Abstract
To inform future Dutch COVID-19 testing policies we did an experimental vignette study to investigate whether inclusion of the less reliable lateral flow tests (self-tests) would change test-uptake sufficiently to improve population-level test sensitivity. A representative sample (n = 3,270) participated in a 2-by-2 online experiment to evaluate the effects of test-guidelines including self-testing advice (IV1), and the effects of self-test availability (IV2) on expected test uptake (PCR test, self-test or no test) and sensitivity of the overall test strategy (primary outcome). Across four scenarios, changing test advice did not affect expected testing behaviour. Self-test availability, however, increased the timeliness of testing, the number of people testing, and overall test strategy sensitivity. Based on these findings, we recommend that (national) policy facilitates a supply of self-tests at home, for example through free and pro-active distribution of test-kits during a pandemic. This could substantially enhance the chances of timely detecting and isolating patients.
Similar content being viewed by others
Introduction
Throughout the pandemic, testing for COVID-19 has been key to monitoring the spread of SARS-CoV-2 and slowing down the spread of the virus through isolation of infected individuals, contact tracing and quarantine. Between July 2020 and May 2022, Dutch citizens with symptoms indicative of COVID-19 were eligible to test for free at test facilities from the Municipal Health Services (MHS) for (primarily) Polymerase chain reaction (PCR) tests. Government institutions have consistently advised citizens with symptoms indicative of a COVID-19 infection to get tested at MHS test facilities. This recommendation mostly has two purposes; (1) PCR tests have high test sensitivity, (2) contact tracing is centralised. Lateral Flow Tests for at-home use (self-tests) became available in the Netherlands in May 2021, and were introduced only for testing in situations for prevention, not in case of symptoms.
Despite these recommendations, the proportion of people self-testing with symptoms slowly but steadily increased and testing at MHS test facilities slowly but steadily decreased1. This suggests that an increasing proportion of people preferred (less sensitive) self-testing over testing at the MHS, in contrast to government recommendations. This deviation of citizen testing behaviour from governmental testing guidelines was also observed in the United Kingdom2,3. Various modelling studies suggest that turnaround time (i.e., how quickly people test after symptom onset) and frequency of testing are more important for COVID-19 control than test sensitivity4,5,6. Hence, changing from primarily a PCR testing strategy to a strategy that allows for the less sensitive but easier to conduct lateral flow tests, might translate into a higher probability of timely COVID-19 detection. The higher the prevalence of infection, the higher the positive predictive value of self-testing7. However, there are no studies that have experimentally examined the impact of such a policy change and other strategies (e.g., easier access to self-tests) on the effectiveness of the test strategy. The current study therefore addresses the following question: if the test policy would incorporate a recommendation to use a self-test in case of symptoms, would an increase in self-testing (lower sensitivity) increase overall test-uptake sufficiently to compensate for a possible decline in PCR-testing (higher sensitivity)?
Why was this transition in preference for self-testing observed in the first place? The practical benefits of self-tests are probably one of the main reasons self-test use increased, in the absence of government guidance. Self-tests are relatively easy to use independently and can provide immediate results, as a positive test result implies infectiousness. This also directly affects the tester as symptomatic people with a negative test result were not required to stay at home. A faster diagnosis would also contribute to the timeliness of contact tracing. In accordance with this line of thought, the WHO advised that self-testing should be offered in addition to professionally administered testing services8. Given these advantages, it is plausible that more people would test when self-testing is recommended in case of symptoms in addition to PCR testing. This could potentially also lead to people testing more promptly after symptom presentation, and more willingness to repeatedly test when regularly experiencing symptoms.
Besides government recommendations on what test to use, having self-tests readily available—as opposed to having to purchase them when symptomatic (which could also be a moment of increased risk of transmission)—could be another important factor influencing test uptake. Quasi-experimental research has shown that testing at MHS test facilities increases if the distance to test facilities decreases9. Other experimental evidence shows that willingness to use self-tests decreases when their costs increase10 but also that availability of tests influences isolation intention11. In the Netherlands, self-tests are widely available at supermarkets and pharmacies for approximately 3 euros per unit, whereas in countries such as the United Kingdom people could order self-tests free online. We were interested in examining the potential impact of people having self-tests available at home when experiencing symptoms as opposed to having to purchase them or asking someone else to do so. This could provide valuable insights for advising the government to pro-actively distribute free self-test supplies to Dutch citizens.
Given the impossibility of carrying out this research in a real-life randomized trial due to the time-sensitivity of the policy change and practical reasons, we decided to conduct a vignette study on the role of self-tests in close collaboration with epidemiologists and virologists with expertise in COVID-19 testing to advise the Dutch Outbreak Management Team and government. An experimental vignette allows researchers to manipulate independent variables and creates insight into causal relationships which made it a good design for studying test expectations12.
In this study we used an online, 2-by-2 vignette to investigate two hypotheses: first, that advising symptomatic people to either self-test or test at an MHS test facility, as opposed to only test at an MHS test facility, increases the probability of detecting positive cases, through an increase in testing and a decrease of time to testing. Second, that the availability of self-tests at home as opposed to having to purchase them, increases the probability of detecting positive cases, through an increase in testing and a testing more promptly after symptom onset. Additionally we explored if the probability of detecting positive cases would decline over time, as people were expected to test less frequently after consecutive episodes of symptoms, and if government advice and the availability of self-tests at home could counter this decline.
All scenarios were carefully designed by following the best practice recommendations to enhance accuracy and experimental realism12. Consenting participants were each presented with four episodes of symptoms over four consecutive months in the near future. The type of symptoms in each scenario, ranging from one to multiple symptoms, were based on their actual distribution in the population. Participants were first prompted to depict their typical activities on the relevant weekday in an open text box, which, in the vignettes, featured the initial symptoms occurring on a Tuesday. This step aimed to enhance realism and increase immersion. Next, they were asked to indicate whether—given their symptoms—they expected to not test, go to an MHS test facility or use a self-test that day. If participants did not select the MHS test facility (the optimal test), they were told their symptoms persisted for another 2 days and were asked again what test choice they expected to make. We assessed participants behavioural expectations, as this should reflect behavioural intentions (I plan to do x) adjusted for other influential factors such as past behaviour or specific circumstances on that day. Some studies suggest that behavioural expectations are better predictors of behaviour than behavioural intentions, although the evidence is mixed13,14,15,16,17.
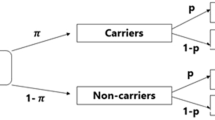
To test the hypotheses, respondents were randomly allocated to scenarios describing the testing advice: (1) ‘When you have corona-related symptoms, get tested at an MHS test facility’ (current government recommendation) or the adjusted advice: ‘When you have corona-related symptoms, get tested at an MHS test facility. If this is not possible, use a self-test’; and testing availability: (2) Having self-tests available at home versus not having a supply at home, when COVID-19 symptoms present. The primary outcome was overall strategy sensitivity: an average COVID-19 test sensitivity score based on participants’ test choices on day 1 and by day 3 of symptoms across all four scenarios, taking into account differences in self-test versus PCR tests detection probability (sensitivity)7,18 and considering that viral load is highest at the time of symptom onset19,20. Additionally, we examined whether participants opted for testing sooner, whether more people opted for testing, and whether this changed over time.
Results
Participant flow
Of the 6,053 participants who were approached for participation and were selected by an online research panel on demographic representativeness, 3,589 consented. Of those, 319 were excluded due to: fast completion (< 4 min; n = 17), not finishing the questionnaire (n = 286) and not answering crucial questions (n = 16) as per standard protocol from the data collection agency (not described in pre-registration). See Fig. 1 for participant flow diagram.
Descriptive statistics
From a total of 3,270 participants, 50.8% were female. Their median age was 53.3 (standard deviation = 17.3) years and 40.2% was highly educated. 79.5% said to have a Dutch background and 20.2% said to have a migration background (7.7% non-western and 12.5% western). Respondents reported to live alone (29.8%), with a partner (39.2%) or with a partner and children (20.5%). See Supplementary Materials (S1) for more details on demographics.
Across scenarios, respondents assigned to experience multiple symptoms (coughing, sneezing and a slight fever) relative to those assigned to experience one mild symptom indicated that they would test more often (90.3% vs. 74.9%), would do so sooner (77.3% vs. 53.5% immediately), and preferred to do so at an MHS test facility (57%) rather than by means of a self-test (19%) or by means of a self-test followed by a test at an MHS test facility (14%) (see Supplementary Materials S2).
By the third day of symptoms (day 1 and day 3 inclusive), respondents on average opted to test in 78.8% across the four episodes of symptoms (46.9% MHS test facility, 37.5% self-test and 15.5% both; 59.5% tested on day 1). Participants willingness to test varied with time (76.8% November, 81.6% December, 79.4% January, 77.3% February), with the highest test rate before the Christmas holidays: a behaviour we had actually observed in December 202021.
Primary analyses
We calculated the overall strategy sensitivity score (the probability of detecting positive cases) by converting the type of test chosen into the respective sensitivity scores on day 1 and by day 3 of symptoms averaged over all four scenarios, see “Methods” for details. There was no effect of changing the test advice on the overall strategy sensitivity score (F(2, 3265) = 0.43, p = 0.654). There was a significant effect of self-test availability at home on the overall strategy sensitivity scores, showing higher sensitivity scores when self-tests were available at home (F(2, 3265) = 38.5, p < 0.001, ηp2 = 0.023). This effect was present on day 1 (F(1, 3266) = 67.8, p < 0.001, ηp2 = 0.020) and still prevalent by day 3 of symptoms (F(1, 3266) = 19.3, p < 0.001, ηp2 = 0.006). There was no significant interaction between test advice and self-test availability (F(2, 3265) = 1.209, p = 0.299). Strategy sensitivity scores are shown in Fig. 2.
Secondary analysis
Next we analysed whether participants opted for testing sooner, and whether more people opted for testing. Test availability had a significant effect on the number of people that expected to test either at an MHS test facility or self-test (F(2, 3265) = 59.42, p < 0.001, ηp2 = 0.035). Moreover, when self-test were available at home, people expected to test sooner as more participants indicated to test on Day 1 than participants without self-tests at home (F(1, 3266) = 117.87, p < 0.001, ηp2 = 0.035). The significant effects found for testing sooner and more often are driven by the increase in use of self-tests. Also, more participants expected to test (by day 3 of symptoms) with self-tests at home than participants without self-tests at home (F(1, 3266) = 51.03, p < 0.001, ηp2 = 0.015). There was no effect of changing the test advice on expected test uptake or time to testing (F(2, 3265) = 0.31, p = 0.736).
The shift in choice of testing behaviour is shown in Fig. 3. On day 1, expected self-test use doubled resulting in 21.6% difference between groups using self-tests if self-tests were available at home. This comes paired with a decrease of 7.7% of testing at MHS test facilities.
Percentages of selected testing behaviours with COVID-19 symptoms averaged over 4 scenarios by testing advice (a) and availability of self-tests (b) on day 1 of symptoms and by day 3 of symptoms. By day 3 also contains participants who chose to visit the MHS test facility on day 1. Percentages above 100% represent participants who expected to use a self-test on day 1, and expected to go to the MHS test facility on day 3.
Consecutive episodes of symptoms over time on strategy sensitivity
We expected that strategy sensitivity would decline over time and that people would expect to test less after consecutive episodes of symptoms. However, we also expected that changing the testing advice towards allowing for self-tests in case of symptoms, and having self-tests available at home would counter this decline. Indeed, the consecutive episodes of symptoms over time yielded a significant main effect by day 1 (F(2.99, 9775.38) = 155.23, p = < 0.001, ηp2 = 0.045) and by day 3 of symptoms (F(2.97, 9690.01) = 34.57, p ≤ 0.001, ηp2 = 0.01). A Greenhouse–Geisser correction was used due to a violation of sphericity. Pairwise comparisons show that the increase in overall strategy sensitivity was especially large from November to December, after which a small decline set in, yet sensitivity scores remain higher than the start in November (Fig. 4a,b).
The four consecutive episodes of symptoms over time showed a significant interaction with testing advice on strategy sensitivity scores on day 1 (F(3, 3264) = 3.27, p = 0.020, η2 = 0.003) suggesting that the effect of testing advice varied over time: strategy sensitivity scores were slightly higher for the current government guideline testing advice (test at an MHS test facility) during the first two months, and then slightly higher for the (self-)testing advice during the last 2 months. This effect was, however minimal, no longer apparent by day 3 (F(3, 3264) = 1.158, p = 0.324). No other effects were found on consecutive episodes of symptoms, testing advice and availability of self-tests.
Robustness check
The primary outcome analyses were repeated using a 10% lower sensitivity score for self-tests (0.7 instead of 0.8 on day 1 and 0.6 instead of 0.7 on day 3), but the conclusions on governmental testing advice and availability remained. No difference was detected for testing advice (F(2, 3265) = 0.50, p > 0.05) and availability of self-tests at home still showed a significant difference in sensitivity scores between conditions (F(2, 3265) = 27.9, p < 0.001, ηp2 = 0.017). This effect remained strongest on day 1 (F(1, 3266) = 44.08, p < 0.001, ηp2 = 0.013) and remained in the maximum strategy sensitivity score on day 3 (F(1, 3266) = 8.68, p = 0.003, ηp2 = 0.003).
Discussion
In this vignette study we found that having self-tests available at home—but not the change in test advice—substantially increased respondents expected test uptake, reduced time to testing, and led to an increase in the overall strategy sensitivity. Following this study the Dutch Outbreak Management Team advised the government to provide free self-tests to all Dutch citizens. An advice that was, however, not followed-up because of market regulation issues. Free self-tests were already provided to people attending food banks, and to students.
In the study, we observed no changes in expected test uptake following a change in testing advice. We note that quite a number of people had already been using self-tests to determine if their symptoms were due to COVID-19. This could explain why we did not observe a difference in people’s expected testing behaviour. It could also be possible that the message was not correctly comprehended by the respondents, as the message was not pre-tested. However, the scenario was under direct consideration by the Dutch Outbreak Management Team during the time of the study. After this study was conducted, Dutch governmental testing advice changed to include a recommendation to self-test when experiencing symptoms. Survey research has since shown that people did report using more self-tests after the advice changed (39% with corona-related symptoms) than before (28.7%)1. Nevertheless this increase could have been caused by the increased attention for COVID-19 due to the simultaneous infection peak that occurred upon the introduction of Omicron.
Having self-tests available at home decreased the expected time to testing and substantially increased the number of people who expected to test. Modelling studies have shown that frequent testing, i.e. increasing COVID-19 detection probability, is beneficial for mitigation of COVID-194,5,6. Furthermore, viral shedding is highest on or just before onset of symptoms19, and early transmission could therefore be reduced with sooner testing. This may indicate that providing free self-tests can help mitigate pandemics. Some governments, such as in the UK, have provided free self-tests to the population during the pandemic22, which is likely to reduce (financial) barriers to having self-tests at home and thus promote more rapid testing following the onset of symptoms23. Evaluation of this widescale testing pointed towards positive effects on public health24.This serves as a strong start to improving test uptake, but some groups may need additional provisions as research shows that higher education and above average income is positively associated with motivation to use and order self-tests25, and that costs of self-tests are related to intended use10. Research on self-reported testing behaviour shows that respondents who find self-tests more expensive report to use self-tests less often with corona-related symptoms. Interestingly, this effect was found across various person characteristics, including those with higher education (as an indicator of financial capacity)26. As costs of self-tests could pose a barrier to having self-tests available and using self-tests, providing sufficient self-tests for free would provide a good alternative across the population27.
Finally, we did not find evidence of test fatigue, where consecutive episodes of symptoms over time would lead to decline in test uptake28. It is possible that the hypothetical nature of our study was not optimal for detecting this. Instead, we have been seeing a modest but steady increase in test uptake over time as self-testing became increasingly popular29. Attesting to the validity of our findings, the peak in strategy sensitivity in December was mirrored by self-reported testing data from the corona behavioural unit cohort study and can most probably be explained by December being a traditional time to celebrate with family, when respondents do not want to risk infecting loved ones1,16. There are also other indications of the validity of the results from this Vignette study. For example, socio-demographic predictors of expected test behaviour in the Vignette study are similar to those we have seen in our ongoing surveys: women, vaccinated respondents, younger and higher educated respondents test more frequently1,2,3. Also, severity of symptoms in the scenarios was predictive of expected test uptake, in the same way as we have seen in surveys on actual test uptake1,2,30. These comparisons support the conclusions from this vignette study, and of the method more generally, as having predictive value.
Strengths of this study are the carefully-designed scenarios using available data (e.g., on type of symptoms and their frequency) and following best-practice guidelines, the multi-disciplinary research team, the nationally representative data and the comparisons that support its validity. Limitations are that this is, ultimately, a vignette study using expected behaviour as an outcome and that conclusions are based on assumptions about the sensitivity of PCR and self-tests. As self-tests may be somewhat less sensitive for Omicron, the variant that rapidly took over in December 2022, than Delta7, the variant that circulated between July 2021 and December 2022, this could affect the relevance of the results. However all results were similar when we assumed a 10% lower sensitivity scores for self-tests than Delta sensitivity scores. The self-test availability hypothesis was accidentally categorised under follow-up analysis in the study’s registration. However, as the study was designed and powered with the availability-arm as a main hypothesis in mind, as further described in the pre-registration, we believe we have remained true to our pre-registration.
In conclusion, self-testing for COVID-19 appears to be a relatively low-effort activity that many people agree to doing immediately when symptoms present themselves. Although this study did not provide evidence to support modifications in self-test advice, it did show a substantial effect of having self-tests available at home on expected test uptake. As costs do pose a barrier to testing10,23,26 we recommend governments to pro-actively provide free self-tests to all its citizens—as the timely detection of COVID-19, immediate isolation and consecutive contact tracing are highly effective strategies in reducing the spread of SARS-CoV-2.
Methods
Study design
We did an online randomized hypothetical scenario study (vignette study) in which participants were randomised to assess four scenarios. Between subject we manipulated the testing advice (IV1; 2 levels) and the availability of self-tests (IV2; 2 levels). Corona-related symptoms were presented at random (IV3; 4 levels). We asked participants to assess their most likely behaviour on day 1 of symptoms and day 3 of unchanged symptoms (Time 1: Day of corona-related symptoms; 2 levels). And new episodes of symptoms over time were presented in additional vignettes referring to later months (Time 2: Consecutive episodes of symptoms over time; 4 levels). Symptoms (75% only one symptom and 25% more than one symptom) were based on symptom profiles found in Dutch national research1. See Table 1 for independent variables. We commissioned the data collection agency I&O Research to carry out this online vignette study, between 11 and 16th of November 2021. The Medical Review Ethics Committee of the National Institute of Public Health and the Environment (RIVM) of the Netherlands reviewed the study proposal and confirmed that the study met the ethical standards for human participation research and confirmed that further clinical approval was not needed [G&M-537]. The study was pre-registered at ClinicalTrials.gov [NCT05215483]. All methods were carried out in accordance with relevant guidelines and regulations.
Participants
Participants were recruited by I&O Research using an online research panel representative of the Dutch population. Subjects were eligible if they were aged 18 and above, and living in the Netherlands. Invitations were sent to a selected sample based on the demographics age, gender, educational level, region and to best effort migration background. For full descriptives see Supplementary Materials (S1). Participants received credits interchangeable for online purchases for participating and informed consent was obtained from all participants.
36% of participants reported to have experienced corona-related symptoms during the past six weeks, not caused by underlying medical issues. 54.8% of these respondents say to have tested due to these symptoms, either at an MHS test facility (21.4%), with self-tests (26.3%) or both (7.1%). This is slightly higher than numbers found in Dutch representative sample studies (November 2021: 43%) during the same timeframe29.
21.8% of respondents report to have underlying medical issues, 18.7% have confirmed to have been tested (no self-tests) in the past 6 weeks, and 30.5% have used (at least one) self-tests in the past 6 weeks. 19.7% were experiencing corona-related symptoms during the vignette study (such as a cold, or sneezing or coughing). 18.8% (think) to have been infected with corona in the past and 91.6% are fully vaccinated for corona. Although the data collection agency aimed to provide a representative sample and was successful regarding demographics, the percentage of fully vaccinated participants (91.6%) was higher than the Dutch average in November 2021 of ~ 84%31.
Interventions
Participants were automatically randomised at the start of the survey to one of four groups (advice × availability). Corona-related symptoms were randomised before the start of each scenario. Participants were asked to describe their activities on a regular Tuesday to increase immersion and informed that it is normal that people do not always follow the testing guidelines12. Participants were then presented with a vignette where they would wake up on a Tuesday with corona-related symptoms, their testing advice, visually presented in style of the Dutch corona campaign and text (Supplementary Materials S3), and their selected availability of self-tests in text and asked what they expected that their most likely behaviour would be: (1) no test (2) wait and see how symptoms develop (3) make an appointment with an MHS test facility or (4) use a self-test/arrange for and use a self-tests. Participants who did not choose the test facility on day 1 were presented with the same vignette referring to day 3 with unchanged symptoms, and were asked their most likely behaviour again. Participants were not aware of the hypothesis of the study.
Study materials
We used an online questionnaire including four vignettes (see Supplementary Materials S4). Additional questions concerned demographics, previous test experience, risk profile for corona, corona-related symptoms, reasons to (not) get tested (PCR or self-tests), vaccination status, previous corona infection, own availability of self-tests, distance to nearest MHS test facility, perceived reliability self-tests, descriptive norm, risk perception, self-efficacy and response efficacy. Psychosocial constructs were measured as previous research has shown that these constructs are significant predictors for test-uptake32. Questions were based on the Dutch Cohort Questionnaire33.
Outcomes
The primary outcomes were defined as the average strategy sensitivity over time, referring to the probability of detecting positive cases. The sensitivity of the test chosen after symptoms onset was used to convert each answer: MHS test facility on day 1 or day 3 = 1, self-test on day 1 = 0.8, self-test on day 3 = 0.7, Wait and see and No test on day 1 or day 3 = 07,18. Sensitivity refers to a test’s ability to designate an individual with disease as positive. For strategy sensitivity scores on day 1 of symptoms, day 1 sensitivity scores from all four scenarios were averaged. To determine sensitivity scores by the third day of testing, the highest score was selected from day 1 or day 3 of symptoms per scenario and averaged over all four scenarios. We refer to this accumulated score as “by day 3 of symptoms”. Participants who chose to visit the MHS test facility on day 1 were not asked about their most likely behaviour again on day 3, therefore scores from day 1 were used to calculate sensitivity scores by day 3. Sensitivity scores of self-tests on day 1 are higher than day 3 as viral loads were observed to peak at the onset of symptoms and subsequently decrease19,20. Secondary outcomes were willingness to test sooner (day 1, self-tests or MHS test facility, averaged over four scenarios); and if respondents would test more often (by the third day of symptoms, self-tests or MHS test facility, averaged over four scenarios).
Power
In our sample size calculations we estimated a two tailed t-test to calculate the difference between two independent groups. This resulted in a total of 1,302 participants for 95% power (α = 0.05). As three days were scheduled for data collection, we oversampled and sent out 6.053 invitations.
Statistical methods
Sensitivity scores (day 1 and by day 3) were normally distributed based on the Skewness (day 1: − 0.27, by day 3: − 1.09) and Kurtosis (day 1: − 1.28, day 3: 0.06). Variance between groups was not equal, as shown by a significant Levene’s test for sensitivity scores on day 1 (F(3, 3266) = 6.469, p < 0.001), and by day 3 (F(3, 3266) = 25.10, p < 0.001) and Box’s test of equality of covariance matrices was significant (F(9, 119192744) = 13.594, p < 0.001) and therefore not all assumptions were met for parametric testing. Yet based on the large sample size and the central limit theorem, parametric tests were used to analyse the data.
As we hypothesised that changing the governmental advice on testing, and having self-tests available at home would increase the strategy sensitivity for citizens with COVID-19 symptoms on day 1 and by day 3 we used a Multivariate GLM with Bonferroni correction. Secondary outcomes, predicting that respondents would test sooner and more often, were also analysed using Multivariate GLM.
Finally, to analyse the predicted decline in strategy sensitivity over time, due to a repeated incidence of symptoms over time, we used a repeated measures ANOVA for strategy sensitivity scores on day 1 and by day 3. Analyses were done in SPSS version 28.
Data availability
The data that support the findings of this study are not publicly available due to the European privacy regulation (GDPR) and participants of this study did not give written consent for their data to be shared publicly. Aggregated data are available from the corresponding author, C.Z., upon reasonable request.
References
National Institute for Public Health and the Environment (RIVM). Dutch cohort questionnaire behaviour and wellbeing, https://www.rivm.nl/gedragsonderzoek/maatregelen-welbevinden (2022).
Smith, L. E. et al. Do members of the public think they should use lateral flow tests (LFT) or polymerase chain reaction (PCR) tests when they have COVID-19-like symptoms? The COVID-19 Rapid Survey of Adherence to Interventions and Responses study. Public Health 198, 260–262. https://doi.org/10.1016/j.puhe.2021.07.023 (2021).
Smith, L. E. et al. Who is engaging with lateral flow testing for COVID-19 in the UK? The COVID-19 Rapid Survey of Adherence to Interventions and Responses (CORSAIR) study. BMJ Open 12, e058060. https://doi.org/10.1136/bmjopen-2021-058060 (2022).
Larremore, D. B. et al. Test sensitivity is secondary to frequency and turnaround time for COVID-19 screening. Sci. Adv. https://doi.org/10.1126/sciadv.abd5393 (2021).
Paltiel, A. D., Zheng, A. & Sax, P. E. Clinical and economic effects of widespread rapid testing to decrease SARS-CoV-2 transmission. Ann. Intern. Med. 174, 803–810. https://doi.org/10.7326/m21-0510 (2021).
Mina, M. J., Parker, R. & Larremore, D. B. Rethinking Covid-19 test sensitivity—A strategy for containment. N. Engl. J. Med. 383, e120. https://doi.org/10.1056/NEJMp2025631 (2020).
Schuit, E. et al. Diagnostic accuracy of Covid-19 rapid antigen tests with unsupervised self-sampling in people with symptoms in the omicron period: Cross sectional study. BMJ 378, e071215. https://doi.org/10.1136/bmj-2022-071215 (2022).
WHO. Use of SARS-CoV-2 Antigen-Detection Rapid Diagnostic Tests for COVID-19 Self-testing (World Health Organization, 2022).
Sanders, J. G. et al. The effect of proximity of COVID-19 test facilities on test uptake: Two quasi-experimental trials. https://doi.org/10.31234/osf.io/rhvmc (2022).
Betsch, C. et al. Empirical evidence to understand the human factor for effective rapid testing against SARS-CoV-2. Proc. Natl. Acad. Sci. USA https://doi.org/10.1073/pnas.2107179118 (2021).
Zhang, J. C. et al. Examining the role of COVID-19 testing availability on intention to isolate: A randomized hypothetical scenario. PLoS ONE https://doi.org/10.1371/journal.pone.0262659 (2022).
Aguinis, H. & Bradley, K. J. Best practice recommendations for designing and implementing experimental vignette methodology studies. Organ. Res. Methods 17, 351–371. https://doi.org/10.1177/1094428114547952 (2014).
Armitage, C. J., Norman, P., Alganem, S. & Conner, M. Expectations are more predictive of behavior than behavioral intentions: Evidence from two prospective studies. Ann. Behav. Med. 49, 239–246. https://doi.org/10.1007/s12160-014-9653-4 (2015).
Courneya, K. S. & McAuley, E. Are there different determinants of the frequency, intensity, and duration of physical activity?. Behav. Med. 20, 84–90. https://doi.org/10.1080/08964289.1994.9934621 (1994).
Sheppard, B., Hartwick, J. & Warshaw, P. The theory of reasoned action: A meta-analysis of past research with recommendations for modifications and future research. J. Consumer Res. https://doi.org/10.1086/209170 (1988).
Sheeran, P. & Orbell, S. Do intentions predict condom use? Meta-analysis and examination of six moderator variables. Br. J. Soc. Psychol. 37(Pt 2), 231–250. https://doi.org/10.1111/j.2044-8309.1998.tb01167.x (1998).
Webb, T. L. & Sheeran, P. Does changing behavioral intentions engender behavior change? A meta-analysis of the experimental evidence. Psychol. Bull. 132, 249–268. https://doi.org/10.1037/0033-2909.132.2.249 (2006).
Schuit, E. et al. Head-to-head comparison of the accuracy of saliva and nasal rapid antigen SARS-CoV-2 self-testing: Cross-sectional study. BMC Med. 20, 406. https://doi.org/10.1186/s12916-022-02603-x (2022).
He, X. et al. Temporal dynamics in viral shedding and transmissibility of COVID-19. Nat. Med. 26, 672–675. https://doi.org/10.1038/s41591-020-0869-5 (2020).
Stankiewicz Karita, H. C. et al. Trajectory of viral RNA load among persons with incident SARS-CoV-2 G614 infection (Wuhan Strain) in association with COVID-19 symptom onset and severity. JAMA Netw Open 5, e2142796. https://doi.org/10.1001/jamanetworkopen.2021.42796 (2022).
Corona Dashboard. Testing with corona-related symptoms https://coronadashboard.rijksoverheid.nl/landelijk/gedrag (2023).
Crozier, A., Rajan, S., Buchan, I. & McKee, M. Put to the test: Use of rapid testing technologies for Covid-19. BMJ 372, n208. https://doi.org/10.1136/bmj.n208 (2021).
Hajek, A. & König, H. H. Willingness to pay for SARS-CoV-2 rapid antigen tests during the COVID-19 pandemic: Evidence from the general adult population. Public Health 207, 19–23. https://doi.org/10.1016/j.puhe.2022.03.016 (2022).
UK Health Security Agency. COVID-19: general public testing behaviours, https://www.gov.uk/government/publications/lfd-tests-how-and-why-they-were-used-during-the-pandemic/covid-19-general-public-testing-behaviours (2023).
Bien-Gund, C. et al. Factors associated with US public motivation to use and distribute COVID-19 self-tests. JAMA Netw. Open 4, e2034001–e2034001. https://doi.org/10.1001/jamanetworkopen.2020.34001 (2021).
National Institute for Public Health and the Environment (RIVM). Affordability of self-tests and testing behaviour, https://www.rivm.nl/gedragsonderzoek/betaalbaarheid-van-zelftesten-en-testgedrag (2022).
D&B. Use of self-tests at the food bank (Dutch). 1–30 (Rijksoverheid, 2021).
World Health Organization. Regional Office for, E. Pandemic fatigue—Reinvigorating the public to prevent COVID-19: Policy framework for supporting pandemic prevention and management. (World Health Organization. Regional Office for Europe, Copenhagen, 2020).
National Institute for Public Health and the Environment (RIVM). Dutch national trend data on behaviour and support COVID-19, https://www.rivm.nl/gedragsonderzoek/trendonderzoek (2023).
Mowbray, F., Woodland, L., Smith, L. E., Amlôt, R. & Rubin, G. J. Is my cough a cold or Covid? A qualitative study of COVID-19 symptom recognition and attitudes toward testing in the UK. Front. Public Health https://doi.org/10.3389/fpubh.2021.716421 (2021).
Valk, A. et al. Vaccinatiegraad COVID-19 Vaccinatie Nederland, 2021 (Rijksinstituut voor Volksgezondheid en Milieu RIVM, 2022).
Smith, L. E. et al. Factors associated with adherence to self-isolation and lockdown measures in the UK; A cross-sectional survey. Public Health 187, 41 (2020).
van den Boom, W. et al. Cohort profile: The Corona Behavioral Unit cohort, a longitudinal mixed-methods study on COVID-19-related behavior, well-being and policy support in the Netherlands. PLOS ONE 18, e0289294. https://doi.org/10.1371/journal.pone.0289294 (2023).
Acknowledgements
We would like to thank our colleagues with the National Institute for Public Health and the Environment (RIVM) Sacha de Stoppelaar, George Sips, Mariska Hafkamp, Wijnand van den Boom and Mart van Dijk for their expertise.
Funding
This study is funded by the National Institute for Public Health and the Environment of the Netherlands.
Author information
Authors and Affiliations
Contributions
M.B., R.J., F.K., J.S. and C.Z. contributed to conceptualisation and methodology of the study. C.Z. performed the statistical analysis and wrote the initial draft of the manuscript. All authors contributed to the interpretation of the results. M.B., F.K., J.S. and R.J. critically revised and complemented the manuscript. All authors contributed, reviewed, and accepted the final version of the manuscript for submission. C.Z. was responsible for the project administration. M.B., F.K. and R.J. supervised research activities.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zomer, C.L., Kroese, F., Sanders, J.G. et al. Estimating the impact of COVID-19 self-test availability and modifications in test-strategy on overall test uptake using an experimental vignette study. Sci Rep 14, 5887 (2024). https://doi.org/10.1038/s41598-024-54988-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-54988-9
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.