Efficacy and Safety of the mRNA-1273 SARS-CoV-2 Vaccine
Abstract
Background
Vaccines are needed to prevent coronavirus disease 2019 (Covid-19) and to protect persons who are at high risk for complications. The mRNA-1273 vaccine is a lipid nanoparticle–encapsulated mRNA-based vaccine that encodes the prefusion stabilized full-length spike protein of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the virus that causes Covid-19.
Methods
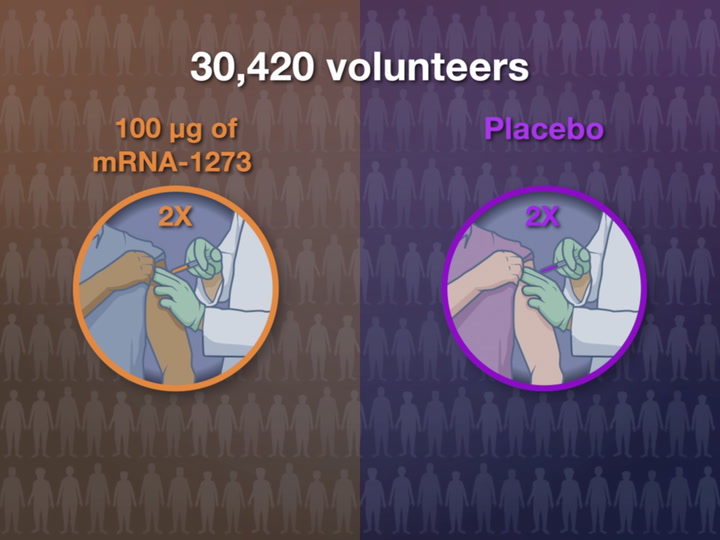
This phase 3 randomized, observer-blinded, placebo-controlled trial was conducted at 99 centers across the United States. Persons at high risk for SARS-CoV-2 infection or its complications were randomly assigned in a 1:1 ratio to receive two intramuscular injections of mRNA-1273 (100 μg) or placebo 28 days apart. The primary end point was prevention of Covid-19 illness with onset at least 14 days after the second injection in participants who had not previously been infected with SARS-CoV-2.

Results
The trial enrolled 30,420 volunteers who were randomly assigned in a 1:1 ratio to receive either vaccine or placebo (15,210 participants in each group). More than 96% of participants received both injections, and 2.2% had evidence (serologic, virologic, or both) of SARS-CoV-2 infection at baseline. Symptomatic Covid-19 illness was confirmed in 185 participants in the placebo group (56.5 per 1000 person-years; 95% confidence interval [CI], 48.7 to 65.3) and in 11 participants in the mRNA-1273 group (3.3 per 1000 person-years; 95% CI, 1.7 to 6.0); vaccine efficacy was 94.1% (95% CI, 89.3 to 96.8%; P<0.001). Efficacy was similar across key secondary analyses, including assessment 14 days after the first dose, analyses that included participants who had evidence of SARS-CoV-2 infection at baseline, and analyses in participants 65 years of age or older. Severe Covid-19 occurred in 30 participants, with one fatality; all 30 were in the placebo group. Moderate, transient reactogenicity after vaccination occurred more frequently in the mRNA-1273 group. Serious adverse events were rare, and the incidence was similar in the two groups.
Conclusions
The mRNA-1273 vaccine showed 94.1% efficacy at preventing Covid-19 illness, including severe disease. Aside from transient local and systemic reactions, no safety concerns were identified. (Funded by the Biomedical Advanced Research and Development Authority and the National Institute of Allergy and Infectious Diseases; COVE ClinicalTrials.gov number, NCT04470427.)
The emergence in December 2019 of a novel coronavirus, the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), has had devastating consequences globally. Control measures such as the use of masks, physical distancing, testing of exposed or symptomatic persons, contact tracing, and isolation have helped limit the transmission where they have been rigorously applied; however, these actions have been variably implemented and have proved insufficient in impeding the spread of coronavirus disease 2019 (Covid-19), the disease caused by SARS-CoV-2. Vaccines are needed to reduce the morbidity and mortality associated with Covid-19, and multiple platforms have been involved in the rapid development of vaccine candidates.1-9
The mRNA vaccine platform has advantages as a pandemic-response strategy, given its flexibility and efficiency in immunogen design and manufacturing. Earlier work had suggested that the spike protein of the coronavirus responsible for the 2002 SARS outbreak was a suitable target for protective immunity.10 Numerous vaccine candidates in various stages of development are now being evaluated.11-13 Shortly after the SARS-CoV-2 genetic sequence was determined in January 2020, mRNA-1273, a lipid-nanoparticle (LNP)–encapsulated mRNA vaccine expressing the prefusion-stabilized spike glycoprotein, was developed by Moderna and the Vaccine Research Center at the National Institute of Allergy and Infectious Diseases (NIAID), within the National Institutes of Health (NIH).14 The mRNA-1273 vaccine demonstrated protection in animal-challenge experiments15 and encouraging safety and immunogenicity in early-stage human testing.1,4 The efficacy and safety of another mRNA vaccine, BNT162b2, was recently demonstrated.16
The Coronavirus Efficacy (COVE) phase 3 trial was launched in late July 2020 to assess the safety and efficacy of the mRNA-1273 vaccine in preventing SARS-CoV-2 infection. An independent data and safety monitoring board determined that the vaccine met the prespecified efficacy criteria at the first interim analysis. We report the primary analysis results of this ongoing pivotal phase 3 trial.
Methods
Trial Oversight
This phase 3 randomized, stratified, observer-blinded, placebo-controlled trial enrolled adults in medically stable condition at 99 U.S. sites. Participants received the first trial injection between July 27 and October 23, 2020. The trial is being conducted in accordance with the International Council for Harmonisation of Technical Requirements for Pharmaceuticals for Human Use, Good Clinical Practice guidelines, and applicable government regulations. The central institutional review board approved the protocol and the consent forms. All participants provided written informed consent before enrollment. Safety is reviewed by a protocol safety review team weekly and by an independent data and safety monitoring board on a continual basis. The trial Investigational New Drug sponsor, Moderna, was responsible for the overall trial design (with input from the Biomedical Advanced Research and Development Authority, the NIAID, the Covid-19 Prevention Network, and the trial cochairs), site selection and monitoring, and data analysis. Investigators are responsible for data collection. A medical writer funded by Moderna assisted in drafting the manuscript for submission. The authors vouch for the accuracy and completeness of the data and for the fidelity of the trial to the protocol. The trial is ongoing, and the investigators remain unaware of participant-level data. Designated team members within Moderna have unblinded access to the data, to facilitate interface with the regulatory agencies and the data and safety monitoring board; all other trial staff and participants remain unaware of the treatment assignments.
Participants, Randomization, and Data Blinding
Eligible participants were persons 18 years of age or older with no known history of SARS-CoV-2 infection and with locations or circumstances that put them at an appreciable risk of SARS-CoV-2 infection, a high risk of severe Covid-19, or both. Inclusion and exclusion criteria are provided in the protocol (available with the full text of this article at NEJM.org). To enhance the diversity of the trial population in accordance with Food and Drug Administration Draft Guidance, site-selection and enrollment processes were adjusted to increase the number of persons from racial and ethnic minorities in the trial, in addition to the persons at risk for SARS-CoV-2 infection in the local population. The upper limit for stratification of enrolled participants considered to be “at risk for severe illness” at screening was increased from 40% to 50%.17
Participants were randomly assigned in a 1:1 ratio, through the use of a centralized interactive response technology system, to receive vaccine or placebo. Assignment was stratified, on the basis of age and Covid-19 complications risk criteria, into the following risk groups: persons 65 years of age or older, persons younger than 65 years of age who were at heightened risk (at risk) for severe Covid-19, and persons younger than 65 years of age without heightened risk (not at risk). Participants younger than 65 years of age were categorized as having risk for severe Covid-19 if they had at least one of the following risk factors, based on the Centers for Disease Control and Prevention (CDC) criteria available at the time of trial design: chronic lung disease (e.g., emphysema, chronic bronchitis, idiopathic pulmonary fibrosis, cystic fibrosis, or moderate-to-severe asthma); cardiac disease (e.g., heart failure, congenital coronary artery disease, cardiomyopathies, or pulmonary hypertension); severe obesity (body mass index [the weight in kilograms divided by the square of the height in meters] ≥40); diabetes (type 1, type 2, or gestational); liver disease; or infection with the human immunodeficiency virus.18
Vaccine dose preparation and administration were performed by pharmacists and vaccine administrators who were aware of treatment assignments but had no other role in the conduct of the trial. Once the injection was completed, only trial staff who were unaware of treatment assignments performed assessments and interacted with the participants. Access to the randomization code was strictly controlled at the pharmacy. The data and safety monitoring board reviewed efficacy data at the group level and unblinded safety data at the participant level.
Trial Vaccine
The mRNA-1273 vaccine, provided as a sterile liquid at a concentration of 0.2 mg per milliliter, was administered by injection into the deltoid muscle according to a two-dose regimen. Injections were given 28 days apart, in the same arm, in a volume of 0.5 ml containing 100 μg of mRNA-1273 or saline placebo.1 Vaccine mRNA-1273 was stored at 2° to 8°C (35.6° to 46.4°F) at clinical sites before preparation and vaccination. No dilution was required. Doses could be held in syringes for up to 8 hours at room temperature before administration.
Safety Assessments
Safety assessments included monitoring of solicited local and systemic adverse events for 7 days after each injection; unsolicited adverse reactions for 28 days after each injection; adverse events leading to discontinuation from a dose, from participation in the trial, or both; and medically attended adverse events and serious adverse events from day 1 through day 759. Adverse event grading criteria and toxicity tables are described in the protocol. Cases of Covid-19 and severe Covid-19 were continuously monitored by the data and safety monitoring board from randomization onward.
Efficacy Assessments
The primary end point was the efficacy of the mRNA-1273 vaccine in preventing a first occurrence of symptomatic Covid-19 with onset at least 14 days after the second injection in the per-protocol population, among participants who were seronegative at baseline. End points were judged by an independent adjudication committee that was unaware of group assignment. Covid-19 cases were defined as occurring in participants who had at least two of the following symptoms: fever (temperature ≥38°C), chills, myalgia, headache, sore throat, or new olfactory or taste disorder, or as occurring in those who had at least one respiratory sign or symptom (including cough, shortness of breath, or clinical or radiographic evidence of pneumonia) and at least one nasopharyngeal swab, nasal swab, or saliva sample (or respiratory sample, if the participant was hospitalized) that was positive for SARS-CoV-2 by reverse-transcriptase–polymerase-chain-reaction (RT-PCR) test. Participants were assessed for the presence of SARS-CoV-2–binding antibodies specific to the SARS-CoV-2 nucleocapsid protein (Roche Elecsys, Roche Diagnostics International) and had a nasopharyngeal swab for SARS-CoV-2 RT-PCR testing (Viracor, Eurofins Clinical Diagnostics) before each injection. SARS-CoV-2–infected volunteers were followed daily, to assess symptom severity, for 14 days or until symptoms resolved, whichever was longer. A nasopharyngeal swab for RT-PCR testing and a blood sample for identifying serologic evidence of SARS-CoV-2 infection were collected from participants with symptoms of Covid-19.
The consistency of vaccine efficacy at the primary end point was evaluated across various subgroups, including age groups (18 to <65 years of age and ≥65 years), age and health risk for severe disease (18 to <65 years and not at risk; 18 to <65 years and at risk; and ≥65 years), sex (female or male), race and ethnic group, and risk for severe Covid-19 illness. If the number of participants in a subgroup was too small, it was combined with other subgroups for the subgroup analyses.
A secondary end point was the efficacy of mRNA-1273 in the prevention of severe Covid-19 as defined by one of the following criteria: respiratory rate of 30 or more breaths per minute; heart rate at or exceeding 125 beats per minute; oxygen saturation at 93% or less while the participant was breathing ambient air at sea level or a ratio of the partial pressure of oxygen to the fraction of inspired oxygen below 300 mm Hg; respiratory failure; acute respiratory distress syndrome; evidence of shock (systolic blood pressure <90 mm Hg, diastolic blood pressure <60 mm Hg, or a need for vasopressors); clinically significant acute renal, hepatic, or neurologic dysfunction; admission to an intensive care unit; or death. Additional secondary end points included the efficacy of the vaccine at preventing Covid-19 after a single dose or at preventing Covid-19 according to a secondary (CDC), less restrictive case definition: having any symptom of Covid-19 and a positive SARS-CoV-2 test by RT-PCR (see Table S1 in the Supplementary Appendix, available at NEJM.org).
Statistical Analysis
For analysis of the primary end point, the trial was designed for the null hypothesis that the efficacy of the mRNA-1273 vaccine is 30% or less. A total of 151 cases of Covid-19 would provide 90% power to detect a 60% reduction in the hazard rate (i.e., 60% vaccine efficacy), with two planned interim analyses at approximately 35% and 70% of the target total number of cases (151) and with a one-sided O’Brien–Fleming boundary for efficacy and an overall one-sided error rate of 0.025. The efficacy of the mRNA-1273 vaccine could be demonstrated at either the interim or the primary analysis, performed when the target total number of cases had been observed. The Lan–DeMets alpha-spending function was used for calculating efficacy boundaries at each analysis. At the first interim analysis on November 15, 2020, vaccine efficacy had been demonstrated in accordance with the prespecified statistical criteria. The vaccine efficacy estimate, based on a total of 95 adjudicated cases (63% of the target total), was 94.5%, with a one-sided P value of less than 0.001 to reject the null hypothesis that vaccine efficacy would be 30% or less. The data and safety monitoring board recommendation to the oversight group and the trial sponsor was that the efficacy findings should be shared with the participants and the community (full details are available in the protocol and statistical analysis plan).
Vaccine efficacy was assessed in the full analysis population (randomized participants who received at least one dose of mRNA-1273 or placebo), the modified intention-to-treat population (participants in the full analysis population who had no immunologic or virologic evidence of Covid-19 on day 1, before the first dose), and the per-protocol population (participants in the modified intention-to-treat population who received two doses, with no major protocol deviations). The primary efficacy end point in the interim and primary analyses was assessed in the per-protocol population. Participants were evaluated in the treatment groups to which they were assigned. Vaccine efficacy was defined as the percentage reduction in the hazard ratio for the primary end point (mRNA-1273 vs. placebo). A stratified Cox proportional hazards model was used to assess the vaccine efficacy of mRNA-1273 as compared with placebo in terms of the percentage hazard reduction. (Details regarding the analysis of vaccine efficacy are provided in the Methods section of the Supplementary Appendix.)
Safety was assessed in all participants in the solicited safety population (i.e., those who received at least one injection and reported a solicited adverse event). Descriptive summary data (numbers and percentages) for participants with any solicited adverse events, unsolicited adverse events, unsolicited severe adverse events, serious adverse events, medically attended adverse events, and adverse events leading to discontinuation of the injections or withdrawal from the trial are provided by group. Two-sided 95% exact confidence intervals (Clopper–Pearson method) are provided for the percentages of participants with solicited adverse events. Unsolicited adverse events are presented according to the Medical Dictionary for Regulatory Activities (MedDRA), version 23.0, preferred terms and system organ class categories.
To meet the regulatory agencies’ requirement of a median follow-up duration of at least 2 months after completion of the two-dose regimen, a second analysis was performed, with an efficacy data cutoff date of November 21, 2020. This second analysis is considered the primary analysis of efficacy, with a total of 196 adjudicated Covid-19 cases in the per-protocol population, which exceeds the target total number of cases (151) specified in the protocol. This was an increase from the 95 cases observed at the first interim analysis data cutoff on November 11, 2020. Results from the primary analysis are presented in this report. Subsequent analyses are considered supplementary.
Results
Trial Population
Between July 27, 2020, and October 23, 2020, a total of 30,420 participants underwent randomization, and the 15,210 participants in each group were assigned to receive two doses of either placebo or mRNA-1273 (100 μg) (Figure 1). More than 96% of participants received the second dose (Fig. S1). Common reasons for not receiving the second dose were withdrawal of consent (153 participants) and the detection of SARS-CoV-2 by PCR before the administration of the second dose on day 29 (114 participants: 69 in the placebo group and 45 in the mRNA-1273 group). The primary efficacy and safety analyses were performed in the per-protocol and safety populations, respectively. Of the participants who received a first injection, 14,073 of those in the placebo group and 14,134 in the mRNA-1273 group were included in the primary efficacy analysis; 525 participants in the placebo group and 416 in the mRNA-1273 group were excluded from the per-protocol population, including those who had not received a second dose by the day 29 data cutoff (Figure 1). As of November 25, 2020, the participants had a median follow-up duration of 63 days (range, 0 to 97) after the second dose, with 62% of participants having more than 56 days of follow-up.
Figure 1

Randomization and Analysis Populations.
The data cutoff for the primary analysis occurred on November 25, 2020. The full analysis population consisted of participants who underwent randomization and received at least one dose of mRNA-1273 or placebo; the modified intention-to-treat population comprised participants in the full analysis population who had no immunologic or virologic evidence of Covid-19 on day 1, before the first dose; and the per-protocol analysis population included participants in the modified intention-to-treat population who received two doses, with no major protocol deviations. The safety population included all participants who received at least one injection. Among participants who received an incorrect injection, three participants in the mRNA-1273 group received at least one dose of placebo and no dose of mRNA-1273 and were included in the placebo safety population, and three received one dose of placebo and one dose of mRNA-1273 and were included in the mRNA-1273 safety population; in the placebo group all seven received mRNA-1273 and were included in the mRNA-1273 safety population. Participants who received dose 2 outside the window for the per-protocol analysis are those who did not receive the second dose between 7 days before and 14 days after day 29.
Baseline demographic characteristics were balanced between the placebo group and the mRNA-1273 vaccine group (Table 1 and Table S2). The mean age of the participants was 51.4 years, 47.3% of the participants were female, 24.8% were 65 years of age or older, and 16.7% were younger than 65 years of age and had predisposing medical conditions that put them at risk for severe Covid-19. The majority of participants were White (79.2%), and the racial and ethnic proportions were generally representative of U.S. demographics, including 10.2% Black or African American and 20.5% Hispanic or Latino. Evidence of SARS-CoV-2 infection at baseline was present in 2.3% of participants in the mRNA-1273 group and in 2.2% in the placebo group, as detected by serologic assay or RT-PCR testing.
Table 1

| Characteristics | Placebo (N=15,170) |
mRNA-1273 (N=15,181) |
Total (N=30,351) |
|---|---|---|---|
| Sex — no. of participants (%) | |||
| Male | 8,062 (53.1) | 7,923 (52.2) | 15,985 (52.7) |
| Female | 7,108 (46.9) | 7,258 (47.8) | 14,366 (47.3) |
| Mean age (range) — yr | 51.3 (18–95) | 51.4 (18–95) | 51.4 (18–95) |
| Age category and risk for severe Covid-19 — no. of participants (%)† | |||
| 18 to <65 yr, not at risk | 8,886 (58.6) | 8,888 (58.5) | 17,774 (58.6) |
| 18 to <65 yr, at risk | 2,535 (16.7) | 2,530 (16.7) | 5,065 (16.7) |
| ≥65 yr | 3,749 (24.7) | 3,763 (24.8) | 7,512 (24.8) |
| Hispanic or Latino ethnicity — no. of participants (%)‡ | |||
| Hispanic or Latino | 3,114 (20.5) | 3,121 (20.6) | 6,235 (20.5) |
| Not Hispanic or Latino | 11,917 (78.6) | 11,918 (78.5) | 23,835 (78.5) |
| Not reported and unknown | 139 (0.9) | 142 (0.9) | 281 (0.9) |
| Race or ethnic group — no. of participants (%)‡ | |||
| White | 11,995 (79.1) | 12,029 (79.2) | 24,024 (79.2) |
| Black or African American | 1,527 (10.1) | 1,563 (10.3) | 3,090 (10.2) |
| Asian | 731 (4.8) | 651 (4.3) | 1,382 (4.6) |
| American Indian or Alaska Native | 121 (0.8) | 112 (0.7) | 233 (0.8) |
| Native Hawaiian or Other Pacific Islander | 32 (0.2) | 35 (0.2) | 67 (0.2) |
| Multiracial | 321 (2.1) | 315 (2.1) | 636 (2.1) |
| Other | 316 (2.1) | 321 (2.1) | 637 (2.1) |
| Not reported and unknown | 127 (0.8) | 155 (1.0) | 282 (0.9) |
| Baseline SARS-CoV-2 status — no. of participants (%)§ | |||
| Negative | 14,598 (96.2) | 14,550 (95.8) | 29,148 (96.0) |
| Positive | 337 (2.2) | 343 (2.3) | 680 (2.2) |
| Missing data | 235 (1.5) | 288 (1.9) | 523 (1.7) |
| Baseline RT-PCR test — no. of participants (%) | |||
| Negative | 14,923 (98.4) | 14,917 (98.3) | 29,840 (98.3) |
| Positive | 95 (0.6) | 87 (0.6) | 182 (0.6) |
| Missing data | 152 (1.0) | 177 (1.2) | 329 (1.1) |
| Baseline bAb anti–SARS-CoV-2 assay — no. of participants (%) | |||
| Negative | 14,726 (97.1) | 14,690 (96.8) | 29,416 (96.9) |
| Positive | 303 (2.0) | 305 (2.0) | 608 (2.0) |
| Missing data | 141 (0.9) | 186 (1.2) | 327 (1.1) |
| Risk factor for severe Covid-19 — no. of participants (%) | |||
| Chronic lung disease | 744 (4.9) | 710 (4.7) | 1,454 (4.8) |
| Significant cardiac disease | 744 (4.9) | 752 (5.0) | 1,496 (4.9) |
| Severe obesity | 1,021 (6.7) | 1,025 (6.8) | 2,046 (6.7) |
| Diabetes | 1,440 (9.5) | 1,435 (9.5) | 2,875 (9.5) |
| Liver disease | 96 (0.6) | 100 (0.7) | 196 (0.6) |
| Human immunodeficiency virus infection | 87 (0.6) | 92 (0.6) | 179 (0.6) |
| Body-mass index¶ | |||
| No. of participants | 15,007 | 14,985 | 29,992 |
| Mean ±SD | 29.3±6.7 | 29.3±6.9 | 29.3±6.8 |
Demographic and Clinical Characteristics at Baseline.*
*
Internet-based randomization was used to assign participants to treatment groups on the basis of information entered by the investigator regarding the participant’s age and coexisting conditions. Percentages are based on the full analysis population; baseline demographics and characteristics for the per-protocol population are provided in the Supplementary Appendix. Percentages may not total 100 because of rounding. The abbreviation bAb denotes binding antibody concentration, and RT-PCR reverse-transcriptase polymerase chain reaction.
†
Risk was based on a stratification factor from the Internet-based interactive response system used for randomization; participants who were younger than 65 years of age were categorized as at risk for severe Covid-19 illness if they had at least one of the risk factors specified in the trial protocol at screening.
‡
Race or ethnic group was reported by the participant. Participants could be included in more than one category.
§
Baseline SARS-CoV-2 status was positive if there was immunologic or virologic evidence of previous illness with Covid-19, as defined by a positive RT-PCR test or a positive bAb against SARS-CoV-2 nucleocapsid assay result that was above the limit of detection or by a lower limit of quantification at day 1. Baseline SARS-CoV-2 status was negative if there was a negative RT-PCR test and negative bAb against SARS-CoV-2 assay result at day 1.
¶
The body-mass index is the weight in kilograms divided by the square of the height in meters.
Safety
Solicited adverse events at the injection site occurred more frequently in the mRNA-1273 group than in the placebo group after both the first dose (84.2%, vs. 19.8%) and the second dose (88.6%, vs. 18.8%) (Figure 2 and Tables S3 and S4). In the mRNA-1273 group, injection-site events were mainly grade 1 or 2 in severity and lasted a mean of 2.6 and 3.2 days after the first and second doses, respectively (Table S5). The most common injection-site event was pain after injection. Delayed injection-site reactions (those with onset on or after day 8) were noted in 244 participants (0.8%) after the first dose and in 68 participants (0.2%) after the second dose. Reactions were characterized by erythema, induration, and tenderness, and they resolved over the following 4 to 5 days. Solicited systemic adverse events occurred more often in the mRNA-1273 group than in the placebo group after both the first dose (54.9%, vs. 42.2%) and the second dose (79.4%, vs. 36.5%). The severity of the solicited systemic events increased after the second dose in the mRNA-1273 group, with an increase in proportions of grade 2 events (from 16.5% after the first dose to 38.1% after the second dose) and grade 3 events (from 2.9% to 15.8%). Solicited systemic adverse events in the mRNA-1273 group lasted a mean of 2.9 days and 3.1 days after the first and second doses, respectively (Table S5). Both solicited injection-site and systemic adverse events were more common among younger participants (18 to <65 years of age) than among older participants (≥65 years of age). Solicited adverse events were less common in participants who were positive for SARS-CoV-2 infection at baseline than in those who were negative at baseline (Tables S6 and S7).
Figure 2

Solicited Local and Systemic Adverse Events.
Shown is the percentage of participants who had a solicited local or systemic adverse event within 7 days after injection 1 or injection 2 of either the placebo or the mRNA-1273 vaccine.
The frequency of unsolicited adverse events, unsolicited severe adverse events, and serious adverse events reported during the 28 days after injection was generally similar among participants in the two groups (Tables S8 through S11). Three deaths occurred in the placebo group (one from intraabdominal perforation, one from cardiopulmonary arrest, and one from severe systemic inflammatory syndrome in a participant with chronic lymphocytic leukemia and diffuse bullous rash) and two in the vaccine group (one from cardiopulmonary arrest and one by suicide). The frequency of grade 3 adverse events in the placebo group (1.3%) was similar to that in the vaccine group (1.5%), as were the frequencies of medically attended adverse events (9.7% vs. 9.0%) and serious adverse events (0.6% in both groups). Hypersensitivity reactions were reported in 1.5% and 1.1% of participants in the vaccine and placebo groups, respectively (Table S12). Bell’s palsy occurred in the vaccine group (3 participants [<0.1%]) and the placebo group (1 participant [<0.1%]) during the observation period of the trial (more than 28 days after injection). Overall, 0.5% of participants in the placebo group and 0.3% in the mRNA-1273 group had adverse events that resulted in their not receiving the second dose, and less than 0.1% of participants in both groups discontinued participation in the trial because of adverse events after any dose (Table S8). No evidence of vaccine-associated enhanced respiratory disease was noted, and fewer cases of severe Covid-19 or any Covid-19 were observed among participants who received mRNA-1273 than among those who received placebo (Tables S13 and S14). Adverse events that were deemed by the trial team to be related to the vaccine or placebo were reported among 4.5% of participants in the placebo group and 8.2% in the mRNA-1273 group. The most common treatment-related adverse events (those reported in at least 1% of participants) in the placebo group and the mRNA-1273 group were fatigue (1.2% and 1.5%) and headache (0.9% and 1.4%). In the overall population, the incidence of treatment-related severe adverse events was higher in the mRNA-1273 group (71 participants [0.5%]) than in the placebo group (28 participants [0.2%]) (Tables S8 and S15). The relative incidence of these adverse events according to vaccine group was not affected by age.
Efficacy
After day 1 and through November 25, 2020, a total of 269 Covid-19 cases were identified, with an incidence of 79.7 cases per 1000 person-years (95% confidence interval [CI], 70.5 to 89.9) among participants in the placebo group with no evidence of previous SARS-CoV-2 infection. For the primary analysis, 196 cases of Covid-19 were diagnosed: 11 cases in the vaccine group (3.3 per 1000 person-years; 95% CI, 1.7 to 6.0) and 185 cases in the placebo group (56.5 per 1000 person-years; 95% CI, 48.7 to 65.3), indicating 94.1% efficacy of the mRNA-1273 vaccine (95% CI, 89.3 to 96.8%; P<0.001) for the prevention of symptomatic SARS-CoV-2 infection as compared with placebo (Figure 3A). Findings were similar across key secondary analyses (Table S16), including assessment starting 14 days after dose 1 (225 cases with placebo, vs. 11 with mRNA-1273, indicating a vaccine efficacy of 95.2% [95% CI, 91.2 to 97.4]), and assessment including participants who were SARS-CoV-2 seropositive at baseline in the per-protocol analysis (187 cases with placebo, vs. 12 with mRNA-1273; one volunteer assigned to receive mRNA-1273 was inadvertently given placebo], indicating a vaccine efficacy of 93.6% [95% CI, 88.6 to 96.5]). Between days 1 and 42, seven cases of Covid-19 were identified in the mRNA-1273 group, as compared with 65 cases in the placebo group (Figure 3B).
Figure 3

Vaccine Efficacy of mRNA-1273 to Prevent Covid-19.
Shown is the cumulative incidence of Covid-19 events in the primary analysis based on adjudicated assessment starting 14 days after the second vaccination in the per-protocol population (Panel A) and after randomization in the modified intention-to-treat population (Panel B) (see the Supplementary Appendix). The dotted line in Panel A indicates day 42 (14 days after vaccination 2), when the per-protocol follow-up began, and arrows in both panels indicate days 1 and 29, when injections were administered. Tick marks indicate censored data. Vaccine efficacy was defined as 1 minus the hazard ratio (mRNA vs. placebo), and the 95% confidence interval was estimated with the use of a stratified Cox proportional hazards model, with Efron’s method of tie handling and with treatment group as a covariate, with adjustment for stratification factor. Incidence was defined as the number of events divided by number of participants at risk and was adjusted by person-years. Symptomatic Covid-19 case accrual for placebo and vaccine in the modified intention-to-treat population is displayed (does not include asymptomatic cases of SARS-CoV-2 detected at the day 29 by nasopharyngeal swab).
A key secondary end point evaluated the efficacy of mRNA-1273 at preventing severe Covid-19. Thirty participants in the trial had severe Covid-19; all 30 were in the placebo group (indicating vaccine efficacy of 100% [95% CI, could not be estimated to 1.0]), and one death among these participants was attributed to Covid-19 (Table S16). The vaccine efficacy to prevent Covid-19 was consistent across subgroups stratified by demographic and baseline characteristics (Figure 4): age groups (18 to <65 years of age and ≥65 years), presence of risk for severe Covid-19, sex, and race and ethnic group (non-Hispanic White and communities of color). Among participants who were positive for SARS-CoV-2, by serologic or virologic testing, at baseline (337 in the placebo group and 343 in the mRNA-1273 group), one case of Covid-19 was diagnosed by RT-PCR testing in a placebo recipient and no cases were diagnosed in mRNA-1273 recipients (Table S17). Among participants who were negative for SARS-CoV-2 at baseline (by RT-PCR or antibody testing), in addition to symptomatic Covid-19 cases 39 (0.3%) in the placebo group and 15 (0.1%) in the mRNA-1273 group had nasopharyngeal swabs that were positive for SARS-CoV-2 by RT-PCR at the second dose visit (surveillance swab) but had no evidence of Covid-19 symptoms (Table S18).
Figure 4

Vaccine Efficacy of mRNA-1273 to Prevent Covid-19 in Subgroups.
The efficacy of the RNA-1273 vaccine in preventing Covid-19 in various subgroups in the per-protocol population was based on adjudicated assessments starting 14 days after the second injection. Vaccine efficacy, defined as 1 minus the hazard ratio (mRNA-1273 vs. placebo), and 95% confidence intervals were estimated with the use of a stratified Cox proportional hazards model, with Efron’s method of tie handling and with the treatment group as a covariate, adjusting for stratification factor if applicable. Race and ethnic group categories shown are White (non-Hispanic) and communities of color (all others, excluding those whose race and ethnicity were both reported as unknown, were not reported, or were both missing at screening). Data for communities of color were pooled owing to limited numbers of participants in each racial or ethnic group, to ensure that the subpopulations would be large enough for meaningful analyses.
Discussion
The COVE trial provides evidence of short-term efficacy of the mRNA-1273 vaccine in preventing symptomatic SARS-CoV-2 infection in a diverse adult trial population. Of note, the trial was designed for an infection attack rate of 0.75%, which would have necessitated a follow-up period of 6 months after the two vaccine doses to accrue 151 cases in 30,000 participants. The pandemic trajectory accelerated in many U.S. regions in the late summer and fall of 2020, resulting in rapid accrual of 196 cases after a median follow-up of 2 months. It is important to note that all the severe Covid-19 cases were in the placebo group, which suggests that mRNA-1273 is likely to have an effect on preventing severe illness, which is the major cause of health care utilization, complications, and death. The finding of fewer occurrences of symptomatic SARS-CoV-2 infection after a single dose of mRNA-1273 is encouraging; however, the trial was not designed to evaluate the efficacy of a single dose, and additional evaluation is warranted.
The magnitude of mRNA-1273 vaccine efficacy at preventing symptomatic SARS-CoV-2 infection is higher than the efficacy observed for vaccines for respiratory viruses, such as the inactivated influenza vaccine against symptomatic, virologically confirmed disease in adults, for which studies have shown a pooled efficacy of 59%.19 This high apparent efficacy of mRNA-1273 is based on short-term data, and waning of efficacy over time has been demonstrated with other vaccines.20 Also, the efficacy of the vaccine was tested in a setting of national recommendations for masking and social distancing, which may have translated into lower levels of infectious inoculum. The efficacy of mRNA-1273 is in line with that of the recently reported BNT162b2 mRNA vaccine.16 The COVE trial is ongoing, and longitudinal follow-up will allow an assessment of efficacy changes over time and under evolving epidemiologic conditions.
Overall, the safety of the mRNA-1273 vaccine regimen and platform is reassuring; no unexpected patterns of concern were identified. The reactogenicity associated with immunization with mRNA-1273 in this trial is similar to that in the phase 1 data reported previously.1,4 Overall, the local reactions to vaccination were mild; however, moderate-to-severe systemic side effects, such as fatigue, myalgia, arthralgia, and headache, were noted in about 50% of participants in the mRNA-1273 group after the second dose. These side effects were transient, starting about 15 hours after vaccination and resolving in most participants by day 2, without sequelae. The degree of reactogenicity after one dose of mRNA-1273 was less than that observed for the recently approved recombinant adjuvanted zoster vaccine and after the second mRNA-1273 dose was similar to that of the zoster vaccine.21,22 Delayed injection-site reactions, with an onset 8 days or more after injection, were uncommon. The overall incidence of unsolicited adverse events reported up to 28 days after vaccination and of serious adverse events reported throughout the entire trial was similar for mRNA-1273 and placebo. A risk of acute hypersensitivity is sometimes observed with vaccines; however, no such risk was evident in the COVE trial, although the ability to detect rare events is limited, given the trial sample size. The anecdotal finding of a slight excess of Bell’s palsy in this trial and in the BNT162b2 vaccine trial arouses concern that it may be more than a chance event, and the possibility bears close monitoring.16
The mRNA-1273 vaccine did not show evidence in the short term of enhanced respiratory disease after infection, a concern that emerged from animal models used in evaluating some SARS and Middle East respiratory syndrome (MERS) vaccine constructs.23-25 A hallmark of enhanced respiratory disease is a Th2-skewed immune response and eosinophilic pulmonary infiltration on histopathological examination. Of note, preclinical testing of mRNA-1273 and other SARS-CoV-2 vaccines in advanced clinical evaluation has shown a Th1-skewed vaccine response and no pathologic lung infiltrates.15,26–28 Whether mRNA-1273 vaccination results in enhanced disease on exposure to the virus in the long term is unknown.
Key limitations of the data are the short duration of safety and efficacy follow-up. The trial is ongoing, and a follow-up duration of 2 years is planned, with possible changes to the trial design to allow participant retention and ongoing data collection. Another limitation is the lack of an identified correlate of protection, a critical tool for future bridging studies. As of the data cutoff, 11 cases of Covid-19 had occurred in the mRNA-1273 group, a finding that limits our ability to detect a correlate of protection. As cases accrue and immunity wanes, it may become possible to determine such a correlate. In addition, although our trial showed that mRNA-1273 reduces the incidence of symptomatic SARS-CoV-2 infection, the data were not sufficient to assess asymptomatic infection, although our results from a preliminary exploratory analysis suggest that some degree of prevention may be afforded after the first dose. Evaluation of the incidence of asymptomatic or subclinical infection and viral shedding after infection are under way, to assess whether vaccination affects infectiousness. The relatively smaller numbers of cases that occurred in older adults and in participants from ethnic or racial minorities and the small number of previously infected persons who received the vaccine limit efficacy evaluations in these groups. Longer-term data from the ongoing trial may allow a more careful evaluation of the vaccine efficacy in these groups. Pregnant women and children were excluded from this trial, and additional evaluation of the vaccine in these groups is planned.
Within 1 year after the emergence of this novel infection that caused a pandemic, a pathogen was determined, vaccine targets were identified, vaccine constructs were created, manufacturing to scale was developed, phase 1 through phase 3 testing was conducted, and data have been reported. This process demonstrates what is possible in the context of motivated collaboration among key sectors of society, including academia, government, industry, regulators, and the larger community. Lessons learned from this endeavor should allow us to better prepare for the next pandemic pathogen.
Notes
This article was published on December 30, 2020, and updated on January 15, 2021, at NEJM.org.
A data sharing statement provided by the authors is available with the full text of this article at NEJM.org.
Supported by the Office of the Assistant Secretary for Preparedness and Response, Biomedical Advanced Research and Development Authority (contract 75A50120C00034) and by the National Institute of Allergy and Infectious Diseases (NIAID). The NIAID provides grant funding to the HIV Vaccine Trials Network (HVTN) Leadership and Operations Center (UM1 AI 68614HVTN), the Statistics and Data Management Center (UM1 AI 68635), the HVTN Laboratory Center (UM1 AI 68618), the HIV Prevention Trials Network Leadership and Operations Center (UM1 AI 68619), the AIDS Clinical Trials Group Leadership and Operations Center (UM1 AI 68636), and the Infectious Diseases Clinical Research Consortium leadership group 5 (UM1 AI148684-03).
Dr. Baden reports being funded by the NIH to conduct clinical trials in collaboration with Crucell/Janssen and Moderna; Dr. Rouphael, receiving grant support from Pfizer, Merck, Sanofi–Pasteur, Eli Lilly, and Quidel; Dr. Creech, receiving grant support from Merck, consulting fees from Horizon Pharma and GSK, and fees for serving on a data and safety monitoring board from Astellas; Dr. Neuzil, receiving grant support from Pfizer; Dr. Graham, holding pending patent WO/2018/081318 on prefusion coronavirus spike proteins and their use and pending patent 62/972,886 on 2019-nCoV vaccine; Dr. Bennett, being employed by and owning stock and stock options in Moderna; Dr. Pajon, being employed by and owning stock in Moderna; Dr. Knightly, being employed by and owning stock and stock options in Moderna; Drs. Leav, Deng, and Zhou being employees of Moderna; Dr. Han, being employed by and owning stock and stock options in Moderna; Dr. Ivarsson, being employed by and owning share options in Moderna; Dr. Miller, being employed by and owning stock and stock options in Moderna; and Dr. Zaks, being employed by and owning stock options in Moderna. No other potential conflict of interest relevant to this article was reported.
Disclosure forms provided by the authors are available with the full text of this article at NEJM.org.
We thank the participants in the trial and the members of the mRNA-1273 trial team (listed in the Supplementary Appendix) for their dedication and the contributions to the trial, and the members of the data and safety monitoring board (Richard J. Whitley [chair], University of Alabama School of Medicine; Abdel Babiker, MRC Clinical Trials Unit at University College, London; Lisa A. Cooper, Johns Hopkins University School of Medicine and Bloomberg School of Public Health; Susan S. Ellenberg, University of Pennsylvania; Alan Fix, Vaccine Development Global Program Center for Vaccine Innovation and Access PATH; Marie Griffin, Vanderbilt University Medical Center; Steven Joffe, Perelman School of Medicine, University of Pennsylvania; Jorge Kalil, Heart Institute, Hospital das Clínicas da Faculdade de Medicina da Universidade de São Paulo; Myron M. Levine, University of Maryland School of Medicine; Malegapuru W. Makgoba, University of KwaZulu-Natal; Anastasios A. Tsiatis, North Carolina State University; Renee H. Moore, Emory University); and Sally Hunsberger [Executive Secretary], NIAID) for their hard work, support, and guidance of the trial; and the adjudication committee (Richard J. Hamill [chair], Baylor College of Medicine; Lewis Lipsitz, Harvard Medical School; Eric S. Rosenberg, Massachusetts General Hospital; and Anthony Faugno, Tufts Medical Center) for their critical and timely review of the trial data. We also acknowledge the contribution from the mRNA-1273 Product Coordination Team from the Biomedical Advanced Research and Development Authority (BARDA) (Robert Bruno, Richard Gorman, Holli Hamilton, Gary Horwith, Chuong Huynh, Nutan Mytle, Corrina Pavetto, Xiaomi Tong, and John Treanor), and Joanne E. Tomassini (JET Scientific), for assistance in writing the manuscript for submission, and Frank J. Dutko, for editorial support (funded by Moderna).
Supplementary Material
Research Summary (nejmoa2035389_research-summary.pdf)
- Download
- 3.51 MB
Protocol (nejmoa2035389_protocol.pdf)
- Download
- 3.25 MB
Supplementary Appendix (nejmoa2035389_appendix.pdf)
- Download
- 1.03 MB
Disclosure Forms (nejmoa2035389_disclosures.pdf)
- Download
- 643.60 KB
Data Sharing Statement (nejmoa2035389_data-sharing.pdf)
- Download
- 69.58 KB
References
1.
Jackson LA, Anderson EJ, Rouphael NG, et al. An mRNA vaccine against SARS-CoV-2 — preliminary report. N Engl J Med 2020;383:1920-1931.
2.
Keech C, Albert G, Cho I, et al. Phase 1–2 trial of a SARS-CoV-2 recombinant spike protein nanoparticle vaccine. N Engl J Med 2020;383:2320-2332.
3.
Walsh EE, Frenck RW Jr, Falsey AR, et al. Safety and immunogenicity of two RNA-based Covid-19 vaccine candidates. N Engl J Med 2020;383:2439-2450.
4.
Anderson EJ, Rouphael NG, Widge AT, et al. Safety and immunogenicity of SARS-CoV-2 mRNA-1273 vaccine in older adults. N Engl J Med 2020;383:2427-2438.
5.
Folegatti PM, Ewer KJ, Aley PK, et al. Safety and immunogenicity of the ChAdOx1 nCoV-19 vaccine against SARS-CoV-2: a preliminary report of a phase 1/2, single-blind, randomised controlled trial. Lancet 2020;396:467-478.
6.
Ramasamy MN, Minassian AM, Ewer KJ, et al. Safety and immunogenicity of ChAdOx1 nCoV-19 vaccine administered in a prime-boost regimen in young and old adults (COV002): a single-blind, randomised, controlled, phase 2/3 trial. Lancet 2021;396:1979-1993.
7.
Zhang Y, Zeng G, Pan H, et al. Safety, tolerability, and immunogenicity of an inactivated SARS-CoV-2 vaccine in healthy adults aged 18-59 years: a randomised, double-blind, placebo-controlled, phase 1/2 clinical trial. Lancet Infect Dis 2020 November 17 (Epub ahead of print).
8.
Zhu FC, Guan XH, Li YH, et al. Immunogenicity and safety of a recombinant adenovirus type-5-vectored COVID-19 vaccine in healthy adults aged 18 years or older: a randomised, double-blind, placebo-controlled, phase 2 trial. Lancet 2020;396:479-488.
9.
Voysey M, Clemens SAC, Madhi SA, et al. Safety and efficacy of the ChAdOx1 nCoV-19 vaccine (AZD1222) against SARS-CoV-2: an interim analysis of four randomised controlled trials in Brazil, South Africa, and the UK. Lancet 2020 December 8 (Epub ahead of print).
10.
He Y, Li J, Heck S, Lustigman S, Jiang S. Antigenic and immunogenic characterization of recombinant baculovirus-expressed severe acute respiratory syndrome coronavirus spike protein: implication for vaccine design. J Virol 2006;80:5757-5767.
11.
Bennet BM, Wolf J, Laureano R, Sellers RS. Review of current vaccine development strategies to prevent coronavirus disease 2019 (COVID-19). Toxicol Pathol 2020;48:800-809.
12.
Lurie N, Saville M, Hatchett R, Halton J. Developing Covid-19 vaccines at pandemic speed. N Engl J Med 2020;382:1969-1973.
13.
Thanh Le T, Andreadakis Z, Kumar A, et al. The COVID-19 vaccine development landscape. Nat Rev Drug Discov 2020;19:305-306.
14.
Corbett KS, Edwards D, Leist SR, et al. SARS-CoV-2 mRNA vaccine development enabled by prototype pathogen preparedness. June 11, 2020 (https://www.biorxiv.org/content/10.1101/2020.06.11.145920v1). preprint.
15.
Corbett KS, Flynn B, Foulds KE, et al. Evaluation of the mRNA-1273 vaccine against SARS-CoV-2 in nonhuman primates. N Engl J Med 2020;383:1544-1555.
16.
Polack FP, Thomas SJ, Kitchin N, et al. Safety and efficacy of the BNT162b2 Covid-19 vaccine. N Engl J Med 2020;383:2603-2615.
17.
Department of Health and Human Services, Food and Drug Administration, Center for Drug Evaluation and Research (CDER), Center for Biologics Evaluation and Research (CBER). Enhancing the diversity of clinical trial populations — eligibility criteria, enrollment practices, and trial designs: guidance for industry. November 2020 (https://www.fda.gov/media/127712/download).
18.
Centers for Disease Control and Prevention. Coronavirus disease 2019 (COVID 19). 2020 (https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-at-higher-risk.html).
19.
Osterholm MT, Kelley NS, Sommer A, Belongia EA. Efficacy and effectiveness of influenza vaccines: a systematic review and meta-analysis. Lancet Infect Dis 2012;12:36-44.
20.
Ferdinands JM, Shay DK. Magnitude of potential biases in a simulated case-control study of the effectiveness of influenza vaccination. Clin Infect Dis 2012;54:25-32.
21.
Cunningham AL, Lal H, Kovac M, et al. Efficacy of the herpes zoster subunit vaccine in adults 70 years of age or older. N Engl J Med 2016;375:1019-1032.
22.
Lal H, Cunningham AL, Heineman TC. Adjuvanted herpes zoster subunit vaccine in older adults. N Engl J Med 2015;373:1576-1577.
23.
Agrawal AS, Tao X, Algaissi A, et al. Immunization with inactivated Middle East respiratory syndrome coronavirus vaccine leads to lung immunopathology on challenge with live virus. Hum Vaccin Immunother 2016;12:2351-2356.
24.
Bolles M, Deming D, Long K, et al. A double-inactivated severe acute respiratory syndrome coronavirus vaccine provides incomplete protection in mice and induces increased eosinophilic proinflammatory pulmonary response upon challenge. J Virol 2011;85:12201-12215.
25.
Tseng CT, Sbrana E, Iwata-Yoshikawa N, et al. Immunization with SARS coronavirus vaccines leads to pulmonary immunopathology on challenge with the SARS virus. PLoS One 2012;7(4):e35421-e35421.
26.
Guebre-Xabier M, Patel N, Tian JH, et al. NVX-CoV2373 vaccine protects cynomolgus macaque upper and lower airways against SARS-CoV-2 challenge. Vaccine 2020;38:7892-7896.
27.
van Doremalen N, Lambe T, Spencer A, et al. ChAdOx1 nCoV-19 vaccine prevents SARS-CoV-2 pneumonia in rhesus macaques. Nature 2020;586:578-582.
28.
Vogel AB, Kanevsky I, Che Y, et al. A prefusion SARS-CoV-2 spike RNA vaccine is highly immunogenic and prevents lung infection in non-human primates. September 8, 2020 (https://www.biorxiv.org/content/10.1101/2020.09.08.280818v1). preprint.
Information & Authors
Information
Published In
Copyright
Copyright © 2020 Massachusetts Medical Society. All rights reserved.
History
Published online: December 30, 2020
Published in issue: February 4, 2021
Topics
Authors
Affiliations
From Brigham and Women’s Hospital (L.R.B.), Boston, and Moderna, Cambridge (H.B., R.P., C.K., B.L., W.D., H.Z., S.H., M.I., J. Miller, T.Z.) — both in Massachusetts; Baylor College of Medicine (H.M.E.S.) and Centex Studies (J.S.) — both in Houston; Meridian Clinical Research, Savannah (B.E., S.K., A.B.), and Emory University (N.R.) and Atlanta Clinical Research Center (N.S.), Atlanta — all in Georgia; University of Maryland School of Medicine, Baltimore (K.K., K.N.), and National Institute of Allergy and Infectious Diseases, Bethesda (D.F., M.M., J. Mascola, L.P., J.L., B.S.G.) — both in Maryland; Saint Louis University School of Medicine, St. Louis (S.F.); University of Illinois, Chicago, Chicago (R.N.); George Washington University School of Medicine and Health Sciences, Washington, DC (D.D.); University of California, San Diego, San Diego (S.A.S.); Vanderbilt University School of Medicine, Nashville (C.B.C.); Quality of Life Medical and Research Center, Tucson, AZ (J. McGettigan); Johnson County Clin-Trials, Lenexa, KS (C.F.); Research Centers of America, Hollywood, FL (H.S.); and Fred Hutchinson Cancer Research Center, Seattle (L.C., P.G., H.J.).
Metrics & Citations
Metrics
Altmetrics
Citations
Export citation
Select the format you want to export the citation of this publication.
Cited by
- A Case of Combination of IgA Nephropathy and Interstitial Nephritis After COVID-19 Vaccination, Cureus, (2024).https://doi.org/10.7759/cureus.52981
- COVID-19 mRNA Vaccines: Lessons Learned from the Registrational Trials and Global Vaccination Campaign, Cureus, (2024).https://doi.org/10.7759/cureus.52876
- AstraZeneca COVID-19 Vaccine and Diabetes Mellitus: A Prospective Clinical Study Regarding Vaccine Side Effects, Cureus, (2024).https://doi.org/10.7759/cureus.51583
- Altered transcriptomic immune responses of maintenance hemodialysis patients to the COVID-19 mRNA vaccine, eLife, 13, (2024).https://doi.org/10.7554/eLife.83641
- Short-term Safety of Covaxin, Sinopharm, Sputnik V, and AstraZeneca COVID-19 Vaccines Among Iranian Healthcare Workers: A Cross-Sectional Study, Archives of Clinical Infectious Diseases, 19, 1, (2024).https://doi.org/10.5812/archcid-142157
- Impact of shift work and other work-related factors on anti-SARS-CoV-2 spike-protein serum concentrations in healthcare workers after primary mRNA vaccination – a retrospective cohort study, Swiss Medical Weekly, 154, 3, (3708), (2024).https://doi.org/10.57187/s.3708
- The Rise of RNA-Based Therapeutics: Recent Advances and Therapeutic Potential, Journal for Research in Applied Sciences and Biotechnology, 2, 6, (216-226), (2024).https://doi.org/10.55544/jrasb.2.6.31
- Rule Based Mamdani Fuzzy Inference System to Analyze Efficacy of COVID19 Vaccines, EAI Endorsed Transactions on Pervasive Health and Technology, 10, (2024).https://doi.org/10.4108/eetpht.10.5571
- Vaccine Safety: Assessing the Prevalence and Severity of Adverse Events Following COVID-19 Vaccination amongst Healthcare Workers in Tertiary Health Facilities in Nigeria, Nigerian Postgraduate Medical Journal, 31, 1, (1-7), (2024).https://doi.org/10.4103/npmj.npmj_227_23
- Assessment of some immunological markers in patients and vaccinated individuals with COVID-19 in Kirkuk city, Medical Journal of Babylon, 20, Supplement 1, (S115-S122), (2024).https://doi.org/10.4103/MJBL.MJBL_171_22
- See more
Loading...