Abstract
Background
Aneurysmal subarachnoid hemorrhage (SAH) is associated with high mortality and long-term functional impairment. Data on clinical management and functional outcomes from developing countries are scarce. We aimed to define patient profiles and clinical practices and evaluate long-term outcomes after SAH in a middle-income country.
Methods
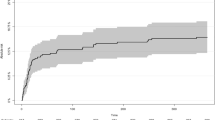
This was a prospective study including consecutive adult patients admitted with SAH to two reference centers in Brazil from January 2016 to February 2020. The primary outcome was functional status at 6 months using the modified Rankin Scale. Mixed multivariable analysis was performed to determine the relationship between clinical variables and functional outcomes.
Results
From 471patients analyzed, the median time from symptom onset to arrival at a study center was 4 days (interquartile range 0–9). Median age was 55 years (interquartile range 46–62) and 353 (75%) patients were women. A total of 426 patients (90%) were transferred from nonspecialized general hospitals, initial computed tomography revealed thick hemorrhage in 73% of patients (modified Fisher score of 3 or 4), and 136 (29%) had poor clinical grade (World Federation of Neurological Surgeons score of 4 or 5). A total of 312 (66%) patients underwent surgical clipping, and 119 (25%) underwent endovascular coiling. Only 34 patients (7%) underwent withdrawal or withholding of life-sustaining therapy during their hospital stay, and in-hospital mortality was 24%. A total of 187 (40%) patients had an unfavorable long-term functional outcome (modified Rankin Scale score of 4 to 6). Factors associated with unfavorable outcome were age (adjusted odds ratio [OR] 1.05, 95% confidence interval [CI] 1.03–1.08), hypertension (adjusted OR 1.81, 95% CI 1.04–3.16), poor clinical grade (adjusted OR 4.92, 95% CI 2.85–8.48), external ventricular drain (adjusted OR 3.8, 95% CI 2.31–6.24), postoperative deterioration (adjusted OR 2.33, 95% CI 1.32–4.13), cerebral infarction (adjusted OR 3.16, 95% CI 1.81–5.52), rebleeding (adjusted OR 2.95, 95% CI 1.13–7.69), and sepsis (adjusted OR 2.68, 95% CI 1.42–5.05).
Conclusions
Our study demonstrated that SAH management in a middle-income country diverges significantly from published cohorts and current guidelines, despite comparable clinical profiles on presentation and admission to high-volume referral centers. Earlier aneurysm occlusion and increased use of endovascular therapy could potentially reduce modifiable in-hospital complications and improve functional outcomes in Brazil.



Similar content being viewed by others
References
Okazaki T, Kuroda Y. Aneurysmal subarachnoid hemorrhage: intensive care for improving neurological outcome. J Intensive Care. 2018;6:28.
Flynn L, Andrews P. Advances in the understanding of delayed cerebral ischaemia after aneurysmal subarachnoid haemorrhage. F1000Research [Internet] 2015 [cited 2018 Jun 30];4. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4752028/
Burns SK, Brewer KJ, Jenkins C, Miller S. Aneurysmal subarachnoid hemorrhage and vasospasm. AACN Adv Crit Care. 2018;29(2):163–74.
van Gijn J, Kerr RS, Rinkel GJE. Subarachnoid haemorrhage. Lancet Lond Engl. 2007;369(9558):306–18.
Johnston SC, Selvin S, Gress DR. The burden, trends, and demographics of mortality from subarachnoid hemorrhage. Neurology. 1998;50(5):1413–8.
Truelsen T, Bonita R, Duncan J, Anderson NE, Mee E. Changes in subarachnoid hemorrhage mortality, incidence, and case fatality in New Zealand between 1981–1983 and 1991–1993. Stroke. 1998;29(11):2298–303.
Alcalá-Cerra G, Young AMH, Paternina-Caicedo Á, Ribas ESC. Trends in the mortality of non-traumatic subarachnoid hemorrhage in Colombia: a 10-year analysis of a nationwide registry. Arq Neuropsiquiatr. 2013;71(11):841–5.
Cruz C, Campuzano-Rincón JC, Calleja-Castillo JM, et al. Temporal trends in mortality from ischemic and hemorrhagic stroke in Mexico, 1980–2012. J Stroke Cerebrovasc Dis. 2017;26(4):725–32.
de Santana NM, Dos Santos Figueiredo FW, de Melo Lucena DM, et al. The burden of stroke in Brazil in 2016: an analysis of the global burden of disease study findings. BMC Res Notes. 2018;11(1):735.
Dantas LF, Marchesi JF, Peres IT, Hamacher S, Bozza FA, Quintano Neira RA. Public hospitalizations for stroke in Brazil from 2009 to 2016. PLoS ONE. 2019;14(3): e0213837.
Brant LCC, Nascimento BR, Passos VMA, et al. Variações e diferenciais da mortalidade por doença cardiovascular no Brasil e em seus estados, em 1990 e 2015: estimativas do Estudo Carga Global de Doença. Rev Bras Epidemiol. 2017;20:116–28.
Lotufo PA, Goulart AC, Fernandes TG, Benseñor IM. A reappraisal of stroke mortality trends in Brazil (1979–2009). Int J Stroke. 2013;8(3):155–63.
Kurtz P, Taccone FS, Bozza FA, et al. Systemic severity and organ dysfunction in subarachnoid hemorrhage: a large retrospective multicenter cohort study. Neurocrit Care. 2020. https://doi.org/10.1007/s12028-020-01139-3.
Gonçalves B, Turon R, Mendes A, et al. Effect of early brain infarction after subarachnoid hemorrhage: a systematic review and meta-analysis. World Neurosurg. 2018;115:e292–8.
Lucci FR, Lereis VP, Ameriso S, et al. Mortalidad intrahospitalaria por accidente cerebrovascular. 2013;4.
Yáñez Lermanda A, Ruiz-Aburto AA. Tratamiento de la hemorragia subaracnoidea aneurismática en el Hospital Clínico de la Universidad de Chile. Rev Médica Chile. 2014;142(8):982–8.
Diringer MN, Bleck TP, ClaudeHemphill J, et al. Critical care management of patients following aneurysmal subarachnoid hemorrhage: recommendations from the neurocritical care society’s multidisciplinary consensus conference. Neurocrit Care. 2011;15(2):211–40.
Connolly ES, Rabinstein AA, Carhuapoma JR, et al. Guidelines for the management of aneurysmal subarachnoid hemorrhage: a guideline for healthcare professionals from the American heart association/American stroke association. Stroke. 2012;43(6):1711–37.
Ruiz-Sandoval JL, Cantú C, Chiquete E, et al. Aneurysmal subarachnoid hemorrhage in a Mexican multicenter registry of cerebrovascular disease: the renamevasc study. J Stroke Cerebrovasc Dis. 2009;18(1):48–55.
Drake CG. Report of world federation of neurological surgeons committee on a universal subarachnoid hemorrhage grading scale. J Neurosurg. 1988;68(6):985–6.
Claassen J, Bernardini GL, Kreiter K, et al. Effect of cisternal and ventricular blood on risk of delayed cerebral ischemia after subarachnoid hemorrhage: the fisher scale revisited. Stroke. 2001;32(9):2012–20.
Vergouwen MDI, Vermeulen M, van Gijn J, et al. Definition of delayed cerebral ischemia after aneurysmal subarachnoid hemorrhage as an outcome event in clinical trials and observational studies: proposal of a multidisciplinary research group. Stroke. 2010;41(10):2391–5.
Lindegaard KF, Nornes H, Bakke SJ, Sorteberg W, Nakstad P. Cerebral vasospasm diagnosis by means of angiography and blood velocity measurements. Acta Neurochir (Wien). 1989;100(1–2):12–24.
Singer M, Deutschman CS, Seymour CW, et al. The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA. 2016;315(8):801–10.
van Swieten JC, Koudstaal PJ, Visser MC, Schouten HJ, van Gijn J. Interobserver agreement for the assessment of handicap in stroke patients. Stroke. 1988;19(5):604–7.
Baggio JAO, Santos-Pontelli TEG, Cougo-Pinto PT, et al. Validation of a structured interview for telephone assessment of the modified Rankin Scale in Brazilian stroke patients. Cerebrovasc Dis Basel Switz. 2014;38(4):297–301.
Leifer D, Fonarow GC, Hellkamp A, et al. Association between hospital volumes and clinical outcomes for patients with nontraumatic subarachnoid hemorrhage. J Am Heart Assoc. 2021;10(15): e018373.
Hammer A, Steiner A, Ranaie G, et al. Impact of comorbidities and smoking on the outcome in aneurysmal subarachnoid hemorrhage. Sci Rep. 2018;8:12335.
Mourelo-Fariña M, Pértega S, Galeiras R. A model for prediction of in-hospital mortality in patients with subarachnoid hemorrhage. Neurocrit Care. 2021;34(2):508–18.
van Donkelaar CE, Bakker NA, Birks J, et al. Impact of treatment delay on outcome in the international subarachnoid aneurysm trial. Stroke. 2020;51(5):1600–3.
Molyneux AJ, Kerr RSC, Yu L-M, et al. International subarachnoid aneurysm trial (ISAT) of neurosurgical clipping versus endovascular coiling in 2143 patients with ruptured intracranial aneurysms: a randomised comparison of effects on survival, dependency, seizures, rebleeding, subgroups, and aneurysm occlusion. Lancet Lond Engl. 2005;366(9488):809–17.
Suarez JI. Diagnosis and management of subarachnoid hemorrhage. Contin Minneap Minn. 2015;21(5):1263–87.
Kassell NF, Torner JC, Haley EC, Jane JA, Adams HP, Kongable GL. The international cooperative study on the timing of aneurysm surgery. Part 1: overall management results. J Neurosurg. 1990;73(1):18–36.
D’Andrea G, Picotti V, Familiari P, Barbaranelli C, Frati A, Raco A. Impact of early surgery of ruptured cerebral aneurysms on vasospasm and hydrocephalus after SAH: our preliminary results. Clin Neurol Neurosurg. 2020;192: 105714.
Lanzino G, Kassell NF. Double-blind, randomized, vehicle-controlled study of high-dose tirilazad mesylate in women with aneurysmal subarachnoid haemorrhage. Part II. A cooperative study in North America. J Neurosurg. 1999;90(6):1018–24.
Wartenberg KE, Schmidt JM, Claassen J, et al. Impact of medical complications on outcome after subarachnoid hemorrhage. Crit Care Med. 2006;34(3):617–23.
Etminan N, Beseoglu K, Eicker SO, Turowski B, Steiger H-J, Hänggi D. Prospective, randomized, open-label phase II trial on concomitant intraventricular fibrinolysis and low-frequency rotation after severe subarachnoid hemorrhage. Stroke. 2013;44(8):2162–8.
Arakawa Y, Kikuta K, Hojo M, et al. Milrinone reduces cerebral vasospasm after subarachnoid hemorrhage of WFNS grade IV or V. Neurol Med Chir (Tokyo). 2004;44(8):393–400.
Kurogi R, Kada A, Ogasawara K, et al. Effects of case volume and comprehensive stroke center capabilities on patient outcomes of clipping and coiling for subarachnoid hemorrhage. J Neurosurg. 2020;134(3):929–39.
Lee JY, Heo NH, Lee MR, et al. Short and long-term outcomes of subarachnoid hemorrhage treatment according to hospital volume in Korea: a nationwide multicenter registry. J Korean Med Sci. 2021;36(22): e146.
Funding
This study was financed in part by the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior, Brazil, Finance Code 001. No additional funding was available for this study.
Author information
Authors and Affiliations
Contributions
FAB, PK, CR, RT, BG, FM, and CR contributed to the study conception and design, and data interpretation. VC, MP, TS, NC, and CR performed data collection and adjudication. PK and BG performed data processing and statistical analysis. PK, CR, and BG and TS, DG, and TG drafted the first version or critically reviewed the article. FAB, PK, FM, and CR supervised the study. All authors had full access to data, participated in data interpretation, revised the article, and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the article. All authors declare that they have no conflict of interest.
Ethical Approval
This article adheres to ethical guidelines and was approved by the Ethics Review Board of the Evandro Chagas National Institute of Infectious Diseases—Oswaldo Cruz Foundation (Rio de Janeiro). The data were de-identified for analysis.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Gonçalves, B., Rynkowski, C., Turon, R. et al. Clinical Characteristics and Outcomes of Patients with Aneurysmal Subarachnoid Hemorrhage: A Prospective Multicenter Study in a Middle-Income Country. Neurocrit Care 38, 378–387 (2023). https://doi.org/10.1007/s12028-022-01629-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-022-01629-6