Abstract
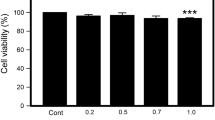
Neutrophil granulocytes are the largest leukocyte population in the blood and major players in the innate immune response. Impaired neutrophil function has been reported in in vivo studies with zinc-deficient human subjects and experimental animals. Moreover, in vitro formation of neutrophil extracellular traps has been shown to depend on free intracellular Zn2+. This study investigates the requirement of Zn2+ for several other essential neutrophil functions, such as chemotaxis, phagocytosis, cytokine production, and degranulation. To exclude artifacts resulting from indirect effects of zinc deprivation, such as impaired hematopoietic development and influences of other immune cells, direct effects of zinc deprivation were tested in vitro using cells isolated from healthy human donors. Chelation of Zn2+ by the membrane permeable chelator N,N,N′,N′-tetrakis-(2-pyridylmethyl)-ethylenediamine (TPEN) reduced granulocyte migration toward N-formyl-l-methionyl-l-leucyl-l-phenylalanine (fMLF) and IL-8, indicating a role of free intracellular Zn2+ in chemotaxis. However, a direct action of Zn2+ as a chemoattractant, as previously reported by others, was not observed. Similar to chemotaxis, phagocytosis, oxidative burst, and granule release were also impaired in TPEN-treated granulocytes. Moreover, Zn2+ contributes to the regulatory role of neutrophil granulocytes in the inflammatory response by affecting the cytokine production by these cells. TPEN inhibited the lipopolysaccharide-induced secretion of chemotactic IL-8 and also anti-inflammatory IL-1ra. In conclusion, free intracellular Zn2+ plays essential roles in multiple neutrophil functions, affecting extravasation to the site of the infection, uptake and killing of microorganisms, and inflammation.





Similar content being viewed by others
References
Amulic B, Cazalet C, Hayes GL et al (2012) Neutrophil function: from mechanisms to disease. Annu Rev Immunol 30:459–489. doi:10.1146/annurev-immunol-020711-074942
Lee WL, Harrison RE, Grinstein S (2003) Phagocytosis by neutrophils. Microbes Infect 5:1299–1306
Vieira OV, Botelho RJ, Grinstein S (2002) Phagosome maturation: aging gracefully. Biochem J 366:689–704. doi:10.1042/BJ20020691
Dahlgren C, Karlsson A (1999) Respiratory burst in human neutrophils. J Immunol Methods 232:3–14
Borregaard N, Cowland JB (1997) Granules of the human neutrophilic polymorphonuclear leukocyte. Blood 89:3503–3521
Brinkmann V, Reichard U, Goosmann C et al (2004) Neutrophil extracellular traps kill bacteria. Science 303:1532–1535. doi:10.1126/science.1092385
Cassatella MA (1995) The production of cytokines by polymorphonuclear neutrophils. Immunol Today 16:21–26
Schröder AK, von der Ohe M, Kolling U et al (2006) Polymorphonuclear leucocytes selectively produce anti-inflammatory interleukin-1 receptor antagonist and chemokines, but fail to produce pro-inflammatory mediators. Immunology 119:317–327. doi:10.1111/j.1365-2567.2006.02435.x
Kumar V, Sharma A (2010) Neutrophils: Cinderella of innate immune system. Int Immunopharmacol 10:1325–1334. doi:10.1016/j.intimp.2010.08.012
Keen CL, Gershwin ME (1990) Zinc deficiency and immune function. Annu Rev Nutr 10:415–431. doi:10.1146/annurev.nu.10.070190.002215
Björkstén B, Bäck O, Gustavson KH et al (1980) Zinc and immune function in Down’s syndrome. Acta Paediatr Scand 69:183–187
Briggs WA, Pedersen MM, Mahajan SK et al (1982) Lymphocyte and granulocyte function in zinc-treated and zinc-deficient hemodialysis patients. Kidney Int 21:827–832
Dreno B, Vandermeeren MA, Boiteau HL et al (1986) Plasma zinc is decreased only in generalized pustular psoriasis. Dermatologica 173:209–212
Weston WL, Huff JC, Humbert JR et al (1977) Zinc correction of defective chemotaxis in acrodermatitis enteropathica. Arch Dermatol 113:422–425
Sheikh A, Shamsuzzaman S, Ahmad SM et al (2010) Zinc influences innate immune responses in children with enterotoxigenic Escherichia coli-induced diarrhea. J Nutr 140:1049–1056. doi:10.3945/jn.109.111492
Hujanen ES, Seppä ST, Virtanen K (1995) Polymorphonuclear leukocyte chemotaxis induced by zinc, copper and nickel in vitro. Biochim Biophys Acta 1245:145–152
Hasegawa H, Suzuki K, Nakaji S, Sugawara K (2000) Effects of zinc on the reactive oxygen species generating capacity of human neutrophils and on the serum opsonic activity in vitro. Luminescence 15:321–327. doi:10.1002/1522-7243(200009/10)15:5<321::AID-BIO605>3.0.CO;2-O
Hasan R, Rink L, Haase H (2012) Zinc signals in neutrophil granulocytes are required for the formation of neutrophil extracellular traps. Innate Immunol 19:253–264. doi:10.1177/1753425912458815
Haase H, Rink L (2014) Multiple impacts of zinc on immune function. Metallomics 6:1175–1180. doi:10.1039/c3mt00353a
Yamasaki S, Sakata-Sogawa K, Hasegawa A et al (2007) Zinc is a novel intracellular second messenger. J Cell Biol 177:637–645. doi:10.1083/jcb.200702081
Haase H, Ober-Blöbaum JL, Engelhardt G et al (2008) Zinc signals are essential for lipopolysaccharide-induced signal transduction in monocytes. J Immunol 181:6491–6502. doi:10.4049/jimmunol.181.9.6491
Kitamura H, Morikawa H, Kamon H et al (2006) Toll-like receptor-mediated regulation of zinc homeostasis influences dendritic cell function. Nat Immunol 7:971–977. doi:10.1038/ni1373
Brieger A, Rink L, Haase H (2013) Differential regulation of TLR-dependent MyD88 and TRIF signaling pathways by free zinc ions. J Immunol 191:1808–1817. doi:10.4049/jimmunol.1301261
Altstaedt J, Kirchner H, Rink L (1996) Cytokine production of neutrophils is limited to interleukin-8. Immunology 89:563–568
Park JH, Grandjean CJ, Antonson DL, Vanderhoof JA (1986) Effects of isolated zinc deficiency on the composition of skeletal muscle, liver and bone during growth in rats. J Nutr 116:610–617
Luecke RW, Simonel CE, Fraker PJ (1978) The effect of restricted dietary intake on the antibody mediated response of the zinc deficient A/J mouse. J Nutr 108:881–887
Shi HN, Scott ME, Stevenson MM, Koski KG (1998) Energy restriction and zinc deficiency impair the functions of murine T cells and antigen-presenting cells during gastrointestinal nematode infection. J Nutr 128:20–27
Vruwink KG, Fletcher MP, Keen CL et al (1991) Moderate zinc deficiency in rhesus monkeys. An intrinsic defect of neutrophil chemotaxis corrected by zinc repletion. J Immunol 146:244–249
Graves V, Gabig T, McCarthy L et al (1992) Simultaneous mobilization of Mac-1 (CD11b/CD18) and formyl peptide chemoattractant receptors in human neutrophils. Blood 80:776–787
Sengeløv H, Boulay F, Kjeldsen L, Borregaard N (1994) Subcellular localization and translocation of the receptor for N-formylmethionyl-leucyl-phenylalanine in human neutrophils. Biochem J 299(Pt 2):473–479
Condliffe AM, Kitchen E, Chilvers ER (1998) Neutrophil priming: pathophysiological consequences and underlying mechanisms. Clin Sci (Lond) 94:461–471
Volk APD, Barber BM, Goss KL et al (2011) Priming of neutrophils and differentiated PLB-985 cells by pathophysiological concentrations of TNF-α is partially oxygen dependent. J Innate Immunol 3:298–314. doi:10.1159/000321439
Mollinedo F, Nakajima M, Llorens A et al (1997) Major co-localization of the extracellular-matrix degradative enzymes heparanase and gelatinase in tertiary granules of human neutrophils. Biochem J 327(Pt 3):917–923
Sengeløv H, Kjeldsen L, Kroeze W et al (1994) Secretory vesicles are the intracellular reservoir of complement receptor 1 in human neutrophils. J Immunol 153:804–810
Carlos TM, Harlan JM (1994) Leukocyte-endothelial adhesion molecules. Blood 84:2068–2101
Lominadze G, Powell DW, Luerman GC et al (2005) Proteomic analysis of human neutrophil granules. Mol Cell Proteomics 4:1503–1521. doi:10.1074/mcp.M500143-MCP200
Schröder AK, Uciechowski P, Fleischer D, Rink L (2006) Crosslinking of CD66B on peripheral blood neutrophils mediates the release of interleukin-8 from intracellular storage. Hum Immunol 67:676–682. doi:10.1016/j.humimm.2006.05.004
Borregaard N (2010) Neutrophils, from marrow to microbes. Immunity 33:657–670. doi:10.1016/j.immuni.2010.11.011
Chavakis T, May AE, Preissner KT, Kanse SM (1999) Molecular mechanisms of zinc-dependent leukocyte adhesion involving the urokinase receptor and beta2-integrins. Blood 93:2976–2983
Parks WC, Wilson CL, López-Boado YS (2004) Matrix metalloproteinases as modulators of inflammation and innate immunity. Nat Rev Immunol 4:617–629. doi:10.1038/nri1418
Papayannopoulos V, Metzler KD, Hakkim A, Zychlinsky A (2010) Neutrophil elastase and myeloperoxidase regulate the formation of neutrophil extracellular traps. J Cell Biol 191:677–691. doi:10.1083/jcb.201006052
May RC, Machesky LM (2001) Phagocytosis and the actin cytoskeleton. J Cell Sci 114:1061–1077
Fällman M, Andersson R, Andersson T (1993) Signaling properties of CR3 (CD11b/CD18) and CR1 (CD35) in relation to phagocytosis of complement-opsonized particles. J Immunol 151:330–338
Mansfield PJ, Hinkovska-Galcheva V, Shayman JA, Boxer LA (2002) Granulocyte colony-stimulating factor primes NADPH oxidase in neutrophils through translocation of cytochrome b(558) by gelatinase-granule release. J Lab Clin Med 140:9–16
Arend WP, Malyak M, Guthridge CJ, Gabay C (1998) Interleukin-1 receptor antagonist: role in biology. Annu Rev Immunol 16:27–55. doi:10.1146/annurev.immunol.16.1.27
Prasad AS, Beck FWJ, Bao B et al (2008) Duration and severity of symptoms and levels of plasma interleukin-1 receptor antagonist, soluble tumor necrosis factor receptor, and adhesion molecules in patients with common cold treated with zinc acetate. J Infect Dis 197:795–802. doi:10.1086/528803
Acknowledgments
We thank Dr. Jörg Häseler, TU Berlin, for critically reading the manuscript. This study was supported in part by German Research Council (DFG) grant HA4318/3 to H. H. Furthermore, R. H. received a scholarship from the German Academic Exchange Service (DAAD).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hasan, R., Rink, L. & Haase, H. Chelation of Free Zn2+ Impairs Chemotaxis, Phagocytosis, Oxidative Burst, Degranulation, and Cytokine Production by Neutrophil Granulocytes. Biol Trace Elem Res 171, 79–88 (2016). https://doi.org/10.1007/s12011-015-0515-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12011-015-0515-0