Abstract
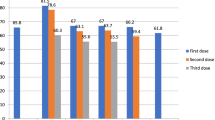
Measles outbreaks were recently reported in Europe due to low immunization rates. In this scenario, identifying the reasons of no vaccination is crucial to set up strategies to improve immunization rate. A cross-sectional study was conducted to investigate the determinants of missed vaccination in children living in Southern Italy, during the 2016 outbreak. A standardized face-to-face questionnaire was used to record demographic data, immunization status, and reasons for missed vaccination. A total of 1141 children (median age 86 months, male 47.2%) was enrolled, 77.8% of the children were adequately vaccinated for age, 6.3% were incompletely vaccinated for age, and 15.9% did not receive any vaccine dose. Vaccination rate and reasons for not vaccinating significantly varied according to age, with children ≤ 24 months showing the lowest rate (67.8%). Reasons for not vaccinating included fear for side effects (51%), presence of underlying chronic conditions (12.2%), skip scheduled appointment (12.2%), refusal of vaccination (10.3%), acute illnesses (7.2%), and allergy to eggs (4.6%). The presence of underlying condition was a risk factor for inadequate immunization (p < 0.0001). Only 4.7% of conditions were true contraindications to vaccine administration.
Conclusion: We reported inadequate measles immunization rate in Southern Italy, with lowest rates in children ≤ 2 years or with underlying conditions. Only a minority had true contraindications to vaccine uptake. Implementation strategies addressed to health-care professionals and families should focus on the reported determinants to increase measles vaccination coverage.
What is Known: • Measles is a viral, highly communicable disease, preventable by vaccine. • Measles elimination in Europe failed as demonstrated by outbreaks in several countries, due to low immunization rates. |
|
What is New: • Inadequate measles immunization rate due to false contraindications in Southern Italy, with lowest rates in children ≤ 2 years. • The presence of underlying disease is a risk factor for inadequate immunization. |



Similar content being viewed by others
Abbreviations
- DTaP-HB-IPV-Hib:
-
Diphtheria/tetanus/pertussis/hepatitis B/polio/haemophilus influenzae type b
- MMR:
-
Measles-mumps-rubella
- WHO:
-
World Health Organization
References
American Academy of Pediatrics – RedBook Edition 2015
Bednarczyk RA, Orenstein WA, Omer SB (2016) Estimating the number of measles-susceptible children and adolescents in the United States using data from the National Immunization Survey-Teen (NIS-Teen). Am J Epidemiol 184(2):148–156
Bester JC (2016) Measles and measles vaccination: a review. JAMA Pediatr 170(12):1209–1215
Bochennek K, Allwinn R, Langer R, Becker M, Keppler OT, Klingebiel T, Lehrnbecher T (2014) Differential loss of humoral immunity against measles, mumps, rubella and varicella-zoster virus in children treated for cancer. Vaccine 3227:3357–3361
Bocquier A, Ward J, Raude J, Peretti-Watel P, Verger P (2017) Socioeconomic differences in childhood vaccination in developed countries: a systematic review of quantitative studies. Expert Rev Vaccines 16:1107–1118
Brown KF, Kroll JS, Hudson MJ, Ramsay M, Green J, Long SJ, Vincent CA, Fraser G, Sevdalis N (2010) Factors underlying parental decisions about combination childhood vaccinations including MMR: a systematic review. Vaccine 28(26):4235–4248
Center for Diseases control and prevention n.d. Traveler’s health: Measles in Italy. Available from: https://wwwnc.cdc.gov/travel/notices/watch/measles-italy
Centers for Disease Control and Prevention (CDC) (2003) Measles epidemic attributed to inadequate vaccination coverage--Campania, Italy, 2002. MMWR Morb Mortal Wkly Rep 52:1044–1047
Covolo L, Ceretti E, Passeri C, Boletti M, Gelatti U (2017) What arguments on vaccinations run through YouTube videos in Italy? A content analysis. Hum Vaccin Immunother 31:1–7
De Marco G, Ummarino D, Giannetti E, Magurno T, Guarino A (2005) Impact of mass media communication in the implementation of influenza vaccination for infants. Arch Pediatr Adolesc Med 159:596
ECDC Surveillance and disease data. Monthly measles epidemiological updates. Available from: http://ecdc.europa.eu/en/healthtopics/measles/epidemiological_data/Pages/measles_surveillance_reports.aspx
Epicentro. Morbillo & Rosolia News: il bollettino della sorveglianza integrata morbillo-rosolia, Available from: http://www.epicentro.iss.it/problemi/morbillo/bollettino/RM_News_2016_34.pdf. (accessed 30 Oct 2018)
Epicentro. Available from: http://www.epicentro.iss.it/temi/vaccinazioni/dati_Ita.asp#morbillo (accessed 30 Oct 2018)
Filia A, Bella A, Rota M, Tavilla A, Magurano F, Baggieri M, Nicoletti L, Iannazzo S, Pompa M, Declich S (2013) Analysis of national measles surveillance data in Italy from October 2010 to December 2011 and priorities for reaching the 2015 measles elimination goal. Euro Surveill 18(20)
Fombonne E, Zakarian R, Bennett A, Meng L, McLean-Heywood D (2006) Pervasive developmental disorders in Montreal, Quebec, Canada: prevalence and links with immunizations. Pediatrics 118(1):e139–e150
Giambi C, Fabiani M, D'Ancona F, Ferrara L, Fiacchini D, Gallo T, Martinelli D, Pascucci MG, Prato R, Filia A, Bella A, Del Manso M, Rizzo C, Rota MC (2018) Parental vaccine hesitancy in Italy - results from a national survey. Vaccine 36(6):779–787
Giannattasio A, Lo Vecchio A, Franzese A, Prisco F, Femiano P, Guarino A (2010) Redundancy of roles by physicians in charge of paediatric diabetes is a barrier to flu immunisation. Arch Dis Child 95:399–400
Godlee F, Smith J, Marcovitch H (2011) Wakefield’s article linking MMR vaccine and autism was fraudulent. BMJ 342:c7452
Grammens T, Maes V, Hutse V, Laisnez V, Schirvel C, Trémérie JM, Sabbe M (2016) Different measles outbreaks in Belgium, January to June 2016 - a challenge for public health. Euro Surveill 21(32)
Hethcote HW (1983) Measles and rubella in the United States. Am J Epidemiol 1171:2–13
Honda H, Shimizu Y, Rutter M (2005) No effect of MMR withdrawal on the incidence of autism: a total population study. J Child Psychol Psychiatry 46(6):572–579
Jain A, Marshall J, Buikema A, Bancroft T, Kelly JP, Newschaffer CJ (2015) Autism occurrence by MMR vaccine status among US children with older siblings with and without autism. JAMA 313(15):1534–1540
Leask J, Chapman S, Hawe P, Burgess M (2006) What maintains parental support for vaccination when challenged by anti-vaccination messages? A qualitative study. Vaccine 24(49–50):7
Lo NC, Hotez PJ (2017) Public health and economic consequences of vaccine hesitancy for measles in the United States. JAMA Pediatr 171(9):887–892
Mankertz A, Mulders MN, Shulga S, Kremer JR, Brown KE, Santibanez S, Muller CP, Tikhonova N, Lipskaya G, Jankovic D, Khetsuriani N, Martin R, Gavrilin E (2011) Molecular genotyping and epidemiology of measles virus transmission in the World Health Organization European region, 2007-2009. J Infect Dis 204(Suppl 1):S335–S342
McIntosh ED, Janda J, Ehrich JH, Pettoello-Mantovani M, Somekh E (2016) Vaccine hesitancy and refusal. J Pediatr 175:248–249
McLean HQ, Fiebelkorn AP, Temte JL, Wallace GS (2013) Prevention of measles, rubella, congenital rubella syndrome, and mumps, 2013: summary recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep 62(RR-04):1–34
Rota PA, Moss WJ, Takeda M, de Swart RL, Thompson KM, Goodson JL (2016) Measles. Nature Rev Dis Primers 2:16049
Vaccine Recommendations and Guidelines of the ACIP n.d. Contraindications and precautions updates. Available from: https://www.cdc.gov/vaccines/hcp/acip-recs/general-recs/contraindications.html
World Health Organization (WHO). Renewed commitment to measles and rubella elimination and prevention of congenital rubella syndrome in the WHO European Region by 2015. Regional Committee for Europe. Sixtieth session. Moscow, 13–16 September 2010
World Health Organization (WHO). Surveillance guidelines for measles, rubella and congenital rubella syndrome in the WHO European region. Update December 2012. Available at: http://www.euro.who.int/__data/assets/pdf_file/0018/79020/e93035-2013.pdf
World Health Organization (WHO) (2012) Global measles and rubella strategic plan: 2012–2020. WHO, Geneva Available from: http://apps.who.int/iris/bitstream/10665/70254/1/WHO_IVB_10.02_eng.pdf. (accessed 30 Oct 2018)
World Health Organization (WHO). Measles. Fact sheet no 286. 2013. MRI report 2012. Available at: http://www.measlesrubellainitiative.org/wp-content/uploads/2013/07/MRI-2012-Annual-Report.pdf
Author information
Authors and Affiliations
Contributions
ALV and AG conceived the study.
ALV and MDC designed the study protocol and prepared the first draft of the survey.
AG revised and approved the survey before dissemination.
MDC, MCF, FC, and FWB administered the survey to families and caregivers.
MDC and MCF developed the database. ALV performed the statistical analysis and wrote the first draft of the manuscript. ALV and MDC produced tables and figures.
AG and MMDG provided substantial contribution to draft the paper and reviewed the final manuscript.
All authors gave their final approval of the version to be published and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Communicated by Nicole Ritz
Electronic supplementary material
Supplemental table S1
STROBE checklist (PDF 96 kb)
Supplemental figure S2
The frequency of real contraindications (black) and false contraindications and other barriers (shaded in black) are reported according to each category. On the right column, different strategies to be addressed to health-care workers and general population are proposed to improve vaccination coverage
Rights and permissions
About this article
Cite this article
Lo Vecchio, A., Cambriglia, M.D., Fedele, M.C. et al. Determinants of low measles vaccination coverage in children living in an endemic area. Eur J Pediatr 178, 243–251 (2019). https://doi.org/10.1007/s00431-018-3289-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-018-3289-5