Global Burden of Disease

Executive summary
* One of the most important challenges in the field of nutrition has been published in The Lancet. It was a letter challenging the reliability of The Lancet flagship project "The Global Burden of Disease" (GBD).
* The GBD project started in 1990 and has been revised five times since. The project attempts to quantify the health effects of more than 100 diseases and harms, by age, sex and region. It estimates the ill health and deaths that could arise from different disease burdens from pollution to consumption of sugary drinks.
* The letter focused on the dietary assumptions in the most recent GBD report (2019). Substantial changes occurred between the 2017 and 2019 reports and the impact was that deaths attributed to diets high in red meat (not even processed meat) increased 36-fold.
* The key challenges made in the letter were:
1) Was this 36-fold increase reliable?
2) GBD 2019 assumed that any red meat or processed meat intake whatsoever (even one gram a day) was harmful. This in effect declared meat as a toxin. Why? What’s the evidence for this?
3) Standard procedures required by The Lancet were not followed and information was missing. Where is this?
4) Were the lost benefits of meat considered? Given that malnutrition, iron deficiency, vitamin A deficiency and zinc deficiency were recognised as key causes of disease, did the authors balance their view that no red meat should be consumed with the nutrients that this would remove from global diets?
* The authors were given the opportunity to respond to the letter but have not done so. Was GBD 2019 indefensible?
Introduction
One of the most important challenges in the field of nutrition was published in The Lancet on February 25th, 2022. It was a letter written by Alice V Stanton, Frédéric Leroy, Christopher Elliott, Neil Mann, Patrick Wall, and Stefaan De Smet (Ref 1). The letter was called “36-fold higher estimate of deaths attributable to red meat intake in GBD 2019: is this reliable?” It challenged the entire reliability of the Global Burden of Disease (2019) report (Ref 2).
The Global Burden of Disease (GBD) project began in 1990 as a single study commissioned by the World Bank (Ref 3). It attempted to quantify the health effects of more than 100 diseases and harms for 8 regions of the world giving estimates of morbidity (ill health) and mortality (death) by age, sex and region. The first study in 1990 introduced the concept of disability-adjusted life years (DALYs). The DALY concept provided a methodology to capture the entire amount of ill health which would, on average, be incurred during one’s lifetime because of new cases of disease and injury (Ref 4). The lead author from the outset has been Professor Christopher Murray. Interestingly, Murray was the final named author (therefore the senior author) on the EAT Lancet diet report (Ref 5). The first named author on the EAT Lancet diet was Professor Walter Willett.
The GBD study was institutionalized at the World Health Organization and research has mainly been conducted by researchers at Harvard and the WHO (Ref 6).
The GBD study 2010 was published in December 2012 (Ref 7).
The GBD study 2015 was published in October 2016 (Ref 8).
The GBD study 2016 was published in September 2017 (Ref 9).
The GBD study 2017 was published in November 2018 (Ref 10).
The GBD study 2019 was published in October 2020 (Ref 11).
Since and including the GBD 2010 report, the Gates Foundation has funded the work (Ref 12). Gates has invested in processed plant foods (Ref 13).
I have done a podcast with Frédéric (Ref 14) and have found his knowledge about food and global food supply to be highly impressive. I have spoken to Frédéric about this week’s note to get some more background details to the letter. It has taken a long time for the letter to be published. As it is highly critical of a flagship Lancet study (arguably the flagship Lancet study), The Lancet would understandably be reluctant to publish it. Professor Stanton and the other authors were tenacious and the letter has finally been published. The GBD 2019 report authors were invited to submit a response but have declined this opportunity. Perhaps there is no defence to the allegations made.
The GDB 2019
The Global Burden of Disease project places risk in four levels:
– Level 1 represents the overarching categories (behavioural, environmental and occupational, and metabolic);
– Level 2 contains both single risks and risk clusters (such as child and maternal malnutrition);
– Level 3 contains the single risks from within Level 2 risk clusters (such as low birthweight and short gestation); and
– Level 4 takes risks down to the most specific level, such as (continuing with the children theme above) the subcomponents of child growth failure (stunting, wasting, underweight), and suboptimal breastfeeding (discontinued and non-exclusive breastfeeding).
The main findings from the GBD 2019 report were as follows. The leading Level 2 risk factor globally for attributable deaths was high systolic blood pressure (the top number when you have your blood pressure tested). This was estimated to have accounted for 10·8 million deaths (19·2% of all deaths in 2019). This was followed by tobacco (smoked, second-hand, and chewing), which accounted for 8·71 million deaths (15·4% of all deaths in 2019). The leading Level 2 risk factor for attributable disability adjusted life years (DALYs) globally in 2019 was child and maternal malnutrition, which obviously largely affects health in the youngest age groups. This was estimated to have accounted for 295 million DALYs (11·6% of all global DALYs that year). Unsurprisingly, risk factors varied considerably in 2019 between age groups and locations. Among children aged 0–9 years, the three leading risk factors for attributable DALYs were all related to malnutrition. Iron deficiency was the leading risk factor for those aged 10–24 years, alcohol use for those aged 25–49 years, and high systolic blood pressure for those aged 50–74 years and 75 years and older.
The word “meat” appeared only three times in the 27-page GBD 2019 main paper. It appeared twice in the only table in the paper. The table title was “Global age-standardised summary exposure values (SEVs) for both sexes combined in 1990, 2010, and 2019, and annualised rate of change between 1990 and 2019 and 2010 and 2019.” The summary exposure value is on a 0–100 scale where 100 means the entire population is at maximum risk and 0 means everyone in the population is at minimum risk.
Values were reported in the table for everything from a diet low in seafood omega-3 fatty acids, which had an SEV of 93.52 (estimating that the entire population was close to maximum risk for this) to an SEV of 0.19 for drug use (estimating that the entire population was close to minimum risk for this). The SEV for low physical activity jarred with me. It was 3.54. Is it really the case that the global population is at close to minimum risk from low physical activity? The SEVs attributed to a diet high in red meat and a diet high in processed meat were 43.94 and 29.81 respectively.
“A diet high in meat…” What was meant by high? The paper contained two key passages to answer this. On p2, the “research in context” summary box stated: “For dietary risks, the theoretical minimum risk exposure level (TMREL) has been revised based on the new systematic reviews.” On p4, the subheading “Determining the TMREL” opened with “For harmful risk factors… the theoretical minimum risk level was set to 0.” Table 1b of the 386-page Appendix 1 (supplemental file) reported that 92 sources were used in the estimation of relative risks of diets high in red meat (and 41 for processed meat), but these were not listed anywhere (Ref 15).
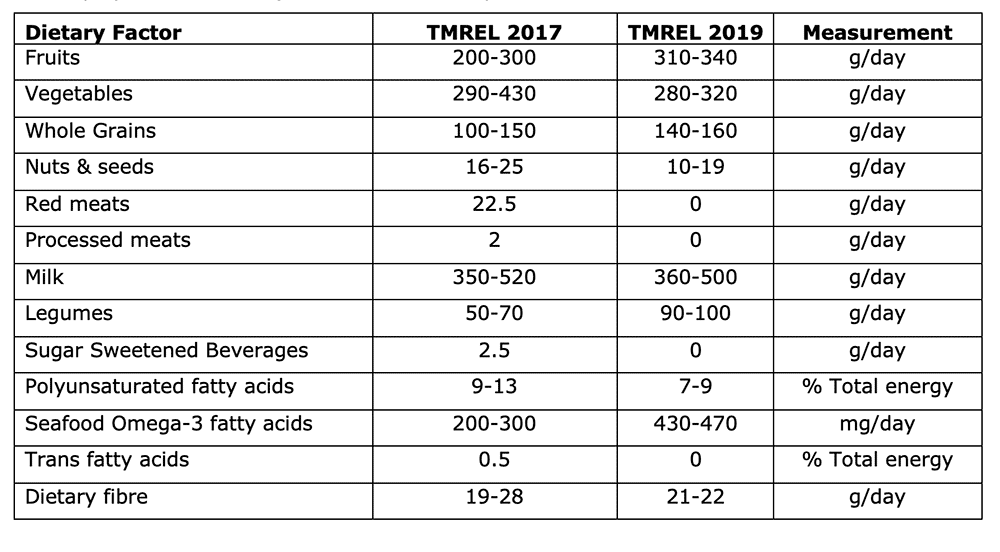
The research web site (Ref 16) could be used to compile the theoretical minimum exposure level. I’ve done this and put the numbers in the table below. Read the numbers as – this is what the researchers think we should consume. GBD 2019 thus recommended that intake of red meat, processed meat, trans fatty acids and sugary drinks should be zero. Fruit intake should be 310-340g/day and vegetable intake 280-320g/day, as examples from the table below. It’s interesting to see what went up (e.g., fruit, legumes) and what went down (e.g., nuts, polyunsaturated fat) between the two reports.
On p22 of the main GBD 2019 paper there was a subheading "Substantial changes compared with GBD 2017." This opened by saying "Compared with GBD 2017, our GBD 2019 estimates of the burden (as measured by percentage of total DALYs) attributable to diet quality in 2017 were 29·7% lower." The third reference to meat appeared just below this: “Although there were changes in the overall burden of diet, there were larger changes in the diet components themselves, particularly the substantial increase in the attributable burden from red meat and the decline in the burden attributable to low vegetable intake.” So, diet overall was less of a risk in 2019 when compared with 2017 but the risk attributed to red meat substantially increased. As the title of the letter by Stanton et al set out “36-fold higher estimate of deaths attributable to red meat intake in GBD 2019: is this reliable?”
The letter
The letter raised the following key issues:
1) The burden of disease (deaths and DALYs) attributed to diets high in red meat increased multiple times over. Was this reliable?
The GBD 2017 analysis attributed 25,000 deaths and 1.3 million DALYs to diets high in red meat. Red meat intake was the least important of 15 dietary risk factors. Then, in GBD 2019, a diet high in red meat was reported to be responsible for 896,000 deaths and 23·9 million DALYs and was considered to be the fifth leading dietary risk factor for attributable DALYs.
As Stanton et al pointed out, that was a 36-fold increase in estimates of attributable deaths and an 18-fold increase in estimates of attributable DALYs. Was this reliable? Especially in the context that disease burdens attributed to diets low in fruit, nuts and seeds, vegetables, seafood omega-3 fatty acids, and polyunsaturated fatty acids declined by more than 50%.
2) Any intake of meat whatsoever was considered harmful. Why?
This vast increase will have been driven by the setting of the theoretical minimum risk exposure level (TMREL) of red and processed meat at zero. The “GBD 2019 Demographics Collaborators”, as the authors are collectively known, set the TMREL for red and processed meat at zero, having decided that it was harmful. Defining harmful intake as anything above zero means that meat is seen as a toxin. Even one gram will do harm. Where is the evidence for this? As Stanton et al challenged “The assumption of a red meat TMREL of zero is counterintuitive given the role of meat in evolutionary diets and in contemporary hunter gatherer populations, in which cardiometabolic diseases were and still are uncommon.” To claim that our most ancestral food is harmful at one gram of intake is absurd.
3) Procedures were not followed; information is missing. Where are the check list items?
The Lancet requires that standardized processes and procedures for academic research are adhered to. GATHER (the Guidelines for Accurate and Transparent Health Estimates Reporting) and PRISMA (Preferred Reporting Items for Systematic reviews and Meta-Analyses) are the two systems of relevance to this research. GATHER comprises a check list of 18 items. Stanton et al claimed that items 3-6 cannot be found and the 92 studies referred to as the source of the relative risks attributed to meat cannot be found. PRISMA comprises a check list of 27 items. Stanton et al reported “We can find no record in the main GBD 2019 Article, nor in the appendices, of the GBD 2019 systematic review protocols, nor of the required peer-reviewed publications that comprehensively address the 27-item PRISMA (2009 or 2020) checklists.”
4) Were the lost benefits of meat considered?
The main GBD 2019 study reported that nutrient deficiencies were key factors in global disease. As reported above, among children aged 0–9 years, the three leading risk factors for attributable DALYs were all related to malnutrition. Iron deficiency was the leading risk factor for those aged 10–24 years. The summary exposure value for 2019 for iron deficiency was 19.57. That’s the global population at measurable risk. The SEVs for vitamin A and zinc deficiency were 15.01 and 8.78 respectively. Risks had all dramatically improved between 1990 and 2019. The summary exposure value for vitamin A deficiency had more than halved. What would happen to global nutrient deficiency if meat were seen as a toxin?
Stanton et al questioned whether the benefits of meat had been taken into account in setting the TMREL at zero. If public health messaging followed the GBD 2019 and set meat intake recommendations at zero, iron deficiency anemia, sarcopenia, and child and maternal nutrition would be impacted. These are already noted as disease issues in the GBD analysis.
The implications
This is one of the most important challenges in nutrition that has been made. We looked at a paper in a Monday note in December 2021 where the Global Burden of Disease 2019 report had been used to estimate deaths attributable to trade in red meat (Ref 17). Last summer, 2021, we reviewed the National Food Strategy for England (Ref 18). This also cited the GBD 2019 report as a reference upon which recommendations had been made. Despite only being published in October 2020, GBD 2019 has been cited by 635 documents, including 351 scientific papers and 9 policy documents. The report would be cited in many different subject areas, from breastfeeding to pollution, but where it is being used to validate dietary policy, its reliability is vital. If GBD 2019 is not robust, and compelling questions have been asked of it, it should be retracted or amended. The fact that the GBD 2019 authors have not even attempted to rebut this letter is of grave concern.
p.s. some media coverage can be seen here (Ref 19).
References
Ref 1: Stanton et al. 36-fold higher estimate of deaths attributable to red meat intake in GBD 2019: is this reliable? The Lancet. February 2022. https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(22)00311-7/fulltext
Ref 2: GBD 2019 risk factors collaborators. Global burden of 87 risk factors in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. The Lancet. October 2020. https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(20)30752-2/fulltext#seccestitle10
Ref 3: https://www.thelancet.com/gbd
Ref 4: Murray et al. The global burden of disease in 1990: summary results, sensitivity analysis and future directions. Bull World Health Organ. 1994. https://pubmed.ncbi.nlm.nih.gov/8062404/
Ref 5: https://www.thelancet.com/commissions/EAT
Ref 6: Institute for Health Metrics and Evaluation and World Health Organization sign new agreement. Institute for Health Metrics and Evaluation. May 2015. https://www.healthdata.org/announcement/institute-health-metrics-and-evaluation-and-world-health-organization-sign-new
Ref 7: https://www.thelancet.com/journals/lancet/issue/vol380no9859/PIIS0140-6736(12)X6053-7
Ref 8: https://www.thelancet.com/journals/lancet/issue/vol388no10053/PIIS0140-6736(16)X0042-6
Ref 9: https://www.thelancet.com/journals/lancet/issue/vol390no10100/PIIS0140-6736(17)X0041-X
Ref 10: https://www.thelancet.com/journals/lancet/issue/vol392no10159/PIIS0140-6736(18)X0048-8
Ref 11: https://www.thelancet.com/journals/lancet/issue/vol396no10258/PIIS0140-6736(20)X0042-0
Ref 12: This shows the funding for the 2010 report. Wang et al. Age-specific and sex-specific mortality in 187 countries, 1970–2010: a systematic analysis for the Global Burden of Disease Study 2010. The Lancet. December 2012. https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(12)61719-X/fulltext
Open each main article for the other years and funding is similarly reported as “Funding. Bill & Melinda Gates Foundation.”
Ref 13: https://www.geekwire.com/2017/bill-gates-invests-veggie-burger-bleeds-like-beef-feed-masses-save-planet/
Ref 14: https://www.dietandhealthtoday.com/2021/07/zoe-chats-with-frederic-leroy-about-the-global-demonisation-of-livestock-farming/ and Frederic’s twitter commentary of the letter https://twitter.com/fleroy1974/status/1497356586037227520
Ref 15: https://www.thelancet.com/cms/10.1016/S0140-6736(20)30752-2/attachment/54711c7c-216e-485e-9943-8c6e25648e1e/mmc1.pdf
Ref 16: https://www.healthdata.org/results/gbd_summaries/2019
Ref 17: https://www.zoeharcombe.com/2021/12/global-meat-trade-health/
Ref 18: https://www.zoeharcombe.com/2021/07/the-national-food-strategy-the-plan/
Ref 19: https://www.thegrocer.co.uk/health/red-meat-health-risks-study-is-unreliable-claim-scientists/661762.article
https://www.independent.ie/business/farming/news/scientists-challenge-data-linking-red-meat-to-health-risks-41396008.html





