Gross Anatomy
The anatomy of the large intestine includes the cecum (along with appendix) and the colon; in some descriptions (and the author agrees), it also includes the anorectum (rectum and anal canal). [1, 2, 3, 4, 5]
The large intestine, which is the terminal part of gastrointestinal (GI) tract, is so called because its lumen (diameter) is larger, not because its length is greater, than that of the small intestine (duodenum, jejunum, ileum); in fact, small intestine is longer than the large intestine. The large intestine develops partly from the midgut (from cecum to distal transverse colon), the hindgut (from distal transverse colon to dentate line in anorectum), and proctodeum (below the dentate line).
The cecum, which is the proximal blind end (pouch) of the ascending (right) colon, is a blind cul-de-sac below the level of the ileocecal junction that lies in the right iliac fossa. The terminal ileum opens into the cecum at its medial wall, and the opening is guarded by an ileocecal valve.
The appendix (an appendage of the cecum), also called vermiform process or vermiform appendix, is a tubular structure with a blind end attached to the cecum. The base of the appendix lies on the posteromedial wall of the cecum 1-2 cm below the ileocecal junction. The tip of the appendix, however, floats in the peritoneal cavity and may be pelvic, preileal, postileal, or even retrocecal in position.
The cecum (the widest part of large intestine) leads to the ascending (right) colon, which ascends vertically from right iliac fossa through the right lumbar region into right hypochondrium under the liver. It then takes a right turn and continues as the horizontally placed transverse colon, which reaches across the epigastrium to the left hypochondrium under the spleen. It then takes a right turn again and descends vertically through the left lumbar region to the left iliac fossa as the descending (left) colon. The descending colon is followed by the inverted V-shaped sigmoid colon (the narrowest part of colon), which becomes the rectum at S3 level. The cecum and colon have 3 longitudinal muscular bands called tenia and multiple sacculations called haustra.
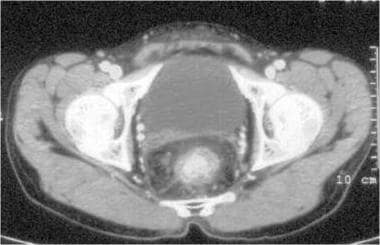
The rectum lies in the concavity of the sacrococcygeal hollow and changes to the anal canal at the anorectal angle created by the puborectal sling formed by the innermost fibers of the levator ani muscle. The rectum has a dilated middle part called the ampulla, which contains 3 semilunar transverse mucosal folds called "valves of Houston." The rectum is related anteriorly to the urinary bladder (see the image below), prostate, seminal vesicles, and urethra in males and to the uterus, cervix, and vagina in females. Anterior to the rectum is the rectovesical pouch in males and the rectouterine pouch in females. The rectum changes to anal canal at the level of the coccyx. The anal canal is related to the perineal body in front and the anococcygeal body behind; both of these are fibromuscular structures.
The greater omentum (gastrocolic ligament) is like an apron with 4 layers of peritoneum (often fused). Two layers go down from stomach and then run upward to be attached to the transverse colon.
The appendix, transverse colon, and sigmoid colon have a mesentery (called mesoappendix, transverse mesocolon and sigmoid mesocolon, respectively), but the ascending colon and descending colon and the rectum and anal canal are retroperitoneal; the cecum does not have its own mesentery but is covered in all aspects by peritoneum.
There are several peritoneal fossae (eg, superior and inferior ileocecal, subcecal, retrocecal) around the cecum, which can be sites of internal herniation of the small bowel. Transverse mesocolon, containing the middle colic vessels, is attached to the anterior surface of the pancreas. Sigmoid mesocolon, containing superior rectal vessels, has an inverted-V – shaped attachment to the posterior abdominal wall — the tip of the V lying on the pelvic brim over the left ureter. The rectum does not have a proper mesentery, but the soft tissue around the rectum is often referred to as "mesorectum" by surgeons.
The posterior surface of entire rectum is retroperitoneal (extraperitoneal). Its upper third is covered by peritoneum on the front and sides, the middle third is covered by peritoneum on the front only, and the lower third is completely retroperitoneal (extraperitoneal).
The large intestine, especially the colon, is covered with numerous omental appendages (appendices epiploicae)—appendages of fat, each containing a vessel of its own from the colonic wall. These are visible during surgery.
Histology
The large intestine has the same 4 layers found in most parts of the GI tract. They are as follows:
-
Mucosa - Includes a columnar epithelium with large number of mucus-secreting goblet cells (villi; present in small intestine; absent in colon), lamina propria, and muscularis mucosa; the appendix is rich in mucosa-associated lymphoid tissue (MALT)
-
Submucosa - Contains the blood vessels and Meissner nerve plexus
-
Muscularis propria - Contains continuous inner circular and outer longitudinal muscles arranged in bands and myenteric (Auerbach) nerve plexus; tenia coli are formed by bands of the outer longitudinal muscles (tinea are present in the colon only and are not present in the rectum, where the outer longitudinal muscle is continuous)
-
Serosa - Visceral peritoneum
Natural Variants
In malrotation of the gut, the entire large intestine lies in the left half of the abdomen (the right half is occupied by loops of small intestine).
Pathophysiological Variants
A cecum with mesentery is mobile and prone to volvulus.
The ileocecal valve is usually competent; colonic obstruction, therefore, may cause a closed loop, leading to cecal distension without small bowel dilatation. If the ileocecal valve is incompetent, colonic obstruction results in small bowel dilatation.
The colon, especially the sigmoid colon, may develop diverticula that can be complicated by infection (diverticulitis) or bleeding.
Blood Supply
The large intestine is supplied by branches of the superior mesenteric artery (SMA), as follows:
-
Ileocolic artery through its cecal and appendicular branches
-
Right colic artery, which has a descending (anastomoses with the cecal artery) and an ascending branch
-
Middle colic artery, which has a right (anastomoses with the ascending branch of right colic artery) and a left branch and
The large intestine is supplied by the branches of the inferior mesenteric artery (IMA) as follows:
-
Left colic artery, which has an ascending (anastomoses with the left branch of the middle colic artery) and a descending branch
-
Multiple sigmoid arteries
-
Superior rectal artery
The arc of Riolan (meandering mesenteric artery) is a communication between SMA and IMA.
Anorectum also receives blood supply from the internal iliac arteries as follows:
-
Middle rectal artery
-
Inferior rectal artery (a branch of internal pudendal artery)
A continuing series of anastomoses between the distal branch of the proximal artery and the proximal branch of the distal artery runs along the mesenteric (inner) border of colon and is called the marginal artery of Drummond. The terminal branches of this arcade entering the wall of the large intestine are called the vasa recta; "core colectomy" for ulcerative colitis is performed by dividing the vasa recta between the colonic wall and the marginal artery. This arcade is poorest at the splenic flexure; ischemic colitis and strictures are, therefore, most common at the splenic flexure.
The superior mesenteric vein (SMV) accompanies the superior mesenteric artery (SMA), but the inferior mesenteric vein (IMV) does not accompany the inferior mesenteric artery (IMA). The inferior mesenteric vein runs vertically upward to the left of the duodenojejunal junction (flexure) and joins the splenic vein or its junction with the superior mesenteric vein (to form the portal vein).
Lymphatics of the large intestine drain into the epicolic (on the intestine), pericolic (next to intestine), intermediate (along branches of vessels), and the main (also named ileocolic, right colic, middle colic, and left colic arteries) lymph nodes.
Imaging of the Large Intestine Radiologic appearance of the large intestine
On plain abdominal radiographs, the large intestine appears to be filled with air and some fecal material. The maximum diameter of the cecum is 9 cm; the maximum diameter of the colon is 6 cm. The colon is identified by its irregular, incomplete sacculations (haustra). (See the image below)
Imaging studies
The large intestine can be evaluated with lower GI endoscopy (anoproctosigmoid colonoscopy) and lower GI series (enema) using radiologic contrast media (eg, barium, Gastrografin). Late films of a barium follow-through study may also show large intestine.
The large intestine's wall and masses in the large intestine can be evaluated with contrast-enhanced (intravenous and rectal contrast) computed tomography (CT) scanning. Reconstruction of CT scans (CT colonography) gives as good an inside view of the colon as does colonoscopy (virtual colonoscopy). Magnetic resonance imaging (MRI) is useful for evaluation of the anorectum. Ultrasonography is not useful for the evaluation of the large intestine, but endoscopic ultrasonography (EUS) is useful in evaluation of the anorectum.
Endoscopy
The total length of the small bowel is about 150 cm; colonoscopes, therefore, are 160-200 cm long. On anoproctosigmoidocolonoscopy, the dentate line, rectal vales, colonic haustra, and flexures are well appreciated.
Physiology
The proximal large intestine absorbs water and some electrolytes; the distal large intestine is mainly for storage and expulsion of feces.
-
Rectum with urinary bladder in front in a male patient
-
Redundant transverse colon
-
Splenic (left) flexure higher than hepatic (right) flexure
-
Total colectomy specimen
-
Anatomy of the large intestine.
-
Haustra of descending (left) colon