Abstract
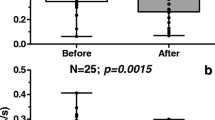
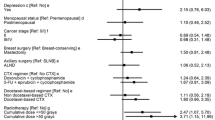
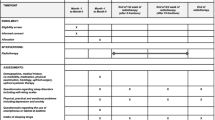
Depression, anxiety and sleep disturbances are known problems in patients with breast cancer. The effect of melatonin as an antidepressant in humans with cancer has not been investigated. We investigated whether melatonin could lower the risk of depressive symptoms in women with breast cancer in a three-month period after surgery and assessed the effect of melatonin on subjective parameters: anxiety, sleep, general well-being, fatigue, pain and sleepiness. Randomized, double-blind, placebo-controlled trial undertaken from July 2011 to December 2012 at a department of breast surgery in Copenhagen, Denmark. Women, 30–75 years, undergoing surgery for breast cancer and without signs of depression on Major Depression Inventory (MDI) were included 1 week before surgery and received 6 mg oral melatonin or placebo for 3 months. The primary outcome was the incidence of depressive symptoms measured by MDI. The secondary outcomes were area under the curve (AUC) for the subjective parameters. 54 patients were randomized to melatonin (n = 28) or placebo (n = 26) and 11 withdrew from the study (10 placebo group and 1 melatonin group, P = 0.002). The risk of developing depressive symptoms was significantly lower with melatonin than with placebo (3 [11 %] of 27 vs. 9 [45 %] of 20; relative risk 0.25 [95 % CI 0.077–0.80]), giving a NNT of 3.0 [95 % CI 1.7–11.0]. No significant differences were found between AUC for the subjective parameters. No differences in side effects were found (P = 0.78). Melatonin significantly reduced the risk of depressive symptoms in women with breast cancer during a three-month period after surgery.






Similar content being viewed by others
References
Massie MJ (2004) Prevalence of depression in patients with cancer. J Natl Cancer Inst Monogr 32:57–71
Davidson JR, MacLean AW, Brundage MD, Schulze K (2002) Sleep disturbance in cancer patients. Soc Sci Med 54:1309–1321
Hjerl K, Andersen EW, Keiding N, Mortensen PB, Jorgensen T (2002) Increased incidence of affective disorders, anxiety disorders, and non-natural mortality in women after breast cancer diagnosis: a nation-wide cohort study in Denmark. Acta Psychiatr Scand 105:258–264
Fann JR, Thomas-Rich AM, Katon WJ, Cowley D, Pepping M, McGregor BA, Gralow J (2008) Major depression after breast cancer: a review of epidemiology and treatment. Gen Hosp Psychiatry 30:112–126
Burgess C, Cornelius V, Love S, Graham J, Richards M, Ramirez A (2005) Depression and anxiety in women with early breast cancer: five year observational cohort study. BMJ 330:702
Colagiuri B, Christensen S, Jensen AB, Price MA, Butow PN, Zachariae R (2011) Prevalence and predictors of sleep difficulty in a national cohort of women with primary breast cancer three to four months postsurgery. J Pain Symptom Manage 42:710–720
Caplette-Gingras A, Savard J (2008) Depression in women with metastatic breast cancer: a review of the literature. Palliat Support Care 6:377–387
Colleoni M, Mandala M, Peruzzotti G, Robertson C, Bredart A, Goldhirsch A (2000) Depression and degree of acceptance of adjuvant cytotoxic drugs. Lancet 356:1326–1327
DiMatteo MR, Lepper HS, Croghan TW (2000) Depression is a risk factor for noncompliance with medical treatment: meta-analysis of the effects of anxiety and depression on patient adherence. Arch Intern Med 160:2101–2107
Bui QU, Ostir GV, Kuo YF, Freeman J, Goodwin JS (2005) Relationship of depression to patient satisfaction: findings from the barriers to breast cancer study. Breast Cancer Res Treat 89:23–28
Watson M, Haviland JS, Greer S, Davidson J, Bliss JM (1999) Influence of psychological response on survival in breast cancer: a population-based cohort study. Lancet 354:1331–1336
Satin JR, Linden W, Phillips MJ (2009) Depression as a predictor of disease progression and mortality in cancer patients: a meta-analysis. Cancer 115:5349–5361
Pandi-Perumal SR, Moscovitch A, Srinivasan V, Spence DW, Cardinali DP, Brown GM (2009) Bidirectional communication between sleep and circadian rhythms and its implications for depression: lessons from agomelatine. Prog Neurobiol 88:264–271
Wiebe ST, Cassoff J, Gruber R (2012) Sleep patterns and the risk for unipolar depression: a review. Nat Sci Sleep 4:63–71
Detanico BC, Piato AL, Freitas JJ, Lhullier FL, Hidalgo MP, Caumo W, Elisabetsky E (2009) Antidepressant-like effects of melatonin in the mouse chronic mild stress model. Eur J Pharmacol 607:121–125
Hickie IB, Rogers NL (2011) Novel melatonin-based therapies: potential advances in the treatment of major depression. Lancet 378:621–631
de Bodinat C, Guardiola-Lemaitre B, Mocaer E, Renard P, Munoz C, Millan MJ (2010) Agomelatine, the first melatonergic antidepressant: discovery, characterization and development. Nat Rev Drug Discov 9:628–642
Moher D, Hopewell S, Schulz KF, Montori V, Gøtzsche PC, Devereaux PJ, Elbourne D, Egger M, Altman DG (2010) CONSORT 2010 explanation and elaboration: updated guidelines for reporting parallel group randomised trials. BMJ 340:c869
Hansen MV, Madsen MT, Hageman I, Rasmussen LS, Bokmand S, Rosenberg J, Gögenur I (2012) The effect of MELatOnin on Depression, anxietY, cognitive function and sleep disturbances in patients with breast cancer. The MELODY trial: protocol for a randomised, placebo-controlled, double-blinded trial. BMJ Open 2:e000647
Folstein MF, Folstein SE, McHugh PR (1975) ”Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 12:189–198
Moller JT, Cluitmans P, Rasmussen LS, Houx P, Rasmussen H, Canet J, Rabbitt P, Jolles J, Larsen K, Hanning CD, Langeron O, Johnson T, Mauven PM, Kristensen PA, Biedler A, van Beem H, Fraidakis O, Silverstein JH, Beneken JEW, Gravenstein JS for the ISPOCD investigators (1998) Long-term postoperative cognitive dysfunction in the elderly ISPOCD1 study. International Study of Post-Operative Cognitive Dysfunction. Lancet 351:857–861
Olsen LR, Mortensen EL, Bech P (2004) Prevalence of major depression and stress indicators in the Danish general population. Acta Psychiatr Scand 109:96–103
Olsen LR, Jensen DV, Noerholm V, Martiny K, Bech P (2003) The internal and external validity of the Major Depression Inventory in measuring severity of depressive states. Psychol Med 33:351–356
Bech P, Rasmussen NA, Olsen LR, Noerholm V, Abildgaard W (2001) The sensitivity and specificity of the Major Depression Inventory, using the Present State Examination as the index of diagnostic validity. J Affect Disord 66:159–164
Akerstedt T, Gillberg M (1990) Subjective and objective sleepiness in the active individual. Int J Neurosci 52:29–37
Andersen I, Thielen K, Bech P, Nygaard E, Diderichsen F (2011) Increasing prevalence of depression from 2000 to 2006. Scand J Public Health 39:857–863
Carman JS, Post RM, Buswell R, Goodwin FK (1976) Negative effects of melatonin on depression. Am J Psychiatry 133:1181–1186
Leibenluft E, Feldman-Naim S, Turner EH, Wehr TA, Rosenthal NE (1997) Effects of exogenous melatonin administration and withdrawal in five patients with rapid-cycling bipolar disorder. J Clin Psychiatry 58:383–388
Dolberg OT, Hirschmann S, Grunhaus L (1998) Melatonin for the treatment of sleep disturbances in major depressive disorder. Am J Psychiatry 155:1119–1121
Dalton EJ, Rotondi D, Levitan RD, Kennedy SH, Brown GM (2000) Use of slow-release melatonin in treatment-resistant depression. J Psychiatry Neurosci 25:48–52
Serfaty MA, Osborne D, Buszewicz MJ, Blizard R, Raven PW (2010) A randomized double-blind placebo-controlled trial of treatment as usual plus exogenous slow-release melatonin (6 mg) or placebo for sleep disturbance and depressed mood. Int Clin Psychopharmacol 25:132–142
Rahman SA, Kayumov L, Shapiro CM (2010) Antidepressant action of melatonin in the treatment of Delayed Sleep Phase Syndrome. Sleep Med 11:131–136
Bellipanni G, Bianchi P, Pierpaoli W, Bulian D, Ilyia E (2001) Effects of melatonin in perimenopausal and menopausal women: a randomized and placebo controlled study. Exp Gerontol 36:297–310
Garzon C, Guerrero JM, Aramburu O, Guzman T (2009) Effect of melatonin administration on sleep, behavioral disorders and hypnotic drug discontinuation in the elderly: a randomized, double-blind, placebo-controlled study. Aging Clin Exp Res 21:38–42
Somerset W, Stout SC, Miller AH, Musselman D (2004) Breast cancer and depression. Oncology (Williston Park) 18:1021–1034
Pirl WF, Roth AJ (1999) Diagnosis and treatment of depression in cancer patients. Oncology (Williston Park) 13:1293–1301
Pezzella G, Moslinger-Gehmayr R, Contu A (2001) Treatment of depression in patients with breast cancer: a comparison between paroxetine and amitriptyline. Breast Cancer Res Treat 70:1–10
Kelly CM, Juurlink DN, Gomes T, Duong-Hua M, Pritchard KI, Austin PC, Paszat LF (2010) Selective serotonin reuptake inhibitors and breast cancer mortality in women receiving tamoxifen: a population based cohort study. BMJ 340:c693
Papakostas GI (2010) The efficacy, tolerability, and safety of contemporary antidepressants. J Clin Psychiatry 71(Suppl) E1:e03
Seabra ML, Bignotto M, Pinto LR Jr, Tufik S (2000) Randomized, double-blind clinical trial, controlled with placebo, of the toxicology of chronic melatonin treatment. J Pineal Res 29:193–200
Acknowledgments
This work was supported by grants from the University of Copenhagen, The Aase and Ejnar Danielsens Foundation, The A.P. Møller Foundation for the Advancement of Medical Science, The Else and Mogens Wedell Wedellborgs Foundation, The Beckett Foundation, The Hede Nielsen Family Foundation, The Dagmar Marshalls Foundation and Manufacturer Einar Willumsen’s Memorial Scholarship. These abovementioned funders have had no influence on the design and conduct of the study; collection, management analysis, and interpretation of data; preparation, review, or approval of the manuscript; or decision to submit the manuscript for publication. All these activities are done by the authors. Pharma Nord provided the melatonin and placebo tablets but had no influence on the design and conduct of the study; collection, managementanalysis and interpretation of data; preparation, review, or approval of the manuscript; or decision to submit the manuscript for publication. The study received no financial support from the industry. The authors would also like to thank Rikke Søby Andersen, research nurse, for her help with the study and the patients for their time and participation.
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical standards
The experiments comply with the current laws in Denmark.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hansen, M.V., Andersen, L.T., Madsen, M.T. et al. Effect of melatonin on depressive symptoms and anxiety in patients undergoing breast cancer surgery: a randomized, double-blind, placebo-controlled trial. Breast Cancer Res Treat 145, 683–695 (2014). https://doi.org/10.1007/s10549-014-2962-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-014-2962-2