Key Points
Local inflammation includes elements — pain and vasodilation — that are neurally mediated.
The systemic acute-phase response includes neurally mediated elements — fever and activation of the central hormonal stress response — that are mediated by the effects of immune factors on the hypothalamus.
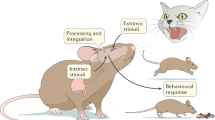
The cellular and molecular components of the innate immune system provide the first line of defence against invading pathogens, through recognition of pathogen-associated molecular patterns (PAMPs) and initial nonspecific cellular and humoral responses. Immune mediators and cytokines that are subsequently released by the innate immune system rapidly activate nonspecific neural responses that both amplify local immune responses to clear pathogens and trigger systemic neuroendocrine and regional neural responses that eventually return the system to a resting state.
These neural responses include systemic hormonal responses (through the hypothalamic–pituitary–adrenal axis); regional neuronal responses (through the sympathetic and parasympathetic nervous systems) that innervate immune organs; and local neuronal responses (through the peripheral nervous system).
Immune cells contain the molecular machinery to respond to neural signals, including receptors and signalling pathways. Neurotransmitters (including noradrenaline and acetylcholine), neuropeptides (including opioids, substance P, neuropeptide Y and calcitonin gene-related peptide and hormones (glucocorticoids) alter innate immune-cell function through these molecular mechanisms.
The nervous system and innate immune system form a cohesive and integrated early host response to pathogens.
This interplay constitutes an important feedback loop that optimizes innate inflammatory responses to invading pathogens. Prolonged or inappropriate central nervous system counter-regulatory responses could predispose the host to excess inflammation (in the context of inadequate hormonal suppression) or uncontrolled infection (in the context of excess or prolonged anti-inflammatory hormonal responses).
Abstract
The central nervous system (CNS) regulates innate immune responses through hormonal and neuronal routes. The neuroendocrine stress response and the sympathetic and parasympathetic nervous systems generally inhibit innate immune responses at systemic and regional levels, whereas the peripheral nervous system tends to amplify local innate immune responses. These systems work together to first activate and amplify local inflammatory responses that contain or eliminate invading pathogens, and subsequently to terminate inflammation and restore host homeostasis. Here, I review these regulatory mechanisms and discuss the evidence indicating that the CNS can be considered as integral to acute-phase inflammatory responses to pathogens as the innate immune system.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Cook, D. N., Pisetsky, D. S. & Schwartz, D. A. Toll-like receptors in the pathogenesis of human disease. Nature Immunol. 5, 975–979 (2004).
Beutler, B. The Toll-like receptors: analysis by forward genetic methods. Immunogenetics 57, 385–392 (2005). A review of landmark studies on TLRs.
Grimm, M. C. et al. Opiate inhibition of chemokine-induced chemotaxis. Ann. N. Y. Acad. Sci. 840, 9–20 (1998).
Milligan, E. D. et al. Controlling neuropathic pain by adeno-associated virus driven production of the anti-inflammatory cytokine, interleukin-10. Mol. Pain 1, 9 (2005).
Watkins, L. R. & Maier, S. F. Implications of immune-to-brain communication for sickness and pain. Proc. Natl Acad. Sci. USA 96, 7710–7713 (1999).
Dhabhar, F. S. Stress-induced enhancement of cell-mediated immunity. Ann. N. Y. Acad. Sci. 840, 359–372 (1998).
Madden, K. S., Felten, S. Y., Felten, D. L., Sundaresan, P. R. & Livnat, S. Sympathetic neural modulation of the immune system. I. Depression of T cell immunity in vivo and vitro following chemical sympathectomy. Brain Behav. Immun. 3, 72–89 (1989).
Amaral, L. A., Diaz-Guilera, A., Moreira, A. A., Goldberger, A. L. & Lipsitz, L. A. Emergence of complex dynamics in a simple model of signalling networks. Proc. Natl Acad. Sci. USA 101, 15551–15555 (2004).
Kawashima, K. & Fujii, T. Expression of non-neuronal acetylcholine in lymphocytes and its contribution to the regulation of immune function. Front. Biosci. 9, 2063–2085 (2004). A comprehensive review of non-neuronal cholinergic regulation of immunity.
Maestroni, G. J. & Mazzola, P. Langerhans cells β2-adrenoceptors: role in migration, cytokine production, Th priming and contact hypersensitivity. J. Neuroimmunol. 144, 91–99 (2003).
Woltman, A. M., Massacrier, C., de Fijter, J. W., Caux, C. & van Kooten, C. Corticosteroids prevent generation of CD34+-derived dermal dendritic cells but do not inhibit Langerhans cell development. J. Immunol. 168, 6181–6188 (2002).
Chakravarty, S. & Herkenham, M. Toll-like receptor 4 on nonhematopoietic cells sustains CNS inflammation during endotoxemia, independent of systemic cytokines. J. Neurosci. 25, 1788–1796 (2005).
Olson, J. K. & Miller, S. D. Microglia initiate central nervous system innate and adaptive immune responses through multiple TLRs. J. Immunol. 173, 3916–3924 (2004).
Koedel, U. et al. MyD88 is required for mounting a robust host immune response to Streptococcus pneumoniae in the CNS. Brain 127, 1437–1445 (2004).
Hench, P. S., Kendall, E. C., Slocumb, C. H. & Polley, H. F. Effects of cortisone acetate and pituitary ACTH on rheumatoid arthritis, rheumatic fever and certain other conditions. Arch. Med. Interna 85, 545–666 (1950).
Agarwal, S. K. & Marshall, G. D. Jr. Dexamethasone promotes type 2 cytokine production primarily through inhibition of type 1 cytokines. J. Interferon Cytokine Res. 21, 147–155 (2001).
Wick, G. et al. The obese strain of chickens: an animal model with spontaneous autoimmune thyroiditis. Adv. Immunol. 47, 433–500 (1989).
Sternberg, E. M. et al. A central nervous system defect in biosynthesis of corticotropin-releasing hormone is associated with susceptibility to streptococcal cell wall-induced arthritis in Lewis rats. Proc. Natl Acad. Sci. USA 86, 4771–4775 (1989).
Crofford, L. J. et al. Hypothalamic-pituitary-adrenal axis perturbations in patients with fibromyalgia. Arthritis Rheum. 37, 1583–1592 (1994).
Johnson, E. O., Vlachoyiannopoulos, P. G., Skopouli, F. N., Tzioufas, A. G. & Moutsopoulos, H. M. Hypofunction of the stress axis in Sjogren's syndrome. J. Rheumatol. 25, 1508–1514 (1998).
Sternberg, E. M. et al. Inflammatory mediator-induced hypothalamic-pituitary-adrenal axis activation is defective in streptococcal cell wall arthritis-susceptible Lewis rats. Proc. Natl Acad. Sci. USA 86, 2374–2378 (1989).
Edwards, C. K., Yunger, L. M., Lorence, R. M., Dantzer, R. & Kelley, K. W. The pituitary gland is required for protection against lethal effects of Salmonella typhimurium. Proc. Natl Acad. Sci. USA 88, 2274–2277 (1991).
Ruzek, M. C., Pearce, B. D., Miller, A. H. & Biron, C. A. Endogenous glucocorticoids protect against cytokine-mediated lethality during viral infection. J. Immunol. 162, 3527–3533 (1999).
Gomez, S. A. et al. Endogenous glucocorticoids attenuate Shiga toxin-2-induced toxicity in a mouse model of haemolytic uraemic syndrome. Clin. Exp. Immunol. 131, 217–224 (2003).
MacPhee, I. A., Antoni, F. A. & Mason, D. W. Spontaneous recovery of rats from experimental allergic encephalomyelitis is dependent on regulation of the immune system by endogenous adrenal corticosteroids. J. Exp. Med. 169, 431–445 (1989).
Derijk, R. H. et al. A human glucocorticoid receptor gene variant that increases the stability of the glucocorticoid receptor β-isoform mRNA is associated with rheumatoid arthritis. J. Rheumatol. 28, 2383–2388 (2001).
Leung, D. Y. & Szefler, S. J. Diagnosis and management of steroid-resistant asthma. Clin. Chest Med. 18, 611–625 (1997).
Adcock, I. M. et al. Differences in binding of glucocorticoid receptor to DNA in steroid-resistant asthma. J. Immunol. 154, 3500–3505 (1995).
DeRijk, R. H., Eskandari, F. & Sternberg, E. M. Corticosteroid resistance in a subpopulation of multiple sclerosis patients as measured by ex vivo dexamethasone inhibition of LPS induced IL-6 production. J. Neuroimmunol. 151, 180–188 (2004).
van Winsen, L. M. et al. Sensitivity to glucocorticoids is decreased in relapsing remitting multiple sclerosis. J. Clin. Endocrinol. Metab. 90, 734–740 (2005).
Towers, R. et al. High levels of glucocorticoid receptors in patients with active Crohn's disease may predict steroid resistance. Clin. Exp. Immunol. 141, 357–362 (2005).
Ogawa, S. et al. Molecular determinants of crosstalk between nuclear receptors and Toll-like receptors. Cell 122, 707–721 (2005). This study defines nuclear receptor–TLR interactions and clinical implications for glucocorticoid effects in different infections.
Lee, Y. M. et al. A mutation of the glucocorticoid receptor gene in patients with systemic lupus erythematosus. Tohoku J. Exp. Med. 203, 69–76 (2004).
Jiang, T. et al. The phase-shift mutation in the glucocorticoid receptor gene: potential etiologic significance of neuroendocrine mechanisms in lupus nephritis. Clin. Chim. Acta 313, 113–117 (2001).
Mingrone, G. et al. The steroid resistance of Crohn's disease. J. Investig. Med. 47, 319–325 (1999).
Diaz-Borjon, A. et al. Multidrug resistance-1 (MDR-1) in rheumatic autoimmune disorders. Part II: Increased P-glycoprotein activity in lymphocytes from systemic lupus erythematosus patients might affect steroid requirements for disease control. Joint Bone Spine 67, 40–48 (2000).
DeRijk, R. H., Schaaf, M. & de Kloet, E. R. Glucocorticoid receptor variants: clinical implications. J. Steroid Biochem. Mol. Biol. 81, 103–122 (2002). A recent review describing the concept and clinical implications of glucocorticoid resistance.
Oakley, R. H., Sar, M. & Cidlowski, J. A. The human glucocorticoid receptor β isoform. Expression, biochemical properties, and putative function. J. Biol. Chem. 271, 9550–9559 (1996). An interesting study describing the expression, biochemical properties, and function of the glucocorticoid receptor-β in humans.
Leung, D. Y. et al. Association of glucocorticoid insensitivity with increased expression of glucocorticoid receptor β. J. Exp. Med. 186, 1567–1574 (1997).
Webster, J. I. et al. Anthrax lethal factor represses glucocorticoid and progesterone receptor activity. Proc. Natl Acad. Sci. USA 100, 5706–5711 (2003). The first report of bacterial toxin repressing nuclear hormone receptor transactivation.
Moayeri, M., Webster, J. I., Wiggins, J. F., Leppla, S. H. & Sternberg, E. M. Endocrine perturbation increases susceptibility of mice to anthrax lethal toxin. Infect. Immun. 73, 4238–4244 (2005).
Glaser, R. & Kiecolt-Glaser, J. K. Stress-induced immune dysfunction: implications for health. Nature Rev. Immunol. 5, 243–251 (2005). A comprehensive review of mechanisms of stress effects on immunity.
Vedhara, K. et al. Chronic stress in elderly carers of dementia patients and antibody response to influenza vaccination. Lancet 353, 627–631 (1999).
DeRijk, R. et al. Exercise and circadian rhythm-induced variations in plasma cortisol differentially regulate interleukin-1 β (IL-1 β), IL-6, and tumour necrosis factor-α (TNF α) production in humans: high sensitivity of TNFα and resistance of IL-6. J. Clin. Endocrinol. Metab. 82, 2182–2191 (1997).
Singh, A. et al. Lymphocyte subset responses to exercise and glucocorticoid suppression in healthy men. Med. Sci. Sports Exerc. 28, 822–828 (1996).
Matyszak, M. K., Citterio, S., Rescigno, M. & Ricciardi-Castagnoli, P. Differential effects of corticosteroids during different stages of dendritic cell maturation. Eur. J. Immunol. 30, 1233–1242 (2000).
Moser, M. et al. Glucocorticoids downregulate dendritic cell function in vitro and in vivo. Eur. J. Immunol. 25, 2818–2824 (1995).
Sacedon, R., Vicente, A., Varas, A., Jimenez, E. & Zapata, A. G. Early differentiation of thymic dendritic cells in the absence of glucocorticoids. J. Neuroimmunol. 94, 103–108 (1999).
Ma, W. et al. Dexamethasone inhibits IL-12p40 production in lipopolysaccharide-stimulated human monocytic cells by downregulating the activity of c-Jun N-terminal kinase, the activation protein-1, and NF-κB transcription factors. J. Immunol. 172, 318–330 (2004).
Murray, S. E. et al. Overproduction of corticotropin-releasing hormone blocks germinal center formation: role of corticosterone and impaired follicular dendritic cell networks. J. Neuroimmunol. 156, 31–41 (2004).
Ghosh, S., May, M. J. & Kopp, E. B. NF-κB and Rel proteins: evolutionarily conserved mediators of immune responses. Annu. Rev. Immunol. 16, 225–260 (1998).
Scheinman, R. I., Gualberto, A., Jewell, C. M., Cidlowski, J. A. & Baldwin, A. S. Jr. Characterization of mechanisms involved in transrepression of NF-κ B by activated glucocorticoid receptors. Mol. Cell. Biol. 15, 943–953 (1995).
Cronstein, B. N., Kimmel, S. C., Levin, R. I., Martiniuk, F. & Weissmann, G. A mechanism for the antiinflammatory effects of corticosteroids: the glucocorticoid receptor regulates leukocyte adhesion to endothelial cells and expression of endothelial-leukocyte adhesion molecule 1 and intercellular adhesion molecule 1. Proc. Natl Acad. Sci. USA 89, 9991–9995 (1992).
Atsuta, J., Plitt, J., Bochner, B. S. & Schleimer, R. P. Inhibition of VCAM-1 expression in human bronchial epithelial cells by glucocorticoids. Am. J. Respir. Cell Mol. Biol. 20, 643–650 (1999).
Pitzalis, C. et al. Corticosteroids inhibit lymphocyte binding to endothelium and intercellular adhesion: an additional mechanism for their anti-inflammatory and immunosuppressive effect. J. Immunol. 158, 5007–5016 (1997).
Miyamasu, M. et al. Glucocorticoids inhibit chemokine generation by human eosinophils. J. Allergy Clin. Immunol. 101, 75–83 (1998).
Sewell, W. A., Scurr, L. L., Orphanides, H., Kinder, S. & Ludowyke, R. I. Induction of interleukin-4 and interleukin-5 expression in mast cells is inhibited by glucocorticoids. Clin. Diagn. Lab. Immunol. 5, 18–23 (1998).
Richards, D. F., Fernandez, M., Caulfield, J. & Hawrylowicz, C. M. Glucocorticoids drive human CD8+T cell differentiation towards a phenotype with high IL-10 and reduced IL-4, IL-5 and IL-13 production. Eur. J. Immunol. 30, 2344–2354 (2000).
Pype, J. L. et al. Expression of monocyte chemotactic protein (MCP)-1, MCP-2, and MCP-3 by human airway smooth-muscle cells. Modulation by corticosteroids and T-helper 2 cytokines. Am. J. Respir. Cell Mol. Biol. 21, 528–536 (1999).
Homma, T. et al. Corticosteroid and cytokines synergistically enhance Toll-like receptor 2 expression in respiratory epithelial cells. Am. J. Respir. Cell Mol. Biol. 31, 463–469 (2004).
Hermoso, M. A., Matsuguchi, T., Smoak, K. & Cidlowski, J. A. Glucocorticoids and tumour necrosis factor α cooperatively regulate Toll-like receptor 2 gene expression. Mol. Cell Biol. 24, 4743–4756 (2004).
Shuto, T. et al. Glucocorticoids synergistically enhance nontypeable Haemophilus influenzae-induced Toll-like receptor 2 expression via a negative cross-talk with p38 MAP kinase. J. Biol. Chem. 277, 17263–17270 (2002).
Bornstein, S. R. et al. Impaired adrenal stress response in Toll-like receptor 2-deficient mice. Proc. Natl Acad. Sci. USA 101, 16695–16700 (2004). This paper provides evidence for a crucial role of TLR2 in adrenal glucocorticoid regulation in septicaemia.
Takeuchi, O., Hoshino, K. & Akira, S. Cutting edge: TLR2-deficient and MyD88-deficient mice are highly susceptible to Staphylococcus aureus infection. J. Immunol. 165, 5392–5396 (2000).
Drennan, M. B. et al. Toll-like receptor 2-deficient mice succumb to Mycobacterium tuberculosis infection. Am. J. Pathol. 164, 49–57 (2004).
Silverman, M. N., Miller, A. H., Biron, C. A. & Pearce, B. D. Characterization of an interleukin-6- and adrenocorticotropin-dependent, immune-to-adrenal pathway during viral infection. Endocrinology 145, 3580–3589 (2004).
Sanders, V. M. Interdisciplinary research: noradrenergic regulation of adaptive immunity. Brain Behav. Immun. 11 Oct 2005 (doi: 10.1016/j.bbi.2005.08.005).
Johnson, J. D. et al. Adrenergic receptors mediate stress-induced elevations in extracellular Hsp72. J. Appl. Physiol. 99, 1789–1795 (2005).
Madden, K. S., Sanders, V. M. & Felten, D. L. Catecholamine influences and sympathetic neural modulation of immune responsiveness. Annu. Rev. Pharmacol. Toxicol. 35, 417–448 (1995).
Benschop, R. J. et al. Effects of β-adrenergic blockade on immunologic and cardiovascular changes induced by mental stress. Circulation 89, 762–769 (1994).
Chelmicka-Schorr, E., Checinski, M. & Arnason, B. G. Chemical sympathectomy augments the severity of experimental allergic encephalomyelitis. J. Neuroimmunol. 17, 347–350 (1988).
van der Poll, T., Jansen, J., Endert, E., Sauerwein, H. P. & van Deventer, S. J. Noradrenaline inhibits lipopolysaccharide-induced tumour necrosis factor and interleukin 6 production in human whole blood. Infect. Immun. 62, 2046–2050 (1994).
Hasko, G., Elenkov, I. J., Kvetan, V. & Vizi, E. S. Differential effect of selective block of α 2-adrenoreceptors on plasma levels of tumour necrosis factor-α, interleukin-6 and corticosterone induced by bacterial lipopolysaccharide in mice. J. Endocrinol. 144, 457–462 (1995).
Woiciechowsky, C. et al. Sympathetic activation triggers systemic interleukin-10 release in immunodepression induced by brain injury. Nature Med. 4, 808–813 (1998).
Lang, K., Drell, T. L., Niggemann, B., Zanker, K. S. & Entschladen, F. Neurotransmitters regulate the migration and cytotoxicity in natural killer cells. Immunol. Lett. 90, 165–172 (2003).
Straub, R. H. et al. Neurotransmitters of the sympathetic nerve terminal are powerful chemoattractants for monocytes. J. Leukoc. Biol. 67, 553–558 (2000).
Schwarz, H., Villiger, P. M., von Kempis, J. & Lotz, M. Neuropeptide Y is an inducible gene in the human immune system. J. Neuroimmunol. 51, 53–61 (1994).
Larhammar, D. Structural diversity of receptors for neuropeptide Y, peptide YY and pancreatic polypeptide. Regul. Pept. 65, 165–174 (1996).
Straub, R. H. et al. Neuropeptide Y cotransmission with noradrenaline in the sympathetic nerve-macrophage interplay. J. Neurochem. 75, 2464–2471 (2000).
Jetschmann, J. U. et al. Expression and in-vivo modulation of α- and β-adrenoceptors on human natural killer (CD16+) cells. J. Neuroimmunol. 74, 159–164 (1997).
Oberbeck, R. et al. Adrenergic modulation of survival and cellular immune functions during polymicrobial sepsis. Neuroimmunomodulation 11, 214–223 (2004).
Papanicolaou, D. A., Tsigos, C., Oldfield, E. H. & Chrousos, G. P. Acute glucocorticoid deficiency is associated with plasma elevations of interleukin-6: does the latter participate in the symptomatology of the steroid withdrawal syndrome and adrenal insufficiency? J. Clin. Endocrinol. Metab. 81, 2303–2306 (1996).
Metz-Boutigue, M. H., Kieffer, A. E., Goumon, Y. & Aunis, D. Innate immunity: involvement of new neuropeptides. Trends Microbiol. 11, 585–592 (2003).
Tracey, K. J. The inflammatory reflex. Nature 420, 853–859 (2002). A review of antifungal and antibacterial properties of some adrenal peptides.
Laye, S. et al. Subdiaphragmatic vagotomy blocks induction of IL-1 β mRNA in mice brain in response to peripheral LPS. Am. J. Physiol. 268, R1327–R1331 (1995).
Wang, H. et al. Nicotinic acetylcholine receptor α7 subunit is an essential regulator of inflammation. Nature 421, 384–388 (2003). This paper provides evidence for a role for nicotinic acetylcholine receptor in regulating inflammation.
de Jonge, W. J. et al. Stimulation of the vagus nerve attenuates macrophage activation by activating the Jak2-STAT3 signalling pathway. Nature Immunol. 6, 844–851 (2005). The mechanism of action of non-pharmacological cholinergic anti-inflammatory intervention (vagus nerve stimulation) is described.
Czura, C. J. & Tracey, K. J. Autonomic neural regulation of immunity. J. Intern. Med. 257, 156–166 (2005).
van Westerloo, D. J. et al. The cholinergic anti-inflammatory pathway regulates the host response during septic peritonitis. J. Infect. Dis. 191, 2138–2148 (2005).
Borovikova, L. V. et al. Vagus nerve stimulation attenuates the systemic inflammatory response to endotoxin. Nature 405, 458–462 (2000).
Yang, H. et al. Reversing established sepsis with antagonists of endogenous high-mobility group box 1. Proc. Natl Acad. Sci. USA 101, 296–301 (2004).
Chen, G. et al. Suppression of HMGB1 release by stearoyl lysophosphatidylcholine:an additional mechanism for its therapeutic effects in experimental sepsis. J. Lipid Res. 46, 623–627 (2005).
Lotze, M. T. & Tracey, K. J. High-mobility group box 1 protein (HMGB1): nuclear weapon in the immune arsenal. Nature Rev. Immunol. 5, 331–342 (2005).
Reyes-Reyna, S., Stegall, T. & Krolick, K. A. Muscle responds to an antibody reactive with the acetylcholine receptor by upregulating monocyte chemoattractant protein 1: a chemokine with the potential to influence the severity and course of experimental myasthenia gravis. J. Immunol. 169, 1579–1586 (2002).
Saeed, R. W. et al. Cholinergic stimulation blocks endothelial cell activation and leukocyte recruitment during inflammation. J. Exp. Med. 201, 1113–1123 (2005).
Bulloch, K. et al. Induction of calcitonin gene-related peptide-like immunoreactivity in hippocampal neurons following ischemia: a putative regional modulator of the CNS injury/immune response. Exp. Neurol. 150, 195–205 (1998).
Agelaki, S., Tsatsanis, C., Gravanis, A. & Margioris, A. N. Corticotropin-releasing hormone augments proinflammatory cytokine production from macrophages in vitro and in lipopolysaccharide-induced endotoxin shock in mice. Infect. Immun. 70, 6068–6074 (2002).
Cuesta, M. C., Quintero, L., Pons, H. & Suarez-Roca, H. Substance P and calcitonin gene-related peptide increase IL-1β, IL-6 and TNFα secretion from human peripheral blood mononuclear cells. Neurochem. Int. 40, 301–306 (2002).
Green, P. G., Luo, J., Heller, P. H. & Levine, J. D. Further substantiation of a significant role for the sympathetic nervous system in inflammation. Neuroscience 55, 1037–1043 (1993).
Baker, C., Richards, L. J., Dayan, C. M. & Jessop, D. S. Corticotropin-releasing hormone immunoreactivity in human T and B cells and macrophages: co-localization with arginine vasopressin. J. Neuroendocrinol. 15, 1070–1074 (2003).
Webster, E. L. et al. In vivo and in vitro characterization of antalarmin, a nonpeptide corticotropin-releasing hormone (CRH) receptor antagonist: suppression of pituitary ACTH release and peripheral inflammation. Endocrinology 137, 5747–5750 (1996).
Brain, S. D. & Grant, A. D. Vascular actions of calcitonin gene-related peptide and adrenomedullin. Physiol. Rev. 84, 903–934 (2004).
Carucci, J. A. et al. Calcitonin gene-related peptide decreases expression of HLA-DR and CD86 by human dendritic cells and dampens dendritic cell-driven T cell-proliferative responses via the type I calcitonin gene-related peptide receptor. J. Immunol. 164, 3494–3499 (2000).
Tran, M. T., Ritchie, M. H., Lausch, R. N. & Oakes, J. E. Calcitonin gene-related peptide induces IL-8 synthesis in human corneal epithelial cells. J. Immunol. 164, 4307–4312 (2000).
Park, S. H., Hsiao, G. Y. & Huang, G. T. Role of substance P and calcitonin gene-related peptide in the regulation of interleukin-8 and monocyte chemotactic protein-1 expression in human dental pulp. Int. Endod. J. 37, 185–192 (2004).
Millet, I. et al. Inhibition of NF-κB activity and enhancement of apoptosis by the neuropeptide calcitonin gene-related peptide. J. Biol. Chem. 275, 15114–15121 (2000).
Mapp, C. E. et al. The distribution of neurokinin-1 and neurokinin-2 receptors in human central airways. Am. J. Respir. Crit. Care Med. 161, 207–215 (2000).
Lotz, M., Vaughan, J. H. & Carson, D. A. Effect of neuropeptides on production of inflammatory cytokines by human monocytes. Science 241, 1218–1221 (1988).
Croitoru, K., Ernst, P. B., Bienenstock, J., Padol, I. & Stanisz, A. M. Selective modulation of the natural killer activity of murine intestinal intraepithelial leucocytes by the neuropeptide substance P. Immunology 71, 196–201 (1990).
Feistritzer, C. et al. Natural killer cell functions mediated by the neuropeptide substance P. Regul. Pept. 116, 119–126 (2003).
Serra, M. C., Calzetti, F., Ceska, M. & Cassatella, M. A. Effect of substance P on superoxide anion and IL-8 production by human PMNL. Immunology 82, 63–69 (1994).
Guhl, S., Lee, H. H., Babina, M., Henz, B. M. & Zuberbier, T. Evidence for a restricted rather than generalized stimulatory response of skin-derived human mast cells to substance P. J. Neuroimmunol. 163, 92–101 (2005).
Wang, L., Stanisz, A. M., Wershil, B. K., Galli, S. J. & Perdue, M. H. Substance P induces ion secretion in mouse small intestine through effects on enteric nerves and mast cells. Am. J. Physiol. 269, G85–G92 (1995).
Helme, R. D., Eglezos, A. & Andrews, P. V. The effects of capsaicin denervation on leucocyte and complement components of the inflammatory response. Clin. Exp. Neurol. 24, 207–211 (1987).
Duffy, R. A. Potential therapeutic targets for neurokinin-1 receptor antagonists. Expert Opin. Emerg. Drugs 9, 9–21 (2004).
Kawasaki, H., Nuki, C., Saito, A. & Takasaki, K. Adrenergic modulation of calcitonin gene-related peptide (CGRP)-containing nerve-mediated vasodilation in the rat mesenteric resistance vessel. Brain Res. 506, 287–290 (1990).
Lee, T. H., Lerner, A. B. & Buettner-Janusch, V. The isolation and structure of α- and β-melanocyte-stimulating hormones from monkey pituitary glands. J. Biol. Chem. 236, 1390–1394 (1961).
Roselli-Rehfuss, L. et al. Identification of a receptor for γ melanotropin and other proopiomelanocortin peptides in the hypothalamus and limbic system. Proc. Natl Acad. Sci. USA 90, 8856–8860 (1993).
Lipton, J. M. & Catania, A. Anti-inflammatory actions of the neuroimmunomodulator α-MSH. Immunol. Today 18, 140–145 (1997).
Taylor, A. W. The immunomodulating neuropeptide α-melanocyte-stimulating hormone (α-MSH) suppresses LPS-stimulated TLR4 with IRAK-M in macrophages. J. Neuroimmunol. 162, 43–50 (2005).
Mandrika, I., Muceniece, R. & Wikberg, J. E. Effects of melanocortin peptides on lipopolysaccharide/interferon-γ-induced NF-κB DNA binding and nitric oxide production in macrophage-like RAW 264.7 cells: evidence for dual mechanisms of action. Biochem. Pharmacol. 61, 613–621 (2001).
Kiss, M. et al. Effects of the neuropeptides substance P, calcitonin gene-related peptide and α-melanocyte-stimulating hormone on the IL-8/IL-8 receptor system in a cultured human keratinocyte cell line and dermal fibroblasts. Inflammation 23, 557–567 (1999).
van Epps, D. E. & Saland, L. β-endorphin and met-enkephalin stimulate human peripheral blood mononuclear cell chemotaxis. J. Immunol. 132, 3046–3053 (1984).
Zhang, N., Hodge, D., Rogers, T. J. & Oppenheim, J. J. Ca2+-independent protein kinase Cs mediate heterologous desensitization of leukocyte chemokine receptors by opioid receptors. J. Biol. Chem. 278, 12729–12736 (2003). Evidence for crosstalk between opioid receptors and chemokine receptors that are potentially relevant to pain mechanisms and therapy.
Bidlack, J. M. Detection and function of opioid receptors on cells from the immune system. Clin. Diagn. Lab. Immunol. 7, 719–723 (2000).
Mellon, R. D. & Bayer, B. M. The effects of morphine, nicotine and epibatidine on lymphocyte activity and hypothalamic-pituitary-adrenal axis responses. J. Pharmacol. Exp. Ther. 288, 635–642 (1999).
Blondel, O. et al. A glia-derived signal regulating neuronal differentiation. J. Neurosci. 20, 8012–8020 (2000).
Hernanz, A., Tato, E., De la Fuente, M., de Miguel, E. & Arnalich, F. Differential effects of gastrin-releasing peptide, neuropeptide Y, somatostatin and vasoactive intestinal peptide on interleukin-1 β, interleukin-6 and tumour necrosis factor-α production by whole blood cells from healthy young and old subjects. J. Neuroimmunol. 71, 25–30 (1996).
Martinez, C. et al. Vasoactive intestinal peptide and pituitary adenylate cyclase-activating polypeptide modulate endotoxin-induced IL-6 production by murine peritoneal macrophages. J. Leukoc. Biol. 63, 591–601 (1998).
Delgado, M., Munoz-Elias, E. J., Gomariz, R. P. & Ganea, D. Vasoactive intestinal peptide and pituitary adenylate cyclase-activating polypeptide enhance IL-10 production by murine macrophages: in vitro and in vivo studies. J. Immunol. 162, 1707–1716 (1999).
Ganea, D. Regulatory effects of vasoactive intestinal peptide on cytokine production in central and peripheral lymphoid organs. Adv. Neuroimmunol. 6, 61–74 (1996).
Delgado, M. & Ganea, D. Vasoactive intestinal peptide inhibits IL-8 production in human monocytes. Biochem. Biophys. Res. Commun. 301, 825–832 (2003).
Delneste, Y. et al. Vasoactive intestinal peptide synergizes with TNF-α in inducing human dendritic cell maturation. J. Immunol. 163, 3071–3075 (1999).
Gomariz, R. P. et al. Time-course expression of Toll-like receptors 2 and 4 in inflammatory bowel disease and homeostatic effect of VIP. J. Leukoc. Biol. 78, 491–502 (2005).
Delgado, M., Pozo, D. & Ganea, D. The significance of vasoactive intestinal peptide in immunomodulation. Pharmacol. Rev. 56, 249–290 (2004).
Webster, J. I., Tonelli, L. & Sternberg, E. M. Neuroendocrine regulation of immunity. Annu. Rev. Immunol. 20, 125–163 (2002).
Steinman, L. Elaborate interactions between the immune and nervous systems. Nature Immunol. 5, 575–581 (2004).
Kobilka, B. K. et al. cDNA for the human β2-adrenergic receptor: a protein with multiple membrane-spanning domains and encoded by a gene whose chromosomal location is shared with that of the receptor for platelet-derived growth factor. Proc. Natl Acad. Sci. USA 84, 46–50 (1987).
Le Tulzo, Y. et al. Hemorrhage increases cytokine expression in lung mononuclear cells in mice: involvement of catecholamines in nuclear factor-κB regulation and cytokine expression. J. Clin. Invest. 99, 1516–1524 (1997).
Marques-Deak, A., Cizza, G. & Sternberg, E. Brain-immune interactions and disease susceptibility. Mol. Psychiatry 10, 239–250 (2005).
Acknowledgements
The author would like to thank H. Gorby and C. Butts for their important contributions to this manuscript.
Author information
Authors and Affiliations
Ethics declarations
Competing interests
The author declares no competing financial interests.
Related links
Glossary
- G-protein-coupled receptors
-
Cell-surface receptors that are coupled to G-proteins, and have seven transmembrane-spanning domains. The acetylcholine, adrenergic and neuropeptide receptors are all members of this family. Typically, activation of the G-protein-coupled receptor produces a diffusible second messenger that, in turn, triggers various biochemical cascades.
- Sympathetic nervous system
-
(SNS). A division of the autonomic nervous system that consists of fibres projecting from the central nervous system, through ganglia near the spinal cord, to innervate organs such as the heart, lungs, intestine, blood vessels and sweat glands. In general, sympathetic nerves dilate the pupils, constrict peripheral blood vessels and increase heart rate.
- Parasympathetic nervous system
-
A division of the autonomic nervous system that consists of nerve fibres projecting from the central nervous system and sacral portion of the spinal cord, which extend to nerve-cell clusters (ganglia) at specific sites, from which fibres are distributed to blood vessels, glands and other internal organs. Functions of parasympathetic nerves include slowing the heart rate; inducing the secretion of bile, insulin and digestive juices; dilating peripheral blood vessels; and contracting the bronchioles, pupils and oesophagus.
- Delayed-type hypersensitivity
-
A cellular immune response to antigen that develops over 24–72 hours with the infiltration of T cells and monocytes, and depends on the production of T helper 1-cell-specific cytokines.
- Noradrenaline
-
The primary neurotransmitter of the sympathetic nervous system. It is a biogenic amine derived from tyrosine and its metabolite dopamine, which is converted to noradrenaline by the enzyme β-hydroxylase.
- Adrenaline
-
A neurotransmitter of the sympathetic nervous system. It is a biogenic amine derived from tyrosine and its metabolite dopamine, which is converted to adrenaline from noradrenaline by the enzyme phenylethanolamine-N-methyl transferase.
- Vagus nerve
-
The main nerve trunk of the parasympathetic nervous system. It contains both afferent fibres that carry signals from the periphery to the brain, and efferent fibres that carry signals from the brain to the peripheral organs that it innervates.
- Pro-opiomelanocortin
-
(POMC). A 241-amino-acid precursor polypeptide that is synthesized in corticotrophin cells of the pituitary gland. Biologically active peptides derived from POMC include adrenocorticotropic hormone, enkephalins and α-melanocyte-stimulating hormone.
- Arcuate nucleus
-
A collection of neurons in the hypothalamus. It regulates the secretion of hormones through afferent dopaminergic projections to the pituitary.
- Paraventricular nucleus
-
(PVN). A collection of neurons in the hypothalamus that are adjacent to the third ventricle. It contains mainly neurosecretory neurons that secrete corticotrophin-releasing hormone, which stimulates pituitary corticotrophs. In addition, PVN neurons project to the sympathetic brainstem nuclei, parasympathetic brainstem pre-ganglionic neurons and spinal cord.
- Endorphins
-
Endogenous opioid peptides that are produced by the pituitary gland and the hypothalamus. They regulate feelings of pain and hunger.
- Enkephalins
-
Short five-amino-acid polypeptides that are members of endogenous opioid family and that bind to opiate receptors.
Rights and permissions
About this article
Cite this article
Sternberg, E. Neural regulation of innate immunity: a coordinated nonspecific host response to pathogens. Nat Rev Immunol 6, 318–328 (2006). https://doi.org/10.1038/nri1810
Issue Date:
DOI: https://doi.org/10.1038/nri1810
This article is cited by
Pathophysiology of acute lung injury in patients with acute brain injury: the triple-hit hypothesis
Critical Care (2024)
Whole blood stimulation provides preliminary evidence of altered immune function following SRC
BMC Immunology (2024)
Fasting-activated ventrolateral medulla neurons regulate T cell homing and suppress autoimmune disease in mice
Nature Neuroscience (2024)
Fibroblastic reticular cells in lymph node potentiate white adipose tissue beiging through neuro-immune crosstalk in male mice
Nature Communications (2023)
Central role for neurally dysregulated IL-17A in dynamic networks of systemic and local inflammation in combat casualties
Scientific Reports (2023)