Safety and Efficacy of the BNT162b2 mRNA Covid-19 Vaccine through 6 Months
Published September 15, 2021
N Engl J Med 2021;385:1761-1773
DOI: 10.1056/NEJMoa2110345
Abstract
Background
BNT162b2 is a lipid nanoparticle–formulated, nucleoside-modified RNA vaccine encoding a prefusion-stabilized, membrane-anchored severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) full-length spike protein. BNT162b2 is highly efficacious against coronavirus disease 2019 (Covid-19) and is currently approved, conditionally approved, or authorized for emergency use worldwide. At the time of initial authorization, data beyond 2 months after vaccination were unavailable.
Methods
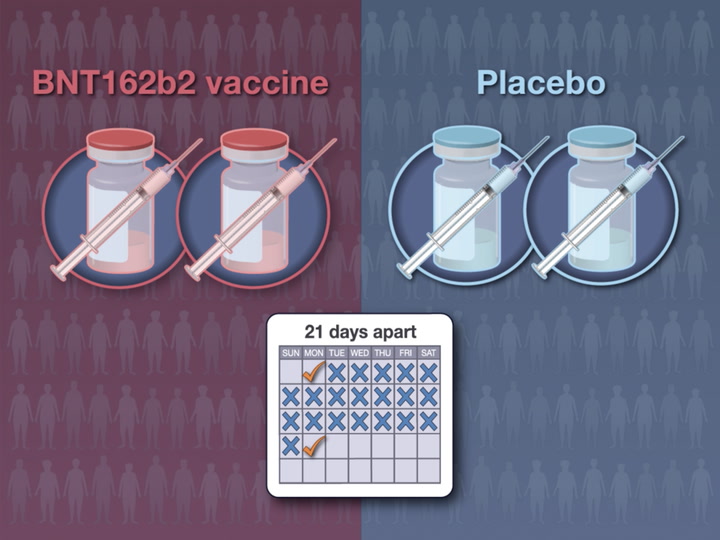
In an ongoing, placebo-controlled, observer-blinded, multinational, pivotal efficacy trial, we randomly assigned 44,165 participants 16 years of age or older and 2264 participants 12 to 15 years of age to receive two 30-μg doses, at 21 days apart, of BNT162b2 or placebo. The trial end points were vaccine efficacy against laboratory-confirmed Covid-19 and safety, which were both evaluated through 6 months after vaccination.

Results
BNT162b2 continued to be safe and have an acceptable adverse-event profile. Few participants had adverse events leading to withdrawal from the trial. Vaccine efficacy against Covid-19 was 91.3% (95% confidence interval [CI], 89.0 to 93.2) through 6 months of follow-up among the participants without evidence of previous SARS-CoV-2 infection who could be evaluated. There was a gradual decline in vaccine efficacy. Vaccine efficacy of 86 to 100% was seen across countries and in populations with diverse ages, sexes, race or ethnic groups, and risk factors for Covid-19 among participants without evidence of previous infection with SARS-CoV-2. Vaccine efficacy against severe disease was 96.7% (95% CI, 80.3 to 99.9). In South Africa, where the SARS-CoV-2 variant of concern B.1.351 (or beta) was predominant, a vaccine efficacy of 100% (95% CI, 53.5 to 100) was observed.
Conclusions
Through 6 months of follow-up and despite a gradual decline in vaccine efficacy, BNT162b2 had a favorable safety profile and was highly efficacious in preventing Covid-19. (Funded by BioNTech and Pfizer; ClinicalTrials.gov number, NCT04368728.)
The coronavirus disease 2019 (Covid-19) pandemic continues, with recent estimates of more than 187 million cases diagnosed and more than 4 million deaths.1 Vaccines are currently available by means of full approval, conditional marketing approval, and emergency use authorization pathways.2-5 BNT162b2 is a lipid nanoparticle–formulated,6 nucleoside-modified RNA7 encoding the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) full-length spike glycoprotein in a prefusion stabilized conformation.8 To date, more than 1 billion doses of BNT162b2 have been distributed.
We previously reported safety and efficacy data obtained through a median of 2 months of postimmunization follow-up from a global phase 1–2–3 trial of BNT162b2 involving persons 16 years of age or older. Vaccine efficacy against Covid-19 was 95%. BNT162b2 had a favorable safety profile in diverse populations.9 These data formed the basis for BNT162b2 emergency or conditional authorizations globally.10 Safety, efficacy, and immunogenicity data from participants 12 to 15 years of age in this trial have been reported.11 Here, we report safety and efficacy findings from a prespecified analysis of the phase 2–3 portion of the trial through approximately 6 months of follow-up. These additional data contributed to the full approval of BNT162b2 in the United States.
Methods
Objectives, Participants, and Oversight
This randomized, placebo-controlled, observer-blinded, phase 1–2–3 trial assessed the safety, efficacy, and immunogenicity of the BNT162b2 vaccine in adolescents and adults. The current report of the findings from the phase 2–3 portion of the trial focuses on safety assessments among participants 16 years of age or older and prespecified assessments of vaccine efficacy among participants 12 years of age or older through 6 months of follow-up after immunization. Because the enrollment of participants 12 to 15 years of age began on October 15, 2020, 6-month postimmunization data are currently unavailable for this age cohort. Shorter-duration safety, immunogenicity, and efficacy data for participants 12 to 15 years of age are reported separately11; however, data for this cohort are included in the analyses of vaccine efficacy in the overall population (all participants ≥12 years of age) reported here.
Participants who were healthy or had stable chronic medical conditions were eligible. An active immunocompromising condition or recent immunosuppressive therapy was an exclusion criterion. Participants with a history of Covid-19 were excluded, although evidence of current or previous SARS-CoV-2 infection on laboratory testing of trial-obtained samples was not an exclusion criterion. Trial-related responsibilities and ethical conduct are summarized in the Supplementary Appendix, available with the full text of this article at NEJM.org. The protocol contains additional details of the trial and is available at NEJM.org. The first draft of the manuscript was written by the fourth author. The authors had the opportunity to review the data included in this article and confirm the accuracy of the data presented through the specified data cutoff date. The authors vouch for the accuracy and completeness of the data and for the fidelity of the trial to the protocol.
Procedures
The participants were randomly assigned in a 1:1 ratio to receive two 30-μg intramuscular injections, 21 days apart, of BNT162b2 (0.3 ml volume per dose) or saline placebo. Randomization was performed with an interactive Web-based system. Starting in December 2020, after BNT162b2 became available under emergency or conditional use authorizations, participants 16 years of age or older who became eligible for Covid-19 vaccination according to national or local recommendations were given the option to learn their trial assignment. Those who had been randomly assigned to receive placebo were offered BNT162b2. After unblinding of the group assignments, participants were followed in an open-label trial period.
Safety
Safety end points included solicited, prespecified local reactions, systemic events, and antipyretic or pain medication use during the first 7 days after receipt of each vaccine or placebo dose, which were recorded in an electronic diary; unsolicited adverse events after receipt of the first dose through 1 month after the second dose; and serious adverse events after receipt of the first dose through 1 and 6 months after the second dose was received. Safety data are presented for the blinded follow-up and open-label periods.
Efficacy
BNT162b2 efficacy against laboratory-confirmed Covid-19 with an onset of 7 days or more after the second dose was assessed and summarized descriptively in participants without serologic or virologic evidence of SARS-CoV-2 infection within 7 days after the second dose and in participants with or without evidence of previous infection. Efficacy against severe Covid-19 was also assessed. Lineages of SARS-CoV-2 detected in midturbinate specimens are reported here for Covid-19 cases that occurred 7 days or more after the second dose in South African participants without evidence of previous infection. Methods for determining SARS-CoV-2 lineages and case definitions for confirmed and severe cases of Covid-19 are summarized in the Supplementary Appendix.
Statistical Analysis
The analysis populations are summarized in Table S1 in the Supplementary Appendix. Safety analyses included participants 16 years of age or older without known human immunodeficiency virus (HIV) infection who provided informed consent and received at least one BNT162b2 or placebo dose. The results of the safety analyses, which are descriptive and not based on formal hypothesis testing, are presented as counts, percentages, and associated Clopper–Pearson 95% confidence intervals for adverse events, according to terms in the Medical Dictionary for Regulatory Activities, version 23.1, and reactogenicity events for each trial group. Safety data that were reported up to March 13, 2021, are summarized here. The 95% confidence intervals in this report were not adjusted for multiplicity.
The analysis of vaccine efficacy during the blinded period of the trial included all participants 12 years of age or older without known HIV infection who received at least one BNT162b2 or placebo dose. Vaccine efficacy was calculated as 100×(1–IRR), where IRR (incidence rate ratio) is the ratio of the rate (number per 1000 person-years of follow-up) of confirmed cases of Covid-19 in the BNT162b2 group to the corresponding rate in the placebo group. Descriptive analyses of vaccine efficacy were performed and associated 95% confidence intervals were calculated with the use of the Clopper–Pearson method, with adjustment for surveillance time, which accounts for potential differential follow-up between the two trial groups. As described in the statistical analysis plan, available with the protocol, hypothesis-testing analyses were performed with the use of a Bayesian approach, and the descriptive analyses presented here were performed with a frequentist approach for clarity of communication. Because the percentage of participants who reported symptoms but were missing a valid polymerase-chain-reaction test result was small and slightly higher in the placebo group, data for these participants were not imputed in the analysis.
The previously reported primary efficacy objective was achieved on the basis of an analysis of 170 accrued cases of Covid-19 that could be evaluated (data cutoff date, November 14, 2020).9 The current report provides updated efficacy analyses that were performed with data from cases that had accrued up to March 13, 2021.
Results
Participants
Between July 27, 2020, and October 29, 2020, a total of 45,441 participants 16 years of age or older underwent screening, and 44,165 underwent randomization at 152 sites (130 sites in the United States, 1 site in Argentina, 2 sites in Brazil, 4 sites in South Africa, 6 sites in Germany, and 9 sites in Turkey) in the phase 2–3 portion of the trial. Of these participants, 44,060 received at least one dose of BNT162b2 (22,030 participants) or placebo (22,030), and 98% (21,759 in the BNT162b2 group and 21,650 in the placebo group) received the second dose (Figure 1). During the blinded period of the trial, 51% of the participants in each group had 4 to less than 6 months of follow-up after the second dose; 8% of the participants in the BNT162b2 group and 6% of those in the placebo group had 6 months of follow-up or more after the second dose. During the combined blinded and open-label periods, 55% of the participants in the BNT162b2 group had 6 months of follow-up or more after the second dose. A total of 49% of the participants were female, 82% were White, 10% were Black, and 26% were Hispanic or Latinx; the median age was 51 years. A total of 34% of the participants had a body-mass index (the weight in kilograms divided by the square of the height in meters) of 30.0 or more, 21% had at least one underlying medical condition, and 3% had baseline evidence of a previous or current SARS-CoV-2 infection (Table 1 and Table S2).
Figure 1

Screening, Randomization, and Follow-up.
The diagram represents all enrolled participants 16 years of age or older through the data cutoff date (March 13, 2021). The diagram includes two deaths that occurred after the second dose in human immunodeficiency virus (HIV)–infected participants (one in the BNT162b2 group and one in the placebo group; these deaths were not reported in the Results section of this article because the analysis of HIV-infected participants is being conducted separately). Information on the screening, randomization, and follow-up of the participants 12 to 15 years of age has been reported previously.11
Table 1

| Characteristic | BNT162b2 (N=22,026) |
Placebo (N=22,021) |
Total (N=44,047) |
|---|---|---|---|
| Sex — no. (%) | |||
| Male | 11,322 (51.4) | 11,098 (50.4) | 22,420 (50.9) |
| Female | 10,704 (48.6) | 10,923 (49.6) | 21,627 (49.1) |
| Race or ethnic group — no. (%)† | |||
| White | 18,056 (82.0) | 18,064 (82.0) | 36,120 (82.0) |
| Black or African American | 2,098 (9.5) | 2,118 (9.6) | 4,216 (9.6) |
| Asian | 952 (4.3) | 942 (4.3) | 1,894 (4.3) |
| American Indian or Alaska Native | 221 (1.0) | 217 (1.0) | 438 (1.0) |
| Native Hawaiian or other Pacific Islander | 58 (0.3) | 32 (0.1) | 90 (0.2) |
| Multiracial | 550 (2.5) | 533 (2.4) | 1,083 (2.5) |
| Not reported | 91 (0.4) | 115 (0.5) | 206 (0.5) |
| Ethnicity† | |||
| Hispanic or Latinx | 5,704 (25.9) | 5,695 (25.9) | 11,399 (25.9) |
| Not reported | 111 (0.5) | 114 (0.5) | 225 (0.5) |
| Country — no. (%) | |||
| Argentina | 2,883 (13.1) | 2,881 (13.1) | 5,764 (13.1) |
| Brazil | 1,452 (6.6) | 1,448 (6.6) | 2,900 (6.6) |
| Germany | 249 (1.1) | 250 (1.1) | 499 (1.1) |
| South Africa | 401 (1.8) | 399 (1.8) | 800 (1.8) |
| Turkey | 249 (1.1) | 249 (1.1) | 498 (1.1) |
| United States | 16,792 (76.2) | 16,794 (76.3) | 33,586 (76.3) |
| Age group at vaccination — no. (%) | |||
| 16–55 yr | 13,069 (59.3) | 13,095 (59.5) | 26,164 (59.4) |
| >55 yr | 8,957 (40.7) | 8,926 (40.5) | 17,883 (40.6) |
| Age at vaccination — yr | |||
| Median | 51.0 | 51.0 | 51.0 |
| Range | 16–89 | 16–91 | 16–91 |
| SARS-CoV-2 status — no. (%)‡ | |||
| Positive | 689 (3.1) | 716 (3.3) | 1,405 (3.2) |
| Negative | 21,185 (96.2) | 21,180 (96.2) | 42,365 (96.2) |
| Missing data | 152 (0.7) | 125 (0.6) | 277 (0.6) |
| Body-mass index — no. (%)§ | |||
| ≥30.0: obese | 7,543 (34.2) | 7,629 (34.6) | 15,172 (34.4) |
| Missing data | 7 (<1) | 6 (<1) | 13 (<1) |
Demographic Characteristics of the Participants at Baseline.*
*
Data are summarized for participants 16 years of age or older in the safety population. The demographic characteristics of participants 12 to 15 years of age were reported previously.11 Percentages may not total 100 because of rounding. SARS-CoV-2 denotes severe acute respiratory syndrome coronavirus 2.
†
Race and ethnicity were reported by the participants. The categories shown are those that were used to collect the data.
‡
Positive status was defined as a positive N-binding antibody result or a positive nucleic acid amplification test (NAAT) result at visit 1 or medical history of coronavirus disease 2019 (Covid-19). Negative status was defined as a negative N-binding antibody result or a negative NAAT result at visit 1 and no medical history of Covid-19.
§
The body-mass index is the weight in kilograms divided by the square of the height in meters.
Between October 15, 2020, and January 12, 2021, a total of 2306 participants 12 to 15 years of age underwent screening, and 2264 underwent randomization at 29 U.S. sites. Of these participants, 2260 received at least one dose of BNT162b2 (1131 participants) or placebo (1129), and 99% (1124 in the BNT162b2 group and 1117 in the placebo group) received the second dose.11 Among participants who received at least one dose of BNT162b2 or placebo, 58% had at least 2 months of follow-up after the second dose, 49% were female, 86% were White, 5% were Black, and 12% were Hispanic or Latinx. Full details of the demographic characteristics of the participants have been reported previously.11
Safety
Reactogenicity
The subgroup that was evaluated for reactogenicity in the current report, in which reactions were reported in an electronic diary, included 9839 participants 16 years of age or older. In this subgroup, 8183 participants had been included in the previous analysis, and 1656 were enrolled after the data cutoff for that analysis.9 The reactogenicity profile of BNT162b2 in this expanded subgroup did not differ substantially from that described previously.9 This subgroup included 364 participants who had evidence of previous SARS-CoV-2 infection, 9426 who did not have evidence, and 49 who lacked the data needed to determine previous infection status.
More participants in the BNT162b2 group than in the placebo group reported local reactions, the most common of which was mild-to-moderate pain at the injection site (Fig. S1A). Local reactions were reported with similar frequency among the participants with or without evidence of previous SARS-CoV-2 infection, and the reactions were of similar severity. No local reactions of grade 4 (according to the guidelines of the Center for Biologics Evaluation and Research12) were reported.
More participants in the BNT162b2 group than in the placebo group reported systemic events, the most common of which was fatigue (Fig. S1B). Systemic events were mostly mild to moderate in severity, but there were occasional severe events. Systemic reactogenicity was similar among those with or without evidence of previous SARS-CoV-2 infection, although BNT162b2 recipients with evidence of previous infection reported systemic events more often after receipt of the first dose, and those without evidence reported systemic events more often after receipt of the second dose. For example, 12% of recipients with evidence of previous SARS-CoV-2 infection and 3% of those without evidence reported fever after receipt of the first dose; 8% of those with evidence of previous infection and 15% of those without evidence reported fever after the second dose. The highest temperature reported was a transient fever of higher than 40.0°C on day 2 after the second dose in a BNT162b2 recipient without evidence of previous infection.
Adverse Events
Analyses of adverse events during the blinded period included 43,847 participants 16 years of age or older (Table S3). Reactogenicity events among the participants who were not in the reactogenicity subgroup were reported as adverse events, which resulted in imbalances between the BNT162b2 group and the placebo group with respect to adverse events (30% vs. 14%), related adverse events (24% vs. 6%), and severe adverse events (1.2% vs. 0.7%). New adverse events attributable to BNT162b2 that were not previously identified in earlier reports included decreased appetite, lethargy, asthenia, malaise, night sweats, and hyperhidrosis. Few participants had serious adverse events or adverse events that led to trial withdrawal. No new serious adverse events were considered by the investigators to be related to BNT162b2 after the data cutoff date of the previous report.9
During the combined blinded and open-label periods, cumulative safety data during follow-up were available through 6 months after the second dose for 12,006 participants who were originally randomly assigned to the BNT162b2 group. No new safety signals relative to the previous report were observed during the longer follow-up period in the current report, which included open-label observation of the original BNT162b2 recipients and placebo recipients who received BNT162b2 after unblinding.9
During the blinded, placebo-controlled period, 15 participants in the BNT162b2 group and 14 in the placebo group died; during the open-label period, 3 participants in the BNT162b2 group and 2 in the original placebo group who received BNT162b2 after unblinding died. None of these deaths were considered to be related to BNT162b2 by the investigators. Causes of death were balanced between BNT162b2 and placebo groups (Table S4).
Safety monitoring will continue according to the protocol for 2 years after the second dose for participants who originally received BNT162b2 and for 18 months after the second BNT162b2 dose for placebo recipients who received BNT162b2 after unblinding.
Efficacy
Among 42,094 participants 12 years of age or older who could be evaluated and had no evidence of previous SARS-CoV-2 infection, Covid-19 with an onset of 7 days or more after the second dose was observed in 77 vaccine recipients and in 850 placebo recipients up to the data cutoff date (March 13, 2021), corresponding to a vaccine efficacy of 91.3% (95% confidence interval [CI], 89.0 to 93.2) (Table 2). Among 44,486 participants with or without evidence of previous infection who could be evaluated, cases of Covid-19 were observed in 81 vaccine recipients and in 873 placebo recipients, corresponding to a vaccine efficacy of 91.1% (95% CI, 88.8 to 93.0).
Table 2

| Efficacy End Point | BNT162b2 | Placebo | Vaccine Efficacy (95% CI)‡ |
||||
|---|---|---|---|---|---|---|---|
| No. of Cases |
Surveillance Time† |
No. at Risk |
No. of Cases |
Surveillance Time† |
No. at Risk |
||
| 1000 person-yr | 1000 person-yr | percent | |||||
| (N=20,998) | (N=21,096) | ||||||
| First occurrence of Covid-19 from 7 days after receipt of the second dose among participants without evidence of previous infection | 77 | 6.247 | 20,712 | 850 | 6.003 | 20,713 | 91.3 (89.0–93.2) |
| (N=22,166) | (N=22,320) | ||||||
| First occurrence of Covid-19 from 7 days after receipt of the second dose among participants with or without evidence of previous infection | 81 | 6.509 | 21,642 | 873 | 6.274 | 21,689 | 91.1 (88.8–93.0) |
Vaccine Efficacy against Covid-19 from 7 Days after Receipt of the Second Dose during the Blinded, Placebo-Controlled Follow-up Period.*
*
This analysis included participants who had no serologic or virologic evidence (within 7 days after receipt of the second dose) of previous SARS-CoV-2 infection (i.e., negative N-binding antibody [serum] test at visit 1 and SARS-CoV-2 not detected by NAAT [nasal swab] at visits 1 and 2) and had a negative NAAT at any unscheduled visit up to 7 days after receipt of the second dose.
†
The surveillance time is the total time (in 1000 person-years) at risk for the given end point across all participants within each group. The time period for the accrual of Covid-19 cases was from 7 days after the second dose to the end of the surveillance period.
‡
Vaccine efficacy was calculated as 100×(1–IRR), where IRR (incidence rate ratio) is the ratio of the rate (number per 1000 person-years of follow-up) of confirmed cases of Covid-19 in the BNT162b2 group to the corresponding rate in the placebo group. The 95% confidence interval for vaccine efficacy was derived with the use of the Clopper–Pearson method, with adjustment for surveillance time.
Among the participants with evidence of previous SARS-CoV-2 infection based on a positive baseline N-binding antibody test, Covid-19 was observed in 2 vaccine recipients after the first dose and in 7 placebo recipients. Among the participants with evidence of previous SARS-CoV-2 infection based on a positive nucleic acid amplification test at baseline, cases of Covid-19 were observed in 10 vaccine recipients and in 9 placebo recipients (Table S5). Covid-19 was less common among the placebo recipients with positive N-binding antibodies at trial entry (7 of 542 participants, for an incidence of 1.3%) than among those without evidence of infection at trial entry (1015 of 21,521, for an incidence of 4.7%); these findings indicate that previous infection conferred approximately 72.6% protection.
Among the participants with or without evidence of previous infection, cases of Covid-19 were observed in 46 vaccine recipients and in 110 placebo recipients from receipt of the first dose up to receipt of the second dose, corresponding to a vaccine efficacy of 58.4% (95% CI, 40.8 to 71.2) (Figure 2). During the interval from the approximate start of observed protection at 11 days after receipt of the first dose up to receipt of the second dose, vaccine efficacy increased to 91.7% (95% CI, 79.6 to 97.4). From its peak after the second dose, observed vaccine efficacy declined. From 7 days to less than 2 months after the second dose, vaccine efficacy was 96.2% (95% CI, 93.3 to 98.1); from 2 months to less than 4 months after the second dose, vaccine efficacy was 90.1% (95% CI, 86.6 to 92.9); and from 4 months after the second dose to the data cutoff date, vaccine efficacy was 83.7% (95% CI, 74.7 to 89.9).
Figure 2

Efficacy of BNT162b2 against Covid-19 after Receipt of the First Dose (Blinded Follow-up Period).
The top of the figure shows the cumulative incidence curves for the first occurrence of coronavirus disease 2019 (Covid-19) after receipt of the first dose (efficacy analysis population of participants ≥12 years of age who could be evaluated). Each symbol represents Covid-19 cases starting on a given day, and filled symbols represent severe Covid-19 cases. Because of overlapping dates, some symbols represent more than one case. The inset shows the same data on an enlarged y axis through 21 days. The bottom of the figure shows the time intervals for the first occurrence of Covid-19 in the efficacy analysis population, as well as the surveillance time, which is given as the total time (in 1000 person-years) at risk for the given end point across all participants within each group. The time period for the accrual of Covid-19 cases was from after receipt of the first dose to the end of the surveillance period for the overall row and from the start to the end of the range stated for each time interval. Vaccine efficacy was calculated as 100×(1–IRR), where IRR (incidence rate ratio) is the ratio of the rate (number per 1000 person-years of follow-up) of confirmed cases of Covid-19 in the BNT162b2 group to the corresponding rate in the placebo group. The 95% confidence interval for vaccine efficacy was derived with the use of the Clopper–Pearson method, with adjustment for surveillance time.
Severe Covid-19, as defined by the Food and Drug Administration,13 with an onset after receipt of the first dose occurred in 31 participants, of whom 30 were placebo recipients; this finding corresponds with a vaccine efficacy of 96.7% (95% CI, 80.3 to 99.9) against severe Covid-19 (Figure 2 and Table S6). Although the trial was not powered to definitively assess efficacy according to subgroup, supplemental analyses indicated that vaccine efficacy after the second dose in subgroups defined according to age, sex, race, ethnic group, presence or absence of coexisting medical conditions, and country was generally consistent with that observed in the overall population (Table 3 and Table S7).
Table 3

| First Occurrence of Covid-19 after Receipt of the First Dose | BNT162b2 (N=20,998) |
Placebo (N=21,096) |
Vaccine Efficacy (95% CI)‡ |
||||
|---|---|---|---|---|---|---|---|
| No. of Cases |
Surveillance Time† |
No. at Risk |
No. of Cases |
Surveillance Time† |
No. at Risk |
||
| 1000 person-yr | 1000 person-yr | percent | |||||
| Overall population | 77 | 6.247 | 20,712 | 850 | 6.003 | 20,713 | 91.3 (89.0 to 93.2) |
| Age group — yr | |||||||
| 16 or 17 | 0 | 0.061 | 342 | 10 | 0.057 | 331 | 100 (58.2 to 100) |
| 16 to 55 | 52 | 3.593 | 11,517 | 568 | 3.439 | 11,533 | 91.2 (88.3 to 93.5) |
| ≥55 | 25 | 2.499 | 8,194 | 266 | 2.417 | 8,208 | 90.9 (86.3 to 94.2) |
| ≥65 | 7 | 1.233 | 4,192 | 124 | 1.202 | 4,226 | 94.5 (88.3 to 97.8) |
| ≥75 | 1 | 0.239 | 842 | 26 | 0.237 | 847 | 96.2 (76.9 to 99.9) |
| Sex | |||||||
| Male | 42 | 3.246 | 10,637 | 399 | 3.047 | 10,433 | 90.1 (86.4 to 93.0) |
| Female | 35 | 3.001 | 10,075 | 451 | 2.956 | 10,280 | 92.4 (89.2 to 94.7) |
| Race or ethnic group§ | |||||||
| White | 67 | 5.208 | 17,186 | 747 | 5.026 | 17,256 | 91.3 (88.9 to 93.4) |
| Black or African American | 4 | 0.545 | 1,737 | 48 | 0.527 | 1,737 | 91.9 (78.0 to 97.9) |
| Asian | 3 | 0.260 | 946 | 23 | 0.248 | 934 | 87.6 (58.9 to 97.6) |
| American Indian or Alaska Native | 0 | 0.041 | 186 | 3 | 0.037 | 176 | 100 (–119.0 to 100) |
| Native Hawaiian or other Pacific Islander | 0 | 0.015 | 54 | 1 | 0.008 | 30 | 100 (–1961.2 to 100) |
| Multiracial | 3 | 0.151 | 518 | 22 | 0.128 | 476 | 88.5 (61.6 to 97.8) |
| Not reported | 0 | 0.026 | 85 | 6 | 0.030 | 104 | 100 (2.8 to 100) |
| Ethnicity§ | |||||||
| Hispanic or Latinx | 29 | 1.786 | 5,161 | 241 | 1.711 | 5,120 | 88.5 (83.0 to 92.4) |
| Non-Hispanic and non-Latinx | 47 | 4.429 | 15,449 | 609 | 4.259 | 15,484 | 92.6 (90.0 to 94.6) |
| Not reported | 1 | 0.032 | 102 | 0 | 0.033 | 109 | NA |
| Country | |||||||
| Argentina | 15 | 1.012 | 2,600 | 108 | 0.986 | 2,586 | 86.5 (76.7 to 92.7) |
| Brazil | 12 | 0.406 | 1,311 | 80 | 0.374 | 1,293 | 86.2 (74.5 to 93.1) |
| Germany | 0 | 0.047 | 236 | 1 | 0.048 | 242 | 100 (–3874.2 to 100) |
| South Africa | 0 | 0.080 | 291 | 9 | 0.074 | 276 | 100 (53.5 to 100) |
| Turkey | 0 | 0.027 | 228 | 5 | 0.025 | 222 | 100 (–0.1 to 100) |
| United States | 50 | 4.674 | 16,046 | 647 | 4.497 | 16,046 | 92.6 (90.1 to 94.5) |
Vaccine Efficacy against Covid-19 up to 7 Days after Receipt of the Second Dose among Participants without Evidence of Infection.*
*
This analysis of vaccine efficacy during the blinded, placebo-controlled follow-up period included all participants who had undergone randomization and were 12 years of age or older without baseline evidence of previous infection who had undergone randomization. NA denotes not applicable.
†
Surveillance time is the total time (in 1000 person-years) at risk for the given end point across all participants within each group. The time period for the accrual of Covid-19 cases was from 7 days after the second dose to the end of the surveillance period.
‡
Vaccine efficacy was calculated as 100×(1–IRR). The 95% confidence interval for vaccine efficacy was derived with the use of the Clopper–Pearson method, with adjustment for surveillance time.
§
Race and ethnicity were reported by the participants. The categories shown are those that were used to collect the data.
Given the concern about the SARS-CoV-2 B.1.351 (or beta) variant, which appears to be neutralized less efficiently by BNT162b2-immune sera than many other lineages,14 whole-viral-genome sequencing was performed on midturbinate samples from Covid-19 cases observed in South Africa, where this lineage was prevalent. Nine cases of Covid-19 were observed in South African participants without evidence of previous SARS-CoV-2 infection, all of whom were placebo recipients; this finding corresponds with a vaccine efficacy of 100% (95% CI, 53.5 to 100) (Table 3). Midturbinate specimens from 8 of 9 cases contained sufficient viral RNA for whole-genome sequencing. All viral genomes were the beta variant (Global Initiative on Sharing All Influenza Data accession codes are provided in the Supplementary Appendix).
Discussion
In this update to the preliminary safety and efficacy report of two 30-μg doses, at 21 days apart, of BNT162b2, 91.1% vaccine efficacy against Covid-19 was observed from 7 days to 6 months after the second dose in participants 12 years of age or older. Vaccine efficacy against severe disease with an onset after receipt of the first dose was approximately 97%. This finding, combined with the totality of available evidence, including real-world effectiveness data,15-18 alleviates theoretical concerns over potential enhancement of vaccine-mediated disease.19
The benefit of BNT162b2 immunization started approximately 11 days after receipt of the first dose, with 91.7% vaccine efficacy from 11 days after receipt of the first dose up to receipt of the second dose. The trial cannot provide information on persistence of protection after a single dose, because 99% of the participants received the second dose as scheduled during the blinded trial period. A recent trial showed that although nonneutralizing viral antigen–binding antibody levels rise between the first and second BNT162b2 dose, serum neutralizing titers are low or undetectable during this interval.20 Early protection against Covid-19 without strong serum neutralization indicates that neutralizing titers alone do not appear to explain early BNT162b2-mediated protection from Covid-19. Other immune mechanisms (e.g., innate immune responses, CD4+ or CD8+ T-cell responses, B-cell memory responses, and antibody-dependent cytotoxicity) may contribute to protection.21-26
Efficacy peaked at 96.2% during the interval from 7 days to less than 2 months after the second dose and declined gradually to 83.7% from 4 months after the second dose to the data cutoff date — an average decline of approximately 6% every 2 months. Ongoing follow-up is needed to understand persistence of the vaccine effect over time, the need for booster dosing, and timing of such a dose. Most participants who initially received placebo have now been immunized with BNT162b2, ending the placebo-controlled period of the trial. Nevertheless, ongoing observation of participants through 2 years in this trial, together with real-world effectiveness data,15-18 will determine whether a booster is likely to be beneficial after a longer interval. Booster trials to evaluate safety and immunogenicity of BNT162b2 are under way to prepare for this possibility.
From 7 days after the second dose, 86 to 100% efficacy was observed across diverse demographic profiles, including age, sex, race or ethnic group, and factors that increase the risk of Covid-19, such as high body-mass index and other coexisting medical conditions. BNT162b2 was also highly efficacious in various geographic regions including North America, Europe, South Africa, and Latin America. Although vaccine efficacy was slightly lower in Latin American countries, BNT162b2 had a high efficacy of approximately 86% in Argentina and Brazil. Circulation of SARS-CoV-2 variants — some of which are associated with more rapid transmission and potentially greater pathogenicity27 — has raised concerns that such variants could evade vaccine-mediated protection. Our studies of in vitro neutralization of a variety of SARS-CoV-2 variants have, to date, showed that all tested BNT162b2-immune sera neutralize all tested variants.14,28–32 The beta variant, which has shown the greatest reduction in neutralization and was the dominant strain in South Africa during the reported observation period, is still neutralized at serum titers higher than those observed at the onset of protection against Covid-19 after the first vaccine dose.9,14,20 We found that BNT162b2 had an observed efficacy of 100% (95% CI, 53.5 to 100) against Covid-19 in South Africa (9 cases occurred in the placebo recipients and 0 cases in the BNT162b2 recipients), and 8 of 9 cases for which sequence information could be obtained involved the beta variant of SARS-CoV-2.
Safety data are now available for approximately 44,000 participants 16 years of age or older; 12,006 participants have at least 6 months of safety follow-up data after a second BNT162b2 dose. The safety profile observed at a median of 2 months after immunization was confirmed through 6 months after immunization in the current analysis. No cases of myocarditis were noted.
Before immunization, 3% of the participants 16 years of age or older had evidence of SARS-CoV-2 infection. Although this group had a slightly higher incidence of systemic reactogenicity events after receipt of the first dose than those without evidence of previous infection, the group had a slightly lower incidence of reactogenicity events after the second dose than those without previous infection. Thus, there was minimal observed difference in the overall reactogenicity profile on the basis of infection status at baseline. Nine cases of Covid-19 were observed among participants with previous serologically defined natural infection: two cases were observed among the vaccine recipients and seven among the placebo recipients. These data support the current practice of immunizing without screening for evidence of previous infection.
This report has several limitations. Duration of protection and safety data that could be collected in a blinded, placebo-controlled manner were limited by the ethical and practical need to immunize eligible initial placebo recipients under emergency use authorization and according to the recommendations of public health authorities. The data presented here do not address whether vaccination prevents asymptomatic infection; however, evaluation of that question is ongoing in this trial, and real-world data suggest that BNT162b2 prevents asymptomatic infection.33,34 Preliminary analyses of breakthrough cases have not yet identified a correlate of protection, since vaccine protection rates remain high. This report does not address vaccine efficacy and safety in pregnant women and in children younger than 12 years of age. Studies evaluating BNT162b2 in these populations are ongoing.
The data in this report show that BNT162b2 prevents Covid-19 effectively for up to 6 months after the second dose across diverse populations, despite the emergence of SARS-CoV-2 variants, including the beta variant, and the vaccine continues to show a favorable safety profile.
Notes
This article was published on September 15, 2021, at NEJM.org.
A data sharing statement provided by the authors is available with the full text of this article at NEJM.org.
Supported by BioNTech and Pfizer.
Disclosure forms provided by the authors are available with the full text of this article at NEJM.org.
We thank all the participants who volunteered for this trial; the investigators in the C4591001 Clinical Trial Group for their contributions; the members of our data monitoring committee (Jonathan Zenilman [chair], Robert Belshe, Kathryn Edwards, Stephen Self, and Lawrence Stanberry) for their review of the data; Tricia Newell, Sheena Hunt, and Philippa Jack of ICON (North Wales, PA) for editorial support, which was funded by Pfizer; the following Pfizer staff: Greg Adams, Negar Aliabadi, Mohanish Anand, Fred Angulo, Ayman Ayoub, Melissa Bishop-Murphy, Mark Boaz, Christopher Bowen, Donna Boyce, Sarah Burden, Andrea Cawein, Patrick Caubel, Darren Cowen, Kimberly Ann Cristall, Michael Cruz, Daniel Curcio, Gabriela Dávila, Carmel Devlin, Gokhan Duman, Niesha Foster, Maja Gacic, Juleen Gayed, Ahmed Hassan, Luis Jodar, Stephen Kay, William Lam, Esther Ladipo, Joaquina Maria Lazaro, Marie-Pierre Hellio Le Graverand-Gastineau, Kwok Lee, Zhenghui Li, Jacqueline Lowenberg, Hua Ma, Rod MacKenzie, Robert Maroko, Jason McKinley, Tracey Mellelieu, Neda Aghajani Memar, Farheen Muzaffar, Brendan O’Neill, Jason Painter, Elizabeth Paulukonis, Allison Pfeffer, Katie Puig, Kimberly Rarrick, Balaji Prabu Raja, Christine Rainey, Kellie Lynn Richardson, Elizabeth Rogers, Melinda Rottas, Charulata Sabharwal, Uzma Sarwar, Vilas Satishchandran, Harpreet Seehra, Judy Sewards, Huiqing Si, Helen Smith, David Swerdlow, James Trammel, Elisa Harkins Tull, Sarah Tweedy, Erica Weaver, John Wegner, Jenah West, Christopher Webber, David C. Whritenour, Fae Wooding, Emily Worobetz, Nita Zalavadia, and Liping Zhang, as well as the Vaccines Clinical Assay Team, the Vaccines Assay Development Team, and all the Pfizer colleagues not named here who contributed to the success of this trial; the following BioNTech staff: Corinna Rosenbaum, Christian Miculka, Andreas Kuhn, Ferdia Bates, Paul Strecker, Ruben Rizzi, Martin Bexon, Eleni Lagkadinou, and Alexandra Kemmer-Brück; and Dietmar Katinger and Andreas Wagner at Polymun.
Supplementary Material
Research Summary (nejmoa2110345_research-summary.pdf)
- Download
- 244.61 KB
Protocol (nejmoa2110345_protocol.pdf)
- Download
- 1.96 MB
Supplementary Appendix (nejmoa2110345_appendix.pdf)
- Download
- 460.93 KB
Disclosure Forms (nejmoa2110345_disclosures.pdf)
- Download
- 1.02 MB
Data Sharing Statement (nejmoa2110345_data-sharing.pdf)
- Download
- 71.49 KB
References
1.
COVID-19 dashboard. 2021 (https://coronavirus.jhu.edu/map.html).
2.
Food and Drug Administration. COVID-19 vaccines. Silver Spring, MD: Food and Drug Administration. 2021 (https://www.fda.gov/emergency-preparedness-and-response/coronavirus-disease-2019-covid-19/covid-19-vaccines).
3.
Medicines and Healthcare Products Regulatory Agency. Decision: conditions of authorisation for COVID-19 vaccine AstraZeneca (regulation 174). 2021 (https://www.gov.uk/government/publications/regulatory-approval-of-covid-19-vaccine-astrazeneca/conditions-of-authorisation-for-covid-19-vaccine-astrazeneca).
4.
Baraniuk C. What do we know about China’s covid-19 vaccines? BMJ 2021;373:n912-n912.
5.
Baraniuk C. Covid-19: what do we know about Sputnik V and other Russian vaccines? BMJ 2021;372:n743-n743.
6.
Pardi N, Tuyishime S, Muramatsu H, et al. Expression kinetics of nucleoside-modified mRNA delivered in lipid nanoparticles to mice by various routes. J Control Release 2015;217:345-351.
7.
Karikó K, Muramatsu H, Welsh FA, et al. Incorporation of pseudouridine into mRNA yields superior nonimmunogenic vector with increased translational capacity and biological stability. Mol Ther 2008;16:1833-1840.
8.
Wrapp D, Wang N, Corbett KS, et al. Cryo-EM structure of the 2019-nCoV spike in the prefusion conformation. Science 2020;367:1260-1263.
9.
Polack FP, Thomas SJ, Kitchin N, et al. Safety and efficacy of the BNT162b2 mRNA Covid-19 vaccine. N Engl J Med 2020;383:2603-2615.
10.
Pfizer, BioNTech. Pfizer-BioNTech COVID-19 vaccine. FDA briefing document. Presented at the Vaccines and Related Biological Products Advisory Committee Meeting, virtual, December 10, 2020 (https://www.fda.gov/media/144245/download).
11.
Frenck RW Jr, Klein NP, Kitchin N, et al. Safety, immunogenicity, and efficacy of the BNT162b2 Covid-19 vaccine in adolescents. N Engl J Med 2021;385:239-250.
12.
Guidance for industry: toxicity grading scale for healthy adult and adolescent volunteers enrolled in preventive vaccine clinical trials. Rockville, MD: Center for Biologics Evaluation and Research. September 2007 (https://www.fda.gov/media/73679/download).
13.
COVID-19: developing drugs and biological products for treatment or prevention: guidance for industry. Silver Spring, MD: Food and Drug Administration. May 2020 (https://www.fda.gov/regulatory-information/search-fda-guidance-documents/covid-19-developing-drugs-and-biological-products-treatment-or-prevention).
14.
Liu Y, Liu J, Xia H, et al. Neutralizing activity of BNT162b2-elicited serum. N Engl J Med 2021;384:1466-1468.
15.
Haas EJ, Angulo FJ, McLaughlin JM, et al. Impact and effectiveness of mRNA BNT162b2 vaccine against SARS-CoV-2 infections and COVID-19 cases, hospitalisations, and deaths following a nationwide vaccination campaign in Israel: an observational study using national surveillance data. Lancet 2021;397:1819-1829.
16.
Abu-Raddad LJ, Chemaitelly H, Butt AA. Effectiveness of the BNT162b2 Covid-19 vaccine against the B.1.1.7 and B.1.351 variants. N Engl J Med 2021;385:187-189.
17.
Lopez Bernal J, Andrews N, Gower C, et al. Effectiveness of the Pfizer-BioNTech and Oxford-AstraZeneca vaccines on covid-19 related symptoms, hospital admissions, and mortality in older adults in England: test negative case-control study. BMJ 2021;373:n1088-n1088.
18.
Vasileiou E, Simpson CR, Shi T, et al. Interim findings from first-dose mass COVID-19 vaccination roll-out and COVID-19 hospital admissions in Scotland: a national prospective cohort study. Lancet 2021;397:1646-1657.
19.
Haynes BF, Corey L, Fernandes P, et al. Prospects for a safe COVID-19 vaccine. Sci Transl Med 2020;12(568):eabe0948-eabe0948.
20.
Walsh EE, Frenck RW Jr, Falsey AR, et al. Safety and immunogenicity of two RNA-based Covid-19 vaccine candidates. N Engl J Med 2020;383:2439-2450.
21.
Sahin U, Muik A, Vogler I, et al. BNT162b2 vaccine induces neutralizing antibodies and poly-specific T cells in humans. Nature 2021;595:572-577.
22.
Goel RR, Apostolidis SA, Painter MM, et al. Distinct antibody and memory B cell responses in SARS-CoV-2 naïve and recovered individuals following mRNA vaccination. Sci Immunol 2021;6(58):eabi6950-eabi6950.
23.
Knudson CJ, Alves-Peixoto P, Muramatsu H, et al. Lipid-nanoparticle-encapsulated mRNA vaccines induce protective memory CD8 T cells against a lethal viral infection. Mol Ther 2021 May 14 (Epub ahead of print).
24.
Tauzin A, Nayrac M, Benlarbi M, et al. A single BNT162b2 mRNA dose elicits antibodies with Fc-mediated effector functions and boost pre-existing humoral and T cell responses. March 18, 2021 (https://www.biorxiv.org/content/10.1101/2021.03.18.435972v1). preprint.
25.
Gallagher KME, Leick MB, Larson RC, et al. SARS-CoV-2 T-cell immunity to variants of concern following vaccination. May 3, 2021 (https://www.biorxiv.org/content/10.1101/2021.05.03.442455v1). preprint.
26.
Painter MM, Mathew D, Goel RR, et al. Rapid induction of antigen-specific CD4+ T cells guides coordinated humoral and cellular immune responses to SARS-CoV-2 mRNA vaccination. April 22, 2021 (https://www.biorxiv.org/content/10.1101/2021.04.21.440862v1). preprint.
27.
Centers for Disease Control and Prevention. SARS-CoV-2 variant classifications and definitions. 2021 (https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/variant-surveillance/variant-info.html#print).
28.
Xie X, Liu Y, Liu J, et al. Neutralization of SARS-CoV-2 spike 69/70 deletion, E484K and N501Y variants by BNT162b2 vaccine-elicited sera. Nat Med 2021;27:620-621.
29.
Zou J, Xie X, Fontes-Garfias CR, et al. The effect of SARS-CoV-2 D614G mutation on BNT162b2 vaccine-elicited neutralization. NPJ Vaccines 2021;6:44-44.
30.
Muik A, Wallisch A-K, Sänger B, et al. Neutralization of SARS-CoV-2 lineage B.1.1.7 pseudovirus by BNT162b2 vaccine-elicited human sera. Science 2021;371:1152-1153.
31.
Liu Y, Liu J, Xia H, et al. BNT162b2-elicited neutralization against new SARS-CoV-2 spike variants. N Engl J Med 2021;385:472-474.
32.
Liu J, Liu Y, Xia H, et al. BNT162b2-elicited neutralization of B.1.617 and other SARS-CoV-2 variants. Nature 2021 June 10 (Epub ahead of print).
33.
Dagan N, Barda N, Kepten E, et al. BNT162b2 mRNA Covid-19 vaccine in a nationwide mass vaccination setting. N Engl J Med 2021;384:1412-1423.
34.
Tande AJ, Pollock BD, Shah ND, et al. Impact of the COVID-19 vaccine on asymptomatic infection among patients undergoing pre-procedural COVID-19 molecular screening. Clin Infect Dis 2021 March 10 (Epub ahead of print).
Information & Authors
Information
Published In
Copyright
Copyright © 2021 Massachusetts Medical Society. All rights reserved.
History
Published online: September 15, 2021
Published in issue: November 4, 2021
Topics
Authors
Affiliations
From the State University of New York, Upstate Medical University, Syracuse (S.J.T.), and Vaccine Research and Development, Pfizer, Pearl River (J.A., A.G., K.A.S., K.K., S.B., W.V.K., D.C., Q.Y., P.L., P.R.D., W.C.G., K.U.J.) — both in New York; Associação Obras Sociais Irmã Dulce and Oswaldo Cruz Foundation, Bahia (E.D.M.), and iTrials-Hospital Militar Central (G.P.M.) and Fundacion INFANT, Buenos Aires (F.P.P.) — all in Brazil; Centro Paulista de Investigação Clinica, São Paulo (C.Z.); Vaccine Research and Development, Pfizer, Hurley, United Kingdom (N.K., S.L., R.B.); Vaccine Research and Development (J.L.P., X.X.) and Worldwide Safety, Safety Surveillance, and Risk Management (D.B.T., S.M.), Pfizer, Collegeville, PA; Global Product Development, Pfizer, Peapack, NJ (S.R.); Cincinnati Children’s Hospital, Cincinnati (R.W.F.); Johns Hopkins Bloomberg School of Public Health, Baltimore (L.L.H.); BioNTech, Mainz (Ö.T., U.Ş.) and Medizentrum Essen Borbeck, Essen (A.S.) — both in Germany; Tiervlei Trial Centre, Karl Bremer Hospital, Cape Town, South Africa (H.N.); Hacettepe University, Ankara, Turkey (S.Ü.); and Worldwide Safety, Safety Surveillance, and Risk Management, Pfizer, Groton, CT (D.B.T., S.M.).
Metrics & Citations
Metrics
Altmetrics
Citations
Export citation
Select the format you want to export the citation of this publication.
Cited by
- Safety and immunogenicity of different booster vaccination schemes for COVID-19 used in El Salvador, Clinical and Experimental Vaccine Research, 13, 1, (35), (2024).https://doi.org/10.7774/cevr.2024.13.1.35
- COVID-19 mRNA Vaccines: Lessons Learned from the Registrational Trials and Global Vaccination Campaign, Cureus, (2024).https://doi.org/10.7759/cureus.52876
- Vogt–Koyanagi–Harada-like presentation: A short case series, Indian Journal of Ophthalmology - Case Reports, 4, 1, (192-196), (2024).https://doi.org/10.4103/IJO.IJO_719_23
- Chimeric Antigen Cytotoxic Receptors for In Vivo Engineering of Tumor-Targeting NK Cells, ImmunoHorizons, 8, 1, (97-105), (2024).https://doi.org/10.4049/immunohorizons.2300099
- Analysis of the COVID-19 model with self-protection and isolation measures affected by the environment, Mathematical Biosciences and Engineering, 21, 4, (4835-4852), (2024).https://doi.org/10.3934/mbe.2024213
- Innate Responses to the Former COVID-19 Vaccine Candidate CVnCoV and Their Relation to Reactogenicity and Adaptive Immunogenicity, Vaccines, 12, 4, (388), (2024).https://doi.org/10.3390/vaccines12040388
- Immunogenicity Parameters of Cancer Patients Receiving the mRNA Vaccine BNT162b2 While Obtaining Radiotherapy: A Longitudinal Cohort Evaluation, Vaccines, 12, 3, (275), (2024).https://doi.org/10.3390/vaccines12030275
- Effect of Platform Type on Clinical Efficacy of SARS-CoV-2 Vaccines in Prime Vaccination Settings: A Systematic Review and Meta-Regression of Randomized Controlled Trials, Vaccines, 12, 2, (130), (2024).https://doi.org/10.3390/vaccines12020130
- The Clinical Impact of SARS-CoV-2 on Hypertrophic Cardiomyopathy, Journal of Cardiovascular Development and Disease, 11, 4, (104), (2024).https://doi.org/10.3390/jcdd11040104
- Enhancing Control of Leishmania infantum Infection: A Multi-Epitope Nanovaccine for Durable T-Cell Immunity, Animals, 14, 4, (605), (2024).https://doi.org/10.3390/ani14040605
- See more
Loading...