Acute ischaemic stroke (AIS) is a devastating disease with high mortality and even higher permanent disability. While systemic fibrinolysis has been the first-line therapy for the past two decades, endovascular mechanical thrombectomy (EMT) now represents a new standard of care in specific subsets of AIS patients1. However, the availability of EMT varies widely across Europe2 (Figure 1) and better access is needed. However, following the strategy currently adopted by the neuro-community of limiting EMT to a small group of neurointerventional specialists in highly specialised centres will probably leave the status quo frozen for years to come. Can we do any better than that?
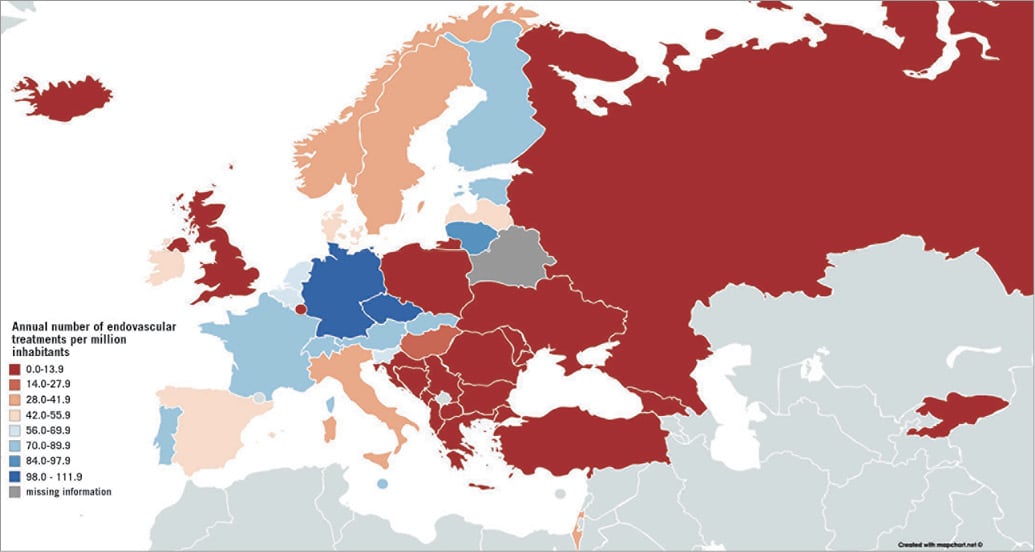
Figure 1. Map of estimated current annual rates of EMT per one million population in 43 European countries (mean 37.1, 95% CI: 26.7-47.5). With permission from2.
Similar to the management of patients with acute coronary syndromes (ACS), the effectiveness of treatment in AIS patients depends on three critical factors - time to treatment, non-stop direct access to EMT and instant availability of skilled EMT-trained teams and operators.
The optimum time-to-treatment is achieved if treatment can be delivered at sites closest to the patient’s home. Furthermore, it has been observed that EMT is utilised the most at sites closest to the patient3. Thus, regional networks (similar to those established in Europe over the past 20 years to treat patients with acute coronary syndromes [ACS]) rather than centralised networks are needed. Because all established ACS centres already provide non-stop services, extension to service AIS patients would represent equipment-related and educational challenges rather than an operational challenge.
To begin with, three main topics would need to be addressed. First, equipment providing high-resolution images of the cerebral vessels is needed, though this should be feasible when we take into account that the majority of manufacturers offer reasonably priced software, upgrades of their existing coronary systems, if needed. Secondly, cardiologists would have to become members of interdisciplinary stroke teams led by neurologists. While functioning stroke teams including interventional cardiologists have been established in some hospitals, the larger stage continues to be dominated by the policy considerations of relevant professional societies. To end this stalemate, the Stroke Council of the European Society of Cardiology is committed to reaching a consensus with all partners primarily represented by the European Stroke Organization (ESO). Establishment of a cross-disciplinary board regulating the stroke team modus operandi, including EMT, should be the first short-term (12 months) goal, with establishment of the EMT curriculum and EMT training centres being a close second. Thirdly, a reasonable number of expert EMT operators must be trained and brought into practice.
Cardiologists are no strangers to stroke care. While stroke is a classic neurological disease, the majority of strokes have cardiovascular causes. Thus, cardiologists traditionally played an important role in stroke prevention by providing comprehensive management of cardiovascular risk factors including atrial fibrillation, recently recognised as the most important cause of embolic stroke of undetermined source (ESUS), and patent foramen ovale as the cause of AIS in selected populations. Strokes complicate heart failure and congenital heart disease and, when associated with cardiovascular interventions, are also of major concern for cardiologists in daily clinical practice.
Interventional cardiologists are primarily trained in endovascular interventions of heart diseases, with an increasing number of interventional programmes including training in treatments of peripheral artery disease, including carotid artery stenting (CAS). In fact, CAS was introduced into cardiology in 1993 after Gary Roubin, then cardiologist at the University of Alabama at Birmingham, was approached by a neurologist Jay Yadav to learn interventional techniques and after teaming up with an interventional neuroradiologist Jiri Vitek (personal communication). Today, some twenty-five years down the road, hundreds of cardiologists worldwide are performing CAS interventions expertly.
Currently, the main obstacle to teaching cardiologists to perform EMT is the lack of support from the neuro community. In most countries this prevents cardiologists from entering the field of interventional stroke management. Several neuro societies produced a multi-society consensus document for training that covers the complete neurointerventional spectrum and virtually excludes interventional cardiologists from obtaining the required qualification, unless they are prepared to complete the entire neurointerventional curriculum4. For experienced interventional cardiologists, the full-time neuro training is neither realistic nor necessary for two reasons: first, no active interventional cardiologist can leave his/her work for two years to learn a single additional procedure and, second, there is no need for interventional cardiologists to learn other intracranial procedures as those procedures will be performed by neuroradiologists. As a consequence, the full training requirement practically excludes interventional cardiologists from participating in acute stroke care and, more importantly, it halts access of thousands of AIS patients to the now established standards of care.
To overcome this impasse, the leaders of both the neuro and cardio communities are urged to resume collaboration. The benefit of patients, and not the particular interests of the specialty, should guide our efforts. It appears sensible to base decisions about the participation of interventional cardiologists in AIS interventional management on two criteria: successful certified training of experienced interventional cardiologists in EMT, and the introduction of external quality assurance programmes, similar to that implemented in CAS, e.g., in Germany5.
In 2016 the European Society of Cardiology (ESC) formed the Council on Stroke to focus on issues related to stroke and to build bridges to other specialists in the field. In its first position paper, the Council suggested that interventional cardiologists should be adequately trained for EMT and interdisciplinary communication would help improve the outcomes of AIS patients6.
To overcome the shortage of EMT expertise and access within a reasonable timeframe of three to five years and to assure high-quality care to the majority of AIS patients in Europe, it appears reasonable to complement the existing workforce of neurointerventional radiologists by interventional cardiologists properly trained in EMT joining the interdisciplinary stroke teams led by neurologists.
Based on the level of cardiologists’ interventional experience a three-tier approach is proposed.
The first tier concerns interventional cardiologists without prior exposure to cerebrovascular interventions. To enter the EMT curriculum, completed certified training in interventional cardiology and at least three years’ subsequent experience including primary PCI for STEMI as first operator would be required. Cardiologists from countries without certified training in interventional cardiology would be required to provide an official document issued by the responsible body (e.g., the National Society of Cardiology) confirming the required qualification and experience. Based on the authors’ experience and that of other colleagues, ≤3 months of focused traning of these experienced interventional cardiologists should be sufficient to obtain the required EMT expertise.
Proposed contents of training include:
1. Supervised carotid and/or vertebral angiography (a total of ≥25 digital subtraction angiography [DSA] procedures as the first operator – previous documented experience included).
2. Supervised carotid stenting (a total of ≥25 procedures as the first operator – previous documented experience included).
3. Acute stroke thrombectomy: ≥20 patients (at least 10 as first operator and the remaining 10 as second operator).
4. Participation in at least ≥50 acute stroke hospital admissions and team decision making including neurologic evaluation, National Institutes of Health Stroke Scale (NIHSS) scoring, and cross-sectional image evaluation.
5. Documented e-learning, computer simulation training and/or related literature (e.g., stroke guidelines, neurointervention guidelines, etc.) reading.
The second tier concerns interventional cardiologists with prior experience as first operators in CAS procedures. For this group, points 3-5 would apply. Ideally, cardiologists in the first and second tier should undergo the proposed curriculum as full-time neuro training. However, where full-time release of a cardiologist from his/her practice is not possible, the training could be obtained on a part-time basis. Simulator training may be included in the training programme at an early stage to become familiar with the technical aspects of CAS and/or EMT procedures. Simulator-based training using modules designed to develop the skills required for CAS and EMT procedures can be employed and may account for up to 20% of cases required for certification.
The third tier concerns interventional cardiologists already performing EMT. Cardiologists in this group would need to provide certified evidence of all procedures, as specified in the first tier contents of training. Procedural and clinical outcome for all documented procedures (CAS, EMT) would need to be provided. If the documentation fulfilled the stated criteria, then no additional training would be required.
When a new centre for acute stroke interventions is established, it should be acceptable to start with one or two interventionists and to add more subsequently based on the case load.
In addition to the training in EMT, specific site requirements applicable to all centres offering EMT services would need to be fulfilled to obtain EMT privileges. These site requirements should include the following:
1. The need for interventional cardiologists to enter the stroke training should be assessed locally, based on the unmet needs of stroke patients in the given region. Differences between cities and rural areas and local distinctions would need to be taken into account.
2. The hospitals performing acute stroke interventions must provide at least the following services: neurology (or stroke medicine), a dedicated stroke unit, interventional cardiology, radiology, anaesthesiology and intensive care medicine on a 24/7/365 basis. Availability of neurosurgery on site is recommended. If not available on site, specific organisation for support from a neurosurgical centre is mandatory. In tertiary centres providing dedicated full-scale neurointerventional services, interdisciplinary collaborations should be cultivated.
3. Cardiologists should not perform intracranial procedures other than EMT. Patients with any intracranial interventions other than acute EMT should be referred to fully trained neurointerventionists.
To assure the quality of EMT treatment, continuous independent external quality control should be established.
1. Patients’ demographics should include detailed data on symptoms, including NIHSS scale indication and the outcome of brain imaging studies before and after the intervention.
2. All patients should be seen by a neurologist prior to and after the intervention; the results of neurologic examination should be detailed and documented.
3. The indication for EMT based on a consensus decision of the team led by a neurologist should be documented.
4. Procedural details including any relevant complications should be documented.
5. Clinical outcome up to 90 days after the index intervention should be provided.
As much as the participation of cardiologists in the management and care of AIS patients is endorsed, a word of caution is necessary. While similarities between heart and brain endovascular interventions exist, major differences must be recognised. In particular, two comments appear pertinent. First, while the heart is a delicate pump, in the majority of cases it sustains function following injury. In contrast, in the brain with its myriads of highly specialised centres, the loss of function is often permanent and devastating, despite neuronal plasticity. Consequently, the conduct of EMT requires not only the greatest diligence but also an understanding of the brain’s radiographic anatomy and corresponding functions. Second, while in ACS the status of microcirculation is not routinely assessed following interventions, it is customary in AIS using brain scans following EMT. Differences between revascularisation and reperfusion outcomes may constitute in some cases a sobering experience.
There is no doubt that cardiologists should play an active role in the managment of AIS patients and, more specifically, in the conduct of EMT. To help our patients suffering from AIS, mutual trust and close collaboration of all players under the leadership of neurologists as well as tight quality control will become essential.
Conflict of interest statement
The authors have no conflicts of interest to declare.