The information in the PDF below is suggested for inclusion into local safety guidelines. It may be helpful to stimulate personal thought, research, and consideration as it compares with information provided by “medical experts”. The articles in following sections provide depth to the summary information in the Safety Protocols below.
The following guidelines have been proposed to various government entities for integration into “official” guidelines. They represent a simplified condensation of more scientific data. They are not a substitute for good judgement – they are a helpful starting point for those with limited science backgrounds. Please use the condensed Safety Protocols until you have the time to read and understand the more detailed source articles. If these ideas can benefit and add to your area’s “official” guidelines, please benefit.
Click Here To Skip Elementary Information And Go To The Science
COVID19SafetyPrototols2020909a




“All identified outbreaks of three or more cases occurred in an indoor environment, which confirms that sharing indoor space is a major SARS-CoV-2 infection risk.”

Viral Load Exposure Factors
While aerosolized indoor transmission has been recognized herein since April 2020, on October 5th, 2020, the CDC formally recognized that aerosol transmission of SARS-CoV-2 is a significant contributor to COVID-19 infections.
The CDC currently defines a close contact as “Someone who was within 6 feet of an infected person for at least 15 minutes“. It appears to indicate that the CDC considers brief contact on the order of a few minutes or few seconds as very unlikely to cause transmission. Unfortunately, the CDC is not more specific about the very large differences between indoor and outdoor transmission risks. Outdoor areas, such as parks and ocean beaches, with natural high volume air exchange that greatly dilutes any viral loads which may be present, results in dramatically decreased levels of transmission relative to indoor areas.
A larger initial exposure viral load can cause increased severity because the exponential viral replication reaches much higher levels before the immune system can respond. This results in dramatically greater viral damage. The increased viral presence also tends to activate a more intense immune response which may result in increased systemic damage from the immune response. Reducing viral loads into a variolative or minor infection range can significantly reduce the likelihood of a severe case. A regular regimen of a few cycles of normal daily exercise improves immune response / speed pre-exposure and immediately following exposure to minimize likelihood of illness.
It is possible to minimize severity of illness by slowing the exponential growth of viral load that develops shortly after exposure which helps the adaptive immune response to mature before exponential viral growth becomes extremely large. The innate immune response tends to slow natural infections; and intelligent behavior (such as using viral inactivation substances such as mouthwash, toothpaste, essential oils / breath-mints / breath-strips, zinc, small amounts of ethyl alcohol, etc.), can slow the exponential growth such that B/T cell activation /maturation occurs before exponential growth of antigen becomes large. Mints and essential oils have been recognized as helpful for many centuries, and many modern mouthwashes that kill bacteria and inactivate viruses are now essential oil rather than alcohol based. Swishing fractions of an ounce of high-percentage ethyl alcohol (hard liquor) into the throat area with tickle/minor-irritation every few hours tends to slow viral growth, although once viral damage to the tissues becomes significant, this tends to create further irritation / tissue damage; and larger amounts of ethyl alcohol may negatively impact immune system response, so this tends to be optimal only for very early “tickle” stages of illness. Placing 1/16th of a zinc supplement (nibble off a small piece) and/or a few grains of salt in room temperature or slightly warm water will make the water much more pleasant to drink, which may help you to remain well hydrated. The zinc also seems to have a throat soothing effect (try it) and may have some mild topical protective characteristics and this tends to be effective in both early and later stages of illness. Just a nibble of a zinc mineral supplement and a few grains of salt go a long way and also tend to make water less irritating to the sore throat – thus encouraging increased hydration which is also helpful. Salt water gargling tends to be helpful. Swishing saliva around within the mouth and onto irritated areas helps to keep them moist and in some cases will help mucosal antibodies find and bind to viruses that may be present near the irritated area that is replicating virus. This can be particularly helpful during re-exposures and in later stages of infections where significant virus specific antibodies may be present within the saliva. Histamine responses also tend to increase likelihood of antibody encounters with viruses within mucosal tissues and also help to purge virus from the body through sneeze and runny nose responses.
It is likely that many infections and transmissions can be avoided or minimized through the use of breath-mints / breath strips during and following potential exposure encounters.
When sick, highly aerobic activity can undesirably facilitate virus movement deeper within the airway and into the lungs, yet light exercise such as walking can stimulate blood/lymph flow without resulting the deep respiration that internally spreads virus within the airway. Similarly, fresh air and avoiding rebreathing “sick-room” viral laden air can help avoid spreading the infection within the airway. Perhaps obviously, keeping considerable physical distance from others while enjoying fresh outdoor air will dilute any viral load that might be shedding when sick and wearing masks can help while in careful transit to some wide open personal space containing fresh air.
A study entitled “COVID-19 Aerosolized Viral Loads, Environment, Ventilation, Masks, Exposure Time, Severity, And Immune Response : A Pragmatic Guide Of Estimates” provides example scenarios and estimates infection risk for people who are not yet immune via vaccine or natural infection recovery. The study is built upon a reference case of a non-infected person in an indoor environment within 2 to 4.8 meters of 2 infected persons. It uses that reference data to estimate the time necessary to cause various exposure levels and resulting infection potential in various indoor and outdoor settings of both Influenza A and COVID-19.
The study helps answer the questions:
How long may a person safely remain within various environments?
What exposure levels could result in immunity without becoming ill via asymptomatic graduated inoculation?
A few observations from this study include:
- It can be shown that over 94% of COVID-19 superspreading events occurred in limited ventilation areas suggesting that aerosolized transmission is a strong contributor to COVID-19 infections.
- In a defined outdoor area with 3 MPH wind has 1056 air exchanges/hour. Typical office is 6 ACPH. Typical home/windows-closed, 0.3 ACPH. Outdoors dilute viral load over 3000x relative to home and over 150x relative to office. Typical office dilutes viral load 20x relative to closed home.
- A level of exercise after exposure can improve the probability and speed of immune response by accelerating viral movement into the Secondary Lymphoid Organs’ (SLO) germinal centers. Regular light to moderate intensity exercise can improve immune response. Light intensity exercise can improve recovery times.
- Specific time duration estimates and likely symptom result estimates given a person with very good general health for many example scenarios
- It could take about 3 hours exercising hard (60 LPM) in a 3 MPH outdoor wind 2 meters from a sick person with neither wearing masks to reach the Minor “cold like” Illness exposure level estimate
- It could take about 15 hours doing light work (12 LPM) in a 3 MPH outdoor wind 2 meters from a sick person with neither wearing masks to reach the Minor “cold like” Illness exposure level estimate
- It could take about 1 hour doing light work (12 LPM) in a 6 ACPH office 2 meters from a sick person with both wearing surgical masks to reach the Minor “cold like” Illness exposure level estimate
- It could take about 8 hours doing light work (12 LPM) in a 6 ACPH office 2 meters from a sick person with both wearing surgical masks to reach the Mild “flu like” Illness exposure level estimate
- It could take about 1 hour doing light work (12 LPM) in a 6 ACPH office 2 meters from a sick person with neither wearing masks to reach the Mild “flu like” Illness exposure level estimate
- It could take about 2 minutes doing light work (12 LPM) in a 0.2 ACPH closed home 2 meters from a where a sick person was resting for many hours (loading up the room air with virus) with neither wearing masks to reach the Mild “flu like” Illness exposure level estimate.
- It could take about 20 minutes doing light work (12 LPM) in a 0.2 ACPH closed home 2 meters from a where a sick person was resting for many hours (loading up the room air with virus) with neither wearing masks to reach the Possibly Severe Illness exposure level estimate.
- Raising ventilation of an indoor space from 6 to 24 ACPH would likely extend these estimates by about 4x. Many activities could become safer with increased ventilation.
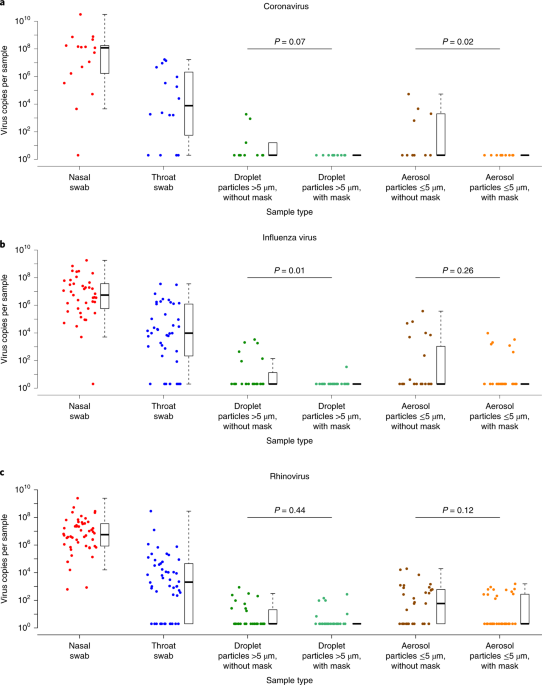
- Both sick and exposed individuals wearing surgical masks would likely extend non-masked estimates by about 9x. Many activities could become safer with mask use. Combining increased ventilation further extends safer periods.
- Increasing the exposure level by 10x is likely to step a Minor “cold like” exposure to a Mild “flu like” exposure.
- Increasing the exposure level by 10x is likely to step a Mild “flu like” exposure to a “Possibly Severe” exposure level.
- It is likely that most severe cases develop from exposures that occur within poor ventilation environments such as closed homes or from very close contact scenarios.
- Every individual’s risk tolerance and optimal exposure level is different. Individuals with health concerns should seek to avoid all exposure. Those already recovered may benefit from light re-exposure challenges that preserve IgA and IgG antibody titer levels and related protective or even sterilizing immunity
- The estimates in the study may help efforts to strike a balance in developing holistic epidemiologic interventions that consider the effects of these interventions on economic, civic, social, and mental health, which have pathologies within their own realms
- In the absence of better information, these estimates should be considered only with additional good judgement and after further verification. Human response to pathogens is widely variant and these estimations assume the normal healthy population with better than average immune response, no co-morbidities, and a very specific set of scenarios.
The estimates found in this study could be a significant improvement over current WHO and CDC guidelines in that they provide specific quantitative number estimates based on data from peer-reviewed studies. The estimates cover various environments include typical ASHRAE office ventilation standards, one example of dramatically improved ventilation (4x), and outdoor 3 MPH conditions. The estimates also consider the infected person as either very sick or pre-symptomatic, the level of exertion of those breathing the air in the vicinity of the infected, with and without masks, and then identifies 4 levels of various Likely Outcomes from Not Ill to Possible Severe Illness.

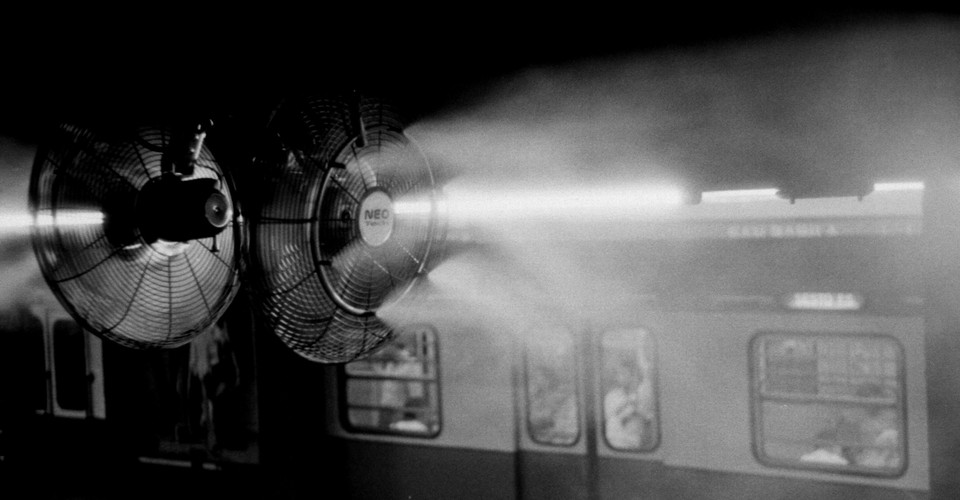
A typical $20 box fan provides ventilation of approximately 1000 to 2000 CFM. A typical school classroom is about 1000 square feet with ceiling heights ranging from 8 to 12 feet, which calculates to volumes up to 12,000 cubic feet. If 2 fans (inlet/exhaust) were used at 2 openings to achieve a fresh air flow of 2000 CFM in a 10,000 cubic foot room, this would translate to 12 ACPH, or even higher when used in conjunction with existing ventilation. Given distance to avoid large droplets, surgical mask use indoors, and Table 2 from the above study, this would result in a scenario that would be about 50% likely to result in minor “cold like” illness levels (not flu “MMID” like) after 22 hours of exposure with an early pre-symptomatic individual present, or about 1.5 hours with a sick individual present. Mild flu-like (MMID) symptoms would be about 20% likely to develop after 16 hours with a sick individual present. In younger adults and children, all of these scenarios would be likely to result in no infection or an asymptomatic case that has some probability of generating immunity without symptoms. Protective focus on teachers could use greater distance between them and students. Vaccinated and natural-infection-recovered teachers likely remove so much overall risk such that no interventions are necessary. Until then, it is likely that 2 box fans per classroom arranged to create a through-flow air exchange would create a dramatically improved and likely tolerable infection risk level for most students and teachers. Special considerations could be applied for those at higher risk for a severe infection. Given that acquiring 2 box fans per-classroom of 20+ students might create a supply issue, it is likely that family / community loans from concerned Parent / Teacher Associations could meet needs for the first year of this intervention. If a box fan lacks the desired elegance of a public entity, examine how potholes are fixed in the streets of major cities so that roads may be used without damaging auto suspension. Cost-effective solutions can be acquired more rapidly than those of great elegance, such as the vaccines to come, which are more like re-paving the road for the long-term. Many office buildings with ASHRAE standard 6 ACPH would likely support low-risk part-time adult in-office work and fans can help assist with ventilation there as well by diluting average viral load to a level below symptomatic infectious dose, which could result in immunity without illness. Again, those at higher risk for severity require special consideration.
For those on the go: Introductory video blog brief overview of
COVID-19 Aerosolized Viral Loads, Environment, Ventilation, Masks, Exposure Time, Severity, And Immune Response: A Pragmatic Guide Of Estimates





are increasing again. We have learnt a lot about SARS-CoV-2 and our ability to test
for and manage COVID-19 has improved, but ongoing debate remains about how SARS-CoV-2
is transmitted.




Ok, was trying to stay off Twitter until Saturday but this question of children masking outdoors (in camps, etc.) keeps coming up. Let's discuss #outdoortransmission. Viral particles disperse quickly in the outside airhttps://t.co/VWJe2Gt2os
— Monica Gandhi MD, MPH (@MonicaGandhi9) May 6, 2021
Also see: Immunology


Surface Transmission, Temperature, Humidity, And Inactivation
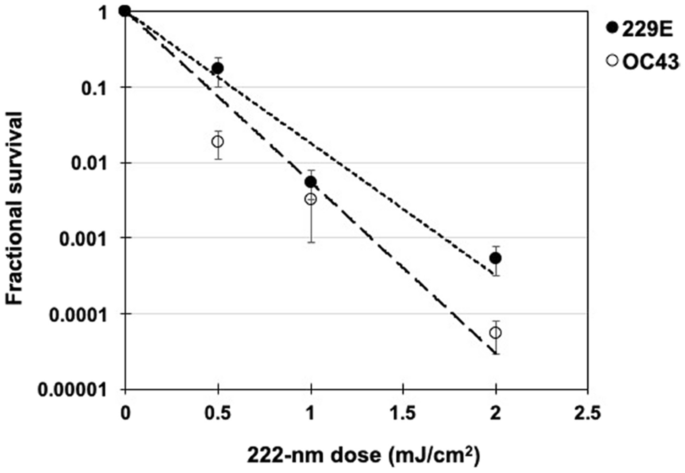
Coronaviruses are a type of virus that have an outer wrapping or envelope that contains the RNA that enables the virus to replicate. This envelope comes from the infected cell, or host, in a process called “budding”. During the budding process, newly formed virus particles become “enveloped” or wrapped in an outer coat that is made from a small piece of the cell’s plasma membrane which is usually delicate mucousal cellular tissue. Anything that sufficiently damages that membrane / envelope (or the spike) will inactivate / kill the virus because the envelope and it’s exterior spike protein protrusions are what enable it to invade a new cell. The RNA still exists, and can fool a PCR viral presence test into a false positive, but without the envelope and spike protein structure, there is no way for the viral RNA to invade a cell. Additionally, damage to the RNA is also likely to inactivate the virus.
Coronaviruses tend to remain viable longest on smooth, non-porous surfaces and in low temperatures. Any “slimy” mucous or liquid surrounding the viruses may help protect the virus envelope from damage. Higher temperatures result in increased brownian-motion which tends to damage the viral envelope over time. Porous surfaces which are generally not smooth to the touch, tend to abrade, chemically react with, help dissolve, or otherwise damage the delicate viral envelope or spike protein. One study shows that coronaviruses tend to be inactivated most at relative humidity of around 50%, gain survival at higher humidity, and survive best at around 20% RH. Another study shows that coronaviruses tend to be inactivated with higher humidity and survive best at lower humidity. Humidity impact appears to be dependent upon many factors. Soap, alcohol, and “essential oils” are known to provide some level of inactivation. Most enveloped viruses are fairly easy to damage / inactivate.
Physically, the SARS-CoV-2 virus is about 0.1 micrometers diameter. An average grain of sand in Hermosa Beach, CA is about 300 micrometers diameter (“average” grains measured with digital caliper). This means that the average grain of sand is about 3000 times larger than the delicate viral envelope. If trapped between grains of sand being walked-upon or vigorously agitated between hands with pressure and rolling action, the virus would likely be destroyed and/or separated from other virions reducing available viral load. It has been demonstrated that viruses are inactivated by high pressure, mechanical agitation, very high frequency ultrasound (and possibly lower frequencies), and mechanical shear forces.
Much is still unknown about surface transmission. Many studies that use PCR testing (for example this CDC publication / Chinese Study) may not be valid as noted above. There are many scholars that believe it is not easily transmitted on surfaces beyond approximately 30 minutes (German scientists in publication below). There are other studies that indicate otherwise. The general consensus appears to be that surface transmission is more rare than aerosol and droplet transmission. Those who are at high-risk for a severe case would likely want to use additional surface sanitizing precautions, erring on the side of safety versus convenience.

health concern causing severe respiratory tract infections in humans. Human-to-human
transmissions have been described with incubation times between 2-10 days, facilitating
its spread via droplets, contaminated ha…







Virus Inactivation












Indoor Contained Air vs Outdoor Air
Outdoor areas, such as parks and ocean beaches, with natural high volume air exchange that greatly dilutes any viral loads which may be present, results in dramatically decreased levels of transmission relative to indoor areas. General population use of masks in essential shared indoor areas such as grocery stores and other businesses helps to keep that indoor air pristine and free of viruses so that care-givers are less likely to bring the virus into areas where they are caring for those at high risk for a severe case.
Ok, was trying to stay off Twitter until Saturday but this question of children masking outdoors (in camps, etc.) keeps coming up. Let's discuss #outdoortransmission. Viral particles disperse quickly in the outside airhttps://t.co/VWJe2Gt2os
— Monica Gandhi MD, MPH (@MonicaGandhi9) May 6, 2021

Indoors At Home
Regarding viral transmission, outdoor groups and professional office settings appear to be statistically safer than indoor families.
“The riskiest place could be our homes”
“Possible rates of household transmission — anywhere from 5 to 30 percent”
Due to the potential for large viral loads to be transmitted over long periods of time in close proximity within the home, the probability of transmission / increased-severity are higher among people co-habitating relative to many other settings. Outdoors environments and professional office settings with ventilation and air-exchange disease prevention optimizations are much lower risk.
When co-habitating, it may be important to wear face coverings and improve ventilation so that the risk more closely approaches the many order of magnitude safer outdoor environments; which data shows to be very low even without use of safety protocols and Non Pharmaceutical Interventions (NPI).
However impractical it may be, it would be more epidemiologically prudent to mandate that people temporarily suspend co-habitation than nearly any other non-super-spreading activity.
With that challenge in mind, education and innovation can enable intelligent, situationally specific, solutions that surpass government mandated edicts that tend to lead to social dysfunction and mental health challenges. The importance of holistic community health includes factors that include and surpass simply limiting viral transmission.
Regarding viral transmission, outdoor groups and well ventilated professional settings appear to be statistically safer than indoor families.






“Household contact was the main setting for transmission of SARS-CoV-2, and the risk for transmission of SARS-CoV-2 among close contacts increased with the severity of index cases”








Vocalizing,Setting5: Refrigeration,Date added/Last updated
ATA1,Antarctica,Antarctica Peninsu…



“Some situations may be particularly risky. Meatpacking plants are likely vulnerable because many people work closely together in spaces where low temperature helps the virus survive. But it may also be relevant that they tend to be loud places, Knight says. The report about the choir in Washington made her realize that one thing links numerous clusters: They happened in places where people shout or sing. And although Zumba classes have been connected to outbreaks, Pilates classes, which are not as intense, have not, Knight notes. “Maybe slow, gentle breathing is not a risk factor, but heavy, deep, or rapid breathing and shouting is.””

Jun 15, 2020: “Right now, I’m feeling pretty upset, pretty sad because they’re good people,” she said. “There’s a lot of good people in there.”



Keep Bathtub and Floor Drains Filled With Water
Disease transmission may occur when “water traps” in floor and bathtub drains are allowed to dry out. If a bathtub or floor drain is left unused and not re-filled with water for a few weeks, sewage gases can enter the room because they are not trapped by water in the “U” shaped water barrier used in plumbing to trap sewer gases. This is particularly important in apartments, condominiums. high-rise buildings, and other high-density housing. “Bioaerosols can be controlled at the source by avoiding any potential gas leaks from the drainage system to indoor spaces. For example, to block fecal aerosol transmission, drainage traps, such as U-shaped water traps, should not be allowed to dry out.” Viral loads allowed to enter and concentrate indoors when lack of ventilation does not allow the viral load to diffuse, dilute, and escape can be particularly infectious when people remain indoors for long periods of time such as sleeping. This can be particularly problematic during colder periods when windows may be closed.

Ocean beaches
Ocean beaches and other land areas close to extremely large bodies of water develop breezes due to water and land temperature differences. These breezes effectively create strong natural sources of ventilation and air exchange which greatly dilutes any viral loads which may be present resulting in dramatically decreased levels of transmission relative to indoor areas. During the day, UV light from the sun very significantly helps to inactivate coronaviruses. Higher temperatures help as well. Since the eyes are one of the primary viral entry points, sunglasses and other protective eye-wear has been shown to significantly reduce infection probability. Porous surfaces such as sand tend to damage the viral envelope (think cellular membrane since coronaviruses “bud” from cellular tissue and use that cellular membrane to create the viral envelope). Anything that sufficiently damages that fragile membrane / envelope will inactivate / kill the virus. Exercise, walking, running, or other activity will increase blood and lymph flow increasing the random chance that any pathogen will encounter a leukocyte that will slow or halt infection. In addition, when moving along outdoor bike / foot paths, transmission is very unlikely during brief encounters. While these attributes of typical ocean beaches use are each helpful individually, the combination of voluminous fresh air exchange, bright sunlight including UV, warmer temperatures, protective eye-wear, harsh surfaces. and exercise work together to drastically reduce any viral load encountered and minimize probability of becoming sick. In fact, with a small viral load and a highly responsive immune system, it may be possible to gain some level of immunity with no or very mild symptoms.
Pool Parties
Significant numbers of outbreaks have been traced to pool parties. Some physical science realities may be linked to the occurrence of transmission at pool parties. Given many of the principles noted above, there exists convincing evidence that contained airspace increases chance of transmission as the virus accumulates in that limited airspace. Keeping in mind that, when swimming, one’s mouth, nose, and eyes are only inches away from the water surface, it may easily be understood that the volume of airspace below the face is not the same in a pool as it is when standing upright (5 feet or so). Any breeze is also often limited as the pool surface is several inches below ground level. This often creates a slow moving “contained airspace” which enables the viral loads to accumulate within the walls of the pool rather than blow away as easily as when one’s head is 5 feet above ground level where the wind blows more strongly than it does only inches above the pool water surface. Additionally, pools tend to be enclosed within walled areas to protect children from entering inadvertently, further limiting open air space and air movement at the water level. While the chlorine in the pool does help inactivate any virus present and any UV light from the sun does as well, the stagnant air volume between the surface of the water and the pool edges makes for a very limited airspace. Using fans to create additional ventilation over the pool surface can be helpful. Also, since most pool parties include an indoor element, using appropriate safety protocols in the indoor areas can also be helpful. Pools in wide open spaces, lakes, and certainly ocean areas with wave motion tend to have greater air movement which reduces the risk of a contained air-space.
Face Mask / Coverings Benefits and Challenges And Other NPI
Masks are important when people are in close proximity for significant periods of time. If just passing somebody briefly or keeping a good distance masks are unnecessary (barring an ill-timed point blank range sneeze or cough). Masks are most helpful indoors where someone who doesn’t yet know they are sick will contain many virus containing droplets within the mask and help keep the indoor air cleaner, especially helpful when air volume per person is small, ventilation is inadequate, and people are in close proximity. Masks are extremely helpful for protecting our high-risk populations in environments such as grocery and other places where low-risk, high-risk, and those caring for high-risk populations intermingle. Mask usage in commonly shared indoor environments enables low-risk populations to continue day to day economic and socially helpful behavior while helping to shield high-risk populations from exposure in the shared environments. High risk populations should use masks and avoid crowded areas.
Masks also accumulate and grow bacteria over time and can be unhelpful to the wearer which should be balanced against any benefit they provide toward containing viral laden droplets. Oxygen level changes due to wearing a mask are generally not a concern at most altitudes. Importantly, face masks also provide a barrier that helps one avoid touching their nose. It also provides a psychological benefit of feeling protected which can reduce stress in some people during viral outbreaks and subsidence transitional times; and lower stress helps improve immune health.





of 1 m or more and provide quantitative estimates for models and contact tracing to
inform policy. Optimum use of face masks, respirators, and eye protection in public
and health-care settings should be informed by …


Register today: https://us02web.zoom.us/webinar/register/WN_xXdHU_zpRqOZaonjy7teKA Cost: $25.00 2020 has become an unprecedented year for reasons that don\’t need to be explained. And it is with disappointment that AAPS had to announce that our in-person annual meeting would not be held largely d…



Regarding concern about lower oxygen levels wearing masks, keep in mind that respiration rate autonomously changes to keep blood oxygen saturation levels (and CO2 levels) appropriate for whatever level of physical exertion / oxygen use is occurring from moment to moment.

/https%3A%2F%2Fspecials-images.forbesimg.com%2Fimageserve%2F5e9884f7a5551f0007387486%2F0x0.jpg%3FcropX1%3D0%26cropX2%3D640%26cropY1%3D6%26cropY2%3D367)
Also see: Staying Healthy
Miscellaneous
YMCA camp on Lake Burton, Georgia, the weather on June 17 low of 53 and high of 62 and June 20 had a low of 55 and high of 81. First symptom report of “chills” was June 22? Per promo video, many fresh water lake activities, indoor activities, and possibly wind-sheltered areas, close proximity activities, shared surfaces / fomites, mostly pre-teens?






health-care workers. This Viewpoint of infectious aerosols is intended to inform appropriate
infection control measures to protect health-care workers. Studies of cough aerosols
and of exhaled breath from patients w…
Asthma, while somewhat increasing risk, does not appear to be a large contributor to increased risk. In this study, the 2 of 26 patients with asthma who did not survive also had hypertension and other heart-related comorbidities that were very high risk factors.

One study indicates surprising results:
“Lead researcher on this team Dan Nicolau, an associate professor at QUT, explained that the asthmatics and those with chronic lung disease and chronic obstructive pulmonary disease (COPD) were on regular inhaler therapy with corticosteroids, were found to have a lesser risk of severe illness in the early phase of the pandemic. He said that this was paradoxical because those with long term lung disease were initially considered to be at a higher risk of a respiratory viral infection such as SARS-CoV-2. He said in his statement, “This seemed paradoxical because COVID-19 affects the lungs – and these patients have lung problems – so they should be more at risk of severe disease from the virus.”” The results in asthma patients are also correlating positively with steroidal treatment benefits in non-asthma patients.



