Abstract
Purpose
To evaluate the prevalence and features of lung apical findings on neck and cervical spine CTs performed in patients with COVID-19.
Methods
This was a retrospective, IRB-approved study performed at a large academic hospital in the USA. Between March 3, 2020, and May 6, 2020, 641 patients with COVID-19 infection diagnosed by RT-PCR received medical care at our institution. A small cohort of patients with COVID-19 infection underwent neck or cervical spine CT imaging for indications including stroke, trauma, and neck pain. The lung apices included in the field of view on these CT scans were reviewed for the presence of findings suspicious for COVID-19 pneumonia, including ground-glass opacities, consolidation, or crazy-paving pattern. The type and frequency of these findings were recorded and correlated with clinical information including age, gender, and symptoms.
Results
Thirty-four patients had neck or spine CTs performed before or concurrently with a chest CT. Of this group, 17 (50%) had unknown COVID-19 status at the time of neck or spine imaging and 10 (59%) of their CT studies had findings in the lung apices consistent with COVID-19 pneumonia.
Conclusion
Lung apical findings on cervical spine or neck CTs consistent with COVID-19 infection are common and may be encountered on neuroimaging performed for non-respiratory indications. For these patients, the emergency radiologist may be the first physician to suspect underlying COVID-19 infection.
Similar content being viewed by others
Introduction
Our understanding of Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-Cov-2) infection is rapidly evolving. The clinical presentation of patients infected with Coronavirus Disease 2019 (COVID-19) typically manifests as an acute respiratory illness with symptoms including fever, cough, and dyspnea [1]. Most of the radiology studies on COVID-19 infection to date have focused on the lung findings in this population, which typically include multifocal, peripheral ground-glass opacities, consolidations, and crazy-paving [2,3,4,5,6,7,8,9,10,11,12].
However, there is growing evidence that the SARS-Cov-2 virus may also involve other organ systems such as the gastrointestinal and central nervous systems (CNS) [13,14,15,16,17,18,19,20]. A recent study described COVID-19 infection findings in the lung bases on CT abdomen studies performed on patients presenting with nausea, vomiting, and abdominal pain [14]. CNS manifestations include non-respiratory symptoms such as altered mental status, seizures, and stroke-like symptoms possibly mediated by hypoxic-ischemic encephalopathy, demyelination, encephalitis, or cerebral thromboembolic disease [15,16,17,18,19,20]. In this population, imaging of the neck or cervical spine may be performed for a myriad of indications, including neck pain, trauma, or neck vascular imaging in the work-up of acute ischemic stroke. A systematic approach to interpreting these studies should include an evaluation of the upper lungs and mediastinum included within the field of view [21].
The purpose of this study was to evaluate the prevalence and characteristics of COVID-19 lung findings detected in patients undergoing CT of the neck or cervical spine.
Methods and materials
Study cohort
This was a retrospective, IRB-approved study performed at a single, large academic hospital in Boston, Massachusetts. Between March 3, 2020, and May 6, 2020, a total of 641 patients received medical care at our hospital for SARS-CoV-2. Included in this study were patients in our emergency department who underwent CT imaging of the neck and cervical spine, which includes the lung apices, and who also tested positive for SARS-CoV-2 via reverse transcriptase polymerase chain reaction (RT-PCR). Exclusion criteria included patients with CT examinations with severe motion artifact precluding a diagnostic assessment, neck CT examinations which included less than 8 consecutive axial images through the lung apices, and patients with suspected SARS-CoV-2 infection but tested negative on RT-PCR.
Clinical data
Basic demographic information for each patient was recorded including age and gender. Date of RT-PCR test positivity and presenting clinical symptoms were also recorded for each patient and included fever, cough, and gastrointestinal symptoms such as nausea/vomiting/diarrhea and loss of appetite.
Imaging technique
CT examinations were obtained on 64-slice MDCT scanners and protocols included in this study were CT angiograms of the neck, contrast-enhanced CT of the neck, and non-contrast CT of the cervical spine. CT examinations were performed on either a Revolution CT (GE Healthcare, Milwaukee, Wisconsin) or a Force CT (Siemens, Erlangen, Germany).
Non-contrast cervical spine CTs were helically acquired (120-kV/auto-mAs) with 1.25-mm thick slices from the level of the skull base to the thoracic inlet. Soft tissue and bone algorithms were available for review with 1.5–2 mm thick/interval coronal and sagittal reconstructions.
CT angiogram images of the neck were obtained from the level of the aortic arch through the superior orbital rim with 0.625–1.25 mm thick slices (120-kVp/auto-mAs), following a dose of 80–100 mL of iohexol (Omnipaque, GE Healthcare, Milwaukee, Wisconsin) or iopamidol (Isovue, Bracco, Princeton, New Jersey), 370 mg/mL administered by a power injector at a rate of 4–5 mL/s. Coronal and sagittal reformatted images at 2-mm thick slices were reconstructed.
Contrast-enhanced CT neck images were helically acquired (120-kV/auto-mAs) with 1.25-mm thick slices following a 60-s delay following intravenous contrast administration (80–160 mL of iohexol or iopamidol, 370mgI/mL) from the level of the skull base through the aortic arch. Soft tissue and bone algorithms were available for review with 2-mm thick/interval coronal and sagittal reconstructions.
Image evaluation
The type of CT examination each patient underwent (CT angiogram of the neck, contrast-enhanced CT of the neck, and cervical spine CT) was recorded. The date and time the neck imaging was performed were also recorded. Many of the patients in this cohort also underwent chest CT imaging. If a chest CT was performed at our institution during the course of the patient’s admission, the date and time of the chest CT were recorded.
The visualized portions of the lung apices were evaluated by a neuroradiology attending and a diagnostic radiology resident. Lung apices were evaluated for the presence of ground glass opacities, focal alveolar consolidation, and evidence of crazy paving (interlobular septal thickening on a background of ground-glass opacity).
Data analysis
The frequency of detection of lung apical findings related to suspected COVID-19 pneumonia and type of lung findings were calculated in our cohort. The temporal relationship between reported lung apical findings on neck CT examinations and RT-PCR positive testing results was also evaluated. The cohort was further stratified into patients where neck CT imaging was performed prior to chest CT imaging and when neck CT imaging was performed concurrently with chest CT imaging.
Results
A total of 37 patients met the inclusion criteria for this study, which included 15 females and 22 males (Fig. 1). Three patients were not analyzed since their CT neck or spine imaging occurred after a CT chest study. The mean age was 55 years (standard deviation 17 years, range: 30–96). The indications for cervical spine or neck imaging included the following: stroke, trauma, and neck pain (Table 1).
Thirty-four patients underwent neck or cervical spine CT imaging either preceding or contemporaneously with a CT chest study. Twenty-four (71%) patients had CT studies demonstrating COVID-19 findings in the lung apices including ground glass opacities in 22 patients (67%), consolidation in 14 patients (42%), and “crazy-paving” pattern in 3 patients (9%). Of all 34 patients, 17 (50%) had unknown COVID-19 status at the time of neck or spine imaging, and 10 (59%) of their CT studies had findings in the lung apices consistent with COVID-19 pneumonia (Figs. 2 and 3). Twelve out of 17 (71%) patients with unknown COVID-19 status at the time of imaging had respiratory symptoms or fever.
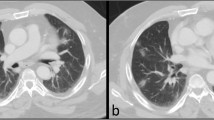
Axial image from a non-contrast cervical spine CT in an 84-year-old female presenting after an unwitnessed fall at home and unknown COVID-19 status. Images of the lung apices demonstrate peripheral, multifocal ground glass opacities (white arrows) with areas of consolidation (white arrowheads), a “typical appearance” of COVID-19 [2]. The patient subsequently tested COVID-19 positive
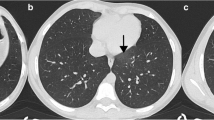
Axial image from non-contrast cervical spine CT in a 56-year-old male found down, unresponsive, and febrile with unknown COVID-19 status. Lung apices demonstrate peripheral, bilateral, ground glass opacities with visible interlobular lines (crazy-paving pattern (white arrow)), a “typical appearance” of COVID-19 [2]. The patient subsequently tested COVID-19 positive
There were 4 (12%) patients who had an unknown COVID-19 status at the time of CT cervical spine or neck imaging and had no preceding or contemporaneous CT chest imaging. Of these patients, 2 had findings in the lung apices consistent with COVID-19 pneumonia.
Discussion
In this study, 59% of patients with undiagnosed SARS-CoV-2 infection demonstrated apical lung findings suggestive of COVID-19 pneumonia on neck or cervical spine CT imaging. The most common manifestation of these findings was the presence of apical ground glass opacities followed by consolidation. Twelve percent of the patients in this cohort with undiagnosed SARS-CoV-2 infection had neck and/or cervical spine CT imaging preceding chest imaging. Furthermore, half of this subset of patients exhibited findings in the lung apex consistent with COVID-19 pneumonia and suspicion for infection was first raised in the emergency radiology report.
These results highlight the importance for emergency radiologists to be familiar with the patterns of COVID-19 lung disease, as they may be the first to encounter evidence of underlying SARS-CoV-2 infection and should be prepared to expeditiously alert the referring providers to these findings. These findings are consistent with prior literature as Kihira et al. reported that approximately 28% of patients undergoing a CT angiogram of the head and neck for stroke had apical lung findings concerning for COVID pneumonia [22]. Similarly, Hossain et al. found findings related to incidental COVID-19 pneumonia in a cohort of 18 patients who underwent neck imaging and 101 patients who underwent abdominal imaging [23]. A case report performed by Barajas et al. illustrated apical lung CT findings consistent with COVID-19 pneumonia on a patient undergoing a cervical spine CT for trauma evaluation [24]. Our study further emphasizes the importance of radiologist diligence when examining the visualized lung fields on multiple types of modality, including neck CT angiogram, CECT neck, and NECT cervical spine studies.
There are limitations to this study. The sample size is relatively small. While many patients underwent imaging evaluation at our institution related to symptoms of COVID-19 infection, imaging of the neck was relatively infrequent. Secondly, based on patient size and patient positioning, different amounts of the lung apices were visible on the neck and cervical spine CT examinations. We set a threshold of having at least 8 consecutive axial images present in the lung apices for inclusion into this study; however, several patients had substantially larger amounts of lung parenchyma visible on these CT examinations than others. In patients with relatively smaller amounts of visible lung tissue on CT, there may be potential findings of COVID-19 related pneumonia that were not included in the field of view.
The results of this study demonstrate that 59% of our patients with unknown COVID-19 status who underwent CT neck or cervical spine demonstrated imaging findings in the visualized portion of the lung apices consistent with COVID-19 pneumonia. This highlights the importance for emergency radiologists to be familiar with lung manifestations of COVID-19 pneumonia to ensure prompt diagnosis and treatment, even in instances where patients have no respiratory symptoms.
Abbreviations
- COVID-19:
-
Coronavirus disease 2019
- NECT:
-
Non-enhanced CT
- CECT:
-
Contrast-enhanced CT
References
Wang W, Tang J, Wei F (2020) Updated understanding of the outbreak of 2019 novel coronavirus (2019-nCoV) in Wuhan, China. J Med Virol 29:441–447. https://doi.org/10.1002/jmv.25689
Simpson S, Kay FU, Abbara S, Bhalla S, Chung JH, Chung M, Henry TS, Kanne JP, Kligerman S, Ko JP, Litt H (2020) Radiological society of North America expert consensus statement on reporting chest CT findings related to COVID-19. Endorsed by the Society of Thoracic Radiology, the American College of Radiology, and RSNA. Radiol Cardiothorac Imaging 2(2). https://doi.org/10.1148/ryct.2020200152
Bernheim A, Mei X, Huang M, Yang Y, Fayad ZA, Zhang N, Diao K, Lin B, Zhu X, Li K, Li S, Shan H, Jacobi A, Chung M (2020) Chest CT findings in coronavirus disease-19 (COVID-19): relationship to duration of infection. Radiology 295:200463. https://doi.org/10.1148/radiol.2020200463
Pan F, Ye T, Sun P, Gui S, Liang B, Li L, Zheng D, Wang J, Hesketh RL, Yang L, Zheng C (2020) Time course of lung changes on chest CT during recovery from 2019 novel coronavirus (COVID-19) pneumonia. Radiology 13:715–721. https://doi.org/10.1148/radiol.2020200370
Xie X, Zhong Z, Zhao W, Zheng C, Wang F, Liu J (2020 February) Chest CT for typical 2019-nCoV pneumonia: relationship to negative RT-PCR testing. Radiology 12:200343. https://doi.org/10.1148/radiol.2020200343
Fang Y, Zhang H, Xu Y, Xie J, Pang P, Ji W (2020) CT manifestations of two cases of 2019 novel coronavirus (2019-nCoV) pneumonia. Radiology 7:208–209. https://doi.org/10.1148/radiol.2020200280
Song F, Shi N, Shan F, Zhang Z, Shen J, Lu H, Ling Y, Jiang Y, Shi Y (2020) Emerging coronavirus 2019-nCoV pneumonia. Radiology 6:210–217. https://doi.org/10.1148/radiol.2020200274
Ng M, Lee E, Yang J et al (2020) Imaging profile of the COVID-19 infection: radiologic findings and literature review. Radiol Cardiothorac Imaging 13. https://doi.org/10.1148/ryct.2020200034
Wu Y, Xie Y, Wang X (2020) Longitudinal CT findings in COVID-19 pneumonia: case presenting organizing pneumonia pattern. Radiol Cardiothorac Imaging 13. https://doi.org/10.1148/ryct.2020200031
Liu T, Huang P, Liu H, Huang L, Lei M, Xu W, Hu X, Chen J, Liu B (2020) Spectrum of chest CT findings in a familial cluster of COVID-19 infection. Radiol Cardiothorac Imaging 2. https://doi.org/10.1148/ryct.2020200025
Li X, Zeng X, Liu B, Yu Y (2020) COVID-19 infection presenting with CT halo sign. Radiol Cardiothorac Imaging 2. https://doi.org/10.1148/ryct.2020200026
Chung M, Bernheim A, Mei X, Zhang N, Huang M, Zeng X, Cui J, Xu W, Yang Y, Fayad ZA, Jacobi A, Li K, Li S, Shan H (2020) CT imaging features of 2019 novel coronavirus (2019-nCoV). Radiology 4:202–207. https://doi.org/10.1148/radiol.2020200230
Pan L, Mu M, Yang P et al (2020) Clinical characteristics of COVID-19 patients with digestive symptoms in Hubei, China: a descriptive, cross-sectional, multicenter study. Am J Gastroenterol 115(5):766–773. https://doi.org/10.14309/ajg.0000000000000620
Siegel et al (2020) Lung base findings of coronavirus disease (COVID-19) on abdominal CT in patients with predominant gastrointestinal symptoms. AJR 215:1–3. https://doi.org/10.2214/AJR.20.23232
Mao L, Jin H, Wang M, Hu Y, Chen S, He Q, Chang J, Hong C, Zhou Y, Wang D, Miao X, Li Y, Hu B (2020) Neurologic manifestations of hospitalized patients with coronavirus disease 2019 in Wuhan, China. JAMA Neurol 77:683
De Felice FG, Tovar-Moll F, Moll J, Munoz DP, Ferreira ST (2020) Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and the central nervous system. Trends Neurosci
Poyiadji N, Shahin G, Noujaim D, Stone M, Patel S, Griffith B (2020) COVID-19-associated acute hemorrhagic necrotizing encephalopathy: CT and MRI features. Radiology 201187
Ye M, Ren Y, Lv T (2020) Encephalitis as a clinical manifestation of COVID-19. Brain Behav Immun
Moriguchi T, Harii N, Goto J, Harada D, Sugawara H, Takamino J, Ueno M, Sakata H, Kondo K, Myose N, Nakao A, Takeda M, Haro H, Inoue O, Suzuki-Inoue K, Kubokawa K, Ogihara S, Sasaki T, Kinouchi H, Kojin H, Ito M, Onishi H, Shimizu T, Sasaki Y, Enomoto N, Ishihara H, Furuya S, Yamamoto T, Shimada S (2020) A first case of meningitis/encephalitis associated with SARS-Coronavirus-2. Int J Infect Dis 94:55–58
Lang M, Buch K, Li MD, Mehan WA Jr, Lang AL, Leslie-Mazwi TM, Rincon SP (2020) Leukoencephalopathy associated with severe COVID-19 infection: sequela of hypoxemia? AJNR Am J Neuroradiol
Cunqueiro A, Gomes WA, Lee PR, Dym RJ, Scheinfeld MH (2019) CT of the Neck: Image Analysis and Reporting in the Emergency Setting. Radiographics 39(6):1760–1781. https://doi.org/10.1148/rg.2019190012
Kihira S, Schefflein J, Chung M et al (2020) Incidental COVID-19 related lung apical findings on stroke CTA during the COVID-19 pandemic. J Neurointerv Surg neurintsurg-2020-016188
Barajas RF Jr, Rufener G, Starkey J, Duncan T, Fuss C (2020) Asymptomatic COVID-19: what the neuroradiologist needs to know about pulmonary manifestations. AJNR Am J Neuroradiol 41:966–968. https://doi.org/10.3174/ajnr.A6561
Hossain R, Lazarus MS, Roudenko A, Dako F, Mehta V, Alis J, Zalta B, Lei B, Haramati LB, White CS (2020) CT Scans obtained for nonpulmonary indications: associated respiratory findings of COVID-19. Radiology 201743
Author information
Authors and Affiliations
Contributions
All authors whose names appear on the submission (1) made substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data; or the creation of new software used in the work; (2) drafted the work or revised it critically for important intellectual content; (3) approved the version to be published; and (4) agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Conflict of interest
Dr. William A. Mehan, Jr. performs consulting work for Kura Oncology as an independent reviewer of head and neck cancer imaging for a clinical trial. He also performs consulting work for health insurance companies by providing expert opinion on medicolegal cases involving neuroimaging. Neither of these activities is related to the submitted work. All other authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Applewhite, B.P., Buch, K., Yoon, B.C. et al. Lung apical findings in coronavirus disease (COVID-19) infection on neck and cervical spine CT. Emerg Radiol 27, 731–735 (2020). https://doi.org/10.1007/s10140-020-01822-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10140-020-01822-0