Abstract
Purpose
Age-related factors including oxidative stress play an important role in prostate carcinogenesis. We hypothesize that germline single-nucleotide polymorphisms (SNPs) in oxidative stress pathway are associated with prostate cancer (PCa) risk. In this study, we aim to examine which of these SNPs is associated with PCa.
Methods
Participants included in this analyses came from the “Genetic Susceptibility, Environment and Prostate Cancer Risk Study” conducted at the Veterans Affairs Portland Health Care System. After applying exclusion criteria, 231 PCa cases and 382 prostate biopsy-negative controls who had genotyping data on twenty-two single-nucleotide polymorphisms (SNPs) in six genes (MAPK14, NRF2, CAT, GPX1, GSTP1, SOD2, and XDH) associated with oxidative stress pathway were included in the analyses. The genotyping of SNPs was conducted by the Illumina BeadXpress VeraCode platform. We investigated these SNPs in relation to overall and aggressive PCa risk using logistic regression models controlling for relevant covariates.
Results
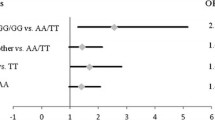
One SNP in the MAPK14 (rs851023) was significantly associated with incident PCa risk. Compared to men carrying two copies of allele A, the presence of one or two copies of the G allele was associated with decreased risk of PCa [OR (95% CI) 0.19 (0.06–0.51)]. There was no statistically significant association between other SNPs in the NRF2, CAT, GPX1, GSTP1, SOD2, and XDH genes and PCa risk.
Conclusions
The MAPK14 gene SNP rs851023 was associated with PCa and aggressive PCa risk after multiple comparison adjustment. Further studies in other populations or functional studies are needed to validate the finding.

Similar content being viewed by others
Abbreviations
- ANOVA:
-
Analysis of variance
- BIC:
-
Bayesian information criterion
- BMI:
-
Body mass index
- 95% CI:
-
95% confidence interval
- GSEP:
-
Genetic Susceptibility, Environment and Prostate Cancer Risk
- NCI:
-
National Cancer Institute
- OHSU:
-
Oregon Health & Science University
- PIN:
-
Prostatic intraepithelial neoplasia
- PSA:
-
Prostate-specific antigen
- PSAD:
-
Prostate-specific antigen density
- SE:
-
Standard Error
- VAPHCS:
-
VA Portland Health Care System
References
Siegel RL, Miller KD, Jemal A (2016) Cancer statistics, 2016. CA Cancer J Clin 66:7–30
Udensi UK, Tchounwou PB (2016) Oxidative stress in prostate hyperplasia and carcinogenesis. J Exp Clin Cancer Res 35:139
Oh B, Figtree G, Costa D et al (2016) Oxidative stress in prostate cancer patients: a systematic review of case control studies. Prostate Int 4:71–87
Kregel KC, Zhang HJ (2007) An integrated view of oxidative stress in aging: basic mechanisms, functional effects, and pathological considerations. Am J Physiol Regul Integr Comp Physiol 292:R18–R36
Roumeguere T, Sfeir J, El Rassy E et al (2017) Oxidative stress and prostatic diseases. Mol Clin Oncol 7:723–728
Arsova-Sarafinovska Z, Eken A, Matevska N et al (2009) Increased oxidative/nitrosative stress and decreased antioxidant enzyme activities in prostate cancer. Clin Biochem 42:1228–1235
Desideri E, Vegliante R, Cardaci S, Nepravishta R, Paci M, Ciriolo MR (2014) MAPK14/p38alpha-dependent modulation of glucose metabolism affects ROS levels and autophagy during starvation. Autophagy 10:1652–1665
Abrigo J, Elorza AA, Riedel CA et al (2018) Role of oxidative stress as key regulator of muscle wasting during cachexia. Oxid Med Cell Longev 2018:2063179
Eeles RA, Kote-Jarai Z, Giles GG et al (2008) Multiple newly identified loci associated with prostate cancer susceptibility. Nat Genet 40:316–321
Thomas G, Jacobs KB, Yeager M et al (2008) Multiple loci identified in a genome-wide association study of prostate cancer. Nat Genet 40:310–315
Geybels MS, van den Brandt PA, van Schooten FJ, Verhage BA (2015) Oxidative stress-related genetic variants, pro- and antioxidant intake and status, and advanced prostate cancer risk. Cancer Epidemiol Biomark Prev 24:178–186
Hu J, Feng F, Zhu S et al (2015) Catalase C-262T polymorphism and risk of prostate cancer: evidence from meta-analysis. Gene 558:265–270
Ntais C, Polycarpou A, Ioannidis JP (2005) Association of GSTM1, GSTT1, and GSTP1 gene polymorphisms with the risk of prostate cancer: a meta-analysis. Cancer Epidemiol Biomark Prev 14:176–181
Martignano F, Gurioli G, Salvi S et al (2016) GSTP1 methylation and protein expression in prostate cancer: diagnostic implications. Dis Mark 2016:4358292
Men T, Zhang X, Yang J et al (2014) The rs1050450 C > T polymorphism of GPX1 is associated with the risk of bladder but not prostate cancer: evidence from a meta-analysis. Tumour Biol 35:269–275
Geybels MS, van den Brandt PA, Schouten LJ et al (2014) Selenoprotein gene variants, toenail selenium levels, and risk for advanced prostate cancer. J Natl Cancer Inst 106:dju003
Kang SW (2015) Superoxide dismutase 2 gene and cancer risk: evidence from an updated meta-analysis. Int J Clin Exp Med 8:14647–14655
de Jong K, Vonk JM, Imboden M et al (2017) Genes and pathways underlying susceptibility to impaired lung function in the context of environmental tobacco smoke exposure. Respir Res 18:142
Son Y, Cheong YK, Kim NH, Chung HT, Kang DG, Pae HO (2011) Mitogen-activated protein kinases and reactive oxygen species: how can ROS activate MAPK pathways? J Signal Transduct 2011:792639
Mulholland DJ, Kobayashi N, Ruscetti M et al (2012) Pten loss and RAS/MAPK activation cooperate to promote EMT and metastasis initiated from prostate cancer stem/progenitor cells. Cancer Res 72:1878–1889
Rodriguez-Berriguete G, Fraile B, Martinez-Onsurbe P, Olmedilla G, Paniagua R, Royuela M (2012) MAP kinases and prostate cancer. J Signal Transduct 2012:169170
Jiang Y, Chen C, Li Z et al (1996) Characterization of the structure and function of a new mitogen-activated protein kinase (p38beta). J Biol Chem 271:17920–17926
Huang X, Chen S, Xu L et al (2005) Genistein inhibits p38 map kinase activation, matrix metalloproteinase type 2, and cell invasion in human prostate epithelial cells. Cancer Res 65:3470–3478
Ricote M, Garcia-Tunon I, Bethencourt F et al (2006) The p38 transduction pathway in prostatic neoplasia. J Pathol 208:401–407
Zheng Q, Ye J, Wu H, Yu Q, Cao J (2014) Association between mitogen-activated protein kinase kinase kinase 1 polymorphisms and breast cancer susceptibility: a meta-analysis of 20 case-control studies. PLoS ONE 9:e90771
Acknowledgments
We greatly appreciate all the veterans and their family members who contributed their time and effort to join the Genetic Susceptibility, Environment and Prostate Cancer Risk (GSEP) study. Gratitude is expressed to our large list of collaborators and providers of tools to make this project successful; use of Case Western University’s Genetic Risk Easy Assessment Tool (GREAT) was provided by Dr. Louise Acheson; Oregon Clinical and Translational Research Institute’s (OCTRI) Biomedical Informatics Program was instrumental in tying all of our electronic questionnaires together into one HIPAA-compliant portal; VAPHCS phlebotomy staff helped us collect research specimens and allowing laboratory space for saliva collection; OCTRI’s Clinical and Translational Research Center (CTRC) Core Laboratory processed, analyzed, and stored subjects’ biological specimens; genotyping was conducted by iGenix in Seattle, Washington. Dr. Shannon’s current and previous research coordinators spent large amounts of time with our numerous in-person and over-the-phone participants in support of this study, assuring quality data collection as well as close, personal attention to our nation’s veterans and their family members choosing to join this study. We are also grateful to VAPHCS Urology Nurses and Operative Care staff for supporting coordinators’ recruitment of research participants.
Funding
Research reported in this publication was supported by the Veterans Affairs’ Biomedical Laboratory Research and Development Merit Review Award, VA Portland Health Care System (VAPHCS), and by the National Center for Advancing Translational Sciences of the National Institutes of Health under award number UL1TR000128. Clinical Trial Registration’s clinicaltrials.gov identifier: NCT01013129. This work was directly supported by the Veterans Affairs’ Biomedical Laboratory Research and Development Merit Review Award, and Oregon Health & Science University/Oregon State University Cancer Prevention and Control Initiative (2017-Horizon-Knight-11).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Zhang, Z., Jiang, D., Wang, C. et al. Polymorphisms in oxidative stress pathway genes and prostate cancer risk. Cancer Causes Control 30, 1365–1375 (2019). https://doi.org/10.1007/s10552-019-01242-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-019-01242-7