Abstract
Background
The coronavirus disease of 2019 (COVID-19) emerged as a global pandemic. Historically, the group of human coronaviruses can also affect the central nervous system leading to neurological symptoms; however, the causative mechanisms of the neurological manifestations of COVID-19 disease are not well known. Seizures have not been directly reported as a part of COVID-19 outside of patients with previously known brain injury or epilepsy. We report two cases of acute symptomatic seizures, in non-epileptic patients, associated with severe COVID-19 disease.
Case Presentations
Two advanced-age, non-epileptic, male patients presented to our northeast Ohio-based health system with concern for infection in Mid-March 2020. Both had a history of lung disease and during their hospitalization tested positive for SARS-CoV-2. They developed acute encephalopathy days into their hospitalization with clinical and electrographic seizures. Resolution of seizures was achieved with levetiracetam.
Discussion
Patients with COVID-19 disease are at an elevated risk for seizures, and the mechanism of these seizures is likely multifactorial. Clinical (motor) seizures may not be readily detected in this population due to the expansive utilization of sedatives and paralytics for respiratory optimization strategies. Many of these patients are also not electrographically monitored for seizures due to limited resources, multifactorial risk for acute encephalopathy, and the risk of cross-contamination. Previously, several neurological symptoms were seen in patients with more advanced COVID-19 disease, and these were thought to be secondary to multi-system organ failure and/or disseminated intravascular coagulopathy-related brain injury. However, these patients may also have an advanced breakdown of the blood–brain barrier precipitated by pro-inflammatory cytokine reactions. The neurotropic effect and neuroinvasiveness of SARS-Coronavirus-2 have not been directly established.
Conclusions
Acute symptomatic seizures are possible in patients with COVID-19 disease. These seizures are likely multifactorial in origin, including cortical irritation due to blood–brain barrier breakdown, precipitated by the cytokine reaction as a part of the viral infection. Patients with clinical signs of seizures or otherwise unexplained encephalopathy may benefit from electroencephalography monitoring and/or empiric anti-epileptic therapy. Further studies are needed to elucidate the risk of seizures and benefit of monitoring in this population.
Similar content being viewed by others
Introduction
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) emerged first in Wuhan, China, in 2019 and spread rapidly worldwide as a pandemic of the twenty-first century. The symptoms and disease manifestations caused by SARS-CoV-2 were named Coronavirus disease 2019 (COVID-19) by the World Health Organization [1]. The neurological manifestations of this disease are not well known, and there is growing evidence that the disease has effects on the central nervous system (CNS) as detailed in retrospective reports from several centers worldwide. An initial retrospective case series from Wuhan, China, showed that neurological manifestations are present in patients with COVID-19 disease [2]. In that series, 45.5% of patients with COVID-19 disease who had severe systemic disease burden also suffered from acute cerebrovascular disease, acute encephalopathy, and skeletal muscle symptoms. These patients also had higher levels of inflammatory markers and greater evidence of multi-organ failure. However, the study did not elucidate how many patients with encephalopathy were monitored and treated for acute symptomatic seizures. Another series of patients were reported in Strasbourg, France, with neurological features of encephalopathy and corticospinal tract signs. Only a small proportion of the patients (8 out of 64) had electroencephalography performed, which demonstrated diffuse slowing consistent with encephalopathy [3]. Seizures have not been directly reported as a part of COVID-19 disease outside of patients with previously known brain injury or epilepsy.
There are several barriers to electrographically monitoring patients with SARS-CoV-2 infection such as prone positioning for respiratory compromise as well as the contamination risk which obviates a need for minimizing procedures in this patient population. Neurointensivists and neurologists are often consulted for severe COVID-19 patients that present with neurological features. In this report, we describe two patients who were electrographically monitored for acute encephalopathy and seizure-like activity, in the setting of normal brain imaging and who were found to have acute symptomatic seizures associated with severe COVID-19 disease.
Case #1
A 76-year-old male with history of chronic asthma on benralizumab, hypertension, chronic kidney disease, hyperlipidemia, left bundle branch block, diastolic dysfunction, and cervical fusion presented to the emergency department with the chief complaint of severe right lower extremity pain, fever (102.5 °F on presentation), and encephalopathy. He was status post recent L3-S1 laminectomy for acute lumbosacral radiculopathy 5 days prior to presentation. Laboratory workup showed neutrophilic leukocytosis (17,200 cells/mm3). He had a Glasgow coma scale of 14, was oriented to name only, and exhibited exaggerated deep tendon reflexes but had no other focal neurological deficits. A computerized tomography (CT) scan of the brain was unremarkable. Magnetic resonance imaging (MRI) of the spine revealed an epidural abscess between L4-S1. Surgical drainage was performed, and the patient was started empirically on vancomycin and piperacillin–tazobactam. Wound cultures grew Pseudomonas aeruginosa. Despite antibiotic therapy, and improved leukocytosis, he continued to have high-grade fevers and acute hypoxemic respiratory failure requiring intensive care unit transfer on postoperative day 1. He was initially managed conservatively with diuresis, preload, and afterload optimization; however, his chest X-ray rapidly progressed to bilateral interstitial and airspace opacification (Fig. 1).
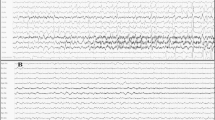
On postoperative day two, the patient suffered several episodes of left upper extremity clonic activity and worsening encephalopathy with decline in level of consciousness as evidenced by increased drowsiness and inability to follow commands. Continuous electroencephalography (EEG) confirmed three focal seizures lasting approximately 30 s each arising from the right centroparietal region (Fig. 2). Levetiracetam was initiated and both clinical and electrographic seizure activity subsided. Antibiotic regimen was broadened to Vancomycin, Meropenem, and Acyclovir for CSF coverage. MRI of the brain and cervical spine with and without contrast was remarkable only for chronic white matter hyperintensities, without acute intracranial lesions, meningeal enhancement or venous sinus thrombosis, and C5–C6 myelomalacia, respectively. Lumbar puncture was not performed due to the risk of seeding infection into neuroaxis. Given persistent high-grade fevers, worsening respiratory status requiring intubation, and recent possible exposures, a respiratory viral panel was sent in addition to separate rapid testing for COVID-19 polymerase chain reaction on postoperative day 4 and COVID-19 testing was confirmed as positive twenty-four hours later. His fibrinogen level was elevated at 631 mg/dL (normal range 200–400 mg/dL) and continued to increase to over 860 mg/dL over the following days. C-reactive protein increased from 1.7 mg/dL on prior admission to 27.3 mg/dL and remained elevated despite antimicrobial therapy. White blood cell count steadily improved over his hospitalization, and platelet count remained stable. Our patient ultimately received a tracheostomy and after 30 days of ICU stay was discharged to a long-term acute care hospital for further ventilator management.
Case #2
An 82-year-old male patient with chronic obstructive pulmonary disease, venous thromboembolic disease, complete heart block, and chronic kidney disease presented to the emergency department with a 10-day history of progressive dyspnea, altered mental status, and generalized weakness. He was found to be hypoxic, febrile, and tachycardic. He was intubated for acute hypoxemic respiratory failure with a chest X-ray showing lung infiltrates consistent with pneumonitis. The patient’s laboratory results were significant for lymphopenia (WBC 3.26 k/μl, absolute lymphocyte count 0.70), coagulopathy (international normalised ratio (INR) 2.5, partial thromboplastin time (PTT) 53.9), elevated D-dimer (590 ng/mL), thrombocytopenia (132 k/μl), acute kidney injury (blood urea nitrogen (BUN) 47 mg/dL, creatinine 3.96 mg/dL), and elevated C-reactive protein initially 12.5 mg/L and increased to 26.2 mg/L. A nasopharyngeal swab polymerase chain reaction (PCR) test for COVID-19 was sent on admission and was positive 24 h later. Continuous video electroencephalogram (EEG) monitoring was ordered on day 5 of admission after events of right eyelid and facial twitching were observed by the care team. Frequent EEG seizures were captured independently from the left more than right frontal–temporal regions (Fig. 3) which eventually progressed to focal status epilepticus. The majority of seizures were non-convulsive. Seizure frequency improved after treatment with levetiracetam. A non-contrast CT-brain demonstrated hypodensities within the supratentorial white matter, consistent with mild microvascular disease but without acute intracranial lesion. He was unable to have an MRI brain performed due to an incompatible cardiac pacemaker. Further vessel imaging was unable to be performed due to patients acute on chronic kidney injury. A lumbar puncture was unable to be performed due to worsening coagulopathy (INR 3.8, PTT 73.5). Patient remained on the ventilator, and after 20 days of ICU stay, the family opted for withdrawal of life-sustaining support.
Discussion
The SARS-Coronavirus-2 belongs to the β-coronavirus group which includes several human pathogenic viruses including middle east respiratory syndrome (MERS) coronavirus and SARS-CoV-1. These group of coronaviruses are associated with respiratory symptoms. Additional neurological symptoms including delirium, dizziness, and headaches have also been reported with other coronavirus infections prior to the SARS-CoV-2 outbreak [4]. The case series of patients from Wuhan, China, with COVID-19 disease, included both central and peripheral neurological manifestations (i.e., headache, dizziness, impaired consciousness, cerebrovascular disease, and neuralgia) [2]. Seizures were not reported as a direct manifestation of SARS-CoV-2 infection. The patients described in our series developed focal seizures and, in the second case, even progressed to non-convulsive status epilepticus. Seizures may be a CNS manifestation of COVID-19 disease. Further investigations are needed to elucidate the mechanism of neurological symptoms in SARS-CoV-2 infection.
Human coronaviruses (HCoV) have been established to infect human astrocytes and microglia in neural cell cultures as well as detection of viral RNA in a study of human brain autopsy samples supporting their neurotropic and neuroinvasive properties [5]. A case report of SARS-CoV-1 infection with CNS symptoms during the SARS epidemic also isolated the virus within a brain tissue specimen [6]. Although direct evidence of a neurotropic effect of SARS-Cov-2 has not been reported as yet through either cerebrospinal fluid (CSF) or autopsy studies, the presence of neurological symptoms in patients with COVID-19 disease during this current pandemic, and the similarity between the two strains of human coronaviruses (CoV-1 and CoV-2), makes this mechanism highly suggestive. Acute symptomatic seizures may be the result of a possible neurotropic effect of the virus or can be a marker of severity of systemic disease itself since CNS symptoms were found mainly in patients with severe COVID-19 disease. After penetration of the blood–brain barrier, the virus can slow the cerebral microcirculation, possibly through the creation of a hypercoagulable state. This allows increased interaction of SARS-CoV-2 with the endothelial receptors and receptors on glial tissue [7]. The interaction at the glia may predispose patients to seizures as seen in other neurological diseases [8, 9].
Previous studies of SARS-coronaviruses have described the proliferation of pro-inflammatory cytokines that are active in promoting blood–barrier breakdown, namely interleukin-8 (IL8) and monocyte chemoattractant protein-1 (MCP1) [10, 11]. A description of coronavirus infections in a Japanese encephalitis mouse model demonstrated CNS viral infection induced astrocyte and microglia proliferation, leading to increased release of IL-8 in the CSF [10]. MCP1 is another pro-inflammatory mediator that is expressed in CNS cells including astrocytes, neurons, and microglia. MCP1 may be up-regulated in conditions which target and degrade the blood–brain barrier and can recruit additional inflammatory cells as the monocytes migrate across the blood–brain barrier [11]. We hypothesize that as a result of the accumulation of inflammatory markers, there may be local cortical irritation that precipitates seizures related to COVID-19 infection. Although cerebrospinal fluid may contain markers of inflammation, the treatment of this infection is largely supportive, and with the additional risk of coagulopathy precipitated by SARS-CoV-2, a lumbar puncture may not be justifiable unless there is an alternative diagnosis to be sought. A limitation of our case series is that cerebrospinal fluid was unable to be obtained due to patient factors that made a lumbar puncture relatively contraindicated and that a CSF-PCR test for SARS-CoV-2 was not yet commercially available. As this disease continues to spread, we will continue to learn about its direct and/or indirect epileptogenesis.
Conclusions
Although there are concerns regarding decreasing transmission risk by limiting healthcare interventions in COVID-19 disease, patients with severe infection who demonstrate either clinical signs of seizures or severe encephalopathy may benefit from continuous electroencephalography monitoring to diagnose and treat symptomatic seizures and also non-convulsive status epilepticus. The mechanism of seizures precipitated by SARS-CoV-2 infection appears to be multifactorial and may involve a possible neurotropism of SARS-CoV-2 in addition to blood–brain barrier breakdown precipitated by pro-inflammatory cytokine reactions.
References
Shereen MA, Khan S, Kazmi A, Bashir N, Siddique R. COVID-19 infection: origin, transmission, and characteristics of human coronaviruses. J Adv Res. 2020;24:91–8.
Mao L, Wang M, Chen S, et al. Neurological manifestations of hospitalized patients with COVID-19 in Wuhan, China: a retrospective case series study. SSRN Electron J. 2020. https://doi.org/10.2139/ssrn.3544840.
Helms J, Kremer S, Merdji H, et al. Neurologic features in severe SARS-CoV-2 infection. New Engl J Med. 2020. https://doi.org/10.1056/NEJMc2008597.
Steardo L, Zorec R, Verkhratsky A. Neuroinfection may contribute to pathophysiology and clinical manifestations of COVID-19. Acta Physiol. 2020. https://doi.org/10.1111/apha.13473.
Arbour N, Day R, Newcombe J, Talbot PJ. Neuroinvasion by human respiratory coronaviruses. J Virol. 2000;74(19):8913–21.
Xu J, Zhong S, Liu J, et al. Detection of severe acute respiratory syndrome coronavirus in the brain: potential role of the chemokine mig in pathogenesis. Clin Infect Dis. 2005;41(8):1089–96.
Baig AM, Khaleeq A, Ali U, Syeda H. Evidence of the COVID-19 virus targeting the CNS: tissue distribution, host-virus interaction, and proposed neurotropic mechanisms. ACS Chem Neurosci. 2020;11(7):995–8.
Newey CR, Kinzy T, Punia V, Hantus S. Continuous electroencephalography in the critically ill: clinical and continuous electroencephalography markers for targeted monitoring. J Clin Neurophys. 2018;35:325–31.
Koch M, Uyttenboogaart M, Polman S, DeKeyser J. Seizures in multiple sclerosis. Epilepsia. 2008;49:948–53.
Li Y, Li H, Fan R, et al. Coronavirus infections in the central nervous system and respiratory tract show distinct features in hospitalized children. Intervirology. 2016;59(3):163–9.
Yao Y, et al. Monocyte chemoattractant protein-1 and the blood–brain barrier. Cell Mol Life Sci. 2013;71(4):683–97.
Funding
The authors as listed above have received no source of financial support for this manuscript.
Author information
Authors and Affiliations
Contributions
The authors listed have contributed equally to the creation and revisions of this manuscript.
Corresponding author
Ethics declarations
Conflict of interest
None of the authors listed have received any financial support for this manuscript and have no conflicts of interest to disclose.
Ethical approval/Informed consent
This study was approved by the instiutional board review of the Cleveland Clinic as a minimal risk quality improvement project and informed consent was waived.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hepburn, M., Mullaguri, N., George, P. et al. Acute Symptomatic Seizures in Critically Ill Patients with COVID-19: Is There an Association?. Neurocrit Care 34, 139–143 (2021). https://doi.org/10.1007/s12028-020-01006-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-020-01006-1