NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases; 2012-.

OVERVIEW
Introduction
Vitamin A is a fat soluble vitamin necessary for health, deficiency of which can cause disorders of vision, skin, bone and immunity. The recommended daily allowance for vitamin A is 300 to 700 μg for children and approximately 700 to 900 μg for adults, amounts which can be provided by a normal diet. Higher doses of vitamin A can be toxic, leading to a constellation of signs and symptoms as well as liver injury, jaundice, enlargement of the liver and spleen, portal hypertension and cirrhosis.
Background
Vitamin A is a retinoid and a fat-soluble vitamin that is commonly found in eggs, milk and liver and in the form of provitamin A in carotenoids in fresh fruits and vegetables particularly those with red, orange or yellow color. Highest levels of vitamin A are found in liver. The recommended daily allowance (RDA) for vitamin A is 700 to 900 μg/day (~2300 to 4300 IU) in adults and 300 to 700 μg/day (~1000 to 2000 IU) in children. Multiple generic forms of vitamin A are available as tablets, capsules, and solutions in over-the-counter preparations, alone and in combination with other vitamins and minerals, as well as a component in herbal mixtures, creams and ointments.
Hepatotoxicity
Normal doses of vitamin A are not associated with liver injury or liver test abnormalities, but higher doses (generally more than 40,000 IU daily, ~12,000 μg) can be toxic. Acute toxicity is caused by a single or a few repeated very high doses (generally >100 times the RDA), arising within days to weeks with a typical symptom complex of severe headache, nausea, vertigo, blurred vision, muscle aches and lack of coordination, followed by skin desquamation and alopecia. Severe overdose can cause increased cerebral spinal fluid pressure, progressive drowsiness and coma. Chronic hypervitaminosis A usually arises 3 months to many years after starting moderately high levels of vitamin A (generally 10 times the RDA) and is marked by dry skin, cheilosis, gingivitis, muscle and joint pains, fatigue, mental dullness, depression and liver test abnormalities. Serum bilirubin is typically only mildly elevated. Serum aminotransferase and alkaline phosphatase levels are variably increased, but usually only 1 to 4 times the upper limit of normal. Serum vitamin A levels are typically, but not invariably elevated. Liver biopsy is diagnostic and shows enlarged, lipid-laden stellate cells with variable degrees of sinusoidal fibrosis. The liver may be hypoechogenic on ultrasound examination and suggest the diagnosis of nonalcoholic fatty liver disease, but the lipid-laden cells found on liver biopsy are not hepatocytes, but rather stellate cells (formerly known as Ito cells or hepatic lipocytes) which contain excess vitamin A. Chronic, moderately high doses of vitamin A (generally over 1 to 8 years) can lead to portal hypertension with ascites and esophageal varices, even before frank cirrhosis can be shown to be present. While high doses of vitamin A are usually achieved by vitamin A supplements, hypervitaminosis A can also occur with excessive dietary intake of liver, particularly that of carnivores (bears, seals, dogs) or salt-water fish (cod liver oil).
Likelihood score: A[H] (well established cause of liver injury when used in high doses).
Mechanism of Injury
Vitamin A in high doses is a direct toxin. Excess vitamin A is stored in stellate cells in the liver and accumulation can lead to their activation and hypertrophy, excess collagen production, fibrosis and liver injury. The toxicity is dose related and can be reproduced in animal models.
Outcome and Management
The liver injury caused by high doses of vitamin A is reversible in its early stages, but may resolve only slowly with discontinuation of ingestion and resumption of a normal diet. Patients should be specifically told to avoid all vitamin supplements that contain vitamin A and to follow a low vitamin A diet. In general, patients with known chronic liver diseases should avoid ingestion of more than the minimal daily requirement of vitamin A as underlying liver disease appears to increase the susceptibility to vitamin A toxicity.
Drug Class: Vitamins
Other Drugs in the Subclass:
CASE REPORTS
Case 1. Hypervitaminosis A in an adult.(1)
An 18 year old woman who had been taking vitamin A for an unspecified skin disorder in a dose of 100,000 to 200,000 IU daily for approximately 16 months developed muscular stiffness and fatigue which was particularly worsened by exercise. She subsequently noted bone pain, headache, poor appetite, nosebleeds, dry skin and generalized pruritus. She denied jaundice. She had no history of liver disease, alcohol abuse or risk factors for viral hepatitis. Physical examination showed dry scaly skin, cheilosis, and enlargement of the liver and spleen. Laboratory tests showed normal serum bilirubin, but AST 80 U/L and alkaline phosphatase of 129 U/L. Serum vitamin A levels were markedly elevated (737 µg/dL [normal 37-45]). All supplementary vitamin A was stopped and her symptoms improved markedly within the next 2 months. However, she continued to have hepatomegaly, mildly elevated serum enzymes and prolongation of prothrombin time (25 seconds) and decrease in serum albumin (3.4 g/dL). Ten months after stopping vitamin A, she still complained of fatigue and nosebleeds. There were mild elevations in serum bilirubin (2.5 mg/dL) and prothrombin time (21 seconds). A liver biopsy showed cirrhosis and fatty change in both hepatocytes and sinusoidal cells, fluorescence microscopy demonstrating vitamin A.
Key Points
| Medication: | Vitamin A (100,000-200,000 IU daily) |
|---|---|
| Pattern: | Minimal serum enzyme elevations |
| Severity: | 4+ (cirrhosis) |
| Latency: | 18 months |
| Recovery: | Incomplete |
| Other medications: | None mentioned |
Laboratory Values
| Time After Starting |
Time After Stopping |
AST (U/L) |
Alk P (U/L) |
Vitamin A (µg/dL) |
Other |
|---|---|---|---|---|---|
| 19 months | 0 | 80 | 129 | 737 | Vitamin A stopped |
| 21 months | 2 months | 55 | 105 | 155 | |
| 23 months | 4 months | 49 | 117 | ||
| 27 months | 8 months | 53 | 129 | 97.2 | |
| 29 months | 10 months | 50 | 94 | Liver biopsy: cirrhosis | |
| 35 months | 16 months | 53 | 71 | 92.1 | |
| Normal Values | <40 | <115 | <45 | ||
Comment
The typical manifestations of vitamin A toxicity are dry skin, cheilosis, dermatitis, joint and bone pain, headaches, and fatigue. A high proportion of patients also have liver test abnormalities, but these are typically mild. Jaundice is uncommon, but enlargement of the liver may be present. The presence of splenomegaly suggests that cirrhosis or portal hypertension was present at the time of initial presentation, as vitamin A is not stored in the spleen and does not cause splenomegaly on its own. The persistence of liver test abnormalities and coagulopathy eventually led to a liver biopsy that showed incomplete cirrhosis. By that time, serum vitamin A levels had fallen (although still elevated) and stellate cell hypertrophy was not prominent.
Case 2. Hypervitaminosis A and cirrhosis in an adult.(2)(3)
A 63 man who had been taking 400,000 IU of vitamin A daily for 8 years developed dry and fissured skin followed by general fatigue and abdominal swelling. He had no history of liver disease, jaundice or alcohol abuse. He had been treated for tuberculosis 3 years previously. He took no other medications; the vitamin A was taken under the belief that it would help prevent upper respiratory tract infections. On physical examination, he was not jaundiced, but had spider nevi, mild ascites and hepatosplenomegaly. Laboratory tests showed minimal elevations in liver tests with serum bilirubin of 1.2 mg/dL, ALT 30 U/L, AST 34 U/L, and alkaline phosphatase 45 U/L. The platelet count was 110,000/µL, albumin 3.0 g/dL and vitamin A level 84.6 µg/dL (normal 30-50). Barium swallow showed esophageal varices, and a liver biopsy revealed marked enlargement of perisinusoidal stellate cells with fat droplets and positive vitamin A fluorescence. There was sinusoidal congestion and an increase in fibrosis without frank cirrhosis. Vitamin A was discontinued, but he showed little improvement when seen 8 months later (Table). Four years after initial presentation, he was admitted to another hospital for worsening ascites. Laboratory testing showed similar liver test abnormalities, although serum albumin had fallen to 2.6 g/dL. A liver biopsy showed marked cirrhosis and presence of multiple hypertrophied stellate cells with characteristic vitamin A fluorescence. The patient was no longer taking high dose vitamin A, but was on a daily multivitamin (with 10,000 IU of vitamin A) and followed a diet that was high in vitamin A (rich in liver and carrot juice, which was calculated to be more than 50,000 IU daily).
Key Points
| Medication: | Vitamin A (400,000 IU daily, later 60,000 IU daily) |
|---|---|
| Pattern: | Minimal serum enzyme elevations |
| Severity: | 4+ (cirrhosis) |
| Latency: | 8 years |
| Recovery: | Incomplete |
| Other medications: | None mentioned |
Laboratory Values
Comment
While signs of portal hypertension were present initially, liver biopsy histology suggested that there was fibrosis without cirrhosis. The portal hypertension (ascites, varices) was attributed to sinusoidal encroachment due to hypertrophy of perisinusoidal stellate cells. Another publication on this same patient described clinical progression and a follow up liver biopsy showing unequivocal cirrhosis. Interestingly, the patient was convinced that vitamin A was important for health and had increased his dietary intake of vitamin A from natural sources, resulting in persistence of vitamin A hepatotoxicity. Hypervitaminosis A and liver disease have been described from excessive dietary intake without supplementation, but this outcome generally requires extraordinary intake from natural sources of the vitamin such as with carrot juice and daily ingestion of liver. Patients with hypervitaminosis A should be instructed to discontinue all supplementation and to avoid foods with high vitamin A content.
Case 3. Acute liver injury due to hypervitaminosis A.(4)
A 31 year old woman with psoriasis was treated with high doses of vitamin A (3.5 million IU daily) for 3 weeks. During the third week of therapy, she developed fatigue, severe headaches, loss of appetite, weight loss, nausea and vomiting, thirst and pains in both legs. After the fourth week, she developed jaundice and was admitted for evaluation. On examination, her skin was dry and scaly, but the psoriatic lesions had mostly healed. She was clinically jaundiced and had hepatomegaly. Laboratory tests showed total bilirubin of 8.1 mg/dL, ALT 11 U/L and alkaline phosphatase 110 U/L. Over the following week, she developed a severe hemolytic anemia with hemoglobin falling from 12.5 to 5.0 g/dL, which was treated with blood transfusions and high doses of methylprednisolone. A liver biopsy showed enlargement of stellate cells with fat droplets and intrahepatic cholestasis. She developed almost total alopecia a few days after stopping vitamin A supplementation, but then began to improve. Two months later, she was asymptomatic of liver disease and all laboratory tests were normal, although her psoriasis was worse.
Key Points
| Medication: | Vitamin A (3,500,000 IU daily) |
|---|---|
| Pattern: | Minimal serum enzyme elevations |
| Severity: | 4+ (cirrhosis) |
| Latency: | 4 weeks |
| Recovery: | Complete in 2 months |
| Other medications: | None mentioned |
Laboratory Values
Comment
Acute hypervitaminosis A is usually marked by severe headaches, nausea, vomiting and bone pain and can be associated with acute hepatic injury which resolves rapidly on stopping excess vitamin A intake.
PRODUCT INFORMATION
REPRESENTATIVE TRADE NAMES
Vitamin A – Generic, Aquasol A®
DRUG CLASS
Vitamins (Vitamin A)
Product labeling at DailyMed, National Library of Medicine, NIH
CHEMICAL FORMULA AND STRUCTURE
| DRUG | CAS REGISTRY NUMBER | MOLECULAR FORMULA | STRUCTURE |
|---|---|---|---|
| Vitamin A (as Retinol) | 68-26-8 | C20-H30-O | 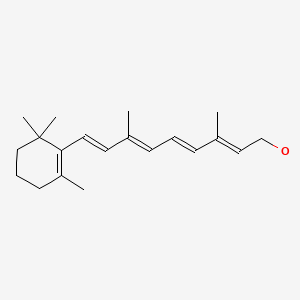 |
CITED REFERENCES
- 1.
-
Muenter MD, Perry HO, Ludwig J. Chronic vitamin A intoxication in adults. Hepatic, neurologic and dermatologic complications. Am J Med. 1971;50:129–36. [PubMed: 4099655]
- 2.
-
Russell RM, Boyer JL, Bagheri SA, Hruban Z. Hepatic injury from chronic hypervitaminosis A resulting in portal hypertension and ascites. N Engl J Med. 1974;291:435–40. [PubMed: 4843409]
- 3.
-
Jacques EA, Buschmann RJ, Layden TJ. The histopathologic progression of vitamin A-induced hepatic injury. Gastroenterology. 1979;76:599–602. [PubMed: 428713]
- 4.
-
Leicht E, Strunz J, von Seebach HB, Meiser RJ, Mäusle E. Med Klin. 1973;68:54–9. [Acute vitamin A intoxication with hemolytic anemia, hypercalcemia and toxic hepatosis] German. [PubMed: 4684742]
ANNOTATED BIBLIOGRAPHY
References updated: 04 November 2020
-
Zimmerman HJ. Vitamin A (retinol). Drugs used in dermatotherapy. In, Zimmerman HJ. Hepatotoxicity: the adverse effects of drugs and other chemicals on the liver. 2nd ed. Philadelphia: Lippincott, 1999, pp. 727-9.(Expert review of hepatotoxicity of vitamin A and the retinoids published in 1999).
-
Seeff L, Stickel F, Navarro VJ. Hepatotoxicity of herbals and dietary supplements. In, Kaplowitz N, DeLeve LD, eds. Drug-induced liver disease. 3rd ed. Amsterdam: Elsevier, 2013: pp, 631-57.(Review of hepatotoxicity of dietary supplements).
-
Henderer JD, Rapuano CJ. Ocular pharmacology. In, Brunton LL, Hilal-Dandan R, Knollman BC, eds. Goodman & Gilman’s the pharmacological basis of therapeutics. 13th ed. New York: McGraw-Hill, 2018, pp. 1251-70.(Textbook of pharmacology and therapeutics).
-
Popper H. Histologic distribution of vitamin A in human organs under normal and pathological conditions. Arch Path. 1941;31:766–802.(Analysis of histological distribution of vitamin A using fluorescence microscopy; fluorescence is not a general property of lipids and identifies vitamin A which in liver is in nonparenchymal cells, interpreted as being macrophages, despite absence of vitamin A fluorescence in the spleen).
-
Popper H, Steigmann F, Zevin S. On the variations of the plasma vitamin A level after the administration of large doses of vitamin A in liver disease. J Clin Invest. 1943;22:775–83. [PMC free article: PMC435294] [PubMed: 16695061](Serum levels of vitamin A were measured in 108 subjects given known amounts, low levels of vitamin A and poor absorption found in patients with obstructive liver disease and hepatitis with jaundice).
-
Rodahl K, Moore T. The vitamin A content and toxicity of bear and seal liver. Biochem J. 1943;37:166–8. [PMC free article: PMC1257872] [PubMed: 16747610](Specimens of polar bear and seal liver from Greenland expeditions were tested for vitamin A levels and found to have 12-26,000 IU per gram, suggesting hypervitaminosis A as the cause of illness after eating bear liver; tests of toxicity in rats "were difficult because of the reluctance of the rats to eat the liver").
-
Josephs HW. Hypervitaminosis A and carotenemia. Am J Dis Child. 1944;67:33–43.(Initial case report of hypervitaminosis A; a 3 year old boy on high doses of vitamin A [daily cod liver oil] developed anorexia followed by listlessness, bone pain, hyperostosis on X-ray, alopecia, hepatosplenomegaly and anemia [vitamin A 910 IU/dL, bilirubin 1.6 mg/dL, Alk P 1.5 times ULN], and improved on stopping cod liver oil supplements).
-
Sulzberger MB, Lazar MP. Hypervitaminosis A: report of a case in an adult. J Am Med Assoc. 1951;146:788–93. [PubMed: 14832059](Initial report in adults: 44 year old woman taking 600,000 IU of vitamin A daily for 18 months presented with alopecia, amenorrhea, bone pains, and cheilosis; no discussion of liver injury).
-
Reyersbach GC, Hanelin J, Joplin RJ. Vitamin A intoxication: report of a case. N Engl J Med. 1952;246:978–80. [PubMed: 14941256](3 year old girl developed bone pain, alopecia and irritability after receiving 240,000 IU of vitamin A daily for 1 year, hyperostosis on bone films, improving one year later; no mention of liver abnormalities).
-
Bifulco E. Vitamin A intoxication: report of a case in an adult. N Engl J Med. 1953;248:691–2. [PubMed: 13037022](52 year old woman on vitamin A [100,000 IU/day] for 4 years developed fatigue, alopecia, joint pains, exophthalmos, and bleeding tendency, improving on stopping vitamin A; no mention of liver abnormalities).
-
Gerber A, Raab AP, Sobel AE. Vitamin A poisoning in adults: with description of a case. Am J Med. 1954;16:729–45. [PubMed: 13148217](Extensive review of the history of vitamin A toxicity and case report; 28 year old woman with multiple admissions over 8 years with unexplained headaches, vertigo, neurological changes, nausea, muscle pains and hepatomegaly, eventually found to have high serum vitamin A levels [due to chronic doses of 500,000 IU vitamin A daily for ichthyosis], improving within 3 months of stopping).
-
Shaw EW, Niccoli JT. Hypervitaminosis A: report of a case in an adult male. Ann Intern Med. 1953;39:131–4. [PubMed: 13065995](25 year old man taking ~350,000 IU of vitamin A daily for two months presented with fatigue, skin rash, desquamation, alopecia and hepatomegaly [bilirubin 1.6 mg/dL, Alk P 1.5 times ULN], with rapid improvement on stopping vitamins).
-
Elliott RA Jr, Dryer RL. Hypervitaminosis A: report of a case in an adult. J Am Med Assoc. 1956;161:1157–9. [PubMed: 13331778](21 year old woman had fatigue and hepatomegaly [bilirubin 0.8 mg/dL, Alk P normal] after taking high doses of vitamin A [~200,000 IU daily] for 5 months for acne, improving within a month of stopping).
-
Oliver TK Jr. Chronic vitamin A intoxication: report of a case in an older child and review of the literature. AMA J Dis Child. 1958;95:57–68. [PubMed: 13487080](14 year old girl developed leg pain, skin rash, desquamation and alopecia after taking 200,000 IU of vitamin A daily for 10 months for acne; literature review identified 27 cases of chronic hypervitaminosis A in children and 6 in adults).
-
Soler-Bechara J, Soscia JL. Chronic hypervitaminosis A: report of a case in an adult. Arch Intern Med. 1963;112:462–6. [PubMed: 14051363](39 year old woman developed fatigue, joint pains, alopecia and peripheral edema having taken excess vitamin A [75,000-150,000 IU daily] for 8 years [bilirubin 1.7 mg/dL, ALT normal, Alk P ~4 times ULN and normal liver biopsy], symptoms improving within weeks of stopping).
-
Bergen SS, Roels OA. Hypervitaminosis A: report of a case. Am J Clin Nutr. 1965;16:265–9. [PubMed: 14253900](62 year old woman with chronic stasis ulcers, chronic musculoskeletal pains, alopecia and dry skin found to be taking high doses of vitamin A for years, normal liver tests; improving within 2 months of stopping).
-
Di Benedetto RJ. Chronic hypervitaminosis A in an adult. JAMA. 1967;201:700–2. [PubMed: 6071832](51 year old woman taking ~600,000 IU of vitamin A daily for at least 3 years presented with joint pains, alopecia, dry skin and hepatomegaly [ALT, and bilirubin normal], resolving within 1-2 months of stopping).
-
Lane BP. Hepatic microanatomy in hypervitaminosis in man and rat. Am J Path. 1968;53:591–8. [PMC free article: PMC2013413] [PubMed: 5677140](24 year old man who had been taking 50,000-5,000,000 IU of vitamin A daily for 5 years had normal ALT and bilirubin, but mildly elevated Alk P, and underwent liver biopsy which showed fat droplets in "Kupffer cells" which were fluorescent, whereas hepatocytes were largely normal; similar findings were reproduced in rats given vitamin A).
-
Rubin E, Florman AL, Degnan T, Diaz J. Hepatic injury in chronic hypervitaminosis A. Am J Dis Child. 1970;119:132–8. [PubMed: 5410560](6 year old girl on daily doses of vitamin A developed jaundice and hepatosplenomegaly [bilirubin 6.6 mg/dL, AST 120-160 U/L], liver biopsy showing lipid and vitamin A-laden stellate cells).
-
Muenter MD, Perry HO, Ludwig J. Chronic vitamin A intoxication in adults. Hepatic, neurologic and dermatologic complications. Am J Med. 1971;50:129–36. [PubMed: 4099655](Two patients, 18 and 53 year old women on 100,000-400,000 IU of vitamin A daily for 1.5 months and 8 years developed bone pains, dry skin and nausea, nose bleeds and headache [bilirubin normal, AST 80, Alk P ~1.5 times ULN], both had cirrhosis: Case 1).
-
Katz CM, Tzagournis M. Chronic adult hypervitaminosis A with hypercalcemia. Metabolism. 1972;21:1171–6. [PubMed: 4641958](18 year old man with weakness and nausea having taken 200,000 IU of vitamin A daily for acne for two years and was found to have hypercalcemia [normal ALT, Alk P 2 times ULN], was treated with iv saline and calcium fell, but he developed ascites, resolving with diuretics, liver biopsy being interpreted as normal).
-
Leicht E, Strunz J, von Seebach HB, Meiser RJ, Mäle E. Med Klin. 1973;68:54–9. [Acute vitamin A intoxication with hemolytic anemia, hypercalcemia and toxic hepatosis] German. [PubMed: 4684742](31 year old woman with psoriasis developed headache, nausea and jaundice 3 weeks after starting high doses [3.5 million units daily] of vitamin A [bilirubin 8.1 mg/dL, ALT 1-2 times ULN, Alk P 1-2 times ULN], accompanied by hemolytic anemia and alopecia, slowly resolving on stopping: Case 3).
-
Frame B, Jackson CE, Reynolds WA, Umphrey JE. Hypercalcemia and skeletal effects in chronic hypervitaminosis A. Ann Intern Med. 1974;80:44–8. [PubMed: 4810349](Three males, ages 7, 16 and 46 years, with hypervitaminosis A with hypercalcemia [12-14 mg/dL], Alk P elevations [~3 times ULN] and periosteal calcifications, all resolving on stopping vitamin A [only minor excess vitamin D intake]).
-
Muenter MD, Hypervitaminosis A. Ann Intern Med. 1974;80:105–6. [PubMed: 4810330](Editorial in response to Frame [1974] mentioning that acute vitamin A toxicity was first described by Kane, the American Arctic explorer, who in 1856 described the syndrome after members of the team ate polar bear liver; editorial argues in favor of an FDA restriction in amount of vitamin A in over-the-counter preparations).
-
Russell RM, Boyer JL, Bagheri SA, Hruban Z. Hepatic injury from chronic hypervitaminosis A resulting in portal hypertension and ascites. N Engl J Med. 1974;291:435–40. [PubMed: 4843409](54 and 63 year old women developed fatigue and weakness 5 and 8 years after starting high doses vitamin A [100,000 to 1.2 million IU/day], with cheilosis, alopecia, hepatosplenomegaly and ascites [bilirubin 2.2 and 1.2 mg/dL, ALT 16 and 30 U/L, Alk P 125 and 45 U/L, prothrombin time normal], biopsies showing stellate cells with fat, increased fibrosis, slow and incomplete improvement over the year after stopping: Case 2).
-
Kent G, Gay S, Inouye T, Bahu R, Minick OT, Popper H. Vitamin A-containing lipocytes and formation of type III collagen in liver injury. Proc Natl Acad Sci USA. 1976;73:3719–22. [PMC free article: PMC431190] [PubMed: 1068482](Administration of vitamin A to rats resulted in increase in "lipocytes" and type III collagen, suggesting the stellate cell is the predecessor of fibroblasts and accounts for fibrosis in the liver).
-
Smith FR, Goodman DS. Vitamin A transport in human vitamin A toxicity. N Engl J Med. 1976;294:805–8. [PubMed: 943041](3 patients with hypervitaminosis A with hepatomegaly, but normal liver tests had serial determinations of vitamin A, retinol, retinyl esters and retinol binding protein [RBP] during recovery; toxicity was associated with a high molar ratio of vitamin A to RBP, suggesting that excess free vitamin A is responsible for toxicity).
-
Farrell GC, Bhathal PS, Powell LW. Abnormal liver function in chronic hypervitaminosis A. Am J Dig Dis. 1977;22:724–8. [PubMed: 879140](57 year old woman developed joint pains, alopecia, dry skin, and abnormal liver tests after taking high doses of vitamin A [~90,000 IU/day] for 3-4 years [bilirubin 0.6 mg/dL, AST 72 U/L, Alk P 108 U/L], biopsy showing hypertrophied stellate cells and vitamin A fluorescence).
-
Kistler HJ, Pluer S, Dickenmann W, Pirozynski W. Schweiz Med Wschr. 1977;107:825–32. [Portal hypertension without cirrhosis due to chronic vitamin A intoxication] [PubMed: 267312](35 year old man developed weakness, alopecia, bone pain and ascites having taken 700,000 IU of vitamin A daily for 13 months [bilirubin 1.7 mg/dL, ALT 12 U/L, Alk P 1.5 times ULN], elevated portal pressure [40 mm Hg], but biopsy showing only mild sinusoidal fibrosis without cirrhosis; withdrawal was followed by resolution of symptoms and ascites).
-
Fleischmann R, Schlote W, Schomerus H, Wolburg H, Castrillon-Oberndorfter WL, Hoensch H. Dtsch Med Wochenschr. 1977;102:1637–40. [Small-nodular liver cirrhosis with marked portal hypertension due to vitamin A intoxication resulting from psoriasis treatment] [PubMed: 303561](36 year old man with psoriasis was treated with high doses of vitamin A [~1 million IU daily] for seven weeks, developing vitamin A toxicity and slowly recovering, but 3 years later was found to have esophageal varices [bilirubin 1.3 mg/dL, ALT and Alk P normal, platelets 100,000/μL] with cirrhosis, ascites and splenomegaly, biopsy showing vitamin A in hypertrophied stellate cells).
-
Babb RR, Kieraldo JH. Cirrhosis due to hypervitaminosis A. West J Med. 1978;128:244–6. [PMC free article: PMC1238074] [PubMed: 636413](72 year old man presented with ascites having taken 40,000 IU of vitamin A daily for 7 years [bilirubin 1.4 mg/dL, AST 80 U/L, Alk P 150 U/L, albumin 3.1 g/dL, prothrombin index 40%], ascites resolving 4 months after stopping vitamin A; although the liver did not show cirrhosis, he ultimately required porto-caval shunt for recurrent variceal hemorrhage).
-
Ferrando R, Truhaut R. Med Chir Dig. 1979;8:419–24. [Vitamin A and hepatotoxicity] French. [PubMed: 574915]
-
Jacques EA, Buschmann RJ, Layden TJ. The histopathologic progression of vitamin A-induced hepatic injury. Gastroenterology. 1979;76:599–602. [PubMed: 428713](Follow up of patient 2 described by Russell [1974] who stopped high doses of vitamin A, but continued excess ingestion by eating large amounts of carrots and liver; 3 years later he presented with worsening ascites [bilirubin 2.3 mg/dL, ALT 29 U/L, Alk P 205 U/L], liver biopsy showing cirrhosis and fat-laden stellate cells: Case 2).
-
Tholen W, Paquet KJ, Rohner HG, Albrecht M. Leber Magen Darm. 1980;10:193–7. [Cirrhosis of the liver and esophageal bleeding after chronic vitamin A intoxication(author's transl)] German. [PubMed: 6969836](21 year old woman with congenital ichthyosis developed jaundice and hepatosplenomegaly after taking high doses of vitamin A for 3 years [bilirubin 3.0 mg/dL, ALT 6 U/L, Alk P 146 U/L, platelets 68,000/μL], with cirrhosis on liver biopsy and death from recurrent variceal hemorrhage 4 years later).
-
Mahoney CP, Margolis MT, Knauss TA, Labbe RF. Chronic vitamin A intoxication in infants fed chicken liver. Pediatrics. 1980;65:893–7. [PubMed: 7189278](Twin 7 month olds developed irritability, vomiting and bulging fontanelles 4 months after starting a diet of chicken livers [~120 g daily], with normal ALT, Alk P and bilirubin, resolving with stopping diet [estimated 40,000 IU or 12,000 μg daily]).
-
Lippe B, Hensen L, Mendoza G, Finerman M, Welch M. Chronic vitamin A intoxication. A multisystem disease that could reach epidemic proportions. Am J Dis Child. 1981;135:634–6. [PubMed: 7246491](Two children, ages 2 and 4, developed rash, headache, bone pain and irritability and were found to have hypercalcemia [11.3 and 15.1 mg/dL] and taking excess vitamin A, resolving on stopping; liver tests normal).
-
Hatoff DE, Gertler SL, Miyai K, Parker BA, Weiss JB. Hypervitaminosis A unmasked by acute viral hepatitis. Gastroenterology. 1982;82:124–8. [PubMed: 7198070](42 year old man on long term vitamin A [25,000 IU daily] and vitamin A enriched diet developed desquamation, headache, alopecia and confusion 3 weeks after onset of acute hepatitis B, biopsy showing stellate cell hypertrophy, acute onset of toxicity being interpreted as due to decreased retinoid binding protein caused by hepatitis).
-
Weber FL Jr, Mitchell GE Jr, Powell DE, Reiser BJ, Banwell JG. Reversible hepatotoxicity associated with hepatic vitamin A accumulation in a protein-deficient patient. Gastroenterology. 1982;82:118–23. [PubMed: 7198069](63 year old man presented with edema and abnormal liver tests having taken high doses of vitamin A [40-50,000 IU daily] for 7 years [bilirubin 2.7 mg/dL, ALT 313 U/L, Alk P 1075 U/L], but had low serum vitamin A levels despite high levels in liver, resolving in 6 weeks on a normal diet).
-
Farris WA, Erdman JW Jr. Protracted hypervitaminosis A following long-term, low-level intake. JAMA. 1982;247:1317–8. [PubMed: 6460882](16 year old boy presented with headaches, nausea and papilledema having taken 50,000 IU of vitamin A daily for 2.5 years for acne [ALT and Alk P normal], resolving in 2 months of stopping).
-
Rosenberg HK, Berezin S, Heyman S, Witzleben C, Watkins JB. Pleural effusion and ascites: unusual presenting features in a pediatric patient with vitamin A intoxication. Clin Pediatr (Phila). 1982;21:435–40. [PubMed: 7083715](9 year old girl developed lethargy, pleural effusion and ascites [ALT and Alk P normal] after taking 300,000 IU of vitamin A daily for at least 1 year, with resolution on stopping, liver biopsy showed minimal fibrosis and mild fat some in sinusoidal cells).
-
Geubel AP, Rahier J. Rev Med Liege. 1983;38:679–84. [Hypervitaminosis A: physiopathology and liver toxicity] French. [PubMed: 6648175]
-
Guarascio P, Portmann B, Visco G, Williams R. Liver damage with reversible portal hypertension from vitamin A intoxication: demonstration of Ito cells. J Clin Pathol. 1983;36:769–71. [PMC free article: PMC498385] [PubMed: 6863568](35 year old woman developed cheilosis and ascites having taken high doses of vitamin A [90-300,000 IU daily] for 2 years [normal bilirubin and ALT], ascites resolving after 2 months of a normal diet, biopsy not showing cirrhosis, but stellate cells encroaching on sinusoids).
-
Olson JA. Adverse effects of large doses of vitamin A and retinoids. Semin Oncol. 1983;10:290–3. [PubMed: 6364354](Review of retinoids and vitamin A which do not share same toxicity but usually have a low therapeutic-toxic index).
-
Podell RN. Vitamin A supplementation. Subclinical overdose "unmasked" by hepatitis. Postgrad Med. 1983;74:297–301. [PubMed: 6684283](Review of vitamin A toxicity and the clinical report of Hatoff [1982]).
-
Bernstein RE. Liver and hypervitaminosis A. N Engl J Med. 1984;311:604. [PubMed: 6379462](Letter describing history of vitamin A toxicity caused by eating liver; particular polar bear and dog liver, but cases also described with chicken liver).
-
Le Marchand P, Benatre A, Metman EH, Couë C, Arbeille-Brassart B, Monegier du Sorbier C, Danquechin-Dorval E, et al. Gastroenterol Clin Biol. 1984;8:116–20. [Cirrhosis induced by vitamin A] French. [PubMed: 6698350](75 year old woman with psoriasis on vitamin A [250,000 IU daily] for 12 years developed jaundice and cirrhosis [bilirubin 2.0 mg/dL, ALT 46 U/L, Alk P 201 U/L, platelets 133,000/μL], biopsy showing cirrhosis; patient subsequently had variceal hemorrhage).
-
Verneau A, Rosenbaum J, Zafrani ES, Roudot-Thoraval F, Leclercq M, Dhumeaux D. Gastroenterol Clin Biol. 1984;8:121–5. [Hepatic fibrosis and portal hypertension in chronic vitamin A poisoning] French. [PubMed: 6538153](36 year old man presented with ascites having taking vitamin A [200,000 IU daily] for psoriasis for 10 years [bilirubin 1.2 mg/dL, ALT 13 U/L, Alk P 33 U/L, albumin 2.8 g/dL and platelets 70,000/uL], liver biopsy showing sinusoidal fibrosis and nodularity).
-
Zafrani ES, Bernuau D, Feldmann G. Peliosis-like ultrastructural changes of the hepatic sinusoids in human chronic hypervitaminosis A: report of three cases. Hum Pathol. 1984;15:1166–70. [PubMed: 6500549](Three patients [2 women and 1 man, ages 25 to 51 years] with hypervitaminosis A after 1-12 years of excessive intake had portal hypertension [venous gradients 14 to 17 mm Hg], biopsies showing abnormal sinusoids, swelling of perisinusoidal space and thickening of endothelial cells).
-
Yamamoto M. Nippon Rinsho. 1985;43:1187–91. [Toxic hepatitis induced by vitamin A] Japanese. [PubMed: 4046190]
-
Baglin A, Hagege C, Franc B, Richaud M, Prinseau J. Ann Med Interne (Paris). 1986;137:142–6. [A systemic-like disease: chronic vitamin A poisoning] French. [PubMed: 3717819]
-
Inkeles SB, Connor WE, Illingworth DR. Hepatic and dermatologic manifestations of chronic hypervitaminosis A in adults. Report of two cases. Am J Med. 1986;80:491–6. [PubMed: 2937294](29 year old man and 41 year old woman developed hypervitaminosis A on a beef liver diet for 8-9 years and high dose vitamin A pulses for 1 year, one with cirrhosis and one with abnormal liver tests [bilirubin normal, ALT 393 and 40 U/L, Alk P 120-121 U/L], improving on stopping excess vitamin A).
-
Witzleben CL. Case 5. Vitamin A hepatotoxicity. Pediatr Pathol. 1986;6:481–4. [PubMed: 3588445]
-
Yob EH, Pochi PE. Side effects and long-term toxicity of synthetic retinoids. Arch Dermatol. 1987;123:1375–8. [PubMed: 3310911](Retinoids are modifications of vitamin A molecule and do not share toxicities necessarily, most are not stored in the liver; hepatotoxicity of retinoids is different from that of vitamin A, usually arising within first 1-2 months and having features of hypersensitivity).
-
Bioulac-Sage P, Quinton A, Saric J, Grimaud JA, Mourey MS, Balabaud C. Chance discovery of hepatic fibrosis in patient with asymptomatic hypervitaminosis A. Arch Pathol Lab Med. 1988;112:505–9. [PubMed: 3358651](50 year old woman with peptic ulcer disease underwent gastric surgery and had liver biopsy that showed stellate cell hypertrophy and sinusoidal fibrosis despite normal ALT, Alk P and bilirubin; had been on high doses of vitamin A for 4 years).
-
Minuk GY, Kelly JK, Hwang WS. Vitamin A hepatotoxicity in multiple family members. Hepatology. 1988;8:272–5. [PubMed: 3356407](3 of 5 family members [father, mother and son] who were taking 20,000-45,000 IU of vitamin A daily for 7-10 years developed nausea and weakness and were found to have liver test abnormalities [bilirubin 0.3-1.0 mg/dL, ALT 71-265 U/L, Alk P 76-258 U/L], resolving in 6-12 months on normal diet).
-
Mendoza FS, Johnson F, Kerner JA, Tune BM, Shochat SJ. Vitamin A intoxication presenting with ascites and a normal vitamin A level. West J Med. 1988;148:88–90. [PMC free article: PMC1026032] [PubMed: 3341140](3 year old girl on 50,000 IU of vitamin A daily for 6 months presented with leg pain, irritability and skin rash and developed ascites and respiratory distress [ALT 31 U/L, Alk P 153 U/L, albumin 3.4 g/dL], liver biopsy showing central fibrosis and stellate cell hypertrophy, resolving in 4-5 months).
-
Smith JW. Vitamin A toxicity presenting as jaundice. Postgrad Med. 1989;85:53–4, 56. [PubMed: 2928281]
-
Baker H, ten Hove W, Kanagasundaram N, Zaki G, Leevy CB, Frank O, Leevy CM. Excess vitamin A injures the liver. J Am Coll Nutr. 1990;9:503–9. [PubMed: 2258538](56 year old woman developed fatigue, weakness, alopecia, bone pain and ascites after taking vitamin A [~60,000 IU daily] for 12 years [bilirubin 3.2 mg/dL, AST 313 U/L, Alk P 1075 U/L], hepatic venous pressure gradient was 19 mm Hg and liver biopsy showed stellate cell hypertrophy, sinusoid fibrosis but not frank cirrhosis, most abnormalities resolved 6 months after stopping excess intake).
-
Belaiche J, Gast P, Lambinet N, Etienne M, Fridman V, Vivario M, Boniver J. Rev Med Liege. 1990;45:381–9. [Hepatic fibrosis with cirrhogenous development in chronic vitamin A poisoning] French. [PubMed: 2218213]
-
Sarles J, Scheiner C, Sarran M, Giraud F. Hepatic hypervitaminosis A: a familial observation. J Pediatr Gastroenterol Nutr. 1990;10:71–6. [PubMed: 2324882](4 siblings with congenital ichthyosis taking high doses of vitamin A developed liver disease [bilirubin 0.4-1.4 mg/dL, ALT 13-54 U/L, Alk P 184-1069 U/L]; biopsies showed stellate cell hypertrophy and variable degrees of fibrosis).
-
Fallon MB, Boyer JL. Hepatic toxicity of vitamin A and synthetic retinoids. J Gastroenterol Hepatol. 1990;5:334–42. [PubMed: 2103414](Review of liver injury due to vitamin A and retinoids identified 18 case reports of vitamin A hepatotoxicity in the English literature, patients ages 6 to 63 years, presenting with rash, fatigue, hepatomegaly and hepatic synthetic dysfunction, biopsy showing fat in stellate cells and fibrosis; in contrast, there is little evidence that isotretinoin causes liver injury other than mild rapidly reversible ALT elevations; etretinate causes ALT elevations in ~20% of patients and case reports of clinically apparent injury have been published, but vary in clinical patterns).
-
Geubel AP, De Galocsy C, Alves N, Rahier J, Dive C. Liver damage caused by therapeutic vitamin A administration: estimate of dose-related toxicity in 41 cases. Gastroenterology. 1991;100:1701–9. [PubMed: 2019375](Retrospective analysis of 41 cases of hypervitaminosis A with liver injury seen between 1976 and 1989 at one institution, diagnosis often delayed [0-10 years], intake of 20,000-400,000 IU daily for 0.2 to 15 years, those with cirrhosis [n=17] having taken more and for a longer time; 6 died of liver disease and two underwent liver transplantation).
-
Anonymous Iatrogenic liver disease from vitamin A. Nutr Rev. 1991;49:309–12. [PubMed: 1749529](Editorial on dangers of vitamin A therapy of dermatologic diseases based on study of Geubel [1991]).
-
Burillo Lorente J, Castellote Alonso J, Massanes Bohigas PR. Rev Clin Esp. 1991;189:396–7. [Portal hypertension and hepatic fibrosis caused by vitamin A] Spanish. [PubMed: 1784812]
-
Dubois A, Balducchi JP, Barbuat C, Fabre J, Flaisler F, Joujoux JM, Pignodel C, et al. Rev Med Interne. 1991;12:295–8. [Portal hypertension and hypervitaminosis A. Apropos of 2 cases and review of the literature] French. [PubMed: 1759070](Two women, 39 and 43 years old, presented with ascites and liver biopsy showing stellate cell hypertrophy, one having taken methoxypsoralen [for tanning] and one Plethoryl [which contains a synthetic retinoid for weight loss] for several years, improving on stopping).
-
Oren R, Ilan Y. Reversible hepatic injury induced by long-term vitamin A ingestion. Am J Med. 1992;93:703–4. [PubMed: 1361304](56 year old woman taking 5000 IU of vitamin A daily developed nausea and abdominal pain [bilirubin normal, ALT 151 U/L, Alk P 870 U/L], liver biopsy showing portal fibrosis [no mention of stellate cell morphology], liver tests improving upon stopping and worsening again upon restarting the "normal doses" of vitamin A).
-
Scoazec JY, Bouma ME, Roche JF, Blache D, Verthier N, Feldmann G, Gay G. Liver fibrosis in a patient with familial homozygous hypobetalipoproteinaemia: possible role of vitamin supplementation. Gut. 1992;33:414–7. [PMC free article: PMC1373841] [PubMed: 1568667](21 year old woman with abetalipoproteinemia and fatty liver was treated with vitamin A [15,000 IU daily] and found to have elevations in ALT [2 times ULN] 2 years later, repeat liver biopsy showing fibrosis and worsening steatosis, but normal stellate cells).
-
Theiler R, Wirth HP, Flury R, Hanck A, Michel BA. Schweiz Med Wochenschr. 1993;123:2405–12. [Chronic vitamin A poisoning with musculoskeletal symptoms and morphological changes of the liver: a case report] German. [PubMed: 8290933]
-
Kowalski TE, Falestiny M, Furth E, Malet PF. Vitamin A hepatotoxicity: a cautionary note regarding 25,000 IU supplements. Am J Med. 1994;97:523–8. [PubMed: 7985711](45 year old woman developed fatigue, pruritus, jaundice and hepatomegaly having taken vitamin A in an over-the-counter preparation of 25,000 IU daily for 6 years [bilirubin 6.3 mg/dL, ALT 67 U/L, Alk P 585 U/L], biopsy showing severe fibrosis, cholestasis and stellate cell hypertrophy; her condition gradually worsened despite stopping and she died 10 weeks later).
-
Horsmans Y, Rahier J, Geubel AP. Hepatic injury and vitamin A ingestion. Am J Med. 1995;98:424. [PubMed: 7755793](Letter in response to Oren [1992] pointing out the unusual clinical features of the case described).
-
Croquet V, Pilette C, Lespine A, Vuillemin E, Rousselet MC, Oberti F, Saint André P, et al. Hepatic hyper-vitaminosis A: importance of retinyl ester level determination. Eur J Gastroenterol Hepatol. 2000;12:361–4. [PubMed: 10750659](32 year old man with history of leukemia and bone marrow transplantation, taking 50,000 IU of vitamin A daily for 15 years presented with variceal hemorrhage, liver biopsy showing stellate cell hypertrophy but no fibrosis [ALT 54 U/L, Alk P 117], vitamin A was stopped but he continued to have liver test abnormalities and presented with ascites 5 years later, biopsy again showing minimal fibrosis).
-
Mawson AR, Steele TA. Possible role of retinoids in hepatitis B virus-associated liver damage. Exp Biol Med (Maywood). 2001;226:734–9. [PubMed: 11520938](Review and hypothesis regarding interactions of vitamin A, retinoids and hepatitis B virus infection).
-
Miksad R, de Lénghen V, McDougall C, Fiel I, Rosenberg H. Hepatic hydrothorax associated with vitamin A toxicity. J Clin Gastroenterol. 2002;34:275–9. [PubMed: 11873112](52 year old woman presented with ascites and dyspnea having taken high doses of vitamin A for 18 years [bilirubin not given, ALT 45 U/L, Alk P 160 U/L], with hydrothorax, liver biopsy showing stellate cell hypertrophy and pericellular fibrosis; hepatic venous pressure gradient was 10 mm Hg; gradual but incomplete improvement on stopping vitamin A).
-
Bahcecioglu IH, Yalniz M, Ilhan N, Ataseven H, Ozercan IH. Levels of serum vitamin A, alpha-tocopherol and malondialdehyde in patients with non-alcoholic steatohepatitis: relationship with histopathologic severity. Int J Clin Pract. 2005;59:318–23. [PubMed: 15857329](Vitamin A levels were higher in 29 patients with nonalcoholic steatohepatitis than in 10 controls [2.1 vs 1.4 μmol/L], whereas vitamin E levels tended to be lower [42.8 vs 47.5 μmol/L]; no correlation with degree of ALT elevations).
-
Nollevaux MC, Guiot Y, Horsmans Y, Leclercq I, Rahier J, Geubel AP, Sempoux C. Hypervitaminosis A-induced liver fibrosis: stellate cell activation and daily dose consumption. Liver Int. 2006;26:182–6. [PubMed: 16448456](Reanalysis of liver biopsy material from 9 of the 41 patients described by Geubel [1991] showed correlation between amount of fibrosis and number of activated stellate cells and perisinusoidal fibrosis and estimated daily consumption of vitamin A).
-
Castaño G, Etchart C, Sookoian S. Vitamin A toxicity in a physical culturist patient: a case report and review of the literature. Ann Hepatol. 2006;5:293–5. [PubMed: 17151585](25 year old man taking 220,000 IU of vitamin A daily developed abnormal liver tests [ALT 104 U/L, Alk P 361 U/L, GGT 392 U/L], biopsy showing hypertrophied stellate cells and advanced fibrosis).
-
Chalasani N, Fontana RJ, Bonkovsky HL, Watkins PB, Davern T, Serrano J, Yang H, Rochon J., Drug Induced Liver Injury Network (DILIN). Causes, clinical features, and outcomes from a prospective study of drug-induced liver injury in the United States. Gastroenterology. 2008;135:1924–34. [PMC free article: PMC3654244] [PubMed: 18955056](Among 300 cases of drug induced liver disease in the US collected between 2004-2008, one was attributed to acitretin, but none to vitamin A).
-
Ramanathan VS, Hensley G, French S, Eysselein V, Chung D, Reicher S, Pham B. Hypervitaminosis A inducing intra-hepatic cholestasis - a rare case report. Exp Mol Pathol. 2010;88:324–5. [PubMed: 19944093](46 year old man developed jaundice having taken multivitamins and a vitamin A containing Herbalife product for 12 years [bilirubin 11.2 mg/dL, ALT 58 U/L, Alk P 193 U/L]; ERCP showed a biliary stricture, but there was little improvement after sphincterotomy and a liver biopsy showed cholestasis and lipid filled stellate cells, abnormalities resolving with stopping vitamin A product).
-
Ferrajolo C, Capuano A, Verhamme KM, Schuemie M, Rossi F, Stricker BH, Sturkenboom MC. Drug-induced hepatic injury in children: a case/non-case study of suspected adverse drug reactions in VigiBase. Br J Clin Pharmacol. 2010;70:721–8. [PMC free article: PMC2997312] [PubMed: 21039766](Worldwide pharmacovigilance database contained 9036 hepatic adverse drug reactions in children, isotretinoin was the most frequently mentioned agent [420 cases: 6.4%], but no information on the characteristics of the cases was provided).
-
Devarbhavi H, Dierkhising R, Kremers WK, Sandeep MS, Karanth D, Adarsh CK. Single-center experience with drug-induced liver injury from India: causes, outcome, prognosis, and predictors of mortality. Am J Gastroenterol. 2010;105:2396–404. [PubMed: 20648003](Among 313 cases of drug induced liver injury seen between 1997 and 2008 at a large hospital in Bangalore, India, no cases were attributed to vitamin A or retinoids).
-
Reuben A, Koch DG, Lee WM., Acute Liver Failure Study Group. Drug-induced acute liver failure: results of a U.S. multicenter, prospective study. Hepatology. 2010;52:2065–76. [PMC free article: PMC3992250] [PubMed: 20949552](Among 1198 patients with acute liver failure enrolled in a US prospective study between 1998 and 2007, 133 were attributed to drug induced liver injury, but none were attributed to vitamin A or a retinoid).
-
Mas Morey P, Nigorra Caro M, Cladera Serra A, Nicolás Picó J. Possible fulminant toxicity by all-trans-retinoic acid in a patient with acute promyelocytic leukemia. Farm Hosp. 2011;35:44–5. [PubMed: 20605103](33 year old woman with promyelocytic leukemia treated with all-trans-retinoic acid developed acute liver failure within 3 weeks of starting [bilirubin 1.1 rising to 17.4 mg/dL], with progressive pulmonary and renal failure and death 25 days later).
-
Stickel F, Kessebohm K, Weimann R, Seitz HK. Review of liver injury associated with dietary supplements. Liver Int. 2011;31:595–605. [PubMed: 21457433](Review of the hepatotoxicity of herbals and nutritional supplements including vitamin A, toxic levels being above 50,000 IU daily, but toxic dose is lower in persons with risk factors such as underlying liver disease).
-
Zhang H, Zhang J, Dong H. Fatal hepatotoxicity due to viaminate. Am J Med Sci. 2018;356:84–6. [PubMed: 30049333](43 year old Chinese woman developed abdominal distension one month after starting viaminate, a tretinoin derivative [bilirubin 9.4 mg/dL, ALT 1504 U/L, Alk P 105 U/L, INR 1.47], with progressively worsening jaundice and hepatic encephalopathy, dying of hepatic failure 38 days after admission and autopsy showing massive necrosis).
-
Fox R, Stace N, Wood K, French C. Liver toxicity from vitamin A. JGH Open 2019; 4: 287-8. [PMC free article: PMC7144761] [PubMed: 32280780](27 year old female developed fatigue 18 months after starting vitamin A [bilirubin 0.9 mg/dL, ALT 15 U/L, Alk P 208 U/L], biopsy showing microvesicular fat and prominent stellate cells] with slow improvement after stopping vitamin A).
-
Kulkarni AV, Kumar P, Talukdar R, Rao NP. Steroids as rescue therapy for vitamin A-induced acute liver failure. BMJ Case Rep. 2020;13(3):e233902. [PMC free article: PMC7059506] [PubMed: 32139453](34 year old man developed jaundice having taken vitamin A [5000 IU] twice daily for 7 years [bilirubin 3.2 mg/dL, ALT 1802 U/L, Alk P 119 U/L, INR 0.96], with abnormal transient elastography and microvesicular fat and prominent stellate cells on liver biopsy; when there was no change in liver tests for 2 weeks after stopping vitamin A, prednisone was started and tests began to improve rapidly; he later tolerated discontinuation of prednisone without a subsequent relapse ).
- PMC
PubMed Central citations
- PubChem Substance
Related PubChem Substances
- PubMed
Links to PubMed
- Review Vitamin D.[LiverTox: Clinical and Researc...]
Review Vitamin D.. LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. 2012
- Review Chapter 29: historical aspects of the major neurological vitamin deficiency disorders: overview and fat-soluble vitamin A.[Handb Clin Neurol. 2010]
Review Chapter 29: historical aspects of the major neurological vitamin deficiency disorders: overview and fat-soluble vitamin A.Lanska DJ. Handb Clin Neurol. 2010; 95:435-44.
- Review Diet and obstructive lung diseases.[Epidemiol Rev. 2001]
Review Diet and obstructive lung diseases.Romieu I, Trenga C. Epidemiol Rev. 2001; 23(2):268-87.
- [Portal hypertension without liver cirrhosis in chronic vitamin A intoxication].[Schweiz Med Wochenschr. 1977]
[Portal hypertension without liver cirrhosis in chronic vitamin A intoxication].Kistler HJ, Plüer S, Dickenmann W, Pirozynski W. Schweiz Med Wochenschr. 1977 Jun 18; 107(24):825-32.
- Hepatic hydrothorax associated with vitamin a toxicity.[J Clin Gastroenterol. 2002]
Hepatic hydrothorax associated with vitamin a toxicity.Miksad R, de Lédinghen V, McDougall C, Fiel I, Rosenberg H. J Clin Gastroenterol. 2002 Mar; 34(3):275-9.
- Vitamin A - LiverTox
Vitamin A - LiverTox
Your browsing activity is empty.
Activity recording is turned off.
See more...