Abstract
Purpose
Studies evaluating the association between statins and colorectal cancer (CRC) have used various methods to address bias and have reported mixed findings. We sought to assess the association in a large cohort of residents in Emilia-Romagna, Italy, using multiple methods to address different sources of confounding. We also sought to explore potential effect measure modification by sex.
Methods
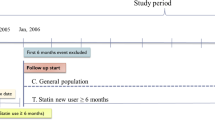
We conducted a retrospective cohort study using the 2003–2010 healthcare database of Emilia-Romagna, Italy. We identified all initiators of statins; initiators of glaucoma medications served as the comparison group to account for confounding by healthy user bias. We followed patients longitudinally to identify CRC cases in hospital discharge data. We used multivariable Cox regression analyses to adjust for confounding by CRC risk factors and we conducted a sensitivity analysis using propensity score matching.
Results
After multivariable adjustment, initiators of statins had a lower incidence rate of CRC as compared to initiators of glaucoma drugs [hazard ratio (HR) 0.79; 95 % CI 0.69–0.90]. In sex-stratified analyses we observed a protective effect in men (HR 0.77; 95 % CI 0.67–0.88) but not in women (HR 0.96; 95 % CI 0.82–1.1). Results were similar in propensity score analyses.
Conclusions
After adjusting for observed risk factors, statin initiation versus glaucoma drug initiation was associated with a reduced risk of CRC in men but not in women. While this study is subject to many limitations, it corroborates a previous study that found sex differences in the association between statins and CRC.
Similar content being viewed by others
References
Kleinrock M (2011) The use of medicines in the united states: review of 2010. Retrieved from http://www.imshealth.com/deployedfiles/imshealth/Global/Content/IMSInstitute/StaticFile/IHII_UseOfMed_report.pdf
Jasinska M, Owczarek J, Orszulak-Michalak D (2007) Statins: a new insight into their mechanisms of action and consequent pleiotropic effects. Pharmacol Rep 59:483–499
Boudreau DM, Yu O, Johnson J (2010) Statin use and cancer risk: a comprehensive review. Expert Opin Drug Saf 9(4):603–621
Hachem C, Morgan R, Johnson M, Kuebeler M, El-Serag H (2009) Statins and the risk of colorectal carcinoma: a nested case–control study in veterans with diabetes. Am J Gastroenterol 104(5):1241–1248
Marelli C, Gunnarsson C, Ross S, Haas S, Stroup DF, Cload P, Clopton P, DeMaria AN (2011) Statins and risk of cancer: a retrospective cohort analysis of 45,857 matched pairs from an electronic medical records database of 11 million adult Americans. J Am Coll Cardiol 58:530–537
Peto R, Emberson J, Landray M, Baigent C, Collins R, Clare R, Califf R (2008) Analyses of cancer data from three ezetimibe trials. N Engl J Med 359:1357–1366
Newman TB, Hulley SB (1996) Carcinogenicity of lipid-lowering drugs. JAMA 275:55–60
Suh N, Reddy BS, DeCastro A, Paul S, Lee HJ, Smolarek AK, So JY, Simi B, Wang CX, Janakiram NB, Steele V, Rao CV (2011) Combination of atorvastatin with sulindac or naproxen profoundly inhibits colonic adenocarcinomas by suppressing the p65/β-catenin/cyclin D1 signaling pathway in rats. Cancer Prev Res 4:1895–1902
Schreiber S, Nikolaus S, Hampe J (1998) Activation of nuclear factor kappa B inflammatory bowel disease. Gut 42:477–484
Ray WA (2003) Evaluating medication effects outside of clinical trials: new-user designs. Am J Epidemiol 158(9):915–920
Danaei G, Tavakkoli M, Hernan MA (2012) Bias in observational studies of prevalent users: lessons for comparative effectiveness research from a meta-analysis of statins. Am J Epidemiol 175(4):250–262
Friedman GD, Flick ED, Udaltsova N, Chan J, Quesenberry CP, Habel LA (2008) Screening statins for possible carcinogenic risk: up to 9 years of follow-up of 361,859 recipients. Pharmacoepidemiol Drug Saf 17(1):27–36
Poynter JN, Gruber SB, Higgins PD, Almog R, Bonner JD, Rennert HS, Low M, Greenson JK, Rennert G (2005) Statins and the risk of colorectal cancer. N Engl J Med 352(21):2184–2192
Setoguchi S, Glynn RJ, Avorn J, Mogun H, Schneeweiss S (2007) Statins and the risk of lung, breast, and colorectal cancer in the elderly. Circulation 115:27–33
Glynn RJ et al (2001) Paradoxical relations of drug treatment with morality in older persons. Epidemiology 12:682–689
Maio V, Yuen E, Rabinowitz C, Louis D, Jimbo M, Donatini A, Mall S, Taroni F (2005) Using pharmacy data to identify those with chronic conditions in Emilia Romagna, Italy. J Health Serv Res Policy 10(4):232–238
Louis D, Yuen EJ, Maio V, Rabinowitz C, Robeson M, Smith K, Gonnella JS (2005) A population-based longitudinal healthcare database in the Emilia-Romagna Region, Italy: a resource for planning and research. Health Policy Newsl 2005:18
ACT/DDD Index WHO collaborating centre for drug statistics methodology. Available at http://www.whocc.no/atcddd/
Quan H, Sundararajan V, Halfon P, Fong A, Burnand B, Luthi JC, Saunders LD, Beck CA, Feasby TE, Ghali WA (2005) Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care 43(11):1130–1139
Schneeweiss S, Wang PS, Avorn J, Gynn RJ (2003) Improved comorbidity adjustment for predicting mortality in medicare populations. Health Serv Res 38(4):1103–1120
Rosenbaum PR, Rubin DB (1983) The central role of the propensity score in observational studies for causal effects. Biometrika 70(1):41–55
Cepdeda MS, Boston R, Farrar JT, Strom BL (2003) Comparison of logistic regression versus propensity score when the number of events is low and there are multiple confounders. Am J Epidemiol 158:280–287
Rubin DB (2010) On the limitations of comparative effectiveness research. Stat Med 29:1991–1995
Bardou M, Barkun A, Martel M (2010) Effect of statin therapy on colorectal cancer. Gut 59:1572–1585
Johnson JR, Lacey JV, Lazovich D, Geller MA, Schairer C, Schatzkin A, Flood A (2009) Menopausal hormone therapy and risk of colorectal cancer. Cancer Epidemiol Biomarkers Prev 18:196–203
Newcomb P, Pocobelli G, Chia V (2008) Why hormones protect against large bowel cancer? Adv Exp Biol 617:259–269
Schachter M (2005) Chemical, pharmacoeconomic and pharmacodynamic properties of statins: an update. Fundam Clin Pharmacol 19(1):117–125
Coogan P, Rosenberg L, Strom B (2007) Statins and cancer. Epidemiology 18(4):520–521
Crocetti E, Buzzoni C, Zappa M (2010) Colorectal cancer incidence rates have decreased in central Italy. Eur J Cancer Prev 19:424–425
Yuen E, Louis D, Cisbani L, Rabinowitz C, De Palma R, Maio V, Leoni M, Grilli R (2011) Using administrative data to identify and stage breast cancer cases: implications for assessing quality of care. Tumori 97:428–435
Acknowledgments
We thank Roberto Grilli, MD, from the Regional Health Care and Social Agency, Regione Emilia-Romagna, Italy; Eleonora Verdini, BS, from the Health Care Authority, Regione Emilia-Romagna, Italy; Daniel Z. Louis, MS, from the Center for Research in Medical Education and Health Care, Thomas Jefferson University, Philadelphia, PA, USA; and Emanuela Masini, MD, from the School of Medicine, University of Florence, Italy. VM affirms that everyone who contributed significantly to this work has been listed. This research was supported through a collaborative agreement between the Regional Health Care and Social Agency, Regione Emilia-Romagna, Italy; the Health Care Authority, Regione Emilia-Romagna, Italy; and the Thomas Jefferson University, Philadelphia, PA, USA. The authors’ work was independent of the funders, and this paper accurately represents the study results. The study sponsors played no roles in the design or conduct of the study; in the collection, management, analysis, or interpretation of data; in the writing of the manuscript; or in the decision to submit the article for publication.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Clancy, Z., Keith, S.W., Rabinowitz, C. et al. Statins and colorectal cancer risk: a longitudinal study. Cancer Causes Control 24, 777–782 (2013). https://doi.org/10.1007/s10552-013-0160-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-013-0160-x