Reference Range
D-dimer is the degradation product of crosslinked (by factor XIII) fibrin. It reflects ongoing activation of the hemostatic system. The reference concentration of D-dimer is < 250 ng/mL, or < 0.4 μ/mL. [1]
The reference range/cutoff value for D-dimer is ideally established by the performing laboratory, or, if a cutoff value published in the literature is used, the value has to be determined with the same methodology, preferably from the same manufacturer.
Point-of-care testing is available to determine the D-dimer amount semiquantitatively (latex agglutination–based). This test has high interobserver variability, making it less clinically valuable.
A quantitative, automated point-of-care D-dimer test has been developed, providing an excellent, cost-effective, and rapid tool, especially in the setting of ruling out pulmonary embolism among patients with a low probability of the condition.
Interpretation
D-dimer is the degradation product of crosslinked fibrin; therefore, it reflects ongoing activation of the hemostatic system. Since there is constant minimal physiologic fibrin formation and degradation in vivo, healthy individuals have a minimal D-dimer level.
Elevated D-dimer levels reflect ongoing activation of the hemostatic and thrombolytic system, providing clinical utility in the following:
-
Evaluation of thrombus formation
-
Ruling out DVT (discussed further below)
-
Monitoring anticoagulative treatment (a decreasing value indicates effective treatment)
-
Snake venom poisoning
Additionally, D-dimer levels may be elevated in the setting of pregnancy, inflammation, malignancy, trauma, postsurgical treatment, liver disease (decreased clearance), and heart disease. [2, 3] It is also frequently high in hospitalized patients. [4]
Lipemia, a high triglyceride level, an elevated bilirubin level, an elevated serum rheumatoid factor level, or hemolysis may falsely increase the D-dimer level.
Keep in mind that the D-dimer level in individuals with factor XIII deficiency remains low (eventually zero in homozygous factor XIII deficiency), even in the presence of a large clot formation, owing to a lack of crosslink formation. Consequently, if these individuals develop thrombosis, they present with increased fibrin degradation products but undetectable plasma D-dimer levels.
Also keep in mind that the D-dimer level increases naturally with age.
Deep venous thrombosis
In adult patients with a clinically low pretest probability (Wells score) of developing DVT, a negative D-dimer test result yields a 99% negative predictive value (NPV) in patients aged 60-80 years but only a 21%-31% NPV in patients older than 80 years. [5]
In patients with a clinically high pretest probability (Wells score) of developing DVT, the D-dimer test has essentially no clinical utility. [6] Anticoagulant therapy is initiated regardless of test result. [5]
In pregnant patients, a negative D-dimer test results has a NPV of 100%.
Collection and Panels
Serum, plasma (with sodium citrate anticoagulant, 3.2%)
Blood is obtained with routine venipuncture. A citrate-containing tube must be properly filled and mixed via inversion. It is transported to the laboratory within 3 hours. If this is not possible, the plasma is separated with centrifugation, frozen, and transported to the laboratory on dry ice.
Panels: DIC
Background
Description
D-dimer is the degradation product of crosslinked (by factor XIII) fibrin. It reflects ongoing activation of the hemostatic system.
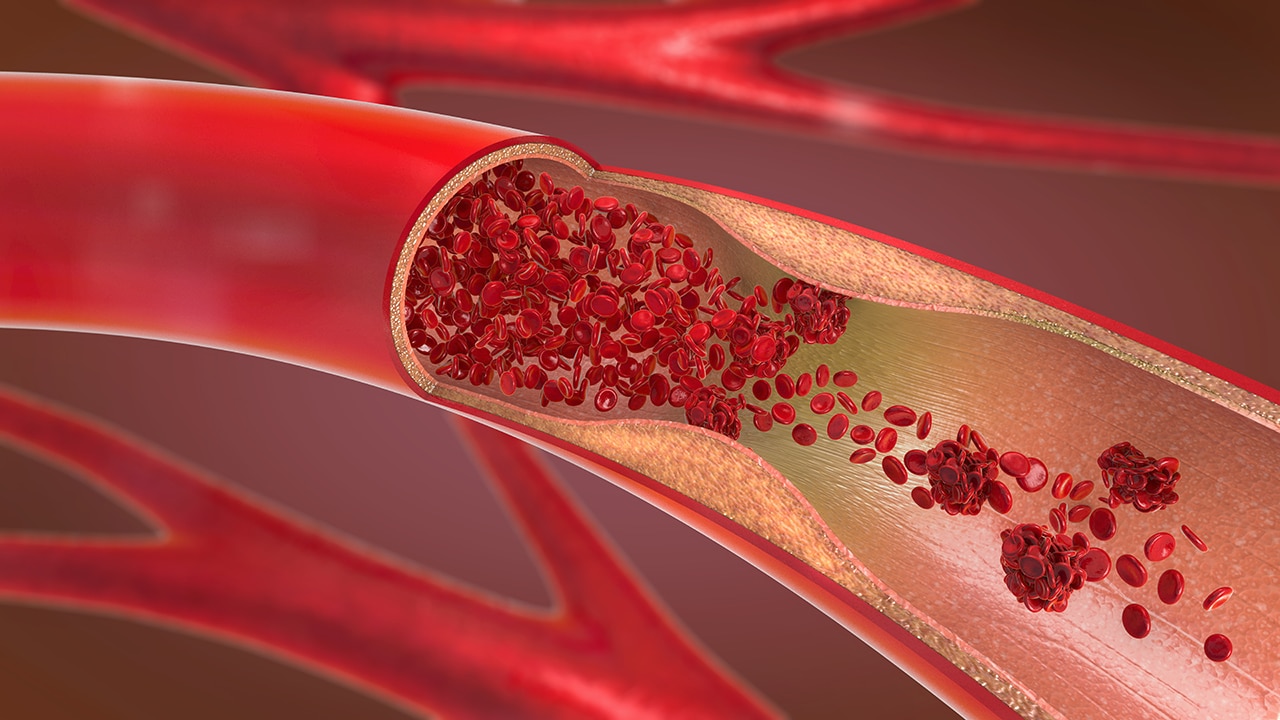
Upon activation of either the intrinsic or extrinsic pathway of the coagulation cascade, thrombin forms and cleaves fibrinopeptide A and B from fibrinogen, resulting in soluble fibrin monomers, which then associate and form fibrin polymers. The D domains of these fibrin polymers are crosslinked by activated factor XIII, producing an insoluble crosslinked fibrin clot.
Owing to the parallel activation of the fibrinolytic system to maintain proper balance between coagulation and fibrinolysis, plasmin, the end product of the fibrinolytic system, cleaves insoluble fibrin polymers, resulting in the production of fibrin degradation products (FDPs). If the polymers were crosslinked between two D domains (hence the name) of the fibrinopeptides, D-dimer is produced.
Indications/Applications
The principal utility of measuring D-dimer is the high NPV of the test in the diagnosis of deep venous thrombosis (DVT) in an appropriate clinical setting. The clinical (pretest) probability (Wells score) of DVT is determined by assessing multiple factors, such as recent or ongoing therapy for cancer, immobilization of the lower extremities, recent major surgeries, localized tenderness, edema, and history of previous DVT. Based on this score, the probability for developing DVT is categorized as low (unlikely to develop) or high (likely to develop).
In the low-moderate group, the NPV of the D-dimer test is 99% among patients aged 60-80 years but drops to 21%-31% if the patient is older than 80 years. Similarly, D-dimer is found to be a very valuable test in pregnant patients; if a pregnant woman has a low pretest probability for DVT, the NPV of a negative D-dimer test result is 100%.
Since D-dimer assumes activation of the coagulation and fibrinolytic systems, it is valuable in the diagnosis and the monitoring of DIC in combination with other parameters.
A 2010 study showed that a low plasma D-dimer level in pediatric patients correlates well with the absence of traumatic brain injury. [7]
In the appropriate setting, the D-dimer test yields a good NPV in the diagnosis of aortic dissection. [8]
In combination with other markers, D-dimer may be useful to differentiate between acute stroke and stroke-mimicking conditions. [9]
COVID-19
A retrospective study by Terra et al indicated that in patients with severe coronavirus disease 2019 (COVID-19), the neutrophil‐to‐lymphocyte ratio (NLR) and D-dimer level are biomarkers for mortality risk. The investigators reported that such patients are more likely to die if their NLR is 10 or greater and their D-dimer level is 2 μg/mL or above, particularly when both of these increases are present at the same time. [10]
In contrast, a study by Cidade et al suggested that a high D-dimer level is not a good predictor of whether a patient will survive severe COVID-19. The investigators compared patients with higher, lower, or intermediate D-dimer values, these being, respectively, levels less than 3 times the normal range value (NRV), specified in this study as 500 ng/mL; levels between 3 times and less than 10 times the NRV; and levels that were at least 10 times the NRV. The study reported that mortality did not differ between the groups. [11]
Considerations
The D-dimer test has a high sensitivity but low specificity. It may be increased in association with the following:
-
Hospitalized patients
-
After surgical procedures
-
Pregnancy
-
Inflammation
-
Malignancy
-
Trauma
-
Liver disease (decreased clearance)
-
Heart disease
Venous thromboembolic diseases are common complications in patients with cancer. Therefore, it is important to keep in mind that false-negative D-dimer results more commonly occur in this patient population.
The major advantage of the D-dimer test is the excellent NPV in the appropriate clinical setting. However, since the positive predictive value (PPV) of the test is low, positive results cannot be used alone in the diagnosis of DVT/pulmonary embolism.
From a practical standpoint, the D-dimer assay only measures the neo-epitope, which is formed after the crosslinking process of the fibrin polymers by factor XIII. Therefore, although it has limited importance in the assessment of primary fibrinolysis, there is no interference with fibrinogen, if it is present in the sample.
Questions & Answers
Overview
How are elevated D-dimer levels interpreted?
What is the role of D-dimer measurement in the workup of deep venous thrombosis (DVT)?
How are samples collected for D-dimer testing?
What are the clinical applications of D-dimer testing?
What should be considered when interpreting D-dimer test results?