerve fibre layer. (b) Negative immunohistochemical staining in human retina with rabbit control IgG. The images are representative of eight donors and were taken at 20× objective. (c) Mouse retinal cryosections were analysed by immunofluorescence for NRF2 (green) and Vimentin (red). (d) Mouse retinal cryosections were analysed by immunofluorescence for NRF2 (green) and GFAP (red). (e) Immunofluorescence for control IgG (green). DAPI (blue) was used to stain nuclei in all retinal sections
NRF2 has a protective effect in human Müller cells against oxidant-induced oxidative stress
To determine whether NRF2 could be beneficial for retinal cells against oxidative stress, we used siRNA to modulate NRF2. We used an adult human Müller glial cell culture system because of the strong expression of NRF2 in Müller cells (Fig. 1) and the important role of Müller cells in DR [29, 30]. Kelch-like ECH-associated protein 1 (KEAP1) is a major repressor of NRF2 that interacts with NRF2 and mediates its ubiquitination and proteolysis. We first confirmed that transfecting NRF2 siRNA and KEAP1 siRNA efficiently decreased and increased, respectively, NRF2 protein levels in MIO-M1 cells (Fig. 2b). NRF2 siRNA significantly decreased mRNA levels of the NRF2 target genes NQO1 and GCLC (n = 4, p < 0.05). KEAP1 knockdown significantly increased the expression of established NRF2-target antioxidant genes, including NQO1, GCLC, GCLM and HO-1 (also known as HMOX1) from 1.6- to 3.4-fold (n = 4, p < 0.01) (Fig. 2a). Western blot analysis further confirmed elevation of NQO1 and HO-1 protein levels in KEAP1 siRNA-transfected MIO-M1 cells (Fig. 2b). To evaluate whether NRF2 knockdown or activation, respectively, regulates oxidative stress, we treated MIO-M1 cells with two oxidants, TBH and H2O2. As shown in Fig. 2c, TBH (10–100 μmol/l) and H2O2 (50–200 μmol/l) significantly increased ROS in MIO-M1 cells compared with PBS control in a dose-dependent fashion. NRF2 knockdown exacerbated TBH- and H2O2-increased ROS (Fig. 2c). Conversely, NRF2 activation by KEAP1 knockdown significantly reduced both TBH and H2O2 induction of ROS.
NRF2 protects against oxidant-induced ROS increase in human Müller cells. (a) Relative expression of NRF2-responsive antioxidant genes in MIO-M1 cells after 48 h of NRF2 siRNA and KEAP1 siRNA transfection. White bars, control siRNA; grey bars, NRF2 siRNA; black bars, KEAP1 siRNA. n = 4; *p < 0.05, **p < 0.01. (b) Western blot analysis of NRF2, NQO1 and HO-1 expression after 48 h of NRF2 siRNA and KEAP1 siRNA transfection. (c) The effect of knocking down NRF2 or KEAP1 on different oxidant-induced ROS increase in MIO-M1 cells. Forty-eight hours after siRNA transfection, cells were challenged by different doses of TBH or H2O2 for 1 h. ROS levels were determined by DCF assay. White bars, control siRNA; grey bars, NRF2 siRNA; black bars, KEAP1 siRNA. n = 4; *p < 0.05 and **p < 0.01 vs control siRNA with PBS treatment; † p < 0.05, ‡ p < 0.05 and ‡‡ p < 0.01 vs control siRNA with respective treatment
Body weight and blood glucose level of STZ-induced diabetic and control mice
The protective role of NRF2 in cultured Müller glial cells encouraged us to investigate whether NRF2 is involved in a protective pathway in a mouse model of DR, using wild-type and Nrf2 −/− mice. After 8 weeks of diabetes, diabetic mice from both wild-type and Nrf2 −/− groups weighed significantly less than their respective control groups (p < 0.001). Blood glucose levels in the diabetic groups of mice were significantly higher than in their respective control groups (p < 0.001). The weight and blood glucose levels were not significantly different when comparing wild-type mice and Nrf2 −/− mice, under both diabetic and non-diabetic conditions (Table 1).
Nrf2 was activated in the retinas of STZ-induced diabetic mice
Nuclear translocation of NRF2 [11] was evaluated to determine whether NRF2 was activated or inactivated during diabetes. There was an approximately twofold (n = 6, p < 0.01) increase of nuclear NRF2 in wild-type diabetic mice compared with non-diabetic controls (Fig. 3) after 8 weeks of diabetes, which indicated that NRF2 was activated during diabetes. We observed no difference in levels of total retinal NRF2 protein between diabetic and non-diabetic mice at 8 weeks of diabetes (data not shown).
Nuclear translocation of NRF2 in diabetic mouse retinas. (a) Western blot analysis of NRF2 with retina nuclear extract from wild-type mice after 8 weeks of diabetes. Lamin B was used as a loading control. (b). Quantitative analysis of nuclear NRF2 protein level. The intensity of NRF2 is presented relative to Lamin B in the same sample and normalised to non-diabetic control retinas. n = 6 for each group; **p < 0.01
NRF2 deficiency increased retinal ROS levels in STZ-induced diabetic mice
To implicate NRF2 as being part of a protective mechanism in DR, we used a loss of function strategy with genetic ablation of NRF2 in mice. We first investigated the role of NRF2 in regulating diabetes-induced oxidative stress, as measured by superoxide generation. Retinas were extracted from non-diabetic and diabetic mice and superoxide levels were measured by lucigenin assay [24]. Retinal superoxide was significantly increased in diabetic Nrf2 −/− mice compared with wild-type mice after 5 weeks of diabetes (Fig. 4).
NRF2-deficient mice exhibit increased oxidative stress in early diabetes. Fresh retinas were isolated from wild-type mice and Nrf2 −/− mice after 5 weeks of diabetes. The level of retinal superoxide was determined by lucigenin assay. White bars, non-diabetic control mice; black bars, diabetic mice. Non-diabetic Nrf2 +/+ mice, n = 6; diabetic Nrf2 +/+ mice, n = 7; non-diabetic Nrf2 −/− mice, n = 6; diabetic Nrf2 −/− mice, n = 5; *p < 0.05, **p < 0.01
GSH is a vital antioxidant that regulates cellular redox status, and NRF2 plays a key role in regulating cellular GSH homeostasis [11]. Retinas were extracted from diabetic mice for measurement of GSH levels [31]. There was no significant difference in GSH levels in non-diabetic control groups between wild-type and Nrf2 −/− mice (Fig. 5). Retinal GSH levels were significantly lower in diabetic Nrf2 −/− mice compared with wild-type diabetic mice (p < 0.05) (Fig. 5).
NRF2-deficient diabetic mice exhibit lower retinal GSH levels compared with wild-type diabetic mice. GSH levels were measured in retinal protein lysates from wild-type and Nrf2 −/− mice after 8 weeks of diabetes using a GSH assay kit. White bars, non-diabetic control mice; black bars, diabetic mice. n = 7 for each group; *p < 0.05
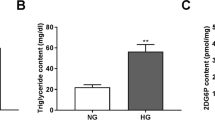
Effect of NRF2 deficiency on diabetes-induced TNF-α expression
TNF-α is thought to play an important role in DR, including BRB dysfunction [26, 32]. Since NRF2 is known to have an anti-inflammatory effect in the retina, including modulation of pro-inflammatory cytokines [16, 17], we investigated its potential effect on retinal levels of TNF-α in wild-type and Nrf2 −/− mice. ELISA results showed that there was no difference in TNF-α in wild-type diabetic mice after 8 weeks of diabetes compared with wild-type controls. In contrast, there was a significantly greater amount of TNF-α protein in diabetic Nrf2 −/− mice compared with their control group (p < 0.05) (Fig. 6).
NRF2-deficient mice exhibit increased retinal TNF-α protein levels in diabetes. After 8 weeks of diabetes, retinas were isolated and processed for TNF-α ELISA assay. White bars, non-diabetic control mice; black bars, diabetic mice. Non-diabetic Nrf2 +/+ mice, n = 10; diabetic Nrf2 +/+ mice, n = 14; non-diabetic Nrf2 −/− mice, n = 10, diabetic Nrf2 −/− mice, n = 8; *p < 0.05; **p < 0.01
Effect of NRF2 deficiency on retinal vascular permeability in diabetic mice
BRB breakdown is a major pathological change in DR, leading to retinal oedema and loss of vision. We investigated the effect of NRF2 deficiency on retinal vascular leakage in the STZ-induced diabetes model. We employed a protocol using [3H]mannitol as a tracer [25, 26] to measure the amount of mannitol leaked by the retinal blood vessels into the surrounding retina. There was a significant increase in retinal vascular leakage in the Nrf2 −/− mice after 8 weeks of diabetes as compared with wild-type diabetic mice (p < 0.05) (Fig. 7).
NRF2-deficient mice exhibit earlier onset of BRB dysfunction in diabetes. BRB dysfunction was determined in Nrf2 +/+ and Nrf2 −/− mice after 8 weeks of diabetes. Radioactivity per mg of retina was measured 1 h after intraperitoneal injection of [3H]mannitol. White bars, non-diabetic control mice; black bars, diabetic mice. Non-diabetic Nrf2 +/+ mice, n = 4; diabetic Nrf2 +/+ mice, n = 5; non-diabetic Nrf2 −/− mice, n = 4; diabetic Nrf2 −/− mice, n = 4; *p < 0.05; **p < 0.01
NRF2 deficiency exacerbated diabetes-induced visual dysfunction in mice
In addition to its effects on the retinal vasculature, diabetes is known to have adverse effects on neuronal function in the retina, including consequences on visual function [33]. In rodent models of diabetes, diabetes-induced neuroretinal dysfunction has been detected using tests of electrical activity [34, 35] as well as direct assessment of visual function by measurement of the optokinetic response [35]. Since NRF2 has neuroprotective effects in the retina [17], we analysed visual function in non-diabetic and diabetic Nrf2 −/− and Nrf2 +/+ mice. We used a virtual optomotor system that allows precise quantification of both SF thresholds and CS [27]. After 8 weeks of diabetes, Nrf2 −/− mice had significant visual deficits in both SF and CS as compared with age-matched non-diabetic Nrf2 −/− controls (p < 0.05) and diabetic wild-type mice (p < 0.01; Fig. 8). Diabetic Nrf2 +/+ mice also had a significantly lower SF threshold compared with non-diabetic Nrf2 +/+controls (p < 0.05; Fig. 8a). There was a trend toward reduction in CS in diabetic Nrf2 +/+ mice compared with non-diabetic Nrf2 +/+ controls, but this did not reach statistical significance (Fig. 8b).
NRF2-deficient mice have increased visual dysfunction induced by diabetes. After 8 weeks of diabetes, the SF (a) and CS (b) thresholds were obtained in wild-type and Nrf2 −/− mice using Optomotry optokinetic testing. White bars, non-diabetic control mice; black bars, diabetic mice. Non-diabetic Nrf2 +/+ mice, n = 6; diabetic Nrf2 +/+ mice, n = 6; non-diabetic Nrf2 −/− mice, n = 6; diabetic Nrf2 −/− mice, n = 4; *p < 0.05 and **p < 0.01
Retinal morphology and integrity were examined in cryosections using haematoxylin and eosin staining, and no differences were found when comparing all four groups (ESM Fig. 2). There was no significant difference in the number of cells in the GCL between non-diabetic and diabetic Nrf2 +/+ mice (Table 2), or between diabetic Nrf2 +/+ and Nrf2 −/− mice (Table 2). There were no significant differences in INL and ONL thickness between all four groups (Table 2). TUNEL and immunostaining of cleaved caspase 3 were also performed to detect any cell apoptosis in the retina. After 8 weeks of diabetes, we did not detect any observable apoptosis in Nrf2 +/+ or Nrf2 −/− diabetic mice (ESM Fig. 3). Overall, this indicates a diabetes-induced neuronal dysfunction at this stage of diabetes, in the absence of overt retinal neuronal death.
Discussion
Although research into DR has largely focused on the identification of pathogenic molecules, there is a growing awareness of the importance of identifying protective pathways [9, 10]. This is highlighted by studies indicating protection from retinopathy in some individuals with very long-standing diabetes [36]. Our group reported a retinal cytoprotective role for NRF2 in ischaemia–reperfusion injury, in which it inhibited both oxidative stress and pro-inflammatory changes [17]. Since both these pathophysiological processes are thought to be critical contributors to DR, we were interested in investigating NRF2 as part of a potential protective mechanism in DR.
Although NRF2 has received significant attention in systemic settings, including the lung, there has been less investigation of NRF2 in the retina. We therefore first determined whether NRF2 is expressed in human retina. NRF2 immunohistochemistry disclosed staining in multiple cell types, including prominent staining in Müller glial cells. Although it is clear that multiple cell types play a role in DR, the Müller glial staining was intriguing given the increasing awareness of its role in DR [29, 30]. These previous studies indicate that the Müller glia may be an important driver in the progression of DR, including involvement in pro-inflammatory effects and production of TNF-α and VEGF. Our studies with cultured human Müller glial cells were therefore very encouraging in suggesting a protective role for NRF2 against oxidative stress. To determine whether NRF2 is part of a protective mechanism in DR, we used a loss of function strategy with Nrf2 −/− mice. Our studies indicate that NRF2 does indeed have a protective role in the retina with regard to retinal superoxide, GSH and TNF-α levels. The induction of oxidative stress is considered to be a key pathophysiological process in DR, and superoxide generation is thought to be especially critical [7, 37]. In addition, it is increasingly appreciated that pro-inflammatory processes contribute to DR [4, 5]. TNF-α is thought to be one of the important contributing cytokines [26, 32], with both microglia [38] and Müller cells [29] implicated as important sources in DR.
A crucial endpoint in DR is BRB dysfunction, which contributes to diabetic macular oedema, the most common cause of vision loss in diabetes [39]. There is strong evidence to suggest a role for both oxidative stress and pro-inflammatory cytokines in BRB dysfunction in DR [39, 40]. There is much support for the role of inflammatory cytokines, including TNF-α in producing BRB dysfunction in diabetes [39]. Our studies indicating the protective effect of NRF2 against oxidative stress and TNF-α expression therefore suggest that it might be protective against retinal vascular permeability in DR. Indeed, we found this to be the case, such that Nrf2 −/− mice had significant BRB dysfunction at a time where BRB dysfunction was not yet evident in Nrf2 +/+ mice. This is reminiscent of other disease models such as cigarette smoke-induced emphysema, in which the onset of lung pathology occurred earlier in Nrf2 −/− than in Nrf2 +/+ mice [41, 42], presumably because of the increased susceptibility of the Nrf2 −/− mice. We should note that, in contrast to BRB dysfunction in early diabetes that has been reported in mice in other studies, often using Evans Blue as a tracer [35], we usually do not observe dysfunction until later in diabetes, at 3–6 months (data not shown).
We also examined the effect of NRF2 ablation on neuronal dysfunction. The pathogenesis of neuronal dysfunction in DR is not well understood. However, pro-inflammatory changes are a contributory cause of retinal neuronal apoptosis in DR [38], and treatment with an anti-inflammatory drug corrected retinal electrophysiological abnormalities in a rodent model of DR [43]. This suggests to us that NRF2 might also modulate neuronal dysfunction in DR. An approach for testing optomotor responses, specifically the virtual optomotor system, has emerged for assessing visual function in mice. This approach can ascertain two measures of spatial vision, acuity and CS [27]. We found that 8 weeks of diabetes resulted in a significant reduction of the SF threshold (Fig. 8a) in wild-type mice, similar to the findings of a study using diabetic rats [44]. There was a similar tendency toward a diabetes-induced reduction in CS in wild-type mice, although this did not reach statistical significance (Fig. 8b). Strikingly, we found that Nrf2 −/− mice had a statistically significant reduction in both variables of visual function compared with wild-type mice. This indicates that NRF2 has an important protective role against neuronal dysfunction in the context of diabetes.
NRF2 has previously been demonstrated to have a protective role in DR [18]. Nrf2 −/− mice had significantly greater renal injury compared with Nrf2 +/+ mice in the STZ-induced diabetes model [18]. Therapeutic activation of NRF2 reduced diabetic kidney disease in rodents. This suggests that NRF2 might be involved in a common protective mechanism for diabetic complications, making it an especially attractive pharmacological target, especially as NRF2 is readily amenable to pharmacological activation. Of note, a recent study in rats demonstrated that high glucose levels and diabetes impair NRF2 activity, with a resultant blunting of induction of the NRF2-responsive antioxidant gene Gclc [45]. This very interesting study suggests that individuals with DR might have suboptimal NRF2 activity, further highlighting the importance of pharmacological modulation of NRF2.
In summary, there is emerging appreciation of the importance of identifying endogenous protective factors in DR. Indeed, some protective molecules have already been identified, including manganese superoxide dismutase (MnSOD) [46] and pigment epithelium-derived factor (PEDF) [47]. Augmentation of these respective protective molecules inhibits DR and its pathological consequences [31, 47]. Our studies indicate that NRF2 is involved in an additional protective mechanism in the retina in diabetes. Pharmacological targeting of NRF2 may therefore be a promising strategy for protecting vascular and neuronal function in DR.
Abbreviations
- BRB:
-
Blood–retina barrier
- CS:
-
Contrast sensitivity
- DCF:
-
Dichlorofluorescein
- DR:
-
Diabetic retinopathy
- DTNB:
-
5,5′-Dithio-bis-2-(nitrobenzoic acid)
- GCL:
-
Ganglion cell layer
- GFAP:
-
Glial fibrillary acidic protein
- GSH:
-
Glutathione
- H2O2 :
-
Hydrogen peroxide
- INL:
-
Inner nuclear layer
- KEAP1:
-
Kelch-like ECH-associated protein 1
- NRF2:
-
Nuclear factor erythroid-2-related factor 2
- ONL:
-
Outer nuclear layer
- qPCR:
-
Quantitative PCR
- ROS:
-
Reactive oxygen species
- siRNA:
-
Small interference RNA
- SF:
-
Spatial frequency
- STZ:
-
Streptozotocin
- TBH:
-
tert-Butyl hydroperoxide
- TNB:
-
5-Thio-2-nitrobenzoic acid
- VEGF:
-
Vascular endothelial growth factor
References
Klein BE (2007) Overview of epidemiologic studies of diabetic retinopathy. Ophthalmic Epidemiol 14:179–183
Yau JW, Rogers SL, Kawasaki R et al (2012) Global prevalence and major risk factors of diabetic retinopathy. Diabetes Care 35:556–564
Kowluru RA, Chan PS (2007) Oxidative stress and diabetic retinopathy. Exp Diabetes Res 2007:43603
Tang J, Kern TS (2011) Inflammation in diabetic retinopathy. Prog Retin Eye Res 30:343–358
Zhang W, Liu H, Rojas M, Caldwell RW, Caldwell RB (2011) Anti-inflammatory therapy for diabetic retinopathy. Immunotherapy 3:609–628
Zong H, Ward M, Stitt AW (2011) AGEs, RAGE, and diabetic retinopathy. Curr Diab Rep 11:244–252
Santos JM, Mohammad G, Zhong Q, Kowluru RA (2011) Diabetic retinopathy, superoxide damage and antioxidants. Curr Pharm Biotechnol 12:352–361
Antonetti DA, Klein R, Gardner TW (2012) Diabetic retinopathy. N Engl J Med 366:1227–1239
Rask-Madsen C, King GL (2010) Kidney complications: factors that protect the diabetic vasculature. Nat Med 16:40–41
Jeong IK, King GL (2011) New perspectives on diabetic vascular complications: the loss of endogenous protective factors induced by hyperglycemia. Diabetes Metab J 35:8–11
Kensler TW, Wakabayashi N, Biswal S (2007) Cell survival responses to environmental stresses via the Keap1-Nrf2-ARE pathway. Annu Rev Pharmacol Toxicol 47:89–116
Kaspar JW, Niture SK, Jaiswal AK (2009) Nrf2:INrf2 (Keap1) signaling in oxidative stress. Free Radic Biol Med 47:1304–1309
Chen XL, Kunsch C (2004) Induction of cytoprotective genes through Nrf2/antioxidant response element pathway: a new therapeutic approach for the treatment of inflammatory diseases. Curr Pharm Des 10:879–891
Li N, Nel AE (2006) Role of the Nrf2-mediated signaling pathway as a negative regulator of inflammation: implications for the impact of particulate pollutants on asthma. Antioxid Redox Signal 8:88–98
Kim J, Cha YN, Surh YJ (2010) A protective role of nuclear factor-erythroid 2-related factor-2 (Nrf2) in inflammatory disorders. Mutat Res 690:12–23
Nagai N, Thimmulappa RK, Cano M et al (2009) Nrf2 is a critical modulator of the innate immune response in a model of uveitis. Free Radic Biol Med 47:300–306
Wei Y, Gong J, Yoshida T et al (2011) Nrf2 has a protective role against neuronal and capillary degeneration in retinal ischemia-reperfusion injury. Free Radic Biol Med 51:216–224
Jiang T, Huang Z, Lin Y, Zhang Z, Fang D, Zhang DD (2010) The protective role of Nrf2 in streptozotocin-induced diabetic nephropathy. Diabetes 59:850–860
Zheng H, Whitman SA, Wu W et al (2011) Therapeutic potential of Nrf2 activators in streptozotocin-induced diabetic nephropathy. Diabetes 60:3055–3066
Limb GA, Salt TE, Munro PM, Moss SE, Khaw PT (2002) In vitro characterization of a spontaneously immortalized human Muller cell line (MIO-M1). Invest Ophthalmol Vis Sci 43:864–869
Sussan TE, Rangasamy T, Blake DJ et al (2009) Targeting Nrf2 with the triterpenoid CDDO-imidazolide attenuates cigarette smoke-induced emphysema and cardiac dysfunction in mice. Proc Natl Acad Sci U S A 106:250–255
Harvey CJ, Thimmulappa RK, Sethi S et al (2011) Targeting Nrf2 signaling improves bacterial clearance by alveolar macrophages in patients with COPD and in a mouse model. Sci Transl Med 3:78ra32
Gubitosi-Klug RA, Talahalli R, Du Y, Nadler JL, Kern TS (2008) 5-Lipoxygenase, but not 12/15-lipoxygenase, contributes to degeneration of retinal capillaries in a mouse model of diabetic retinopathy. Diabetes 57:1387–1393
Du Y, Miller CM, Kern TS (2003) Hyperglycemia increases mitochondrial superoxide in retina and retinal cells. Free Radic Biol Med 35:1491–1499
Derevjanik NL, Vinores SA, Xiao WH et al (2002) Quantitative assessment of the integrity of the blood-retinal barrier in mice. Invest Ophthalmol Vis Sci 43:2462–2467
Huang H, Gandhi JK, Zhong X et al (2011) TNFalpha is required for late BRB breakdown in diabetic retinopathy, and its inhibition prevents leukostasis and protects vessels and neurons from apoptosis. Invest Ophthalmol Vis Sci 52:1336–1344
Prusky GT, Alam NM, Beekman S, Douglas RM (2004) Rapid quantification of adult and developing mouse spatial vision using a virtual optomotor system. Invest Ophthalmol Vis Sci 45:4611–4616
Zheng L, Du Y, Miller C et al (2007) Critical role of inducible nitric oxide synthase in degeneration of retinal capillaries in mice with streptozotocin-induced diabetes. Diabetologia 50:1987–1996
Wang J, Xu X, Elliott MH, Zhu M, Le YZ (2010) Muller cell-derived VEGF is essential for diabetes-induced retinal inflammation and vascular leakage. Diabetes 59:2297–2305
Zong H, Ward M, Madden A et al (2010) Hyperglycaemia-induced pro-inflammatory responses by retinal Muller glia are regulated by the receptor for advanced glycation end-products (RAGE). Diabetologia 53:2656–2666
Kowluru RA, Kowluru V, Xiong Y, Ho YS (2006) Overexpression of mitochondrial superoxide dismutase in mice protects the retina from diabetes-induced oxidative stress. Free Radic Biol Med 41:1191–1196
Joussen AM, Poulaki V, Mitsiades N et al (2002) Nonsteroidal anti-inflammatory drugs prevent early diabetic retinopathy via TNF-alpha suppression. Faseb J 16:438–440
Gardner TW, Abcouwer SF, Barber AJ, Jackson GR (2010) An integrated approach to diabetic retinopathy research. Arch Ophthalmol 129:230–235
Shirao Y, Kawasaki K (1998) Electrical responses from diabetic retina. Prog Retin Eye Res 17:59–76
Kern TS, Tang J, Berkowitz BA (2010) Validation of structural and functional lesions of diabetic retinopathy in mice. Mol Vis 16:2121–2131
Sun JK, Keenan HA, Cavallerano JD et al (2011) Protection from retinopathy and other complications in patients with type 1 diabetes of extreme duration: the Joslin 50-year medalist study. Diabetes Care 34:968–974
Zheng L, Kern TS (2009) Role of nitric oxide, superoxide, peroxynitrite and PARP in diabetic retinopathy. Front Biosci 14:3974–3987
Krady JK, Basu A, Allen CM et al (2005) Minocycline reduces proinflammatory cytokine expression, microglial activation, and caspase-3 activation in a rodent model of diabetic retinopathy. Diabetes 54:1559–1565
Frey T, Antonetti DA (2011) Alterations to the blood-retinal barrier in diabetes: cytokines and reactive oxygen species. Antioxid Redox Signal 15:1271–1284
Al-Shabrawey M, Rojas M, Sanders T et al (2008) Role of NADPH oxidase in retinal vascular inflammation. Invest Ophthalmol Vis Sci 49:3239–3244
Iizuka T, Ishii Y, Itoh K et al (2005) Nrf2-deficient mice are highly susceptible to cigarette smoke-induced emphysema. Genes Cells 10:1113–1125
Rangasamy T, Cho CY, Thimmulappa RK et al (2004) Genetic ablation of Nrf2 enhances susceptibility to cigarette smoke-induced emphysema in mice. J Clin Invest 114:1248–1259
Kern TS, Miller CM, Du Y et al (2007) Topical administration of nepafenac inhibits diabetes-induced retinal microvascular disease and underlying abnormalities of retinal metabolism and physiology. Diabetes 56:373–379
Kirwin SJ, Kanaly ST, Hansen CR, Cairns BJ, Ren M, Edelman JL (2011) Retinal gene expression and visually evoked behavior in diabetic long evans rats. Invest Ophthalmol Vis Sci 52:7654–7663
Zhong Q, Mishra M, Kowluru RA (2013) Transcription factor Nrf2-mediated antioxidant defense system in the development of diabetic retinopathy. Invest Ophthalmol Vis Sci 54:3941–3948
Kowluru RA, Atasi L, Ho YS (2006) Role of mitochondrial superoxide dismutase in the development of diabetic retinopathy. Invest Ophthalmol Vis Sci 47:1594–1599
Zhang SX, Wang JJ, Gao G, Shao C, Mott R, Ma JX (2006) Pigment epithelium-derived factor (PEDF) is an endogenous antiinflammatory factor. Faseb J 20:323–325
Acknowledgements
The authors thank A. Limb (Institute of Ophthalmology, UCL, London, UK) for providing human Müller cell line MIO-M1, R. Kowluru (Kresge Eye Institute, Wayne State University School of Medicine, Detroit, MI, USA) for suggestions regarding the GSH assay, M. Hartsock (Department of Ophthalmology, Johns Hopkins School of Medicine, Baltimore, MD, USA) for technical assistance with cell culture studies, K. B. Ebrahimi (Department of Ophthalmology, Johns Hopkins School of Medicine) for suggestions regarding NRF2 immunohistochemistry and J. Wang (Department of Biostatistics, Johns Hopkins School of Medicine) for giving advice on statistical analysis.
Funding
These studies were supported by research grants from the National Institutes of Health EY022383 (EJD), EY022683 (EJD) and EY019904 (JTH), the William & Ella Owens Medical Research Foundation and a generous gift from Cindy and Jeong H. Kim, PhD. EJD is a recipient of an RPB Career Development Award.
Duality of interest
The authors declare that there is no duality of interest associated with this manuscript.
Contribution statement
ZX designed and performed the experiments, interpreted and analysed the data and wrote and edited the manuscript. YW, JG, HC, JKP, ES, HH, LW, CE, YD, TSK and AJB contributed to acquisition and analysis of the data and were involved in drafting the article. JTH, RT and SB contributed to analysis of the data and intellectual input, including ideas for development of the project and drafting the article. EJD conceived the study, designed the experimental plan, wrote the manuscript, supervised the entire work and edited the manuscript. All authors approved the final submitted version of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM Fig. 1
Nrf2 immunostaining in human retinal vasculature. Arrows indicate retinal vasculature. Paraffin-embedded human retinal sections were immunostained with Nrf2 antibody (blue), and counter-stained with nuclear fast red. Images were taken at 40× objective. (PDF 653 kb)
ESM Fig. 2
Analysis of apoptosis in non-diabetic and diabetic retinas from Nrf2 +/+ and Nrf2 -/- mice. Top panel, immunostaining for cleaved caspase 3 (green). Middle panel, TUNEL staining (green) of retinal section after 8 weeks of diabetes. Bottom panel, negative control and positive control for TUNEL staining. Nuclei was stained with DAPI (blue). The images were taken at 20× objective. (PDF 1731 kb)
ESM Fig. 3
Hematoxylin and eosin staining of non-diabetic and diabetic retinas from Nrf2 +/+ and Nrf2 -/- mice. The images were taken at 20× objective. (PDF 933 kb)
Rights and permissions
About this article
Cite this article
Xu, Z., Wei, Y., Gong, J. et al. NRF2 plays a protective role in diabetic retinopathy in mice. Diabetologia 57, 204–213 (2014). https://doi.org/10.1007/s00125-013-3093-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-013-3093-8