Myocarditis and sports in the young: data from a nationwide registry on myocarditis—“MYKKE-Sport”
- 1Department of Pediatric Cardiology, Friedrich-Alexander-Universität, Erlangen-Nürnberg, Germany
- 2School of Clinical and Applied Sciences, Leeds Beckett University, Leeds, Great Britain
- 3Competence Network for Congenital Heart Defects, Berlin, Germany
- 4Department of Pediatric Cardiology, Charité-Universitätsmedizin Berlin, Berlin, Germany
- 5Department of Paediatric Cardiology and Intensive Care Medicine, Hannover Medical School, Hannover, Germany
- 6Clinic for Paediatric Cardiology, Heart Centre, University of Leipzig, Leipzig, Germany
- 7Department for Paediatric Cardiology, University Heart Center Freiburg, Freiburg, Germany
- 8Department for Paediatric Cardiology, University Hospital Tübingen, Tübingen, Germany
- 9Heart- and Diabetes Center North Rhine-Westphalia, Center of Pediatric Cardiology and Congenital Heart Disease, Ruhr University Bochum, Bad Oeynhausen, Germany
- 10Pediatric Cardiology, University Hospital Ulm, Ulm, Germany
- 11Department of Cardiology, German Heart Center Berlin, Berlin, Germany
- 12Department of Cardiology, Charité-Universitätsmedizin, Berlin, Germany
- 13German Centre for Cardiovascular Research, Berlin, Germany
- 14Department of Congenital Heart Disease and Pediatric Cardiology, German Heart Center Berlin, Berlin, Germany
- 15Institute for Imaging Science and Computational Modelling in Cardiovascular Medicine, Charité-Universitätsmedizin Berlin, Berlin, Germany
- 16Experimental and Clinical Research Center, A Cooperation Between the Max-Delbrück-Center for Molecular Medicine in the Helmholtz Association and the Charité-Universitätsmedizin Berlin, Berlin, Germany
Background: Myocarditis represents one of the most common causes of Sudden Cardiac Death in children. Myocardial involvement during a viral infection is believed to be higher as a consequence of intensive exertion. Recommendations for return to sports are based on cohort and case studies only. This study aims to investigate the relationship between physical activity and myocarditis in the young.
Patient: Every patient in the MYKKE registry fulfilling criteria for suspicion of myocarditis was sent a questionnaire regarding the physical activity before, during and after the onset of myocarditis.
Method: This study is a subproject within the MYKKE registry, a multicenter registry for children and adolescents with suspected myocarditis. The observation period for this analysis was 93 months (September 2013–June 2021). Anamnestic, cardiac magnetic resonance images, echocardiography, biopsy and laboratory records from every patient were retrieved from the MYKKE registry database.
Results: 58 patients (mean age 14.6 years) were enrolled from 10 centers. Most patients participated in curricular physical activity and 36% in competitive sports before the onset of myocarditis. There was no significant difference of heart function at admission between the physically active and inactive subjects (ejection fraction of 51.8 ± 8.6% for the active group vs. 54.4 ± 7.7% for the inactive group). The recommendations regarding the return to sports varied widely and followed current guidelines in 45%. Most patients did not receive an exercise test before returning to sports.
Conclusion: Sports before the onset of myocarditis was not associated with a more severe outcome. There is still a discrepancy between current literature and actual recommendations given by health care providers. The fact that most participants did not receive an exercise test before being cleared for sports represents a serious omission.
1. Introduction
Myocarditis, defined as an “inflammatory disease of the heart muscle” is considered one of the most common acquired causes of arrhythmias, myocardial dysfunction, heart failure, and sudden cardiac death (SCD) in young individuals (1, 2).
1.1. Symptoms and diagnosis
Especially in the general population the exact incidence of myocarditis is unclear because of undiagnosed and asymptomatic cases (3). In athletes the incidence rate varies depending on the investigated cohorts but accounts for up to 8% of deaths (1, 4, 5). Myocarditis has been identified as the most common structural cause of Sudden Cardiac Death (SCD) in children in Denmark (6). A study using a nationwide registry on sports related SCD's (SRSD) in Germany also found myocarditis to prevail as cause in young athletes (<35 years of age) (7). Most cases of SRSD due to myocarditis were related to non-elite competitive or recreational activity (6, 7, 8). Almost all cases were preceded by upper respiratory tract infections (7). As a consequence of intensive exertion during physical activity (PA), the amount of myocardial involvement during viral infections has been shown to be higher in animal models and even a short break (8 days) from physical activity led to a significant decrease in mortality due to myocarditis (9). These findings stress the importance of clarifying the relationships between myocarditis and return to sports in the pediatric community.
There are recommendations for return to sport after myocarditis (10). These are based on case series and low-quality cohort and case studies. After suspected or diagnosed myocarditis athletes are recommended to stop training and competing for 3–6 months depending on the extent of reduction in ejection fraction and the myocardial damage seen in magnetic resonance imaging (MRI) (10). Most of the time, conservative approaches with long periods of restraint are suggested, with severe consequences for the children (11). Those, who participate in competitive sports face training losses and in some cases future careers may be at stake. However, in a time in which most children spend too much time with sedentary behavior (12), the decrease in cardiopulmonary fitness due to prolonged restrictions of physical activity with myocarditis could have detrimental effects for the affected children (13).
Another aspect is the fact that long periods of rest are not adhered to by the patients (11). Clear instructions based on evidence in combination with regular follow-ups for insuring compliance are therefore essential in the treatment of myocarditis in young patients and athletes.
This study aims to investigate the relationship between physical activity and the occurrence of myocarditis as well as the compliance to the provided recommendations.
2. Material and methods
This study is a subproject of the MYKKE registry, which is a multicenter registry for children and adolescents with suspected myocarditis (14). Patients with suspected myocarditis have been included since September 2013. The observation period for this analysis was 93 months (September 2013 to June 2021). Patients from the MYKKE registry meeting the following criteria were enrolled (15):
- Age ≥5 years and <18 years at first admission and
- Biopsy proven myocarditis or
- Myocarditis diagnosed in MRI [positive late gadolinium enhancement (LGE) and/or edema] or
- Electrocardiographic (ECG) abnormalities like ST-elevation and T-inversion or
- Elevated cardiac biomarkers (Troponin I and/or N-terminal pro brain natriuretic peptide (NT-proBNP).
We did not include subjects at a lower age as it is very difficult to assess physical activity in the very young.
The study was approved by the ethical committee of the Charité Universitätsmedizin Berlin, Germany and the Friedrich-Alexander-Universität Erlangen-Nürnberg, Germany.
Every patient from the registry fulfilling the mentioned criteria was then sent a questionnaire specifying the physical activity around the occurrence of the myocarditis as well as after 6 and 12 months.
The questionnaire was divided in several sections:
(1) 6 months prior to the onset of myocarditis the participation in curricular physical activities (PA) and the amount of extracurricular PA in type of sport and hours per week was established. It was also investigated whether the sport was performed as a competitive sport and how the children got to school (by bus/car, by bike or on foot)
(2) 2 weeks prior to the onset of myocarditis it was established whether the participant had practiced their sport as before, less or more, whether there were signs of infection and if so what kind of the infection (fever, sore throat, runny nose, diarrhea, other). Was a rest period undertaken.
(3) After treatment for myocarditis was a rest period recommended and if so for how long. What diagnostics were undertaken before return to sports (echocardiography, MRI, stress test, Holter ECG) and what recommendations were given for the return to sports (moderate intensity, individualized training programme, competitive sport) or were special sports prohibited (risk sports, contact sports, competitive sports). How long was the control interval?
(4) The compliance was established by asking whether the recommendations had been adhered to and if not with regards to competitive sports, risk sports, contact sports or intensity. How long was the true resting period before returning to sports and at what intensity.
(5) Symptoms after returning to sports were classified as: dyspnea, chest pain or rhythm disorders and subdivided into occurrence during PA or at rest.
(6) The occurrence of a recurrence as well as whether it had occurred during PA was recorded in a binary fashion.
(7) The question from 1) were then asked again after 6 and after 12 months.
The data from the MYKKE registry included anthropometric data (age, height, weight), data from MRI (LGE occurrence, EF), echocardiography, ECG (rhythm disorder, repolarization abnormalities), the laboratory (CRP, blood count, Troponin, NT/pro-BNP, virology), exercise test (VO2peak, patient characteristics (age, height, weight at the moment of myocarditis),.
2.1. Data analysis
Statistical analysis was performed using SPSS 24.0® (SPSS Inc., Chicago, IL). All measured values are reported as means and standard deviations or as median and interquartile range (P25 and P75) for non-Gaussian distributed data. The Kologomorov-Smirnov test was used to check for normal distribution. Homogeneity of variance was investigated using Levine's F-test. Parametric, normally distributed variables were investigated using Student t-test, non-parametric variables were investigated using χ2-test. A p-value of <0.05 was considered statistically significant.
3. Results
3.1. Demographics
An overall of 220 patients were contacted for completing the questionnaire. In 58 (26.4%) cases we were able to retrieve completed questionnaires. The mean age at the onset of myocarditis was 14.6 (±3.13) years of age (minimum 5.7 years, maximum 18 years). Most of the subjects were between 13 and 17 years of age (70.7%). There were more male subjects (65.5%) than females (34.5%). All the demographic data is represented in Table 1.
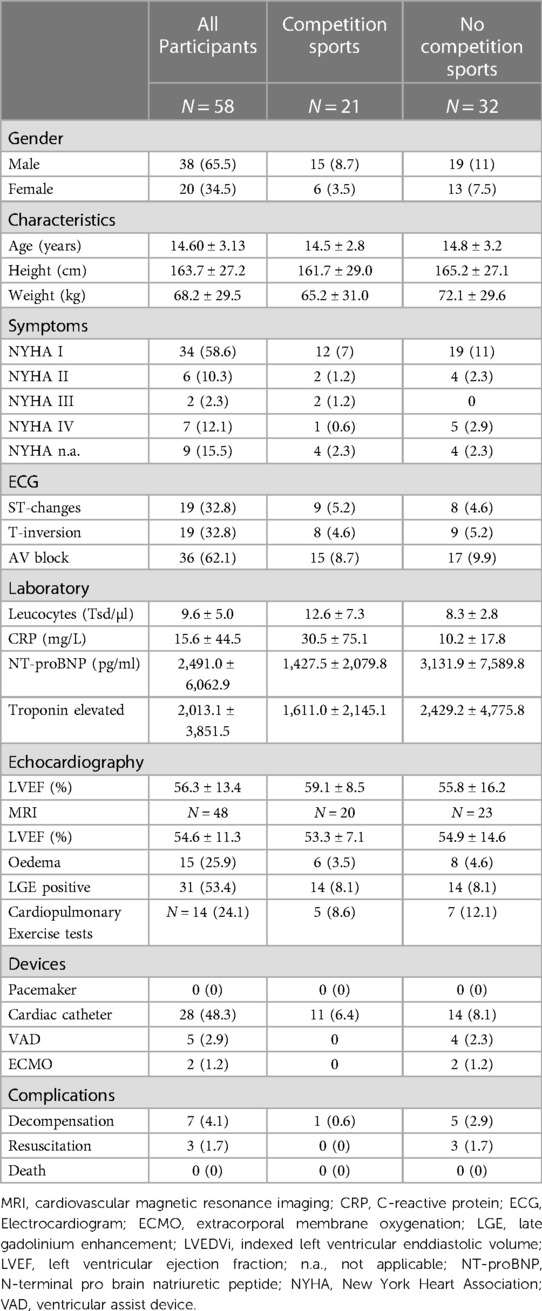
Table 1. Demographics of the participants with values given as absolute numbers with percentage of the total number in parentheses (%), or as means ± standard deviation.
3.2. Before the onset of myocarditis
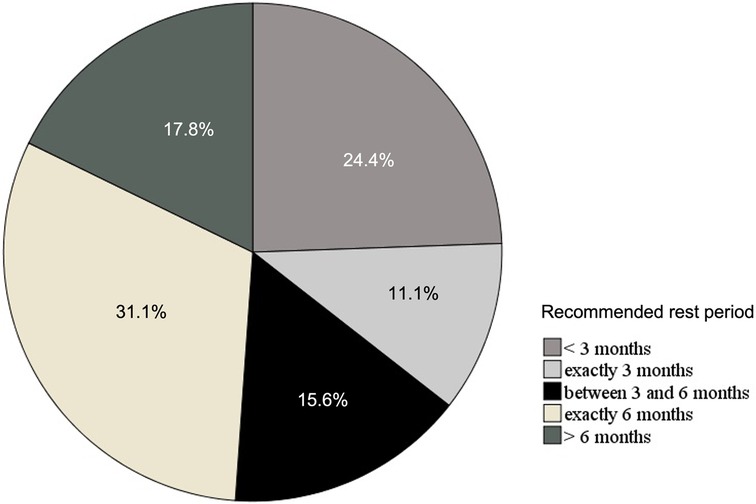
Most of the subjects had participated regularly in school or kindergarten related physical activity (84.5%) 6 months prior to the onset of myocarditis. There was no significant difference between the subjects who had participated in curricular physical activity (PA) and those who had not with regards to the diagnostic parameters (left ventricular ejection fraction (LVEF) in echocardiography, LVEF in MRI, C-reactive protein (CRP), leucocyte count, NT-proBNP, Troponin, or the numbers of participants with ECG abnormalities (ST-changes, T-inversion or AV-Block) at onset of myocarditis. An overall of 21 subjects (36.2%) participated in competition sport. The subjects who competed in sports did not differ significantly from those who didn't with respect to the diagnostic parameters defined above (see Table 1). There were actually more left ventricular assist devices (LVAD) (4 vs.0) and extracorporeal membrane oxygenation (ECMO) patients (2 vs. 0) in the group of myocarditis patients who did not participate in competition sports. Figure 1 represents the different types of extracurricular physical activities performed by the subjects.
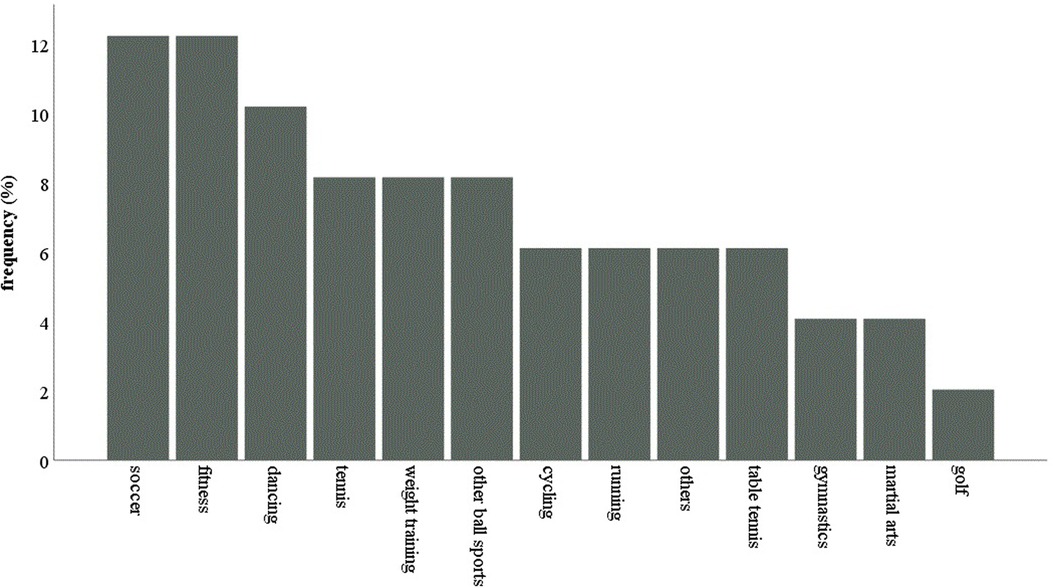
Figure 1. The different types of extracurricular physical activities performed by the subjects before the onset of myocarditis (in %).
3.3. Around the onset of myocarditis
An overall of 35 (60.3%) subjects performed their sport as before 2 weeks before the onset of myocarditis, while 21 (37.9%) subjects had reduced their amount of PA and 2 patients (3.4%) had increased their physical activity compared to 6 months before. The two patients who were doing more sports 2 weeks prior to the onset of myocarditis did not experience more severe symptoms or showed signs of a more serious course of disease. They also did not experience symptoms of an infectious disease and thus did not feel the need to reduce their physical activity.
Symptoms of an infectious disease were reported by 54 (60.3%) participants. The other 4 participants (6.9%) reported no symptoms of an infectious disease. The frequency of the symptoms is depicted in Figure 2. Where subjects reported of more than one symptom, the more severe was listed (fever > sore throat or diarrhea > runny nose > unspecific symptoms). The severity of symptoms was ranked according to the guidelines referred to as the “neck-check”, in which localized symptoms of infectious disease are classified as above the neck and below the neck and recommendations for return to sport are more restrictive when the symptoms are below the neck as they are thought to be more severe (16, 17). Unspecific symptoms, subclassified as “other” were headache and cough.
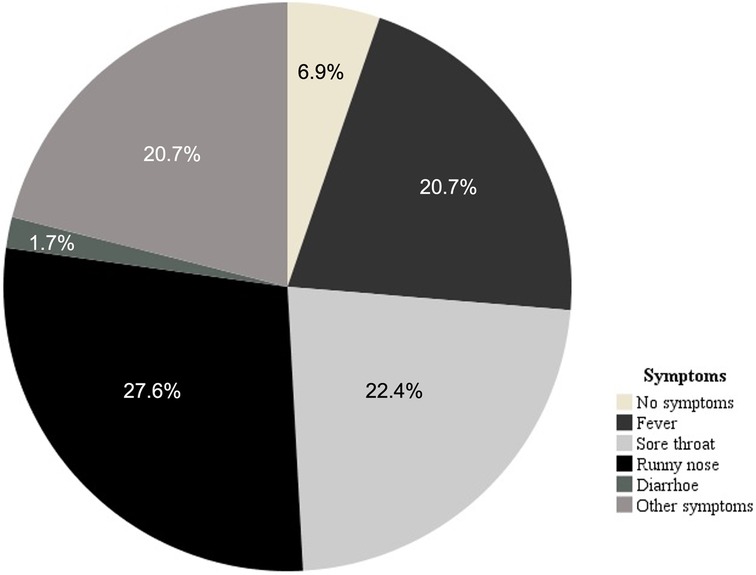
Figure 2. The frequency of symptoms reported by the subjects 2 weeks prior to the onset of myocarditis. Where subjects reported of more than one symptom, the more severe was listed (fever > sore throat or diarrhea > runny nose > unspecific symtpoms).
There were no significant differences with respect to the outcome parameters. [LVEF in MRI or echocardiography, occurrence of LGE, cardiac biomarkers, peak oxygen uptake (VO2peak)] between the patients with symptoms of an infectious disease in comparison to those without (see Table 2). The patients reporting of symptoms of an infectious disease were asked whether that led to a reduction in PA. The 13 patients (37.1%) who continued training showed a significantly higher LVEF in echocardiography (61.6 ± 7.5%) compared to those who stopped with their training (49 ± 15.7%). Even though, this was also true for the LVEF determined using MRI, this difference did not reach significance. All the other outcome parameters were comparable between these two groups (see Table 3).
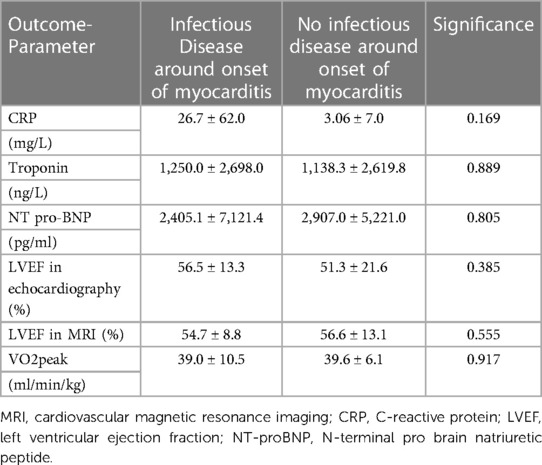
Table 2. Mean values ± standard deviations of outcome parameters for participants who had experienced symptoms of an infectious disease two weeks prior to the onset of myocarditis and those who did not.
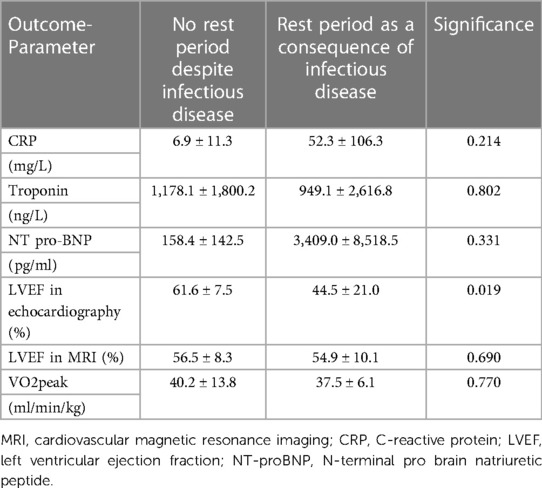
Table 3. Mean values ± standard deviations of outcome parameters for participants who kept training despite symptos of an infectious disease and those who did not.
3.4. Recommendations
Most of the patients (82.8%) were recommended to stop physical activity after the onset of myocarditis by their medical care provider. However, the recommendations varied hugely with respect to return to sports from 4 weeks to 1 year (average 23.6 weeks). The recommended rest periods are represented in Figure 3. In only 44.8% of the cases the recommendations were in accordance with the recent recommendations from the European Society of Cardiology (ESC), whereas in more than half of the cases (55.2%) they were not (10). In those, where the recommendations were not adhered to, 57.9% of the cases were advised to return to sports after less than 3 months and in 42.1% the return to physical activity was longer than 6 months.
The criteria for return to sport include:
- normalization of EF and laboratory parameters (troponin, NT pro-BNP),
- no malignant arrhythmias in Holter Monitoring and/or during cardiopulmonary exercise test (CPET))
All necessary examinations needed for these criteria to be fulfilled were only performed in 15.5%. The most common examination performed before return to sports was the echocardiography with 70.7%. Less than half of the patients (48.3%) received cardiopulmonary exercise testing and Holter monitoring was conducted in 55.2%.
50 patients (86.2%) followed the recommendations with respect to the rest period. After return to sport 31 patients (53.4%) began with moderate intensity continuous training (MICT), 10 followed an individualized training protocol, 4 (6.9%) did not return to sports and 2 (3.4%) returned to competition level.
3.5. Return to sports
Only two patients (3.4%) experienced a relapse of their myocarditis of which one connected the relapse with physical activity. This 13-year-old male patient had been diagnosed with a Parvovirus B19 infection in a biopsy. Before the onset of myocarditis, he had participated in curricular physical activity and had played golf once a week for an hour. Even though his heart function was shown to be normal initially and during control examinations he only returned to sports over 12 months after the onset of myocarditis. A cardiopulmonary exercise test in combination with ECG before return to sports was normal without any signs of arrhythmias. Seventeen days after the last examination he experienced thoracic pain during long jump in school after also having had diarrhoea for three days. The ensuing MRI was suggestive of a relapse with new LGE in the basal and apical parts of the heart but no edema. A new biopsy revealed persistence of Parvovirus B19.
The other patient had a relapse unrelated to physical activity and is therefore not further discussed here.
The majority of patients had no symptoms when returning to sports (69%). Of those (31%) who had symptoms 7 reported of dyspnea, 7 of chest pain, and 9 of perceived tachycardia or arrhythmia.
Six months after the onset of myocarditis more patients did not participate in curricular activities than 6 months before the illness (22.4% vs. 10.3%). This high number of children not participating in school sports remained high after 12 months with 20.7%, even though they had had no severe cases of myocarditis with normal heart function (normal ejection fraction). However, these differences did not reach significance. Most of the subjects who had performed sports on a competition level (9 out of 12) returned to their previous competition sport. None of the competitive athletes experienced a relapse of the myocarditis. They also did not differ with respect to any of the outcome parameters from the group who did not participate in competition sports.
There was no significant difference between the type of extracurricular activity performed before the onset of myocarditis and 6 months later.
Regarding the transport to school or kindergarten nothing changed from before the onset of myocarditis and after. Before and after the onset of myocarditis 70% of all subjects chose the car or the bus to get to school.
4. Discussion
This study used data on a nationwide registry on myocarditis in children to investigate the relationship between myocarditis and sports.
As observed previously (14, 18, 19), there was a male predominance of patients with myocarditis who participated in this study which could be explained by protective effect of female hormones on the immune response (20). Male gender represents an independent risk factor for SCD (21, 22, 23). Most cases in our study ranged from 13 to 17 years of age. This is in accordance with previous reports in which two age peaks could be observed for myocarditis: <2 years of age and in adolescents (13–17 years) (14). Since we did not include children below the age of 6, we only observed the second age peak. As a consequence of the difficulty diagnosing myocarditis (24), this severe illness may be underdiagnosed especially in male adolescents. This in turn could be the cause for the high number of SCD due to myocarditis in this age group if not properly diagnosed, treated and provided with sufficient rest periods from sports.
In our study, the most popular sport disciplines were football and fitness which is in accordance with a previous study on sports related SCD in Germany (7). Since these are also the disciplines most commonly performed by the German youth this is probably merely a reflection of the number of children and adolescents performing these sports and not a reflection of the sports-specific risk with regards to myocarditis (25).
4.1. Around the onset of myocarditis
Interestingly, most of the patients did not reduce the amount of physical activity two weeks prior to the onset of myocarditis. However, most of the patients who experienced symptoms of an infectious disease (21 out of 35 patients) stopped training. From animal models it is known that intensive exertion leads to a higher amount of myocardial involvement (9, 26) and that even a short rest period (< 8 days) before returning to physical activity decreases the mortality due to myocarditis in mouse models (9). Recommendations about the return to sport after infectious disease (27) state that even simple infectious diseases require a sufficient period of convalescence with no sport. Still, 37% did not heed this advice and continued training as before, which did however not lead to a worse outcome.
The most common symptoms were respiratory symptoms as described previously (28), whereas abdominal symptoms were rare which is in contrast with findings from Japan (29). The reason for this discrepancy could lie in the fact, that our population was limited to children older than 6 years. Approximately a third of all patients experienced fever which led to a rest period from physical activity in all of them.
4.2. Recommendations
The fact that the recommendations for the return to sports varied widely between 4 weeks and 1 year reflects our clinical experience. The recommendations are based on a level of evidence of IIa at best (10). As myocarditis is a common cause of ventricular arrhythmias in its acute as well as its chronic phase (24, 30), a recommended time of rest period is paramount for ensuring the safety of the patients. In 19% of the cases the rest period was recommended to be less than 3 months, which is shorter than the current recommendations (10). On the other hand, 13.8% of the patients were advised to rest for more than 6 months, which is longer (10). Given the fact that sedentary behavior leads to serious long-term complications, especially in children and adolescents (31), such recommendations may seem protective but may cause more harm in the long run. The psychological consequences of prolonged breaks from physical activity notwithstanding, the consequences are especially harsh for athletes.
Only 15.5% of all patients received the recommended examinations (echocardiography, Holter Monitoring, CPET, laboratory examination, and ECG). Especially cardiopulmonary exercise testing and Holter monitoring are essential for unmasking malignant arrhythmias which are believed to be the main cause for SCD in athletes in the acute but also the chronic stages of myocarditis (30). Not performing this essential test before clearing children and adolescents for the return to sports could lead to missing malignant arrhythmias and thus represents a dangerous omission. Furthermore, performing an exercise test before clearing young people for the return to sport also enables the physician to state clear recommendations about taking up exercise again. In the case of a reduction in EF, heart rate values around the first ventilatory threshold can be provided for a gradual return to sports. In the case of a normal EF, the recommendation of returning to sports without restriction allows the child or adolescent to accept their recovery from myocarditis.
In our study most patients followed the advice from their health care providers. Especially athletes perceive an infection of the heart muscle as very concerning.
4.3. Return to sports
Only one patient reported of a sport-associated relapse of Parvovirus B19 myocarditis. The MRI was suggestive of a relapse and in the biopsy a persistence of Parvovirus B19 was revealed. However, ECG and cardiac biomarkers were normal, and the patient described no further symptoms after readmission. As Parvovirus B19 persistence has been observed even in asymptomatic individuals (32, 33) it is unclear whether the described symptoms were a true relapse.
Interestingly 31% of all patients described symptoms of dyspnoea, chest pain and perceived tachycardia when returning to sports but persisted with their physical activity without experiencing a relapse. All these symptoms could be interpreted as signs of a relapse or new onset of myocarditis or could stem from detraining. More information is needed on the specificity of symptoms regarding a possible relapse in order to provide the patients with clear recommendations.
There was an increase of children who did not participate in curricular physical activity 6- and 12-months after myocarditis. This is in part attributable to the recommendations from health-care providers. However, in part it is also a consequence of anxiety about the return to sports. After having been instructed to restrict physical activity for a recommended time frame, many parents and children develop anxiety about the return to sports. However, refraining from regular physical activity leads to a worsening of cardiorespiratory fitness (13). As little as an improvement of cardiorespiratory fitness (CRF) by 1 ml/kg/min can reduce the risk for developing overweight or obesity by 10% in 6 years (34). Improving CRF in childhood and adolescence is associated with a healthier cardiovascular profile (31). Given the fact that a physically active childhood enhances a physically active lifestyle over a life span (35), it is extremely important to keep young people active and exercising. It is therefore of the utmost importance to ensure that children and adolescents find their way back into physical activity after the recommended rest period.
4.4. Limitations
Out of 220 patients who were eligible to participate in this study, only 58 returned the questionnaire which in turn leads to a small study group. Not all questions were answered correctly. These incorrections consisted of some participants making two crosses where only one was possible or not answering the question at all. In these cases, no values were recorded for the given variable, limiting the number of answers. This further decreased the reliable data. Also, the study is retrospective in its approach so causalities could not be established.
4.5. Conclusion
Sports participation even on competition level before the onset of myocarditis was not associated with a more severe outcome in this retrospective study. There is still a discrepancy between current literature and actual recommendations given by health care providers with regards to the time of rest before return to sports. Before allowing a child or adolescent to start exercising again, normalization of EF and laboratory parameters (troponin, NT pro-BNP), and the exclusion of malignant arrhythmias in Holter Monitoring and/or during cardiopulmonary exercise test, are necessary. However, the necessary examinations for clearing a patient for return to sports are often not undertaken completely.
The level of evidence for establishing recommendation on physical activity after an episode of myocarditis needs to be increased and there is still a discrepancy between current literature and actual recommendations given by health care providers with regards to the time of rest before return to sports.
Data availability statement
If needed the dataset can be made available. Requests to access these datasets should be directed to isabelle.schoeffl@uk-erlangen.de.
Ethics statement
The studies involving human participants were reviewed and approved by Ethikkommission Friedrich-Alexander-Universität Erlangen-Nürnberg and the Ethics Committee of the Charité Berlin, Germany. Written informed consent to participate in this study was provided by the participants’ legal guardian/next of kin.
Author contributions
Conception and design of the study: IS, SH, SD, TP, FS, AW; Data acquisition: IS, SH, TP, BO, MB, BW, KR, GW, TH, MK, DM, SS, FS, AW; Data analysis and interpretation: IS, SH, AW; Drafting of Manuscript: IS; Critical Revision of Manuscript: IS, SH, SD, TP, BO, MB, BW, KR, GW, TH, MK, DM, SS, FS, AW; Accountability for all aspects of work, ensuring integrity and accuracy: IS, SH, SD, TP, BO, MB, BW, KR, GW, TH, MK, DM, SS, FS, AW. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by the German Heart Foundation (September 2013 to June 2021). The pilot phase and scientific planning of the MYKKE registry was supported by two project grants from Deutsche Herzstiftung (Frankfurt am Main, Germany). Since February 2017 MYKKE has been funded by kinderherzen—Fördergemeinschaft Deutsche Kinderherzzentren e.V. (Bonn, Germany). Logistic support and management of the research database are provided by the Competence Network for Congenital Heart Defects (Berlin, Germany), which received funding from the Federal Ministry of Education and Research, grant number 01GI0601 (until 2014), and the DZHK (German Centre for Cardiovascular Research) as of 2015.
Acknowledgments
The authors would like to thank the “MYKKE consortium”. The „MYKKE consortium“ consists of following researchers: Felix Berger (German Heart Center Berlin and Charité—Universitätsmedizin Berlin); Sven-Christian Weber (Charité—Universitätsmedizin Berlin, Berlin); Sabine Klaassen [Charité—Universitätsmedizin Berlin, Berlin; Experimental and Clinical Research Center (ECRC)]; Sabine Schroeter (German Heart Center Berlin); Philipp Beerbaum (Hannover Medical School); Ingo Dähnert and Jacqueline Richter (Heart Centre, University of Leipzig); Sven Dittrich and Joachim Mannert (University Hospital Erlangen); Brigitte Stiller and Nicolas C. Enriquez (University Heart Center Freiburg); Rainer Kozlik-Feldmann, Maria Grafmann and Adriana Busch (University Heart & Vascular Center Hamburg); Michael Hofbeck (University Hospital Tübingen); Tobias Hecht (Heart- and Diabetescenter NRW, Bad Oeynhausen); Hans-Gerd Kehl (University Hospital Münster); Hashim Abdul-Khaliq and Sandra Pontius (Saarland University Medical Center, Homurg); Nikolaus Haas (Ludwig Maximilians University of Munich); Trong Phi Lê and Levent Celik (Klinikum Links der Weser, Bremen); Andrea Engelhardt Andrea Strötges-Achatz and Peter Ewert (German Heart Centre Munich); Konrad Brockmeier and Jennifer Kramp (University Hospital Cologne); Christian Jux and Anna-Eva Blank (University Hospital Giessen); Christian Apitz (University Hospital Ulm); Thomas Paul and Yannic Wilberg (University Medical Center Göttingen); Anselm Uebing (University Hospital Schleswig-Holstein, Kiel); Gunter Kerst and Stefan Ostermayer (University Hospital RWTH Aachen); Caroline von dem Busche and Johannes Breuer (University Hospital Bonn); Frank Uhlemann (Olgahospital, Stuttgart); Matthias Gorenflo (University Hospital Heidelberg; Heidelberg); Ina Michel-Behnke and Annette-Nicole Ivad (Pediatric Heart Center, Medical University Vienna); Matthias Freund (Hospital Oldenburg); Ralph Grabitz and Ia Zakaraia (University Hospital Halle/Saale); Ulrike Bauer (Competence Network for Congenital Heart Defects, Berlin); Walter Knirsch (Pediatric Heart Center, University Children's Hospital, Zurich); Malte Frenzel (University Children's Hospital Basel); Sascha König and Gleb Tarusivov (Heart Center, Duisburg); Cynthia Huber and Tim Friede (Department of Medical Statistics, University Medical Center Göttingen).
Conflict of interest
The reviewer LF declared a shared affiliation with the author(s) IS, SH, SD to the handling editor at the time of review. The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Harmon KG, Asif IM, Maleszewski JJ, Owens DS, Prutkin JM, Salerno JC, et al. Incidence and etiology of sudden cardiac arrest and death in high school athletes in the United States. Mayo Clin Proc. (2016) 91:1493–502. doi: 10.1016/j.mayocp.2016.07.021
2. Peretto G, Sala S, Rizzo S, De Luca G, Campochiaro C, Sartorelli S, et al. Arrhythmias in myocarditis: state of the art. Heart Rhythm. (2019) 16:793–801. doi: 10.1016/j.hrthm.2018.11.024
3. Pollack A, Kontorovich AR, Fuster V, Dec GW. Viral myocarditis–diagnosis, treatment options, and current controversies. Nat Rev Cardiol. (2015) 12:670–80. doi: 10.1038/nrcardio.2015.108
4. Maron BJ, Haas TS, Ahluwalia A, Rutten-Ramos SC. Incidence of cardiovascular sudden deaths in Minnesota high school athletes. Heart Rhythm. (2013) 10:374–7. doi: 10.1016/j.hrthm.2012.11.024
5. Finocchiaro G, Papadakis M, Robertus JL, Dhutia H, Steriotis AK, Tome M, et al. Etiology of sudden death in sports: insights from a United Kingdom regional registry. J Am Coll Cardiol. (2016) 67:2108–15. doi: 10.1016/j.jacc.2016.02.062
6. Winkel BG, Risgaard B, Sadjadieh G, Bundgaard H, Haunso S, Tfelt-Hansen J. Sudden cardiac death in children (1–18 years): symptoms and causes of death in a nationwide setting. Eur Heart J. (2014) 35:868–75. doi: 10.1093/eurheartj/eht509
7. Bohm P, Scharhag J, Meyer T. Data from a nationwide registry on sports-related sudden cardiac deaths in Germany. Eur J Prev Cardiol. (2016) 23:649–56. doi: 10.1177/2047487315594087
8. Morentin B, Suarez-Mier MP, Monzo A, Molina P, Lucena JS. Sports-related sudden cardiac death due to myocardial diseases on a population from 1 to 35 years: a multicentre forensic study in Spain. Forensic Sci Res. (2019) 4:257–66. doi: 10.1080/20961790.2019.1633729
9. Gatmaitan BG, Chason JL, Lerner AM. Augmentation of the virulence of murine coxsackie-virus B-3 myocardiopathy by exercise. J Exp Med. (1970) 131:1121–36. doi: 10.1084/jem.131.6.1121
10. Pelliccia A, Solberg EE, Papadakis M, Adami PE, Biffi A, Caselli S, et al. Recommendations for participation in competitive and leisure time sport in athletes with cardiomyopathies, myocarditis, and pericarditis: position statement of the sport cardiology section of the European association of preventive cardiology (EAPC). Eur Heart J. (2019) 40:19–33. doi: 10.1093/eurheartj/ehy730
11. Schellhorn P. Sport nach myokarditis: eine einzelfallentscheidung. Deutsches Ärzteblatt. (2017) 114:7–11. doi: 10.3238/PersKardio.2017.11.10.02
12. Tomkinson GR, Olds TS. Secular changes in pediatric aerobic fitness test performance: the global picture. Med Sport Sci. (2007) 50:46–66. doi: 10.1159/000101075
13. Martinez-Gomez D, Ortega FB, Ruiz JR, Vicente-Rodriguez G, Veiga OL, Widhalm K, et al. Excessive sedentary time and low cardiorespiratory fitness in European adolescents: the HELENA study. Arch Dis Child. (2011) 96:240–U246. doi: 10.1136/adc.2010.187161
14. Messroghli DR, Pickardt T, Fischer M, Opgen-Rhein B, Papakostas K, Böcker D, et al. Toward evidence-based diagnosis of myocarditis in children and adolescents: rationale, design, and first baseline data of MYKKE, a multicenter registry and study platform. Am Heart J. (2017) 187:133–44. doi: 10.1016/j.ahj.2017.02.027
15. Caforio AL, Pankuweit S, Arbustini E, Basso C, Gimeno-Blanes J, Felix SB, et al. Current state of knowledge on aetiology, diagnosis, management, and therapy of myocarditis: a position statement of the European society of cardiology working group on myocardial and pericardial diseases. Eur Heart J. (2013) 34:2636–48. 2648a–2648d. doi: 10.1093/eurheartj/eht210
16. Metz JP. Upper respiratory tract infections: who plays, who sits? Curr Sports Med Rep. (2003) 2:84–90. doi: 10.1249/00149619-200304000-00007
17. Snyders C, Pyne DB, Sewry N, Hull JH, Kaulback K, Schwellnus M. Acute respiratory illness and return to sport: a systematic review and meta-analysis by a subgroup of the IOC consensus on “acute respiratory illness in the athlete”. Br J Sports Med. (2022) 56:223–31. doi: 10.1136/bjsports-2021-104719
18. Magnani JW, Danik HJ, Dec GW Jr., DiSalvo TG. Survival in biopsy-proven myocarditis: a long-term retrospective analysis of the histopathologic, clinical, and hemodynamic predictors. Am Heart J. (2006) 151:463–70. doi: 10.1016/j.ahj.2005.03.037
19. Mason JW, O'Connell JB, Herskowitz A, Rose NR, McManus BM, Billingham ME, et al. A clinical trial of immunosuppressive therapy for myocarditis. The myocarditis treatment trial investigators. N Engl J Med. (1995) 333:269–75. doi: 10.1056/NEJM199508033330501
20. Sinagra G, Carriere C, Clemenza F, Mina C, Bandera F, Zaffalon D, et al. Risk stratification in cardiomyopathy. Eur J Prev Cardiol. (2020) 27:52–8. doi: 10.1177/2047487320961898
21. Maron BJ, Doerer JJ, Haas TS, Tierney DM, Mueller FO. Sudden deaths in young competitive athletes: analysis of 1866 deaths in the United States, 1980-2006. Circulation. (2009) 119:1085–92. doi: 10.1161/CIRCULATIONAHA.108.804617
22. Albert CM, McGovern BA, Newell JB, Ruskin JN. Sex differences in cardiac arrest survivors. Circulation. (1996) 93:1170–6. doi: 10.1161/01.CIR.93.6.1170
23. Corrado D, Schmied C, Basso C, Borjesson M, Schiavon M, Pelliccia A, et al. Risk of sports: do we need a pre-participation screening for competitive and leisure athletes? Eur Heart J. (2011) 32:934–44. doi: 10.1093/eurheartj/ehq482
24. Dasgupta S, Iannucci G, Mao C, Clabby M, Oster ME. Myocarditis in the pediatric population: a review. Congenit Heart Dis. (2019) 14:868–77. doi: 10.1111/chd.12835
25. Bille K, Figueiras D, Schamasch P, Kappenberger L, Brenner JI, Meijboom FJ, et al. Sudden cardiac death in athletes: the lausanne recommendations. Eur J Cardiovasc Prev Rehabil. (2006) 13:859–75. doi: 10.1097/01.hjr.0000238397.50341.4a
26. Hosenpud JD, Campbell SM, Niles NR, Lee J, Mendelson D, Hart MV. Exercise induced augmentation of cellular and humoral autoimmunity associated with increased cardiac dilatation in experimental autoimmune myocarditis. Cardiovasc Res. (1987) 21:217–22. doi: 10.1093/cvr/21.3.217
27. Scharhag J, Meyer T. Return to play after acute infectious disease in football players. J Sports Sci. (2014) 32:1237–42. doi: 10.1080/02640414.2014.898861
28. Freedman SB, Haladyn JK, Floh A, Kirsh JA, Taylor G, Thull-Freedman J. Pediatric myocarditis: emergency department clinical findings and diagnostic evaluation. Pediatrics. (2007) 120:1278–85. doi: 10.1542/peds.2007-1073
29. Saji T, Matsuura H, Hasegawa K, Nishikawa T, Yamamoto E, Ohki H, et al. Comparison of the clinical presentation, treatment, and outcome of fulminant and acute myocarditis in children. Circ J. (2012) 76:1222–8. doi: 10.1253/circj.CJ-11-1032
30. Vio R, Zorzi A, Corrado D. Myocarditis in the athlete: arrhythmogenic substrates, clinical manifestations, management, and eligibility decisions. J Cardiovasc Transl Res. (2020) 13:284–95. doi: 10.1007/s12265-020-09996-1
31. Ruiz JR, Castro-Pinero J, Artero EG, Ortega FB, Sjostrom M, Suni J, et al. Predictive validity of health-related fitness in youth: a systematic review. Br J Sports Med. (2009) 43:909–23. doi: 10.1136/bjsm.2008.056499
32. Corcioli F, Zakrzewska K, Rinieri A, Fanci R, Innocenti M, Civinini R, et al. Tissue persistence of parvovirus B19 genotypes in asymptomatic persons. J Med Virol. (2008) 80:2005–11. doi: 10.1002/jmv.21289
33. Schenk T, Enders M, Pollak S, Hahn R, Huzly D. High prevalence of human parvovirus B19 DNA in myocardial autopsy samples from subjects without myocarditis or dilative cardiomyopathy. J Clin Microbiol. (2009) 47:106–10. doi: 10.1128/JCM.01672-08
34. Ortega FB, Lavie CJ, Blair SN. Obesity and cardiovascular disease. Circ Res. (2016) 118:1752–70. doi: 10.1161/CIRCRESAHA.115.306883
Keywords: heart muscle infection, return to sports, cardiomyopathy, sudden cardiac death, prevention
Citation: Schöffl I, Holler S, Dittrich S, Pickardt T, Opgen-Rhein B, Boehne M, Wannenmacher B, Reineke K, Wiegand G, Hecht T, Kaestner M, Messroghli D, Schubert S, Seidel F and Weigelt A (2023) Myocarditis and sports in the young: data from a nationwide registry on myocarditis—“MYKKE-Sport”. Front. Sports Act. Living 5:1197640. doi: 10.3389/fspor.2023.1197640
Received: 31 March 2023; Accepted: 12 June 2023;
Published: 26 June 2023.
Edited by:
Andrea Ermolao, Università di Padova, ItalyReviewed by:
Stephan Gerling, University Medical Center Regensburg, GermanyLeonard Fraunberger, Friedrich-Alexander-Universität Erlangen-Nürnberg, Germany
Ferran Gran, Vall d'Hebron University Hospital, Spain
© 2023 Schöffl, Holler, Dittrich, Pickardt, Opgen-Rhein, Boehne, Wannenmacher, Reineke, Wiegand, Hecht, Kaestner, Messroghli, Schubert, Seidel and Weigelt. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Isabelle Schöffl isabelle.schoeffl@uk-erlangen.de
†These authors share senior authorship
 Isabelle Schöffl
Isabelle Schöffl Sophia Holler1
Sophia Holler1  Sven Dittrich
Sven Dittrich Thomas Pickardt
Thomas Pickardt Bernd Opgen-Rhein
Bernd Opgen-Rhein Michael Kaestner
Michael Kaestner Franziska Seidel
Franziska Seidel