Abstract
Determining the etiologies of left ventricular hypertrophy (LVH) can be challenging due to the similarities of the different manifestations in clinical presentation and morphological features. Depending on the underlying cause, not only left ventricular mass but also left ventricular cavity size, or both, may increase. Patients with LVH remain asymptomatic for a few years, but disease progression will lead to the development of systolic or diastolic dysfunction and end-stage heart failure. As hypertrophied cardiac muscle disrupts normal conduction, LVH predisposes to arrhythmias. Distinguishing individuals with treatable causes of LVH is important for prevention of cardiovascular events and mortality. Athletic’s heart with physiological LVH does not require treatment. Frequent causes of hypertrophy include etiologies due to pressure/volume overload, such as systemic hypertension, hypertrophic cardiomyopathy, or infiltrative cardiac processes such as amyloidosis, Fabry disease, and sarcoidosis. Hypertension and aortic valve stenosis are the most common causes of LVH. Management of LVH involves lifestyle changes, medications, surgery, and implantable devices. In this review we systematically summarize treatments for the different patterns of cardiac hypertrophy and their impacts on outcomes while informing clinicians on advances in the treatment of LVH due to Fabry disease, cardiac amyloidosis, and hypertrophic cardiomyopathy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Left ventricular hypertrophy (LVH) is a common finding when there is an increase in left ventricular mass, either due to an increase in wall thickness or due to left ventricular cavity enlargement, or both, in response to a wide array of pathophysiological stressors. |
In this review, we summarize different etiologies of LVH and its complications, and outline the treatment and management options according to etiologies. We also describe the effect of therapy to reduce LVH and the impact on outcome. |
Pertinent studies and ongoing trials of certain drug treatments have been summarized according to LVH pathologies. |
Management of LVH involves lifestyle changes and medications, and may also include surgery and an implantable device for the prevention of sudden cardiac death depending upon the underlying cause. |
Introduction
Left ventricular hypertrophy (LVH) is a condition in which there is an increase in LV mass (LVM) secondary to an increase in wall thickness, an increase in LV cavity enlargement, or both. The left ventricle may undergo geometric changes in response to pathophysiological stressors such as long-term pressure or volume overload that increase the size of myocardial fibers [1,2,3,4]. LVH is recognized as an independent risk factor for premature cardiovascular morbidity and mortality, including chronic heart failure, cardiac arrhythmias, and sudden cardiac death.
Causes of LVH
Multiple comorbidities have been identified which can play an independent or synergistic role in the phenotype of the disease. The frequent causes of hypertrophy are listed in Table 1.
LVH is present in 15–20% of the general population, and the prevalence is similar in men and women. Hypertension and aortic valve stenosis are the most common causes of LVH, and in both of these conditions the heart is contracting against a pressure overload. Athletic’s heart with physiological LVH is a relatively benign condition in which intensive training results in increased LV muscle mass, wall thickness, and chamber size, but the systolic and diastolic functions remain normal [2].
Prognosis and pathophysiology of LVH
Prognostic associations with LVH include all-cause mortality, atrial fibrillation (AF), congestive heart failure, diastolic dysfunction, myocardial infarction (MI), reduced coronary flow reserve, stroke, sudden cardiac death, and ventricular ectopic activity [1]. In the normal healthy population the posterior wall is used preferentially to the septum to avoid the impact of abnormal septal geometry. Adverse LV remodeling includes concentric remodeling (increased relative wall thickness [RWT] without an increase in LVM, RWT = posterior wall thickness × 2/LV internal diameter at end-diastole), eccentric hypertrophy (increase in LV mass without increased RWT), and concentric hypertrophy (increase in LVM and increased RWT). Transition between any two types of abnormal LV geometry is possible [5]. Hypertension, has been variably associated with either eccentric or concentric LVH in different studies [1]. Diabetes mellitus (DM) causes concentric remodeling (CR), concentric LVH, and changes LV geometry [1]. In an analysis of 1950 patients in the HyperGEN study, even after adjusting for covariates such as body mass index (BMI), systolic blood pressure (SBP), age, and sex, there was still an increased likelihood of LVH in patients with DM [6]. Milani et al. [7] have suggested that concentric LVH was associated to the highest mortality, with less difference between CR and eccentric LVH (10.4, 8.7, and 8.4%, respectively). Another study showed a 40% increase in risk of cardiovascular disease (CVD) for every 39 g/m2 of increase in LVM. Despite this strong association with CVD risk, LVH is not routinely considered in risk stratification assessments [8]. A meta-analysis of 27,141 patients in ten studies showed an 11.1% risk of supraventricular tachycardia (including AF) in those with LVH versus 1.1% risk in those without (p < 0.001) [9]. In another study, the LVH–AF link was found to be strongest in those with eccentric and concentric LVH, less so in those with CR [10].
This article is based on previously conducted studies and does not contain any studies with human participants or animals performed by any of the authors.
Treatments
The association of LVH with increased cardiovascular morbidity and mortality demands aggressive treatment. However, the initial asymptomatic nature of LVH may lead to a delay in treatment. Treatment involves lifestyle changes (including weight reduction and exercise) and, depending upon the cause, may include medications, surgery, and implantable devices for the prevention of sudden cardiac death [1].
Treatment of LVH in Hypertension
Hypertension is a major modifiable risk factor for CVD morbidity and mortality. Lowering the blood pressure with antihypertensive agents decreases cardiac mass in patients with LVH, and weight loss or dietary sodium restriction have additional beneficial effects on the improvement in cardiac mass. Antihypertensive response and type of therapy influence the regression of LVH [11, 12]. A study with echocardiographic follow-up demonstrated that the reduction in LVH by echocardiography was also associated with a reduction in the composite endpoints of CV death, fatal or nonfatal MI, and fatal or nonfatal stroke (hazard ratio 0.78 per − 25 g/m2 in mass reduction, 95% confidence interval 0.65–0.94) [13]. Once the patient has received the appropriate treatment, regression of LVH continues gradually over time (≥ 3 years) and may be associated with complete reversal of LVH and other abnormalities induced by hypertension, such as left atrial enlargement and diastolic dysfunction. Numerous treatment strategies, ranging from thiazide diuretics, renin–angiotensin–aldosterone system (RAAS) inhibitors and calcium channel blockers (CCBs) to sodium-glucose cotransporter type-2 (SGLT2) inhibitors have been shown to regress LVH [14, 15]. Following the Framingham Heart Study, other trials in the early 2000s, such as the Multiple Risk-Factor Intervention Trial (MRFIT), the Heart Outcomes Prevention Evaluation (HOPE) trial, and the Losartan Intervention for Endpoint Reduction in Hypertension (LIFE) trial, confirmed the possibility of LV regression in response to anti-hypertension therapy and related CVD prognostic benefits. The HOPE trial showed that ramipril led to the regression or prevention of LVH and reduction of the risk of CVD mortality, MI, and stroke (12.3 vs. 15.8% for regression/prevention of LVH vs. development/persistence of LVH; p = 0.006) [14, 16,17,18]. The Systolic Blood Pressure Intervention Trial (SPRINT) showed that intensive (< 120 mmHg) SBP control was associated with a 46% lower risk of developing LVH diagnosed on electrocardiography (ECG-LVH) in participants without baseline LVH and 66% higher likelihood of regression/improvement of LVH in participants with baseline LVH [19]. In the LIFE study, LVH regression (diagnosed by ECG utilizing the Sokolow-Lyon index or the Cornell product criteria) in response to losartan improved clinical cardiovascular outcomes independent of blood pressure response [20]. This study randomized 9193 people with hypertension and LVH to either losartan or atenolol and followed them for a mean time of 4.8 ± 0.9 years. There was no difference in mean blood pressure at the end of the study, but the losartan group showed significant reductions in LVH criteria by ECG, as well as a lower composite endpoint of death, stroke, or MI. Those with LVH regression by ECG in the LIFE study had a 12% lower rate of new onset AF for every standard deviation reduction in Cornell ECG product and this corresponded to a decreased rate of stroke in the losartan arm, further solidifying the relationship between changes in LVM, AF, and stroke. Changes in LVH were also associated with improved parameters of diastolic function and with decreased recurrent hospitalizations for heart failure.
Apart from LIFE study, different angiotensin II receptor blockers (ARBs) have shown comparable benefit over beta adrenergic blockers. Losartan decreased LVH and improved renal outcomes in populations with DM and chronic kidney disease (CKD). CVD risk was also decreased similarly in patients without LVH. Starting early treatment while providing the appropriate target blood pressure prevents irreversible LVH [14, 18, 21,22,23,24,25]. In the Prospective Randomized Enalapril Study Evaluating Regression of Ventricular Enlargement (PRESERVE) trial, enalapril was compared to long-acting nifedipine among hypertensive participants with LVH (n = 202). Treatment with both medications led to a similar moderate degree of regression in LVM (26 g vs. 32 g; p = 0.36) (26). In a double blind randomized controlled trial (RCT), similar degrees of LVH regression were provided similarly with eplerenone and enalapril as monotherapies, and the combination of enalapril and eplerenone was found to be more effective in reducing LVM [27]. An ECG sub-study of the ADVANCE trial showed a reduction in LVM index by 2.7 g/m2 (95% CI − 5.0 to − 0.1; p = 0.04) and reduction in major adverse CVD events among those treated with the perindopril and thiazide combination [28]. “CHIP” diuretics (CHlorthalidone, Indapamide, and Potassium-sparing diuretic/hydrochlorothiazide) were compared with hydrochlorothiazide and found to be more effective in reducing LVM. A subsequent head-to-head systematic review involving 12 double-blind RCTs reported that “CHIP” diuretics were better than RAAS inhibitors for the reduction of LVM mass. Spironolactone was found to decrease LVM, and when studied against non-spironolactone therapy, the former improved diastolic parameters and reduced the risk of new-onset symptomatic congestive heart failure [29, 30]. In a meta-analysis of 80 trials and 3767 patients, all drug classes were assessed according to their effect on the LVM index. The results showed a significant reduction in LVM index of 13% with ARBs, 11% with CCBs, 10% with ACE inhibitors, 8% with diuretics, and 6% with β-blockers [31]. Fagard et al. [32] reported that β-blockers’ inferiority was more prominent than the superiority of ARBs. The mechanism behind the marked decrease in LVM by ARBs, angiotensin-converting enzyme (ACE) inhibitors, or CCBs might be explained by: (1) activation of RAAS that stimulates myocardial cells growth; (2) increase in plasma angiotensin II level which is independently associated with LVH; and (3) sympathetic nerve activity that is stimulated through N-type calcium channels. Hypertensive LVH is associated with almost threefold increased risk of ventricular tachycardia (VT)/ventricular fibrillation (VF). LVH increases the risk of sudden cardiac death (SCD). Although beta blockers are not the first choice in hypertensive patients with LVH due to their insufficient capacity to reverse LVH remodeling, it is important to prevent VT/VF in patients at high risk. Therefore, certain beta blockers (such as Bisoprolol) may be reevaluated for priority in guidelines [33, 34]. SGLT2 inhibitors are relatively novel antidiabetic agents with added benefits in terms of blood pressure and weight reduction. Their potential mechanisms of action include decrease LV wall stress secondary to diuresis and natriuresis. They also suppress sodium-hydrogen exchange in cardiomyocytes, which impacts on cardiac remodeling [34]. Schmieder et al. [35] reported that sacubitril/valsartan provided a more significant reduction in LVH compared to olmesartan, which might contribute to the superiority of sacubitril in terms of its favorable outcomes in a randomized trial of 114 patients over 52 weeks. Despite a modest decrease in SBP, but not diastolic blood pressure (DBP), in the sacubitril/valsartan arm, the authors found significant reductions in LVM index (− 6.83 vs. − 3.55 g/m2; p < 0.029). A meta-analysis of 20 studies revealed a significant regression in LVM with sacubitril/valsartan treatment compared to treatments with ACE inhibitors or ARBs among subjects with heart failure with reduced ejection fraction (EF) [36]. Regression of LVH by xanthine oxidase inhibitors (allopurinol) has been shown to be effective for the treatment of hypertrophy in animal studies by reducing oxidative tissue stress. A number of RCTs have shown that allopurinol was associated with a significant regression in LVH without a change in blood pressure in adult patients with coronary artery disease (CAD), CKD or DM [37]. It has also been shown that regular aerobic exercise improves blood pressure and reduces the risk of LVH development [38]. Regular exercise has been found to prevent the development of LVH in older individuals while endurance training causes increased LVM in young individuals [1].
Treatment of Risk Factors for LVH
In a recent study, 53,666 working age Korean men were evaluated according to their smoking status and LV geometry [39]. The authors found that exposure to tobacco use and intensity of smoking were associated with LVH in the working-age population. Abnormal geometry patterns were more prevalent in smokers than in non-smokers, suggesting that the adverse impact of smoking on LV structure begins at a relatively young age. These results provide meaningful implications when establishing policy on smoking cessation [39]. Herbal medications, such as licorice or ephedrine, may cause LVH, and the use of over-the-counter medications should also be questioned. The use of oral contraceptives, cardiac stimulants such as cocaine or amphetamines, as well as excess alcohol intake should be noted in patients’ history and drug cessation should be advised or treated [1, 6].
Obesity is a known risk factor for LVH. Lavie et al. [40] studied a very large population of 30,920 patients, including 11,792 patients with obesity (BMI ≥ 30). They found an increased incidence of abnormal LV geometry in obese patients indexed to body surface area, including increased CR (34 vs. 32%), eccentric LVH (7 vs. 6%), and concentric LVH (8 vs. 6%; p < 0.0001). Interestingly, overall mortality was lower in the obese compared with the non-obese population, but abnormal LV geometry still predicted increased mortality in both groups. A meta-analysis including 1066 patients undergoing bariatric surgery showed a standardized mean difference of − 0.46 in LVM index for individuals before and after bariatric surgery (p < 0.001). The authors also found a significant decrease in LVM, RWT, and left atrial diameter, with a corresponding improvement in diastolic dysfunction [41].
Treatment of LVH in Aortic Stenosis
Aortic stenosis is associated with LVH and diastolic dysfunction. Unfavorable LV remodeling occurs due to adaptive microscopic changes, such as progressive cardiomyocyte hypertrophy, extracellular matrix expansion, and interstitial fibrosis secondary to collagen deposition [42, 43].
Surgical aortic valve replacement (SAVR) has been associated with regression of LVH, improvement in LV pressure, mass-to-volume ratios, EF, and heart failure symptomatology. The LVM and LV volume indices are also improved with SAVR [44, 45]. Interest in the impact of transcatheter aortic valve replacement (TAVR) on LV reverse myocardial remodeling has also increased. Dahiya et al. [45] recently investigated the impact of TAVR among patients with preserved LV systolic function on regression of LVH, LV diastolic dysfunction and the correlation of each with heart failure-related quality of life (QoL). These authors also identified factors impacting the regression of LV hypertrophy post-TAVR. Among patients with moderate or severe LVH treated with TAVR who were alive at the 1-year follow-up, greater LVM index regression at 1 year was associated with lower death and hospitalization rates for up to 5 years. These findings may have implications for the timing of valve replacement and the role of adjunctive medical therapy after TAVR [46].
Risk factor management includes an abundance of data from previous studies, but is not within the scope of this review. Also, this subject would need a separate review article for thorough analysis. We only mention these risks and therapies because they represent some causes of LVH and therapies of underlying causes, respectively, and we wish to draw attention to the treatable causes of LVH.
Hypertrophic Cardiomyopathy
Hypertrophic cardiomyopathy (HCM) is a heterogeneous myocardial disease that is most often caused by autosomal dominant sarcomeric gene mutations. This disease is the most common monogenic cardiomyopathy in humans [47]. Altered levels of the sarcomere protein, calcium sensitivity, or ATPase activity result from a change in amino acid sequence in the sarcomere protein or a deficiency of a sarcomere protein, causing mitochondrial dysfunction and altered transcriptomics or signaling pathways. This ultimately results in myocyte hypertrophy, myocyte disarray, and fibrosis [48]. The phenotypic expression of HCM is manifested by LVH, myocardial hypercontractility, reduced compliance, myofibrillar disarray, and fibrosis. Differential diagnosis should be made from various metabolic and multiorgan syndromes, such as RASopathies (variants in several genes involved in RASMAPK signaling), mitochondrial myopathies, and glycogen/lysosomal storage diseases in children, and Fabry disease, amyloidosis, sarcoidosis, hemochromatosis, and Danon cardiomyopathy in adults [48, 49]. Patients with HCM have an increased incidence of both supraventricular and ventricular arrhythmias and are at an increased risk for SCD. Abnormalities of the mitral valve and subvalvular apparatus contribute to systolic anterior motion and LV outflow tract (LVOT) obstruction. Alterations in cardiac function and symptoms due these changes are given in Table 2.
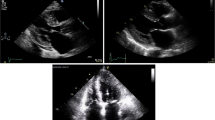
A resting or exercise-provoked LVOT gradient is present in 70% of patients with HCM. Therapies that directly target HCM pathophysiology are needed. Genetic testing should be offered to patients with HCM to elucidate the genetic basis and to allow for family screening. Genetic testing in an HCM proband should include testing for genes for which there is strong evidence to be disease-causing in HCM [49, 50]. Periodic re-evaluation is recommended with ECG, echocardiography (including global longitudinal strain), cardiac rhythm monitoring, cardiac magnetic resonance imaging (CMRI), and cardiopulmonary exercise testing (CPET), including asymptomatic patients [48, 51]. Five major approaches are available for the treatment of LVOT obstruction in patients with HCM: pharmacologic therapy, septal myectomy, alcohol septal ablation, non-alcohol septal ablation, dual chamber pacing. We have been using cyanoacrylate, and in recent years we have seen the emergence of novel pharmacotherapies, minimally-invasive procedures, and gene-directed approaches, all with the potential to fundamentally alter the therapeutic landscape. Myosin inhibitors are evolving as therapeutic targets for HCM. Surgical techniques continue to evolve and now address the mitral valve, including transcatheter mitral valve repair. Radiofrequency myocardial ablation and high-intensity focused ultrasound may offer alternatives for patients with obstructive HCM (gradient > 30 mmHg) [50, 52].
Pharmacotherapy
The pharmacological agents that are used in the the treatment HCM in different pathological conditions are given in Table 3 [47, 50, 53].
Management of atrial fibrillation in HCM
Atrial fibrillation in patients with HCM is often poorly tolerated; therefore, aggressive rhythm control strategies may be required. Rate control strategies, either with beta blockers, verapamil, or diltiazem, are recommended. Catheter ablation plays an important role in the management of AF and typical atrial flutter. However, the results of catheter ablation seem less favorable in this patient group compared with patients without HCM, with the former having a twofold higher risk of recurrence, more frequent need of repeated procedures, and higher use of concomitant antiarrhythmic drugs. In view of the lower success rate of catheter ablation in HCM compared with the general AF population, surgical AF ablation is a potential rhythm management option, especially in patients already undergoing open heart surgery for a surgical myectomy [54, 55]. New-onset and poorly tolerated AF is best treated with cardioversion. Since persistent and paroxysmal AF are risk factors for thromboembolism, long-term anticoagulation is necessary in clinical and subclinical AF (detected by an internal or external cardiac device) [50, 56]. Oral anticoagulation with direct oral anticoagulants as the first-line option and vitamin K antagonists as the second-line option should be considered the default treatment options independent of the CHA2DS2VASc score (Congestive Heart Failure, Hypertension, Age ≥75 [Doubled], Diabetes Mellitus, Prior Stroke or Transient Ischemic Attack [Doubled], Vascular Disease, Age 65–74, Female) [57].
Heart Failure Therapies and Device Therapy
In patients with HCM who develop systolic dysfunction with an LVEF < 50%, guideline-directed therapy for heart failure with reduced EF is recommended. Negative inotropic agents (specifically, verapamil, diltiazem, or disopyramide) may be discontinued. Heart failure symptoms in patients with HCM, in the absence of LVOT obstruction, should be treated similarly to other patients with heart failure symptoms, including the consideration of advanced treatment options (e.g., cardiac resynchronization therapy, LV assist device, transplantation). In patients with HCM, an ejection fraction < 50% is related with significantly impaired systolic function, poor prognosis, and increased risk for SCD. The risk of SCD ranges from 0.5 to 2% per year in adults with HCM, and HCM is the most common cause of SCD in adolescents [48, 50]. In individuals who are genotype-positive, phenotype-negative for HCM, an implantable cardioverter defibrillator (ICD) is not recommended for primary prevention. The patients who have survived a cardiac arrest (> 30 s or associated with hemodynamic compromise) due to ventricular fibrillation or sustained ventricular tachycardia are at high risk, and implantation of an ICD is strongly indicated for secondary prevention (50, 58).
The high-risk features for primary prevention are presented in Table 4. ICD implantation is typically considered in patients who have ≥ 1 of these primary risk factors (47, 50).
Either a single chamber transvenous ICD or a subcutaneous ICD is recommended after a shared decision-making discussion that takes into consideration patient preferences, lifestyle, and expected potential need for pacing for bradycardia or tachycardia termination. Single-coil ICD leads are recommended in preference to dual-coil leads. Dual-chamber ICDs are reasonable for patients with a need for atrial or atrioventricular sequential pacing for bradycardia/conduction abnormalities [50]. Antitachycardia pacing can minimize the risk of shocks. ICD placement for the sole purpose of participation in competitive athletics should not be performed [59, 60].
Apical myectomy may be considered by experienced surgeons at comprehensive centers in highly selected patients with apical HCM with severe dyspnea or despite maximal medical therapy, and with preserved EF and small LV cavity size [61,62,63,64,65]. Nonobstructive HCM patients with an EF < 50% should receive guideline-directed management and therapy (GDMT). After reevaluation for symptoms, if the patients have New York Heart Association (NYHA) class II to ambulatory class IV functional capacity, left bundle branch block (LBBB), and EF < 50%, cardiac resynchronization therapy (CRT) for symptom reduction is reasonable. Regardless of LVEF, if patients experience recurrent ventricular arrhythmias or severe (NYHA class III to class IV) symptoms despite optimization of medical therapy, and septal reduction therapy (SRT) is not an option, heart transplant evaluation is warranted, and cardiopulmonary exercise testing (CPET) plays a role in risk stratification. CPET should be performed to quantify the degree of functional limitation and aid decision-making regarding the selection of patients for heart transplantation or mechanical circulatory support. For patients with NYHA class III to class IV symptoms who are candidates for heart transplantation, continuous-flow LV assist device (LVAD) therapy is reasonable as a bridge to heart transplantation [50, 64,65,66,67,68].
Septal Reduction Therapy and Surgical Myectomy
In patients with obstructive HCM who remain severely symptomatic or having signs of cardiac decompensation despite GDMT, SRT is indicated in eligible patients and the procedure should be performed at experienced centers [50].
General eligibility criteria for septal reduction therapy:
- 1)
Clinical: Severe dyspnea or chest pain (usually NYHA functional class III or class IV), or occasionally other exertional symptoms (e.g., syncope, near syncope), when attributable to LVOT obstruction, that interferes with everyday activity or QoL despite optimal medical therapy.
- 2)
Hemodynamic: Dynamic LVOT gradient at rest or with physiological provocation with approximate peak gradient of ≥ 50 mmHg, associated with septal hypertrophy and systolic anterior motion (SAM) of mitral valve.
- 3)
Anatomic: Targeted anterior septal thickness sufficient to perform the procedure safely and effectively in the judgment of the individual operator.
Surgical myectomy at experienced centers is recommended if the patient has additional pathologies requiring surgery (e.g., associated anomalous papillary muscle, markedly elongated anterior mitral leaflet, intrinsic mitral valve disease, multivessel CAD, valvular aortic stenosis). Mitral valve replacement should not be performed for the sole purpose of relief of LVOT obstruction. Cardiac computed tomography is important in the localization of the appropriate target septal artery for alcohol septal ablation and to limit the area of myocardial necrosis [69,70,71,72]. In a recent study, a novel strategy, targeted septal branch microcirculatory embolization with tris-acryl gelatin microspheres, was found to be an efficient and safe approach to hypertrophic obstructive cardiomyopathy (HOCM) [73].
Treatment of Ventricular Arrhythmia
Antiarrhythmic drug therapies, including amiodarone, dofetilide, mexiletine, and sotalol, are recommended in symptomatic ventricular arrhythmias or recurrent ICD shocks despite beta blocker use, with the choice of agent guided by age, underlying comorbidities, severity of disease, patient preferences, and balance between efficacy and safety. In recurrent symptomatic sustained monomorphic ventricular arrhythmia, or recurrent ICD shocks despite optimal device programming, and in whom antiarrhythmic drug therapy is either ineffective, not tolerated, or not preferred, catheter ablation can be useful for reducing arrhythmia burden. In the case of poorly tolerated life-threatening ventricular tachyarrhythmias refractory to maximal antiarrhythmic drug therapy and ablation, heart transplantation assessment is indicated [74,75,76,77].
Comorbid Conditions
Comorbid conditions may worsen the severity of HCM. Prevention of atherosclerotic CVD is recommended to reduce risk of cardiovascular events. Counseling and comprehensive lifestyle interventions are recommended for achieving and maintaining weight loss and possibly lowering the risk of developing LVOT obstruction, heart failure, and AF in patients who are obese or overweight. Hypertension treatment should include beta blockers and non-dihydropyridine CCBs. Sleep disorders need to be diagnosed and treated. Low-dose diuretics may also be used as antihypertensive agents [50].
Pregnancy
Pregnancy in most women with HCM is well tolerated and maternal mortality is very low. Prenatal genetic counseling is helpful in explaining the risk of transmission of disease. In pregnant women with HCM, selected beta blockers may be prescribed for symptoms related to outflow tract obstruction or arrhythmias, under close monitorization of fetal growth. For pregnant women with HCM and AF or other indications for anticoagulation, low-molecular-weight heparin or vitamin K antagonists (at maximum therapeutic dose of < 5 mg daily) are recommended. Cardioversion for new or recurrent AF, particularly if symptomatic, is reasonable in pregnant patients. Vaginal delivery is recommended as the first-choice delivery option [50, 57].
Future Treatments
Recent developments in treatment include gene-based therapies. Embryonic gene editing has the potential to correct underlying genetic mutations that may result in disease. Most recent drug trials have failed; however, they have advanced our understanding of therapeutic targets, and myosin inhibitors are a promising therapeutic strategy. Novel procedures that target cardiac structural abnormalities include surgical papillary muscle realignment, chordae removal and mitral valve repair (transcatheter/surgical), apical myectomy, radiofrequency septal ablation, and high-intensity focused ultrasound septal ablation. Gene-based therapies include allele-specific gene silencing and embryonic gene repair using CRISPR/Cas 9 which target the genetic underpinnings of HCM [50, 52]. Novel pharmacotherapies and their mechanisms of action are shown in Table 5.
The open-label phase IIa trial of mavacamten (PIONEER-HCM; ClinicalTrials.gov Identifier: NCT02842242) included 21 patients with symptomatic obstructive HCM [78]. Cohort A received higher dose therapy (10, 15, or 20 mg daily); cohort B received lower dose therapy (2 or 5 mg daily). Post-exercise LVOT gradient and NT-proBNP (brain natriuretic peptide) levels were found to be reduced, and there was improvement in NYHA class. There was also a substantial (17%) improvement in exercise capacity (peak oxygen consumption (VO2): + 3.5 mL/kg/min). While improvements in LVOT obstruction (average approx. 25 mmHg decrease in post-exercise LVOT gradient) and exertional capacity were more modest, there was still significant symptomatic improvement. There was no significant effect on the end-diastolic pressure–volume relationship, which is a measure of LV stiffness, despite decreases in inotropic indices [78]. Mavacamten for the treatment of symptomatic obstructive hypertrophic cardiomyopathy (EXPLORER-HCM) is a randomized, double-blind, placebo-controlled, phase III trial. In this study treatment with mavacamten improved exercise capacity, LVOT obstruction, NYHA functional class, and health status in patients with obstructive HCM. Findings from these phase II and III trials suggest that mavacamten is a very promising new therapy that leads to an improvement in the symptomatic and physiological metrics for symptomatic patients with HCM with minimal adverse events [79]. A phase II study of Mavacamten in Adults with Symptomatic Non-Obstructive Hypertrophic Cardiomyopathy (MAVERICK-HCM) showed that treatment was associated with a significant reduction in NT-proBNP and cardiac troponin T (cTnI), suggesting improvement in myocardial wall stress [80]. In HCM mutation carriers, the phosphocreatine to ATP ratio is reduced, consistent with impaired high-energy phosphate metabolism. As a compensatory mechanism, there is increased carbohydrate utilization relative to fatty acids, akin to cardiomyocyte adaptation during ischemia. Perhexiline inhibits carnitine palmitoyltransferase I (CPT-1) and reduces fatty acid uptake into mitochondria, resulting in greater cellular dependence on carbohydrates for ATP production. ATP production is increased for the same O2 consumption and consequently increases myocardial efficiency [81]. The functional capacity increased in patients. While an early phase clinical study (METAL-HCM; NCT00500552) revealed favorable changes in the cardiac metabolome and improvement in exercise capacity compared to placebo, a more recent multicenter phase IIb clinical trial (NCT02862600) was terminated early due lack of efficacy and side effects [52, 82].
Hypertrophic cardiomyopathy is associated with enhanced late sodium current (INaL) activity due to enzyme-induced sodium channel phosphorylation. Dysregulated Ca2+ and Na+ handling may contribute to altered cardiomyocyte mechanics (hyper-contractility and impaired relaxation) and predispose the myocardium to arrhythmias. Ranolazine and eleclazine (both from Gilead Sciences, Foster City, CA, USA) are inhibitors of INaL, which could in theory have several benefits in HCM related to myocardial relaxation, ischemia, and arrhythmogenesis. A reduction in premature ventricular complex burden has been noted with ranolazine; however, studies (RESTYLE-HCM) failed to demonstrate a significant effect on objective measures, such as B-type natriuretic peptide and diastolic function. Additionally, the more potent INaL-inhibitor, eleclazine, was found to be ineffective in a large (n = 180) placebo-controlled trial (LIBERTY-HCM) [83, 84].
Several therapies have attempted to address fibrosis and disease progression in HCM. Although improvement in fibrosis were hypothesized with ARBs, aldosterone antagonists, N-acetyl cysteine, and statins, these molecules mostly failed to demonstrate beneficial effects in the studies. A phase II placebo-controlled trial of valsartan (VANISH; NCT01912534) is currently underway in HCM mutation carriers with asymptomatic or early/mild disease. Recently the introduction of sacubitril/valsartan and the sodium–glucose co-transporter 2 inhibitors (empagliflozin, dapagliflozin) found to be as effective therapies for patients with non-HCM-related systolic heart failure, and while exciting, their efficacy is yet to be established in HCM [85, 88].
Radiofrequency Ablation
Analogous to electrophysiologic procedures, radiofrequency (RF) energy is applied to the endocardial surface of the basal interventricular septum from a retrograde aortic or transseptal approach using electroanatomic or ECG guidance. More recently, percutaneous intramyocardial septal RF ablation was reported in a series of 15 patients with symptomatic obstructive HCM. This novel technique uses transthoracic ECG to guide transapical placement of an intraseptal RF electrode that delivers energy to the core of the hypertrophic segment. The authors reported an impressive septal reduction of 11 mm with resolution of obstruction (mean exercise LVOT gradient: 117–25 mmHg), improvements in NYHA class, and reduced serum NT-proBNP at 6 months [89,90,91].
Other Novel Therapies
High-intensity focused ultrasound (HIFU) uses ultrasound energy to create focal tissue lesions at a pre-determined depth from the ultrasound transducer. As it does not require direct contact with the target tissue, it is free from typical anatomic constraints. While there have been no human studies to date in HCM, HIFU has potential for achieving a completely non-surgical septal reduction in the future (92).
Allele-specific gene silencing and genome editing using CRISPR/Cas9 target the genetic underpinnings of hypertrophic cardiomyopathy. Current techniques including CRISPR/Cas9 cause a double-stranded DNA break at a desired genetic locus followed by intrinsic cellular repair. Germline editing is attractive for the treatment of monogenic diseases, as progeny of the treated embryo could prevent transmission of mutations to future generations [93, 94].
Fabry Disease and Left Ventricular Hypertrophy
Fabry disease, also called Anderson-Fabry disease, is the most prevalent lysosomal storage disorder. It is an X-linked inborn error of the glycosphingolipid metabolic pathway caused by mutations in the Galactosidase alpha (GLA) gene that leads to deficiency of the enzyme alpha-galactosidase A (α-Gal A). This results in accumulation of globotriaosylceramide (Gb3) within lysosomes in a wide variety of cells, causing variable manifestations of the disease [95]. Gb3 accumulation induces pathology via the release of pro-inflammatory cytokines and growth-promoting factors and by oxidative stress, resulting in myocardial extracellular matrix remodeling, LVH, vascular dysfunction, and interstitial fibrosis. Although the major accumulating molecule is Gb3, globotriaosylsphingosine(lyso-Gb3), digalactosylceramide (Gal2Cer), and blood group B and P1 antigens accumulate to a minor degree [96, 97]. Clinical presentation is variable and includes cutaneous, corneal, cardiac, renal, and neurologic manifestations. Cardiovascular manifestations of Fabry disease include LVH, aortic and mitral regurgitation, conduction defects, CAD, hypertension, and aortic root dilatation. In some cases of severe cardiac disease, the septum may appear asymmetrically hypertrophied because the basal posterior wall is thinned due to fibrosis. Many patients are asymptomatic, and a rare number of patients have advanced heart failure symptoms in the setting of unexplained LVH and generally normal LV ejection fraction. Intramural coronary arteries on endomyocardial biopsy reveal luminal narrowing due to hypertrophy and proliferation of smooth muscle and endothelial cells with glycosphingolipid deposits which may cause angina. Symptoms usually become evident in the third or fourth decade of life. Unexplained LVH is more common and more severe in males. While males are more severely diseased, most heterozygous females are also affected, although usually at a later age. Life expectancy is reduced by approximately 20 years in untreated males. Women are more likely to present with the cardiac variant of disease [98,99,100,101].
Management
The treatment of patients with Fabry disease primarily focuses upon replacing the missing or deficient enzyme (alpha-Gal A) with enzyme replacement therapy (ERT) as well as treating the various symptoms and disease complications. Two therapeutic modalities are available clinically for the treatment of Fabry disease: ERT and chaperone therapy. Migalastat hydrochloride is an oral pharmacologic chaperone that facilitates the trafficking of alpha-Gal A to lysosomes; as such, it is a therapeutic option for eligible individuals. The impact of these therapies on mortality is unknown. Other strategies, such as substrate reduction therapy, mRNA-based therapy, and gene therapy, are in development [102, 103]. Patients with Fabry disease with cardiac manifestations should generally receive standard therapies for heart disease, including antianginal medication for angina, standard antiarrhythmic therapy, and guideline-directed therapy for heart failure [104]. Although the impact on cardiovascular outcomes is not known, ERT should be initiated in patients with cardiac manifestations. Angina is frequent caused by small vessel disease; antianginal therapies are frequently needed. Evaluation with stress testing and coronary angiography is indicated in some patients to identify concurrent epicardial CAD [98]. Possible causes of sudden death in Fabry disease include ventricular arrhythmia and bradyarrhythmia. Some patients with advanced cardiomyopathy may require implantable ICD placement to prevent sudden cardiac death. Conduction abnormalities may be caused by glycolipid deposition in the atrioventricular node, His bundle, and bundle branches. Permanent pacemaker implantation is occasionally required to treat symptomatic bradycardia and/or advanced conduction system disease. Antiarrhythmic therapy may be needed for atrial and ventricular arrhythmias. Atrial arrhythmias, including AF, are more common and appear to be related to age. Management of hypertension is needed, and over one-half of the patients develop increases in blood pressure after the onset of CKD. Apart from patients receiving GDMT in heart failure, successful heart transplantation for advanced Fabry cardiac disease has been performed without development of Fabry disease in the graft, likely due to adequate enzyme activity in the graft. Fabry’s disease is not a contraindication for organ transplantation, even in patients presenting with both renal failure and heart failure [105,106,107,108]. Given the risk of development of ascending aortic aneurysm, patients with Fabry disease should be monitored for progressive ascending aortic dilatation [109].
Enzyme Replacement Therapy
As soon as the cardiac manifestations are detected, ERT should be initiated. The effect of ERT on cardiovascular outcomes has not been established. Two formulations of recombinant human alpha-Gal A are available: agalsidase alfa (ReplagalTM, Shire), produced in a genetically engineered human cell line, and agalsidase beta (FabrazymeTM, Genzyme), produced in a Chinese hamster ovary cell line [110]:
agalsidase alfa (ReplagalTM, Shire): 0.2 mg/kg as an intravenous infusion given over 40 min every 2 weeks;
agalsidase beta (FabrazymeTM, Genzyme): 1 mg/kg as an intravenous infusion over a mean of 2-2.5 h every 2 weeks.
A recent 5-year study of male patients aged 5–18 years supports the efficacy of agalsidase beta when delivered as a 1 mg/kg biweekly treatment rather than at a reduced dosage [111]. Clinical trials and observational studies suggest that ERT with agalsidase alpha or agalsidase beta can reduce tissue deposition of Gb3 in endothelial cells (including deposition in the heart) and reduce neuropathic pain, although the impact of ERT on other clinical manifestations of Fabry disease is less clear [112]. Early initiation of ERT in patients with cardiac involvement has been suggested since ERT may not improve segmental function where fibrosis (detected by CMRI) is already present. If the patient is a female carrier or an atypically affected male, ERT is recommended when clinical manifestations are present. However all classically affected males should receive migalastat regardless of clinical manifestations [113, 114]. If Fabry disease-related tissue pathology or clinical symptoms are absent, ERT may not be appropriate. These patients should be monitored regularly by a multidisciplinary care team [115].
Observational studies suggest that ERT can reduce LV wall thicknesses and/or LVM and improve myocardial function (e.g., systolic radial strain rate) but an impact on cardiovascular endpoints has not been established. A small randomized trial found that 4 months of recombinant human α-Gal A resulted in cardiac microvascular clearance of globotriaosylceramide accumulation in 72% of treated patients as compared with 3% of patients on placebo [112, 116]. Wiedemann et al. [113] suggested that treatment with recombinant α-Gal A should best be started before myocardial fibrosis has developed to achieve long-term improvement in myocardial morphology and function and exercise capacity. Data on the impact of ERT on changes in LVH are conflicting, with some studies showing a reduction in LVM and improved myocardial function as assessed by systolic radial strain rate, and others failing to show significant changes in ventricular wall thickness. ERT may cause infusion reactions and is not effective in all patients, such as those with end-stage organ disease or with antibodies to the recombinant enzyme [97, 117]. The Fabry Outcome Survey (FOS) reported that treatment with agalsidase alpha resulted in stability in the LVM index and mid-wall fractional shortening over a period of 5 years. Mehta et al. [118] also showed a sustained reduction in LVM index and a significant increase in mid-wall fractional shortening after 3 years of ERT in those patients with LVH at baseline evaluation. However, an observational study of 40 patients with Fabry disease suggested that long-term ERT may not be sufficient to alter the natural history of the disease [119]. In late-onset Fabry disease, ERT should be considered in the presence of laboratory, histological, or imaging evidence of injury to the heart, kidney, or central nervous system, even in the absence of typical Fabry symptoms [115].
Chaperone Therapy
Migalastat can now be used instead of ERT in patients with amenable genetic variants (present in 35–50% of patients) that allow for substantial increases in enzyme activity with this medication. The concept is that a ligand (i.e., molecular chaperone) of α-Gal A may occupy its active site, thereby promoting enzyme folding and stability. Once the α-Gal A-chaperone complex enters the lysosome, the chaperone is dissociated from the enzyme due to pH-sensitive conformational changes, releasing α-Gal A to act on glycosphingolipid substrates [102]. The presence of genetic variants should be determined before starting treatment to confirm that the GLA gene variant is associated with deficient α-Gal A leukocyte activity. The treatment is contraindicated when the glomerular filtration rate is estimated (eGFR) to be < 30 mL/min per 1.73 m2 [120]. Once it has been confirmed that the patient actually has an enzyme deficiency, the GLA gene variant that is likely to result in a substantial increase in enzyme level can be treated with migalastat. If these patients are already receiving treatment with ERT (α-Gal A or β-Gal), we typically switch them from ERT to migalastat. Migalastat is administered at a dose of 123 mg (equivalent to 150 mg of migalastat hydrochloride) orally once every other day [121]. In one double-blinded trial, 67 patients with Fabry disease who were not on ERT were randomly assigned to treatment with migalastat hydrochloride or placebo every other day for 6 months, followed by open-label migalastat for up to an additional 18 months. No patients progressed to end-stage kidney disease (ESKD), cardiac death, or stroke during the study, and the rate of adverse events was similar between groups. After a follow-up of 18–24 months in the open-label extension, there was a significant improvement in LVMI compared with baseline [121]. In another study, 57 adults were randomly assigned to receive 18 months of migalastat or to continue treatment with ERT. At 18 months, migalastat and ERT had comparable effects on kidney function, the LVM index had decreased from baseline in patients on migalastat but not changed significantly in those on ERT, and there was no significant difference in the rate of kidney, cardiac, or cerebrovascular events or treatment-related adverse events between the two groups [122]. Patients who are started on ERT or migalastat should have a clinical evaluation, routine laboratory tests, and complete blood count every 6 to 12 months. Estimation of the GFR and determination of the urine protein-to-creatinine ratio every 3 to 6 months are needed. Patients with cardiac involvement should have an electrocardiogram every 6 to 12 months [123]. Recent studies show that chaperone therapy coupled with ERT is more efficacious than either option as monotherapy [124]. Pegunigalsidase-a is a novel pegylated form of α-Gal A produced in a ProCellEx system (Protalix Biotherapeutics, Carmiel, Israel) with an increased heart and kidney uptake compared with current ERTs. ERT and migalastat are not recommended in persons with well-characterized benign α-Gal A variants [115].
Substrate reduction therapy (SRT) is gaining interest as an alternate approach to reducing the levels of metabolites that accumulate in Fabry disease by decreasing the synthesis of relevant precursor glycosphingolipids. In patients with residual enzyme activity, SRT might be sufficient to reduce the production of the substrate to a level compatible with the remaining enzyme activity. Glucosylceramide synthase (GCS) inhibition results in decreased Gb3 synthesis [125]. Glucosylceramide synthase inhibitors have been tested in the preclinical setting in Fabry cell and mouse models and in clinical trials for patients with Gaucher disease (glucosylceramidase deficiency). SRT that specifically targets Gb3 synthesis and avoids depletion of lactosylceramide may be a better option in these patients. Novel SRT molecules have been developed and tested for Fabry disease, such as the ceramide-based Venglustat (Sanofi Genzyme, Sanofi S.A., Paris, France) and the galactose derivative lucerastat (Idorsia Pharmaceuticals, Allschwil, Switzerland); both molecules inhibit GCS. Combining different approaches, such as ERT with SRT, might be beneficial, but the high costs of the individual therapies currently form an important barrier to the implementation of this approach [115, 126].
Gene therapy will likely be a future therapeutic option. This therapy has the potential to systemically express α-Gal A in a manner that would be effective for the large number of genetic mutations that cause Fabry disease. Adeno-associated virus capsids are also being evaluated for gene therapy, and novel capsids are in development to improve α-Gal A expression in kidney, heart, and brain. m-RNA-based therapy is an attractive option because the translated α-Gal A would express native post-translational modification [127]. The first in-human study of gene therapy via autologous stem cell transplantation using cells transduced via a lentivirus vector containing the ‘wild-type’ allele of the GLA gene is currently underway [97].
Cardiac Amyloidosis
Amyloidosis is a family of diseases in which misfolded precursor proteins aggregate to form amyloid which is then deposited in body tissues. Proteins fold inappropriately for several reasons. Some proteins have an inherent propensity to misfold and deposit in body tissues when present in high concentrations or when the patient ages (as is the case with transthyretin), while others misfold due to an alteration in the encoding genes of the protein. Abnormal proteolytic remodeling causing a conformational change to the precursor protein may make it more likely to fold inappropriately. In cardiac amyloidosis, amyloid is deposited in the extracellular space of the myocardium, resulting in thickening and stiffening of ventricular walls, with resultant heart failure and conductive dysfunction [128,129,130]. The most pertinent forms of the disease in the setting of cardiac amyloidosis are transthyretin amyloidosis (ATTR) and immunoglobulin-derived light-chain amyloidosis (AL). It is uncommon for secondary (AA) amyloidosis to affect the heart, and this is rarely seen in developed countries where severe chronic inflammatory processes are generally well managed [131, 132]. A high index of suspicion is essential in the early diagnosis and for improvement of the prognosis of these patients. Cardiac complications include heart failure, AF, ventricular arrhythmias, conduction disorders, thromboembolism, aortic stenosis, and treatment should be given according to the underlying pathology.
Immunoglobulin-Derived Amyloid Light-Chain Amyloidosis
The precursor protein of amyloid light-chain amyloidosis (AL amyloidosis) is a monoclonal light chain. The disease is mostly seen in males (> 60%) aged > 50 years. The underlying disorder is plasma cell dyscrasia. AL amyloidosis almost invariably involves the cardiovascular system, with approximately 90% of cases involving the heart. Amyloid deposits in AL amyloidosis have been described to have cytotoxic effects which directly cause cell death of cardiomyocytes. Vascular involvement is common and heart failure is more severe. Other cardiac pathologies can be manifested, such as right-sided heart failure with preserved EF, valve pathologies, atrial/ventricular arrhythmias, or bradyarrhythmia; severe hypotension with ACE inhibitor use is not rare. There may be multiorgan involvement, involving nephrotic syndrome, hepatomegaly/ splenomegaly, periorbital bruising (“panda eyes”), macroglossia, nail dystrophy, submandibular gland enlargement, peripheral polyneuropathy, autonomic neuropathy, and carpal tunnel syndrome, which may be seen as extracardiac manifestations [132].
Treatment
There is no disease-specific therapy and cardiac involvement in AL amyloidosis. Compared to patients with ATTR amyloidosis, those with AL amyloidosis have lower median survival rates from the onset of symptoms (1.7 vs. 6.1 years). The treatment regimens used are similar to those used for multiple myeloma. The choice of therapy is based on dedicated risk stratification and includes criteria such as age, Karnofsky index, number of organs involved, and extent of organ involvement. The primary goal includes preventing disease progression by stopping the production of light chains and inhibiting amyloid fibril formation. The degree of cardiac involvement often limits the choice of chemotherapy [133]. Chemotherapy can incluce steroids (dexamethasone, prednisolone), alkylators (melphalan, cyclophosphamide), proteasome inhibitors (bortezomib, carfilzomib), immunomodulators (lenalidomide, pomalidomide), anti-CD38 antibody (daratumumab), and an anti-SLAMF7 antibody (elotuzumab) [134,135,136].
The drugs have potential side effects, including cardiac decompensation (steroids, carfilzomib) or thrombotic events (lenalidomide and pomalidomide). Chemotherapy using cyclophosphamide, bortezomib, and dexamethasone (CyBorD) is the current standard of care for patients with AL amyloidosis. The ANDROMEDA study effectively demonstrated that CyBorD coupled with daratumumab works effectively to produce responses in patients with AL amyloidosis. The overall organ response rate, including cardiac, kidney and liver, was 64% at 17.3 months. Several promising agents are being tested. Birtamimab (NEODOO1) is an antibody which neutralizes circulating and deposited amyloid. The phase III trial was prematurely discontinued because of a lack of efficacy; however, a post hoc analysis showed that NEODOO1 reduced all-cause mortality in those patients at the highest risk for early mortality. Another potential agent is the green tea polyphenol epigallocatechin-3-gallate (EGCG) [134, 137, 138]. Loop-diuretics and mineralocorticoid receptor antagonists can be beneficial in specific doses, avoiding doses that would decrease preload. There is no evidence for standard heart failure therapies. Sometimes beta blockers can lead to significant hemodynamic deterioration as patients with cardiac amyloidosis (CA) can increase their cardiac output only via the heart rate. Many CA patients develop AF/atrial flutter, which often makes heart rate control necessary. Digitalis derivatives bind to amyloid fibers and cause locally toxic levels. When digitalis derivatives are needed, close monitoring of serum levels and side effects are of utmost important [134]. As a non-drug therapy option, heart transplantation may be considered in selected cases to enable patients to receive high-dose chemotherapy and autologous stem cell transplant afterwards. A complete hematological response is needed in order to avoid recurrence of AL amyloidosis/CA in the transplanted organ so cardiac transplantation as a therapeutic option should be discussed and evaluated [128, 139].
Transthyretin Amyloidosis and Treatment
Transthyretin amyloidosis is a condition in which transthyretin, a physiological protein primarily synthesized by the liver, misfolds into insoluble B-pleated sheets and deposits as amyloid in the extracellular space of the myocardium. The disease may be cardiac-predominant, neuropathy-predominant, or mixed, and usually appears in males aged > 50 years. Deposition of misfolded transthyretin either as the wild-type (ATTRwt) form or mutated/variant (ATTRv) form causes ATTR. In cardiac ATTR, amyloid deposits primarily cause myocardial stiffness and impaired function by affecting myocardial relaxation; in later stages there can be a decline in contractility [131, 140]. ATTR tends to present as heart failure with preserved EF (HFpEF) with signs of right-sided heart failure. The cardiovascular presentation of hereditary ATTR (hATTR) varies according to the causative genetic mutation. The two best well-documented mutations leading to cardiomyopathy are Val122Ile and Thr60Ala. Those persons with the Val30Met transthyretin mutation commonly have conduction issues requiring pacemaker placement, while other variants, such as Val122Ile and Thr60Ala (T60A), commonly affect the cardiovascular system, but do not primarily affect the conduction system. ATTRwt was formerly called senile systemic amyloidosis (non-hereditary ATTR). In comparison to ATTRwt, those with the Val122Ile mutation have a worse NYHA functional class with a lower QoL. Overall survival between these two forms of ATTR are similar. Rhythm disturbances (typically AF) are more frequent in ATTRwt than in hATTR. A useful flag for suspecting ATTR is hypertension that resolves over time and an intolerance of ARBs, ACE inhibitors, or beta blockers. In ATTRwt, carpal tunnel syndrome, lumbar spinal stenosis, and isolated cardiomyopathy may occur. Subjects with ATTR usually have more severe LV thickening than those with AL amyloidosis [131, 141, 142].
The basic policies for CA management are to deal with symptomatic complaints based on HF, together with the consideration of two therapeutic possibilities: general HF pharmacotherapy and causal treatment for CA. Low cardiac output can be easily seen through the restrictive compromise in CA. Correct titration of diuretics is the primary treatment in heart failure. ACE inhibitors and ARBs promote hypotension due to autonomic dysfunction and can only be tolerated in low doses in patients with cardiac amyloidosis. There are limited data with sacubitril/valsartan therapy. Also, digitalis and calcium channel blockers should be used with caution. Intravascular volume depletion may cause hypotension in cases of restrictive hemodynamics, leading to diuretic resistance. Inotropic drugs such as catecholamines and phosphodiesterase inhibitors are used for the treatment of low perfusion. Especially in patients in sinus rhythm, one must be careful not to reduce the heart rate excessively, because an increased heart rate has a compensatory role in a restrictive heart with low stroke volume. Cardiac conduction disorders can be managed by using a pacemaker or an ICD. For AL amyloidosis a heart transplant is recommended while in ATTR, both a heart and liver transplant are needed (143, 144).
Transthyretin Amyloidosis
Transthyretin amyloidosis-modifying therapies and their mechanism of action, indications for use in treatment, and their availability in current treatment modalities are given in Table 6 [138, 145]. Tafamidis for treatment of amyloid cardiomyopathy based on the data from the recently published phase III clinical trial (ATTR-ACT) was approved by the European Medicines Agency (EMA). The safety and efficacy of tafamidis has been evaluated (20 mg and 80 mg dosages) and compared with placebo in patients with amyloid cardiomyopathy. Compared to the placebo group, a significant reduction in mortality was observed in all subgroups. Hospitalizations due to cardiac decompensation were reduced. Also, there was an improvement in 6-min walking test and on the QoL as assessed in the Kansas City Cardiomyopathy Questionnaire (KCCQ-OS). Tafamidis was found to be effective for inhibiting disease progression in patients with ATTR whose functional capacity were NYHA I or II [128, 143, 146]. The approved dosage for treatment of amyloid cardiomyopathy is tafamidis 61 mg, the bioequivalent of 80 mg tafamidis-meglumine. Serious side effects did not occur. The effects of tafamidis are expected in patients with ATTR in the early stage, so it should be started before the patient shows obvious symptoms. Therefore, it is important to diagnose ATTR at an earlier stage using specific cardiac echocardiographic findings. Tafamidis does not seem to improve the pathology of ATTR.
In terms of echocardiographic findings as prognostic predictors in patients with ATTR, LVEF was the most reported finding. Grogan et al. [147] reported that LVEF < 50% was an independent prognostic predictor in patients with ATTRwt CA. Myocardial contraction fraction (MCF), which is the ratio of LVM to LV stroke volume, as well as LVEF should be considered as prognostic predictors for patients with amyloidosis. Moreover, some studies have reported that tricuspid annular plane systolic excursion (TAPSE) and mitral annular plane systolic excursion (MAPSE) are more useful prognostic predictors than LVEF, MCF, and LV global strain. Apical sparing is observed both in patients with ATTR and those with AL amyloidosis. The strain value at the LV apex in patients with ATTR has been shown to be lower than that in patients with AL amyloidosis [143, 148, 149]. Two transthyretin (TTR) messenger RNA (mRNA)interfering drugs, the RNA interference (RNAi) drug patisiran (Onpattro®; Alnylam Pharmaceuticals, Inc., Cambridge, MA, USA), and the antisense oligonucleotide inotersen (Tegsedi®; Ionis Pharmaceuticals, Carlsbad, CA, USA) have been approved in Europe. Patisiran showed a significant reduction of LV wall thickness and NT-proBNP levels in a subgroup of ATTRv patients. Patisiran is applied intravenously every 3 weeks. There is lack of long-term evidence for its efficacy and safety [128, 138, 150,151,152].
AA Amyloidosis and Treatment
Cardiovascular manifestations of secondary amyloidosis include severe ventricular wall thickening with resultant motion abnormalities. Patients with secondary amyloidosis, which is caused by inflammatory disorders (rheumatoid arthritis, juvenile idiopathic arthritis), are less likely to have cardiac involvement than those with other forms of the disease. AA amyloidosis is caused by the deposition of AA fibrils, which are formed from a fragment of the serum amyloid A (SAA) protein in the context of long-lasting inflammatory states. Since AA amyloidosis primarily affects the kidneys, it usually manifests as renal insufficiency, often with proteinuria. Heart involvement is rather rare (< 10%), and there seems to be a genetic predisposition. Important causes of AA amyloidosis are uncontrolled chronic inflammatory rheumatic diseases (e.g., rheumatoid arthritis), chronic inflammatory bowel diseases (ulcerative colitis, Crohn’s disease), chronic infections (e.g., tuberculosis), and hereditary autoinflammatory diseases (e.g., familial Mediterranean fever). There is no specific drug therapy for heart involvement. The main treatment goals are improving underlying disease and preventing the synthesis of the precursor protein SAA. Depending on the underlying disease, various drugs are used, such as anti-infectives for infectious disease, anti-inflammatory drugs, immunosuppressants for autoimmune diseases, and chemotherapy for malignant diseases [153, 154].
Conclusion
Left ventricular hypertrophy increases cardiovascular morbidity and mortality. The asymptomatic nature of LVH may lead to delayed treatment. Creating awareness about LVH and searching for underlying etiologies facilitates initiation of early treatment.
References
Stewart MH, Lavie CJ, Shah S, et al. Prognostic implications of left ventricular hypertrophy. Prog Cardiovasc Dis. 2018;61(5–6):446–55. https://doi.org/10.1016/j.pcad.2018.11.002.
Cuspidi C, Sala C, Negri F, et al. Italian society of hypertension. Prevalence of left-ventricular hypertrophy in hypertension: an updated review of echocardiographic studies. J Hum Hypertens. 2012;26(6):343–9.
Phyllis AR, Stanley P. Brown pathological versus physiological left ventricular hypertrophy: a review. J Sports Sci. 1998;16(2):129–41. https://doi.org/10.1080/026404198366849.
Schillaci G, Battista F, Pucci G. A review of the role of electrocardiography in the diagnosis of left ventricular hypertrophy in hypertension. J Electrocardiol. 2012;45(6):617–23. https://doi.org/10.1016/j.jelectrocard.2012.08.051.
Lieb W, Gona P, Larson MG, et al. The natural history of left ventricular geometry in the community: clinical correlates and prognostic significance of change in LV geometric pattern. JACC Cardiovasc Imaging. 2014;7(9):870–8. https://doi.org/10.1016/j.jcmg.2014.05.008.
Palmieri V, Bella JN, Arnett DK, et al. Effect of type 2 diabetes mellitus on left ventricular geometry and systolic function in hypertensive subjects: Hypertension Genetic Epidemiology Network (HyperGEN) study. Circulation. 2001;103(1):102–7. https://doi.org/10.1161/01.cir.103.1.102.
Milani RV, Lavie CJ, Mehra MR, Ventura HO, Kurtz JD, Messerli FH. Left ventricular geometry and survival in patients with normal left ventricular ejection fraction. Am J Cardiol. 2006;97(7):959–63. https://doi.org/10.1016/j.amjcard.2005.10.030.
Verdecchia P, Carini G, Circo A, et al. Left ventricular mass and cardiovascular morbidity in essential hypertension: the MAVI study. J Am Coll Cardiol. 2001;38(7):1829–35. https://doi.org/10.1016/S0735-1097(01)01663-1.
Chatterjee S, Bavishi C, Sardar P, et al. Meta-analysis of left ventricular hypertrophy and sustained arrhythmias. Am J Cardiol. 2014;114(7):1049–52.
Seko Y, Kato T, Haruna T, et al. Association between atrial fibrillation, atrial enlargement, and left ventricular geometric remodeling. Sci Rep. 2018;8(1):6366. https://doi.org/10.1038/s41598-018-24875-1.101.
Rapsomaniki E, Timmis A, George J, et al. Blood pressure and incidence of twelve cardiovascular diseases: lifetime risks, health Life-years lost, and age specific associations in 1·25 million people. Lancet. 2014;383(9932):1899-911. https://doi.org/10.1016/S0140-6736(14)60685-1.
Ruilope LM, Schmieder RE. Left ventricular hypertrophy and clinical outcomes in hypertensive patients. Am J Hypertens. 2008;21:500.
Devereux RB, Wachtell K, Gerdts E, et al. Prognostic significance of left ventricular mass change during treatment of hypertension. JAMA. 2004, pp. 2350–2356.
Devereux RB, Kjeldsen SE, Julius S, et al. Cardiovascular morbidity and mortality in the losartan intervention for endpoint reduction in hypertension study (LIFE): a randomized trial against atenolol. Lancet. 2002;359(9311):995–1003.
Verma S, Garg A, Yan AT, et al. Effect of Empagliflozin on left ventricular mass and diastolic function in individuals with diabetes: an important clue to the EMPAREG OUTCOME trial? Diabetes Care. 2016;39(12):e212–3. https://doi.org/10.2337/dc16-1312.
Mathew J, Sleight P, Lonn E, et al. Reduction of cardiovascular risk by regression of electrocardiographic markers of left ventricular hypertrophy by the angiotensin converting enzyme inhibitor ramipril. Circulation. 2001;104(14):1615–21.
Prineas RJ, Rautaharju PM, Grandits J, Crow R, et al. Independent risk for cardiovascular disease predicted by modified continuous score electrocardiographic criteria for 6-year incidence and regression of left ventricular hypertrophy among clinically disease-free men: 16-year follow-up for the multiple. J Electrocardiol. 2001;34(2):91–101.
Yildiz M, Oktay AA, Stewart MH, et al. Left ventricular hypertrophy and hypertension. Prog Cardiovasc Dis. 2020;63(1):10–21. https://doi.org/10.1016/j.pcad.2019.11.009.
Soliman EZ, Ambrosius WT, Cushman WC, et al. Effect of intensive blood pressure lowering on left ventricular hypertrophy in patients with hypertension. Circulation. 2017;136(5):440–50. https://doi.org/10.1161/CIRCULATIONAHA.117.028441.
Okin PM, Wachtell K, Devereux RB, et al. Regression of electrocardiographic left ventricular hypertrophy and decreased incidence of new-onset atrial fibrillation in patients with hypertension. JAMA. 2006;296(10):1242. https://doi.org/10.1001/jama.296.10.1242.
Wachtell K, Lehto M, Gerdts E, et al. Angiotensin II receptor blockade reduces new onset atrial fibrillation and subsequent stroke compared to atenolol: the losartan intervention for end point reduction in hypertension (LIFE) study. J Am Coll Cardiol. 2005;45(5):712–9. https://doi.org/10.1016/j.jacc.2004.10.068.
Wachtell K, Bella JN, Rokkedal J, et al. Change in diastolic left ventricular filling after one year of antihypertensive treatment: the losartan intervention for endpoint reduction in hypertension (LIFE) study. Circulation. 2002;105(9):1071–6.
Moroni C, Tolone S, Lopreiato F, et al. Effects of losartan on left ventricular mass: a three-year follow-up in elderly hypertensives with myocardial hypertrophy despite successful conventional antihypertensive treatment. Eur Rev Med Pharmacol Sci 2017;21(6):1323–8. http://www.ncbi.nlm.nih.gov/pubmed/28387895
Galzerano D, Tammaro P, Del Viscovo L, et al. Three-dimensional echocardiographic and magnetic resonance assessment of the effect of telmisartan compared with carvedilol on left ventricular mass: a multicenter, randomized, longitudinal study. Am J Hypertens. 2005;18(12):1563–9. https://doi.org/10.1016/j.amjhyper.2005.06.011.
Boner G, Cooper ME, McCarroll K, et al. Adverse effects of left ventricular hypertrophy in the reduction of endpoints in NIDDM with the angiotensin II antagonist losartan (RENAAL) study. Diabetologia. 2005. https://doi.org/10.1007/s00125-005-1893-1.
Devereux RB, Palmieri V, Sharpe N, et al. Effects of once-daily angiotensin converting enzyme inhibition and calcium channel blockade-based antihypertensive treatment regimens on left ventricular hypertrophy and diastolic filling in hypertension. Circulation. 2007;104(11):1248–54. https://doi.org/10.1161/hc3601.095927.
Pitt B, Reichek N, Willenbrock R, et al. Effects of eplerenone, enalapril, and eplerenone/enalapril in patients with essential hypertension and left ventricular hypertrophy: the 4E-left ventricular hypertrophy study. Circulation. 2003;108(15):1831–8. https://doi.org/10.1161/01.CIR.0000091405.00772.6E.
ADVANCE Echocardiography Substudy Investigators, ADVANCE Collaborative Group. Effects of perindopril-indapamide on left ventricular diastolic function and mass in patients with type 2 diabetes: the ADVANCE Echocardiography Substudy. J Hypertens. 2011;29(7):1439–47. https://doi.org/10.1097/HJH.0b013e3283480fe9.
Roush GC, Abdelfattah R, Song S, et al. Hydrochlorothiazide and alternative diuretics versus renin-angiotensin system inhibitors for the regression of left ventricular hypertrophy: a head-to-head meta-analysis. J Hypertens. 2018;36(6):1247–55.
Gu J, Fan YQ, Han ZH, et al. Association between long-term prescription of aldosterone antagonist and the progression of heart failure with preserved ejection fraction in hypertensive patients. Int J Cardiol. 2016;220(2016):56–60. https://doi.org/10.1016/j.ijcard.2016.06.190.
Klingbeil AU, Schneider M, Martus P, Messerli FH, Schmieder RE. A meta-analysis of the effects of treatment on left ventricular mass in essential hypertension. Am J Med. 2003;115(1):41–6. https://doi.org/10.1016/S0002-9343(03)00158-X.
Fagard RH, Celis H, Thijs L, et al. Regression of left ventricular mass by antihypertensive treatment: a meta-analysis of randomized comparative studies. Hypertension. 2009;54(5):1084–91. https://doi.org/10.1161/HYPERTENSIONAHA.109.136655.
Koracevic G, Stojanovic M, Lovic D, Zdravkovic M, Sakac D. Certain beta blockers (e.g., bisoprolol) may be reevaluated in hypertension guidelines for patients with left ventricular hypertrophy to diminish the ventricular arrhythmic risk. J Hum Hypertens. 2021. https://doi.org/10.1038/s41371-021-00505-8.
Brown AJM, Lang C, McCrimmon R, Struthers A. Does dapagliflozin regress left ventricular hypertrophy in patients with type 2 diabetes? A prospective, double-blind, randomised, placebo-controlled study. BMC Cardiovasc Disord. 2017;17(1):229. https://doi.org/10.1186/s12872-017-0663-6.
Schmieder RE, Wagner F, Mayr M, et al. The effect of sacubitril/valsartan compared to olmesartan on cardiovascular remodelling in subjects with essential hypertension: the results of a randomized, double-blind, active-controlled study. Eur Heart J. 2017;38(44):3308–17. https://doi.org/10.1093/eurheartj/ehx525.
Wang Y, Zhou R, Lu C, Chen Q, Xu T, Li D. Effects of the angiotensin-receptor neprilysin inhibitor on cardiac reverse remodeling: meta-analysis. J Am Heart Assoc. 2019;8(13):e12272. https://doi.org/10.1161/JAHA.119.012272.
Rekhraj S, Gandy SJ, Szwejkowski BR, et al. High-dose allopurinol reduces left ventricular mass in patients with ischemic heart disease. J Am Coll Cardiol. 2013;61(9):926–32. https://doi.org/10.1016/j.jacc.2012.09.066.
Palatini P, Visentin P, Dorigatti F, et al. Regular physical activity prevents development of left ventricular hypertrophy in hypertension. Eur Heart J. 2009;30(2):225–32.
Park SK, Ryoo JH, Kang JG, Jung JY. Smoking status, intensity of smoking and their relation to left ventricular hypertrophy in working aged Korean men. Nicotine Tob Res. 2021;23(7):1176–1182. https://doi.org/10.1093/ntr/ntab020.
Lavie CJ, Milani RV, Ventura HO, et al. Disparate effects of left ventricular geometry and obesity on mortality in patients with preserved left ventricular ejection fraction. Am J Cardiol. 2007;100(9):1460–4. https://doi.org/10.1016/j.amjcard.2007.06.040.
Cuspidi C, Rescaldani M, Tadic M, et al. Effects of bariatric surgery on cardiac structure and function: a systematic review and meta-analysis. Am J Hypertens. 2014;27(2):146–56. https://doi.org/10.1093/ajh/hpt215.
Azevedo CF, Nigri M, Higuchi ML, et al. Prognostic significance of myocardial fibrosis quantification by histopathology magnetic resonance imaging in patients with severe aortic valve disease. J Am Coll Cardiol. 2010;56(4):278–87.
Villari B, Hess OM, Kaufmann P, et al. Effect of aortic valve stenosis (pressure overload) and regurgitation (volume overload) on left ventricular systolic and diastolic function. Am J Cardiol. 1992;69(9):927–34.
Bech-Hanssen O, Caidahl K, Wall B, et al. Influence of aortic valve replacement, prosthesis type, and size on functional outcome and ventricular mass in patients with aortic stenosis. J Thorac Cardiovasc Surg. 1999;118(1):57–65.
Dahiya G, Kyvernitakis A, Joshi AA, et al. Impact of transcatheter aortic valve replacement on left ventricular hypertrophy, diastolic dysfunction and quality of life in patients with preserved left ventricular function. Int J Cardiovasc Imaging. 2021;37:485–92. https://doi.org/10.1007/s10554-020-02015-z.
Chau KH, Douglas PS, Pibarot P, et al. Regression of left ventricular mass after transcatheter aortic valve replacement: the PARTNER trials and registries. J Am Coll Cardiol. 2020;75(19):2446–58. https://doi.org/10.1016/j.jacc.2020.03.042.
Maron BJ. Clinical course and management of hypertrophic cardiomyopathy. N Engl J Med. 2018;379:655–68.
Marian AJ, Braunwald E. Hypertrophic cardiomyopathy: genetics, pathogenesis, clinical manifestations, diagnosis, and therapy. Circ Res. 2017;121(7):749–70. https://doi.org/10.1161/CIRCRESAHA.117.311059.
Spudich JA. Three perspectives on the molecular basis of hypercontractility caused by hypertrophic cardiomyopathy mutations. Pflugers Arch. 2019;471:701–17.
Ommen SR, Mital S, Burke MA, et al. 2020 AHA/ACC guideline for the diagnosis and treatment of patientshyper with hypertrophic cardiomyopathy: executive summary: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2020;142(25):e533–57. https://doi.org/10.1161/CIR.0000000000000938).
Force T, Bonow RO, Houser SR, et al. Research priorities in hypertrophic cardiomyopathy: report of a working group of the National Heart, Lung, and Blood Institute. Circulation. 2010;122:1130–3.
Tuohy CV, Kaul S, Song HK, Nazer B, Heitner SB. Hypertrophic cardiomyopathy: the future of treatment. Eur J Heart Fail. 2020;22(2):228–40. https://doi.org/10.1002/ejhf.1715.
Kirk CR, Gibbs JL, Thomas R, et al. Cardiovascular collapse after verapamil in supraventricular tachycardia. Arch Cardiovasc Dis. 1987;62:1265–6.
Zhao D-S, Shen Y, Zhang Q, et al. Outcomes of catheter ablation of atrial fibrillation in patients with hypertrophic cardiomyopathy: a systematic review and meta-analysis. Europace. 2016;18:508–20.
Providência R, Elliott P, Patel K, et al. Catheter ablation for atrial fibrillation in hypertrophic cardiomyopathy: a systematic review and meta-analysis. Heart. 2016;102:1533–43.
Sherrid MV, Barac I, McKenna WJ, et al. Multicenter study of the efficacy and safety of disopyramide in obstructive hypertrophic cardiomyopathy. J Am Coll Cardiol. 2005;45:1251–8.
Guttmann OP, Rahman MS, O’Mahony C, Anastasakis A, Elliott PM. Atrial fibrillation and thromboembolism in patients with hypertrophic cardiomyopathy: systematic review. Heart. 2014;100:465–72.
Spirito P, Autore C, Formisano F, et al. Risk of sudden death and outcome in patients with hypertrophic cardiomyopathy with benign presentation and without risk factors. Am J Cardiol. 2014;113:1550–5.
Link MS, Bockstall K, Weinstock J, et al. Ventricular tachyarrhythmias in patients with hypertrophic cardiomyopathy and defibrillators: triggers, treatment, and implications. J Cardiovasc Electrophysiol. 2017;28:531–7.
Gersh BJ, Maron BJ, Bonow RO, et al. 2011 ACCF/AHA guideline for the diagnosis and treatment of hypertrophic cardiomyopathy: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Developed in collaboration with the American Association for Thoracic Surgery, American Society of Echocardiography, American Society of Nuclear Cardiology, Heart Failure Society of America, Heart Rhythm Society, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. Circulation. 2011;124:e783-831.
Alvares RF, Goodwin JF. Non-invasive assessment of diastolic function in hypertrophic cardiomyopathy on and off beta-adrenergic blocking drugs. Br Heart J. 1982;48:204–12.
Axelsson A, Iversen K, Vejlstrup N, et al. Efficacy and safety of the angiotensin II receptor blocker losartan for hypertrophic cardiomyopathy: the INHERIT randomised, double-blind, placebo-controlled trial. Lancet Diabetes Endocrinol. 2015;3:123–31.
Nguyen A, Schaff HV, Nishimura RA, Geske JB, Dearani JA, King KS, Ommen SR. Apical myectomy for patients with hypertrophic cardiomyopathy and advanced heart failure. J Thorac Cardiovasc Surg. 2019;S0022-5223(19)30772-X. https://doi.org/10.1016/j.jtcvs.2019.03.088
Yancy CW, Jessup M, Bozkurt B, et al. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2013;128:e240-327.
Harris KM, Spirito P, Maron MS, et al. Prevalence, clinical profile, and significance of left ventricular remodeling in the end-stage phase of hypertrophic cardiomyopathy. Circulation. 2006;114:216–25.
Magri D, Re F, Limongelli G, et al. Heart failure progression in hypertrophic cardiomyopathy-possible insights from cardiopulmonary exercise testing. Circ J. 2016;80:2204–11.
Kato TS, Takayama H, Yoshizawa S, et al. Cardiac transplantation in patients with hypertrophic cardiomyopathy. Am J Cardiol. 2012;110:568–74.
Rowin EJ, Maron BJ, Kiernan MS, et al. Advanced heart failure with preserved systolic function in nonobstructive hypertrophic cardiomyopathy: under-recognized subset of candidates for heart transplant. Circ Heart Fail. 2014;7:967–75.
Maron MS, Olivotto I, Zenovich AG, et al. Hypertrophic cardiomyopathy is predominantly a disease of left ventricular outflow tract obstruction. Circulation. 2006;114:2232–9.
Rowin EJ, Maron BJ, Lesser JR, et al. Papillary muscle insertion directly into the anterior mitral leaflet in hypertrophic cardiomyopathy, its identification and cause of outflow obstruction by cardiac magnetic resonance imaging, and its surgical management. Am J Cardiol. 2013;111:1677–9.
Teo EP, Teoh JG, Hung J. Mitral valve and papillary muscle abnormalities in hypertrophic obstructive cardiomyopathy. Curr Opin Cardiol. 2015;30:475–82.
Holst KA, Hanson KT, Ommen SR, et al. Septal myectomy in hypertrophic cardiomyopathy: national outcomes of concomitant mitral surgery. Mayo Clin Proc. 2019;94:66–73.
Okutucu S, Aksoy H, Sayin BY, Oto A. Targeted septal branch microcirculatory embolization with tris-acryl gelatin microspheres in hypertrophic obstructive cardiomyopathy. Eur Heart J. 2020. https://doi.org/10.1093/ehjci/ehaa946.2093.
Dukkipati SR, d’Avila A, Soejima K, et al. Long-term outcomes of combined epicardial and endocardial ablation of monomorphic ventricular tachycardia related to hypertrophic cardiomyopathy. Circ Arrhythm Electrophysiol. 2011;4:185–94.
Santangeli P, Muser D, Maeda S, et al. Comparative effectiveness of antiarrhythmic drugs and catheter ablation for the prevention of recurrent ventricular tachycardia in patients with implantable cardioverter-defibrillators: a systematic review and meta-analysis of randomized controlled trials. Heart Rhythm. 2016;13:1552–9.
Baquero GA, Banchs JE, Depalma S, et al. Dofetilide reduces the frequency of ventricular arrhythmias and implantable cardioverter defibrillator therapies. J Cardiovasc Electrophysiol. 2012;23:296–301.
Rowin EJ, Maron BJ, Abt P, et al. Impact of advanced therapies for improving survival to heart transplant in patients with hypertrophic cardiomyopathy. Am J Cardiol. 2018;121:986–96.
Heitner SB, Jacoby D, Lester SJ, et al. Mavacamten treatment for obstructive hypertrophic cardiomyopathy: a clinical trial. Ann Intern Med. 2019;170:741–8.
Olivotto I, Oreziak A, Barriales-Villa R, et al. Mavacamten for treatment of symptomatic obstructive hypertrophic cardiomyopathy (EXPLORER-HCM): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet. 2020;396(10253):759–69. https://doi.org/10.1016/S0140-6736(20)31792-X (Erratum in: Lancet. 2020 Sep 12;396(10253):758).
Ho CY, Mealiffe ME, Bach RG. Evaluation of mavacamten in symptomatic patients with nonobstructive hypertrophic cardiomyopathy. J Am Coll Cardiol. 2020;75(21):2649–60.
Horowitz JD, Chirkov YY. Perhexiline and hypertrophic cardiomyopathy: a new horizon for metabolic modulation. Circulation. 2010;122:1547–9.
Abozguia K, Elliott P, McKenna W, et al. Metabolic modulator perhexiline corrects energy deficiency and improves exercise capacity in symptomatic hypertrophic cardiomyopathy. Circulation. 2010;122:1562–9.
Olivotto I, Camici PG, Merlini PA, et al. Efficacy of ranolazine in patients with symptomatic hypertrophic cardiomyopathy: the RESTYLE-HCM randomized, double-blind, placebo-controlled study. Circ Heart Fail. 2018;11: e00412.
Olivotto I, Hellawell JL, Farzaneh-Far R, et al. Novel approach targeting the complex pathophysiology of hypertrophic cardiomyopathy: the impact of Late Sodium Current Inhibition on Exercise capacity in Subjects with Symptomatic Hypertrophic Cardiomyopathy (LIBERTY-HCM) trial. Circ Heart Fail. 2016;9:e002764.
Axelsson Raja A, Shi L, Day SM, et al. Baseline characteristics of the VANISH cohort. Circ Heart Fail. 2019;12(12):e006231.
McMurray JJ, Packer M, Desai AS, et al. Angiotensin-neprilysin inhibition versus enalapril in heart failure. N Engl J Med. 2014;371:993–1004.
Zinman B, Wanner C, Lachin JM, et al. Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. N Engl J Med. 2015;373:2117–28.
McMurray JJ, Solomon SD, Inzucchi SE, et al. Dapagliflozin in patients with heart failure and reduced ejection fraction. N Engl J Med. 2019;381:1995–2008.
Crossen K, Jones M, Erikson C. Radiofrequency septal reduction in symptomatic hypertrophic obstructive cardiomyopathy. Heart Rhythm. 2016;13:1885–90.
Zuo L, Sun C, Yang J, et al. Percutaneous trans-apex intra-septal radiofrequency ablation of hypertrophic cardiomyopathy. Minim Invasive Ther Allied Technol. 2018;27:97–100.
Liu L, Li J, Zuo L, et al. Percutaneous intramyocardial septal radiofrequency ablation for hypertrophic obstructive cardiomyopathy. J Am Coll Cardiol. 2018;72:1898–909.
Nazer B, Gerstenfeld EP, Hata A, Crum LA, Matula TJ. Cardiovascular applications of therapeutic ultrasound. J Interv Card Electrophysiol. 2014;39:287–94.
Ma H, Marti-Gutierrez N, Park SW, et al. Correction of a pathogenic gene mutation in human embryos. Nature. 2017;548:413–9.
Jiang J, Wakimoto H, Seidman JG, Seidman CE. Allele-specific silencing of mutant MYH6 transcripts in mice suppresses hypertrophic cardiomyopathy. Science. 2013;342:111–4.
Germain DP. Fabry disease. Orphanet J Rare Dis. 2010;5:30. https://doi.org/10.1186/1750-1172-5-30.
Lidove O, Kaminsky P, Hachulla E, et al. Fabry disease “The New Great Imposter”: results of the French Observatoire in Internal Medicine Departments (FIMeD). Clin Genet. 2012;81(6):571.
Akhtar MM, Elliott PM. Anderson-Fabry disease in heart failure. Biophys Rev. 2018;10(4):1107–19. https://doi.org/10.1007/s12551-018-0432-5.
O’Mahony C, Elliott P. Anderson-Fabry disease and the heart. Prog Cardiovasc Dis. 2010;52(4):326–35.
Patel MR, Cecchi F, Cizmarik M, et al. Cardiovascular events in patients with fabry disease natural history data from the Fabry registry. J Am Coll Cardiol. 2011;57(9):1093–9.
Sachdev B, Takenaka T, Teraguchi H, et al. Prevalence of Anderson-Fabry disease in male patients with late onset hypertrophic cardiomyopathy. Circulation. 2002;105:1407.
Yousef Z, Elliott PM, Cecchi F, et al. Left ventricular hypertrophy in Fabry disease: a practical approach to diagnosis. Eur Heart J. 2013;34:802.
Miller JJ, Kanack AJ, Dahms NM. Progress in the understanding and treatment of Fabry disease. Biochim Biophys Acta Gen Subj. 2019;1864:129437.
Markham A. Migalastat: first global approval. Drugs. 2016;76:1147–52. https://doi.org/10.1007/s40265-016-0607-y.
Schiffmann R, Hughes DA, Linthorst GE, et al. Screening, diagnosis, and management of patients with Fabry disease: conclusions from a “Kidney Disease: Improving Global Outcomes” (KDIGO) Controversies Conference. Kidney Int. 2017;91:284.
Cantor WJ, Daly P, Iwanochko M, et al. Cardiac transplantation for Fabry’s disease. Can J Cardiol. 1998;14:81.
Shah JS, Hughes DA, Sachdev B, et al. Prevalence and clinical significance of cardiac arrhythmia in Anderson-Fabry disease. Am J Cardiol. 2005;96:842.
Ikari Y, Kuwako K, Yamaguchi T. Fabry’s disease with complete atrioventricular block: histological evidence of involvement of the conduction system. Br Heart J. 1992;68:323.
Rajagopalan N, Dennis DR, O’Connor W. Successful combined heart and kidney transplantation in patient with Fabry’s disease: a case report. Transplant Proc. 2019;51(9):3171–3. https://doi.org/10.1016/j.transproceed.2019.03.032.
Barbey F, Qanadli SD, Juli C, et al. Aortic remodelling in Fabry disease. Eur Heart J. 2010;31:347.
Schiffmann R, Kopp JB, Austin HA 3rd, et al. Enzyme replacement therapy in Fabry disease: a randomized controlled trial. JAMA. 2001;285:2743.
Ramaswami U, Bichet DG, Clarke LA, et al. Low-dose agalsidase beta treatment in male pediatric patients with Fabry disease: a 5-year randomized controlled trial. Mol Genet Metab. 2019;127(1):86–94. https://doi.org/10.1016/j.ymgme.2019.03.010.
Imbriaco M, Pisani A, Spinelli L, et al. Effects of enzyme-replacement therapy in patients with Anderson-Fabry disease: a prospective long-term cardiac magnetic resonance imaging study. Heart. 2009;95:1103.
Weidemann F, Niemann M, Breunig F, et al. Long-term effects of enzyme replacement therapy on fabry cardiomyopathy: evidence for a better outcome with early treatment. Circulation. 2009;119:524.
Schiffmann R, Murray GJ, Treco D, et al. Infusion of alpha-galactosidase A reduces tissue globotriaosylceramide storage in patients with Fabry disease. Proc Natl Acad Sci USA. 2000;97:365.
Pieroni M, Moon JC, Arbustini E, et al. Cardiac involvement in Fabry disease. J Am Coll Cardiol. 2021;77(7):922–36. https://doi.org/10.1016/j.jacc.2020.12.024.
Thurberg BL, Fallon JT, Mitchell R, et al. Cardiac microvascular pathology in Fabry disease: evaluation of endomyocardial biopsies before and after enzyme replacement therapy. Circulation. 2009;119:2561.
Van der Veen SJ, van Kuilenburg ABP, et al. Antibodies against recombinant alpha-galactosidase A in Fabry disease: subclass analysis and impact on response to treatment. Mol Genet Metab. 2019;126(2):162–8. https://doi.org/10.1016/j.ymgme.2018.11.008.
Mehta A, Beck M, Elliott P, et al. Enzyme replacement therapy with agalsidase alfa in patients with Fabry’s disease: an analysis of registry data. Lancet. 2009;374(9706):1986–96. https://doi.org/10.1016/S0140-6736(09)61493-8.
Weidemann F, Niemann M, Störk S. Long-term outcome of enzyme-replacement therapy in advanced Fabry disease: evidence for disease progression towards serious complications. J Intern Med. 2013;274(4):331–41.
Benjamin ER, Della Valle MC, Wu X, et al. The validation of pharmacogenetics for the identification of Fabry patients to be treated with migalastat. Genet Med. 2017;19:430.
Germain DP, Hughes DA, Nicholls K, et al. Treatment of Fabry’s disease with the pharmacologic chaperone migalastat. N Engl J Med. 2016;375(6):545–55.
Hughes DA, Nicholls K, Shankar SP, et al. Oral pharmacological chaperone migalastat compared with enzyme replacement therapy in Fabry disease: 18-month results from the randomised phase III ATTRACT study. J Med Genet. 2017;54:288.
Weidemann F, Sommer C, Duning T, et al. Department-related tasks and organ-targeted therapy in Fabry disease: an interdisciplinary challenge. Am J Med. 2010;123:658.e1.
Xu S, Lun Y, Brignol N, et al. Coformulation of a novel human alpha-galactosidase a with the pharmacological chaperone AT1001 leads to improved substrate reduction in Fabry mice. Mol Ther. 2015;23(7):1169–81. https://doi.org/10.1038/mt.2015.87.
Platt FM. Emptying the stores: lysosomal diseases and therapeutic strategies. Nat Rev Drug Discov. 2018;17(2):133–50. https://doi.org/10.1038/nrd.2017.214.
Van der Veen SJ, Hollak CEM, van Kuilenburg ABP, Langeveld M. Developments in the treatment of Fabry disease. J Inherit Metab Dis. 2020;43:908–12.
Nagree MS, Scalia S, McKillop WM, Medin JA. An update on gene therapy for lysosomal storage disorders. Expert Opin Biol Ther. 2019;19(7):655–70. https://doi.org/10.1080/14712598.2019.1607837.
Ash S, Shorer E, Ramgobin D, et al. Cardiac amyloidosis—a review of current literature for the practicing physician. Clin Cardiol. 2021. https://doi.org/10.1002/clc.23572.
Kittleson M, Maurer M, Ambardekar A, et al. Cardiac amyloidosis: evolving diagnosis and management: a scientific statement from the American Heart Association. Circulation. 2020;142(1):e7–22.
Maleszewski JJ. Cardiac amyloidosis: pathology, nomenclature, and typing. Cardiovasc Pathol. 2015;24(6):343–50. https://doi.org/10.1016/j.carpath.2015.07.008.
Falk R, Alexander K, Liao R, Dorbala S. AL (light-chain) cardiac amyloidosis. J Am Coll Cardiol. 2016;68(12):1323–41. https://doi.org/10.1016/j.jacc.2016.06.053.
Dubrey SW, Hawkins PN, Falk RH. Amyloid diseases of the heart: assessment, diagnosis, and referral. Heart. 2011;97:75–84.
Palladini G, Dispenzieri A, Gertz MA, et al. New criteria for response to treatment in immunoglobulin light chain amyloidosis based on free light chain measurement and cardiac biomarkers: impact on survival outcomes. J Clin Oncol. 2012;30(36):4541–9.
Binder C, Duca F. Diagnosis and supportive therapeutic management of cardiac light chain amyloidosis—a cardiologist’s perspective. Memo. 2021;14:89–97.
Witteles RM, Liedtke M. AL amyloidosis for the cardiologist and oncologist: epidemiology, diagnosis, and management. J Am Coll Cardiol Cardio Oncol. 2019;1:117–30.
Pislaru C, Ionescu F, Alashry M, et al. Myocardial stiffness by intrinsic cardiac elastography in patients with amyloidosis: comparison with chamber stiffness and global longitudinal strain. J Am Soc Echocardiogr. 2019;32:958–68.e4.
Gertz MA, Cohen AD, Comenzo RL, et al. Results of the phase 3 VITAL study of NEOD001 (Birtamimab) plus standard of care in patients with light chain (AL) amyloidosis suggest survival benefit for mayo stage IV patients. Blood. 2019;134:3166.
Mereles D, Buss SJ, Hardt SE, Hunstein W, Katus HA. Effects of the main green tea polyphenol epigallocatechin-3-gallate on cardiac involvement in patients with AL amyloidosis. Clin Res Cardiol. 2010;99:483–90.
Barrett CD, Alexander KM, Zhao H, et al. Outcomes in patients with cardiac amyloidosis undergoing heart transplantation. Heart Fail. 2020;8:461–8.
Gertz MA, Benson MD, Dyck PJ, et al. Diagnosis, prognosis, and therapy of Transthyretin amyloidosis. J Am Coll Cardiol. 2015;66(21):2451–66.
Maurer MS, Hanna M, Grogan M, et al. Genotype and phenotype of transthyretin cardiac amyloidosis: THAOS (Transthyretin amyloid outcome survey). J Am Coll Cardiol. 2016;68(2):161–72. https://doi.org/10.1016/j.jacc.2016.03.596.
Hassan W, Al-Sergani H, Mourad W, et al. Amyloid heart disease. New frontiers and insights in pathophysiology, diagnosis, and management. Tex Heart Inst J. 2005;32(2):178–84.
Kitaoka H, Izumi C, Izumiya Y, et al. JCS 2020 Guideline on diagnosis and treatment of cardiac amyloidosis. Circ J. 2020;84(9):1610–71. https://doi.org/10.1253/circj.CJ-20-0110.-157.
Merlini G. AL amyloidosis: from molecular mechanisms to targeted therapies. Hematol Am Soc Hematol Educ Program. 2017;2017(1):1–12.
Garcia-Pavia P, Rapezzi C, Adler Y, et al. Diagnosis and treatment of cardiac amyloidosis: a position statement of the ESC working group on myocardial and pericardial diseases. Eur Heart J. 2021;42(16):1554–68.
Maurer MS, Schwartz JH, Gundapaneni B, et al. Tafamidis treatment for patients with transthyretin amyloid cardiomyopathy. N Engl J Med. 2018;379(11):1007–16.
Grogan M, Scott CG, Kyle RA, et al. Natural history of wild-type transthyretin cardiac amyloidosis and risk stratification using a novel staging system. J Am Coll Cardiol. 2016;68:1014–20.
Barroso FA, Judge DP, Ebede B, et al. Long-term safety and efficacy of tafamidis for the treatment of hereditary transthyretin amyloid polyneuropathy: results up to 6 years. Amyloid. 2017;24(3):194–204.
Tuzovic M, Yang EH, Baas AS, et al. Cardiac amyloidosis: diagnosis and treatment strategies. Curr Oncol Rep. 2017;19:46.
Karlstedt E, Jimenez-Zepeda V, Howlett JG, White JA, Fine NM. Clinical experience with the use of doxycycline and ursodeoxycholic acid for the treatment of transthyretin cardiac amyloidosis. J Card Fail. 2019;25(3):147–53.
Solomon SD, Adams D, Kristen A, et al. Effects of Patisiran, an RNA interference therapeutic, on cardiac parameters in patients with hereditary transthyretin-mediated amyloidosis. Circulation. 2019;139(4):431–43.
Siepen FAD, Bauer R, Voss A, et al. Predictors of survival stratification in patients with wild-type cardiac amyloidosis. Clin Res Cardiol. 2018;107:158–69.
Rocken C, Shakespeare A. Pathology, diagnosis and pathogenesis of AA amyloidosis. Virchows Arch. 2002;440(2):111–22.
Real de Asua D, Costa R, Galvan JM, et al. Systemic AA amyloidosis: epidemiology, diagnosis, and management. Clin Epidemiol. 2014;6:369–77.
Acknowledgements
Funding
No funding or sponsorship was received for this study or publication of this article.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contribution
All authors contributed to the study conception and design. All authors read and approved the final manuscript.
Disclosures
Begum Yetis Sayin and Ali Oto have nothing to disclose.
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not contain any studies with human participants or animals performed by any of the authors.
Data Availability
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Sayin, B.Y., Oto, A. Left Ventricular Hypertrophy: Etiology-Based Therapeutic Options. Cardiol Ther 11, 203–230 (2022). https://doi.org/10.1007/s40119-022-00260-y
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40119-022-00260-y