Abstract
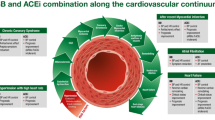
The renin-angiotensin system (RAS) plays a major role in the pathophysiology of cardiovascular disorders. Angiotensin II (Ang-II), the final product of this pathway, is known for its vasoconstrictive and proliferative effects. Angiotensin-converting enzyme 2 (ACE2), a newly discovered homolog of ACE, plays a key role as the central negative regulator of the RAS. It diverts the generation of vasoactive Ang-II into the vasodilatory and growth inhibiting peptide angiotensin(1–7) [Ang(1–7)], thereby providing counter-regulatory responses to neurohormonal activation. There is substantial experimental evidence evaluating the role of ACE2/Ang(1–7) in hypertension, heart failure, and atherosclerosis. In this review, we aim to focus on the conceptual facts of the ACE2-Ang(1–7) axis with regards to clinical implications and therapeutic targets in cardiovascular disorders, with emphasis on the potential therapeutic role in cardiovascular diseases.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
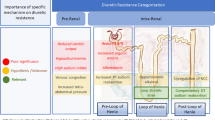
The renin-angiotensin system (RAS) is a pivotal mediator in the development of hypertension and associated cardiovascular diseases. It plays a key role in regulating blood pressure and maintaining fluid and salt balance. Angiotensin II (Ang-II), the main active substrate of RAS pathway, binds to type-1 receptors (AT1R), thereby promoting vasoconstriction, fibrosis, and salt retention. Like most homeostatic mechanisms, the presence of an endogenous counter-regulatory system likely exists to counteract the RAS system. Therefore, since the discovery of angiotensin-converting enzyme 2 (ACE2) in the last decade, mechanistic studies have demonstrated its critical role as a cardioprotective arm of the RAS pathway (Fig. 1) [1, 2•]. While the ACE/Ang-II/AT1R is a well-established axis of the RAS leading to vasoconstrictive and proliferative effects, the ACE2 linking to angiotensin(1–7) [Ang(1–7)] and its G-protein coupled protein receptor (Mas), provides a vasoprotective and anti-proliferative mechanism, resulting in counter regulation of RAS [1]. In this review, we attempt to emphasize the role of the ACE2/Ang-(1–7) pathway as a central regulator of the RAS, and as a potential target for therapy in patients across the spectrum of cardiovascular diseases particularly in the setting of heart failure (HF).
Biochemical Aspects of ACE2 and Ang(1–7) Production
In 2000, genomic-based strategies by two independent research groups characterized cDNA of a new homolog of ACE, called ACE2 [3, 4]. Further investigations suggest that ACE2 is widely expressed in the endothelium of heart, kidney, brain, and vasculature [2•]. In humans, circulating (or soluble) ACE2 level is 200-fold lower than that of circulating ACE. ADAM 17 (A disease Disintegrin And Metalloproteinase, also known as tumor necrosis factor-α-converting enzyme [TACE]) is a major protease that cleaves ACE2 from the cellular membrane to allow its shedding as a fully active soluble glycoprotein [5].
ACE2 is a critical enzyme in controlling any excessive vasoactive and growth promoting effects of the RAS. Interestingly, ACE and ACE2 have similar biochemical protein sequences but different substrate specificities. They both exist as endothelium-bound carboxypeptidases, with approximately 40 % amino acid sequence homology [6]. However, ACE and ACE2 are functionally different enzymes that play opposite actions [7••]. ACE2 catalyzes the conversion of Ang I to angiotensin-(1–9) which, in turn, can be converted to Ang(1–7) by ACE. ACE2 also directly hydrolyzes Ang-II to Ang(1–7) with high catalytic affinity [8]. Ang(1–7) is a biologically active metabolite that counterbalances the cardiovascular effects of Ang-II. Through the Mas receptor, Ang(1–7) exerts vasodilatory and anti-proliferative effects, therefore, counterbalancing Ang-II [9]. In contrast to ACE, ACE2 activity seems to be unaffected by classical ACE inhibitors given distinct substrate-binding pockets [3]. Interestingly, increased cardiovascular expression of ACE2 and plasma Ang(1–7) levels have been demonstrated with treatment of angiotensin receptor blockers (ARB) as well as mineralocorticoid receptor antagonists (MRA) in animals and humans [10–12]. Several other roles of ACE2 have been described in the literature including the modulation of the integrin signaling pathway [13, 14] and interaction with the apelin-APJ pathway [15].
In the absence of ACE2, increased plasma and myocardial Ang-II levels have been attributed to reduced metabolism of plasma Ang-II [16, 17•]. It is therefore conceivable that ACE2 also directly antagonizes the vasoconstrictive and pro-oxidative effects of Ang-II by enhancing its degradation (Fig. 1). Meanwhile, the effects of drug therapy on Ang(1–7) may be different. Production of Ang-II is decreased with increased levels in Ang-I with ACE inhibitors. Hence, Ang(1–7) is increased primarily due to decreased degradation of Ang-I. In contrast, increased circulating levels of Ang-II by ARB drives the catabolism to the unopposed AT2 receptors, and, hence, to increased levels of Ang(1–7).
Cardioprotective Role of ACE2 Against Angiontensin II in Animal Studies
Several observations and experimental evidence from animal models have suggested a beneficial role of the ACE2-Ang(1–7) axis on cardiovascular function. Elevated ACE2 expression appears to occur at the initial stage of several pathologic conditions and declines with disease progression [18]. Loss of ACE2 enhances the susceptibility to myocardial dysfunction, while enhancing ACE2 action prevents adverse pathological remodeling and slows the progression to HF [18, 19]. Mechanistically, loss of ACE2 may also trigger activation of the myocardial NADPH oxidase system, increased production of superoxide, and activation of matrix metalloproteinases, leading to further adverse myocardial remodeling and dysfunction [20].
Animal studies have directly demonstrated a potentially critical role of ACE-2 in counterbalancing the maladaptive pathophysiological effects of Ang-II [21, 22]. In the heart, ACE2 appears to be the primary pathway for the metabolism of Ang-II [23]. At the same time, excess Ang-II may promote its conversion to Ang(1–7) in the presence of ACE2 [24]. Hence, a deficiency of ACE2 can lead to increased tissue and circulating levels of Ang-II and reduced levels of Ang(1–7) as demonstrated in animal models, which result in early cardiac hypertrophy and fibrosis that is reversible with double knockout mice of ACE and ACE2 genes or following treatment with ACE inhibitors or angiotensin receptor blockers (ARB) [18, 19].
Overexpression of ACE2 prevents adverse cardiac remodeling [21], and treatment with Ang(1–7) prevents cardiac fibrosis in animal models [25]. Consistent with a key role of ACE2 in post-MI remodeling, overexpression of ACE2 ameliorates LV remodeling and dysfunction in a rat model of myocardial infarction [26]. On the other hand, loss of ACE2 worsens the pathological remodeling and results in a rapid progression to reduced systolic function and HF in a pressure-overload mouse model [22]. These observations suggest that ACE2 could be an important regulator of LV remodeling.
Role of ACE2 in Cardiac Remodeling and Systolic Dysfunction in Humans
Cardiac remodeling of the heart plays a key role in the progressive deterioration of cardiac function that leads to human HF. In patients with HF, elevated levels of Ang-II and myocardial ACE mRNA level activity have been reported [27]. On the other hand, the role of ACE2 expression in the development of left ventricular remodeling in human HF remained poorly understood [28]. The first evidence of ACE2-mediated formation of Ang(1–7) in human HF came from ACE2 protein and substrate activity analyses of explanted human heart tissues [29]. They found that Ang(1–7)-forming activity from both angiotensin I and Ang-II was increased in failing human heart ventricles but was mediated by at least two different angiotensinases. The first, which demonstrated substrate preference for angiotensin I, was neutral endopeptidase-like, whereas ACE2 appears to favor Ang-II [29]. ACE2 expression is increased regardless of etiology [30].
Meanwhile, the relationship between the expression of ACE2 mRNA and the severity of LV remodeling was investigated in 14 patients with end-stage HF. Interestingly, there was a strong relationship between the amount of ACE2 gene expression and the severity of LV remodeling determined by LV dimensions [31], suggesting that ACE2 expression could be activated as an adaptive compensatory mechanism to militate against LV remodeling. However, ACE2 expression did not correlate with either LV ejection fraction nor plasma BNP levels, implying that such compensatory increased expression of ACE2 may be insufficient to counter pathologic processes as disease progressed [31].
The clinical relevance of ACE2 in the setting of systolic dysfunction was further demonstrated by the detection of soluble ACE2 (sACE2) activity in patients with systolic HF [32•]. Increasing sACE2 plasma activity strongly correlated with a clinical diagnosis of HF regardless of etiology and tracked with worsening functional class and higher natriuretic peptide levels, while independent of other disease states and medication use [32•]. In a separate cohort of 113 patients with chronic systolic HF with detailed echocardiographic analysis, higher sACE2 activity was associated with a lower left ventricular ejection fraction, more right ventricular systolic dysfunction, and larger left ventricular end-diastolic diameter [33]. Furthermore, sACE2 was an independent predictor of adverse clinical events (death, cardiac transplant, and HF hospitalizations), independently of left ventricular ejection fraction and natriuretic peptide levels [33]. These findings have now been substantiated in several independent confirmatory studies [34, 35].
The impact of drug therapy on directly modulating ACE2 activity and expression has not been well described. In the setting of acute decompensated HF in patients with advanced HF, circulating sACE2 activity was found to increase following intensive medical therapy aiming to optimize hemodynamic derangements and relief congestion [35]. Interestingly, patients who experienced >50 % increase in their sACE2 activity were associated with better long-term outcomes, further supporting the potential counter-regulatory role of ACE2. Conventional drugs such as ARBs and MRAs have been reported to increase ACE2-related beneficial effects, thus, providing an additional rationale for their use in the setting of HF. From this perspective, ARBs would appear to have an advantage since they tend to increase Ang-II levels, an effect that along with its promotion of ACE2 activity, would raise the levels of the protective peptide Ang(1–7). However, superiority of the ARBs over ACE inhibitors in either myocardial infarction survivors or HF patients has yet to be demonstrated in large clinical trials, suggesting that the perceived incremental benefit may not be as clinically relevant. Meanwhile, MRA decreased ACE and increased ACE2, each and both are capable of reducing Ang-II level [10]. Studies demonstrating incremental benefit of MRAs in patients with systolic HF have supported its broad adoption, yet to our knowledge, no studies on long term effects of MRA on ACE2 or Ang(1–7) metabolism and effects in humans have been conducted.
Role of ACE2 in Diastolic Dysfunction and Hypertension
Epidemiological studies have consistently demonstrated that HF with preserved ejection fraction (HFpEF) accounts for over 30 % of all HF, particularly in elderly patients. The development of myocardial fibrosis and pathological hypertrophy has been the central hypothesis that contributes to the development of diastolic dysfunction and HFpEF due to increased myocardial stiffness. Indeed, elevated sACE2 levels have been observed in patients with HFpEF as well [32•]. As previously discussed, ACE2 negatively regulates the pathophysiological effects of a pressor and suppressor dose of Ang-II on myocardial structure and function [16]. ACE2 is also a negative regulator of Ang-II-induced myocardial hypertrophy, fibrosis, and diastolic dysfunction [1]. With the paucity of effective drug therapies, strategies to enhance ACE2 effects in patients with HFpEF are promising, although studies showing reversal and recovery of myocardial stiffness after its development are lacking.
Several studies have demonstrated the modulatory effect of ACE2 on blood pressure. ACE2 is present in vascular endothelial walls, and plays a major role in producing Ang(1–7). Based on in vitro biochemical data and in vivo findings, a reduction in ACE2 levels could lead to elevated Ang-II levels, thus promoting increased blood pressure. [16, 36] Overexpression of ACE2 in the vasculature reduces blood pressure and improves endothelial function in hypertensive rats [37]. Moreover, interventions to augment the expression or activity of ACE2 have been shown to significantly reduce blood pressure levels [18]. However, data associating ACE2 polymorphism to hypertension is controversial, with some studies conceding a possible association with left ventricular mass, septal wall thickness and hypertrophy while others refute that association [38–40]. Meanwhile, the vasodilatory effects of Ang(1–7) are attributed to stimulating the production of nitric oxide, prostaglandins, and endothelium derived relaxation factors [23]. In humans, Ang(1–7) elicited a direct vasodilation in forearm circulation of both normotensive and hypertensive patients [9]. Interestingly, Ang(1–7) levels are elevated with treatment of ACE inhibitors and ARB, which might suggest the contribution of this peptide in their antihypertensive effects [41]. Localized ACE2/Ang(1–7) axis in the brain may also modulate centrally-mediated hypertension.
Utilization of ACE2 Activators in Cardiovascular Diseases: Future Prospects
Given that ACE and ACE2 have distinct effects on the metabolism of RAS effector peptides that regulate cardiovascular structure and function, drugs which can modify the homeostatic balance of expressions and activities of these enzymes can be viewed as potential therapeutic tools to treat a variety of cardiovascular diseases [6]. Being a central regulator of LV remodeling, drugs targeting ACE2 represent potential candidates to prevent and treat HF [7••]. It is conceivable that ACE2 could also constitute a valuable novel target to complement existing therapeutic strategies for managing LV dysfunction. Conditions where ACE inhibition and ARB are partially effective, the adjunctive actions of ACE2 may not only reduce clinical escape but also augment the efficacy of interventions.
Studies with recombinant human ACE2 (rhACE2) have shown beneficial cardiac effects [18, 36]. rhACE2 has anti-fibrotic properties and can attenuate effect on systolic and diastolic dysfunction, presumably via Ang-II inhibition [16]. In one study, rhACE2 use in Ang-II infused wild-mice suppressed the hypertrophic and fibrotic response induced by Ang-II, with reduced plasma and myocardial Ang-II and increased plasma Ang(1–7) levels [12]. Similarly, rhACE2 suppresses the direct effect of Ang-II on cardiomyocytes and fibroblasts in a pressure-overloaded model of HF [16]. On the other hand, a conformational-based rational drug strategy has been used to identify small molecules that specifically enhance ACE2 activities. One of these ACE2 activators, xanthenone, has been demonstrated to decrease blood pressure and improve cardiac function with inhibition of cardiac and renal fibrosis in spontaneously hypertensive rats [42•]. Direct supplementation of Ang(1–7) has also been explored as a therapeutic approach. In a rat model for HF, chronic infusion of Ang(1–7) was associated with more preserved contractile function. The first Ang(1–7) analogue, AVE0991, can promote vasorelaxation, lower blood pressure, and attenuate remodeling in a post-infarction animal model [43]. Similarly, Ang(1–7) peptide was shown to rescue systolic dysfunction in ACE2-null mice in a pressure-overloaded induced HF model [44].
However, the effects of these newly-developed reagents directly targeting ACE2 or Mas receptor must be compared with the drugs currently used to treat HF patients (i.e., ARBs and MRAs) to determine if targeting the ACE2/Ang(1–7) pathway alone or targeting multiple components of the RAS offers any advantages beyond those of existing therapies [45]. Furthermore, careful attention may, however, be necessary to optimize the potential therapeutic effects of ACE2, since an endogenous inhibitor and auto-antibodies against ACE2 have been detected in human plasma [46]. However, randomized clinical studies are needed to investigate the long term effects of RAS-blockers on Ang(1–7) metabolism.
Conclusion
The discovery of ACE2 and its role in counteracting the effect of Ang-II through Ang(1–7) formation represents a new avenue for our understanding of the role of the RAS on cardiac pathology. The emerging concept is that an imbalance in ACE2/Ang-(1–7) and ACE/Ang-II axes is critical in the development of cardiovascular diseases. The central role of ACE2, therefore, appears to counter ACE activity by reducing Ang-II bioavailability and increasing Ang(1–7) formation. Recent findings have revealed intriguing possibilities for the use of RAS-modulating agents and molecules as novel therapeutic agents in hypertension and cardiovascular therapeutic research. More human studies and head-to-head comparison trials are needed in determining their clinical efficacies in the setting of HF.
Abbreviations
- ACE:
-
angiotensin converting enzyme
- ACE2:
-
angiotensin converting enzyme2
- Ang:
-
Angiotensin
- Ang(1–7):
-
Angiotensin-(1–7)
- ARB:
-
AT1 receptor blocker
- AT1R:
-
angiotensin receptor type 1
- AT2:
-
angiotensin receptor type 2
- AVE 0991:
-
Angiotensin-(1–7) Mas receptor agonist
- CAD:
-
coronary artery disease
- HF:
-
heart failure
- LV:
-
left ventricle
- LVEF:
-
left ventricular ejection fraction
- NT-proBNP:
-
N-terminal pro brain natriuretic peptide
- NYHA:
-
New York Heart Association
- RAS:
-
Renin Angiotensin System
- rhACE2:
-
recombinant human angiotensin converting enzymes 2
- sACE2:
-
soluble angiotensin-converting enzyme 2
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Wang W, Bodiga S, Das SK, Lo J, Patel V, Oudit GY. Role of ACE2 in diastolic and systolic heart failure. Heart Fail Rev. 2012;17(4–5):683–91.
• Oudit GY, Crackower MA, Backx PH, Penninger JM. The role of ACE2 in cardiovascular physiology. Trends Cardiovasc Med. 2003;13(3):93–101. Comprehensive review on the current physiologic understanding of ACE2 in cardiovascular diseases.
Tipnis SR, Hooper NM, Hyde R, Karran E, Christie G, Turner AJ. A human homolog of angiotensin-converting enzyme. Cloning and functional expression as a captopril-insensitive carboxypeptidase. J Biol Chem. 2000;275(43):33238–43.
Donoghue M, Hsieh F, Baronas E, et al. A novel angiotensin-converting enzyme-related carboxypeptidase (ACE2) converts angiotensin I to angiotensin 1–9. Circ Res. 2000;87(5):E1–9.
Burrell LM, Harrap SB, Velkoska E, Patel SK. The ACE2 gene: its potential as a functional candidate for cardiovascular disease. Clin Sci (Lond). 2013;124(2):65–76.
Iwata M, Cowling RT, Yeo SJ, Greenberg B. Targeting the ACE2-Ang-(1–7) pathway in cardiac fibroblasts to treat cardiac remodeling and heart failure. J Mol Cell Cardiol. 2011;51(4):542–7.
•• Oudit GY, Penninger JM. Recombinant human angiotensin-converting enzyme 2 as a new renin-angiotensin system peptidase for heart failure therapy. Curr Heart Fail Rep. 2011;8(3):176–83. First demonstration of the feasibility and beneficial effects of recumbinant human ACE2 as potential therapy.
Vickers C, Hales P, Kaushik V, et al. Hydrolysis of biological peptides by human angiotensin-converting enzyme-related carboxypeptidase. J Biol Chem. 2002;277(17):14838–43.
Fraga-Silva RA, Costa-Fraga FP, Murca TM, et al. Angiotensin-converting enzyme 2 activation improves endothelial function. Hypertension. 2013;61(6):1233–8.
Keidar S, Gamliel-Lazarovich A, Kaplan M, et al. Mineralocorticoid receptor blocker increases angiotensin-converting enzyme 2 activity in congestive heart failure patients. Circ Res. 2005;97(9):946–53.
Silva AC S e, Silveira KD, Ferreira AJ, Teixeira MM. ACE2, angiotensin-(1–7) and Mas receptor axis in inflammation and fibrosis. Br J Pharmacol. 2013;169(3):477–92.
Zhong JC, Ye JY, Jin HY, et al. Telmisartan attenuates aortic hypertrophy in hypertensive rats by the modulation of ACE2 and profilin-1 expression. Regul Pept. 2011;166(1–3):90–7.
Clarke NE, Fisher MJ, Porter KE, Lambert DW, Turner AJ. Angiotensin converting enzyme (ACE) and ACE2 bind integrins and ACE2 regulates integrin signalling. PLoS One. 2012;7(4):e34747.
Lin Q, Keller RS, Weaver B, Zisman LS. Interaction of ACE2 and integrin beta1 in failing human heart. Biochim Biophys Acta. 2004;1689(3):175–8.
Sato T, Suzuki T, Watanabe H, et al. Apelin is a positive regulator of ACE2 in failing hearts. J Clin Invest 2013.
Zhong J, Basu R, Guo D, et al. Angiotensin-converting enzyme 2 suppresses pathological hypertrophy, myocardial fibrosis, and cardiac dysfunction. Circulation. 2010;122(7):717–28. 718 p following 728.
• Kassiri Z, Zhong J, Guo D, et al. Loss of angiotensin-converting enzyme 2 accelerates maladaptive left ventricular remodeling in response to myocardial infarction. Circ Heart Fail. 2009;2(5):446–55. Important demonstration of the cardioprotective role of ACE2.
Tikellis C, Bernardi S, Burns WC. Angiotensin-converting enzyme 2 is a key modulator of the renin-angiotensin system in cardiovascular and renal disease. Curr Opin Nephrol Hypertens. 2011;20(1):62–8.
Oudit GY, Kassiri Z, Patel MP, et al. Angiotensin II-mediated oxidative stress and inflammation mediate the age-dependent cardiomyopathy in ACE2 null mice. Cardiovasc Res. 2007;75(1):29–39.
Bodiga S, Zhong JC, Wang W, et al. Enhanced susceptibility to biomechanical stress in ACE2 null mice is prevented by loss of the p47(phox) NADPH oxidase subunit. Cardiovasc Res. 2011;91(1):151–61.
Huentelman MJ, Grobe JL, Vazquez J, et al. Protection from angiotensin II-induced cardiac hypertrophy and fibrosis by systemic lentiviral delivery of ACE2 in rats. Exp Physiol. 2005;90(5):783–90.
Yamamoto K, Ohishi M, Katsuya T, et al. Deletion of angiotensin-converting enzyme 2 accelerates pressure overload-induced cardiac dysfunction by increasing local angiotensin II. Hypertension. 2006;47(4):718–26.
Santos RA, Ferreira AJ, ESAC Simoes. Recent advances in the angiotensin-converting enzyme 2-angiotensin(1–7)-Mas axis. Exp Physiol. 2008;93(5):519–27.
Keidar S, Kaplan M, Gamliel-Lazarovich A. ACE2 Of the heart: from angiotensin I to angiotensin (1–7). Cardiovasc Res. 2007;73(3):463–9.
Grobe JL, Der Sarkissian S, Stewart JM, Meszaros JG, Raizada MK, Katovich MJ. ACE2 overexpression inhibits hypoxia-induced collagen production by cardiac fibroblasts. Clin Sci (Lond). 2007;113(8):357–64.
Zhao YX, Yin HQ, Yu QT, et al. ACE2 overexpression ameliorates left ventricular remodeling and dysfunction in a rat model of myocardial infarction. Hum Gene Ther. 2010;21(11):1545–54.
Lazartigues E, Feng Y, Lavoie JL. The two fACEs of the tissue renin-angiotensin systems: implication in cardiovascular diseases. Curr Pharm Des. 2007;13(12):1231–45.
Imai Y, Kuba K, Ohto-Nakanishi T, Penninger JM. Angiotensin-converting enzyme 2 (ACE2) in disease pathogenesis. Circ J. 2010;74(3):405–10.
Zisman LS, Keller RS, Weaver B, et al. Increased angiotensin-(1–7)-forming activity in failing human heart ventricles: evidence for upregulation of the angiotensin-converting enzyme Homologue ACE2. Circulation. 2003;108(14):1707–12.
Goulter AB, Goddard MJ, Allen JC, Clark KL. ACE2 gene expression is up-regulated in the human failing heart. BMC Med. 2004;2:19.
Ohtsuki M, Morimoto S, Izawa H, et al. Angiotensin converting enzyme 2 gene expression increased compensatory for left ventricular remodeling in patients with end-stage heart failure. Int J Cardiol. 2010;145(2):333–4.
• Epelman S, Tang WH, Chen SY, Van Lente F, Francis GS, Sen S. Detection of soluble angiotensin-converting enzyme 2 in heart failure: insights into the endogenous counter-regulatory pathway of the renin-angiotensin-aldosterone system. J Am Coll Cardiol. 2008;52(9):750–4. Demonstration of the clinical relevance of ACE2 in humans by detecting circulating ACE2 activity and its associations with disease severity.
Epelman S, Shrestha K, Troughton RW, et al. Soluble angiotensin-converting enzyme 2 in human heart failure: relation with myocardial function and clinical outcomes. J Card Fail. 2009;15(7):565–71.
Wang Y, Moreira Mda C, Heringer-Walther S, et al. Plasma ACE2 activity is an independent prognostic marker in Chagas' disease and equally potent as BNP. J Card Fail. 2010;16(2):157–63.
Shao Z, Shrestha K, Borowski AG, et al. Increasing serum soluble angiotensin-converting enzyme 2 activity after intensive medical therapy is associated with better prognosis in acute decompensated heart failure. J Card Fail. 2013;19(9):605–10.
Wysocki J, Ye M, Rodriguez E, et al. Targeting the degradation of angiotensin II with recombinant angiotensin-converting enzyme 2: prevention of angiotensin II-dependent hypertension. Hypertension. 2010;55(1):90–8.
Gallagher PE, Ferrario CM, Tallant EA. Regulation of ACE2 in cardiac myocytes and fibroblasts. Am J Physiol Heart Circ Physiol. 2008;295(6):H2373–9.
Lu N, Yang Y, Wang Y, et al. ACE2 gene polymorphism and essential hypertension: an updated meta-analysis involving 11,051 subjects. Mol Biol Rep. 2012;39(6):6581–9.
Vangjeli C, Dicker P, Tregouet DA, Shields DC, Evans A, Stanton AV. A polymorphism in ACE2 is associated with a lower risk for fatal cardiovascular events in females: the MORGAM project. J Renin Angiotensin Aldosterone Syst. 2011;12(4):504–9.
Zhou JB, Yang JK. Meta-analysis of association of ACE2 G8790A polymorphism with Chinese Han essential hypertension. J Renin Angiotensin Aldosterone Syst. 2009;10(1):31–4.
Der Sarkissian S, Huentelman MJ, Stewart J, Katovich MJ, Raizada MK. ACE2: A novel therapeutic target for cardiovascular diseases. Prog Biophys Mol Biol. 2006;91(1–2):163–98.
• Hernandez Prada JA, Ferreira AJ, Katovich MJ, et al. Structure-based identification of small-molecule angiotensin-converting enzyme 2 activators as novel antihypertensive agents. Hypertension. 2008;51(5):1312–7. Promising work on identifying ACE2 activators as therapeutic agents.
Ferreira AJ, Jacoby BA, Araujo CA, et al. The nonpeptide angiotensin-(1–7) receptor Mas agonist AVE-0991 attenuates heart failure induced by myocardial infarction. Am J Physiol Heart Circ Physiol. 2007;292(2):H1113–9.
Patel VB, Bodiga S, Fan D, et al. Cardioprotective effects mediated by angiotensin II type 1 receptor blockade and enhancing angiotensin 1–7 in experimental heart failure in angiotensin-converting enzyme 2-null mice. Hypertension. 2012;59(6):1195–203.
Masson R, Nicklin SA, Craig MA, et al: Onset of experimental severe cardiacfibrosis is mediated by overexpression of Angiotensin-converting enzyme 2.Hypertension 2009, 53(4):694-700.
Takahashi Y, Haga S, Ishizaka Y, Mimori A. Autoantibodies to angiotensin-converting enzyme 2 in patients with connective tissue diseases. Arthritis Res Ther. 2010;12(3):R85.
Compliance with Ethics Guidelines
Conflict of Interest
Mohammed A.R. Chamsi-Pasha declares that he has no conflict of interest.
Zhili Shao declares that he has no conflict of interest.
W.H.W. Wilson Tang is supported by National Institutes of Health grants R01HL103931 and P20HL113452, as well as grants from FoldRx Pharmaceuticals, Inc./Pfizer, Respicardia, Inc., and St. Jude Medical, Inc.; has received compensation from Medtronic, Inc., and St. Jude Medical, Inc. for service as a consultant.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chamsi-Pasha, M.A.R., Shao, Z. & Tang, W.H.W. Angiotensin-Converting Enzyme 2 as a Therapeutic Target for Heart Failure. Curr Heart Fail Rep 11, 58–63 (2014). https://doi.org/10.1007/s11897-013-0178-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11897-013-0178-0